Infrared Thermographic Evaluation of Temperature Modifications Induced during Implant Site Preparation with Steel vs. Zirconia Implant Drill
Abstract
1. Introduction
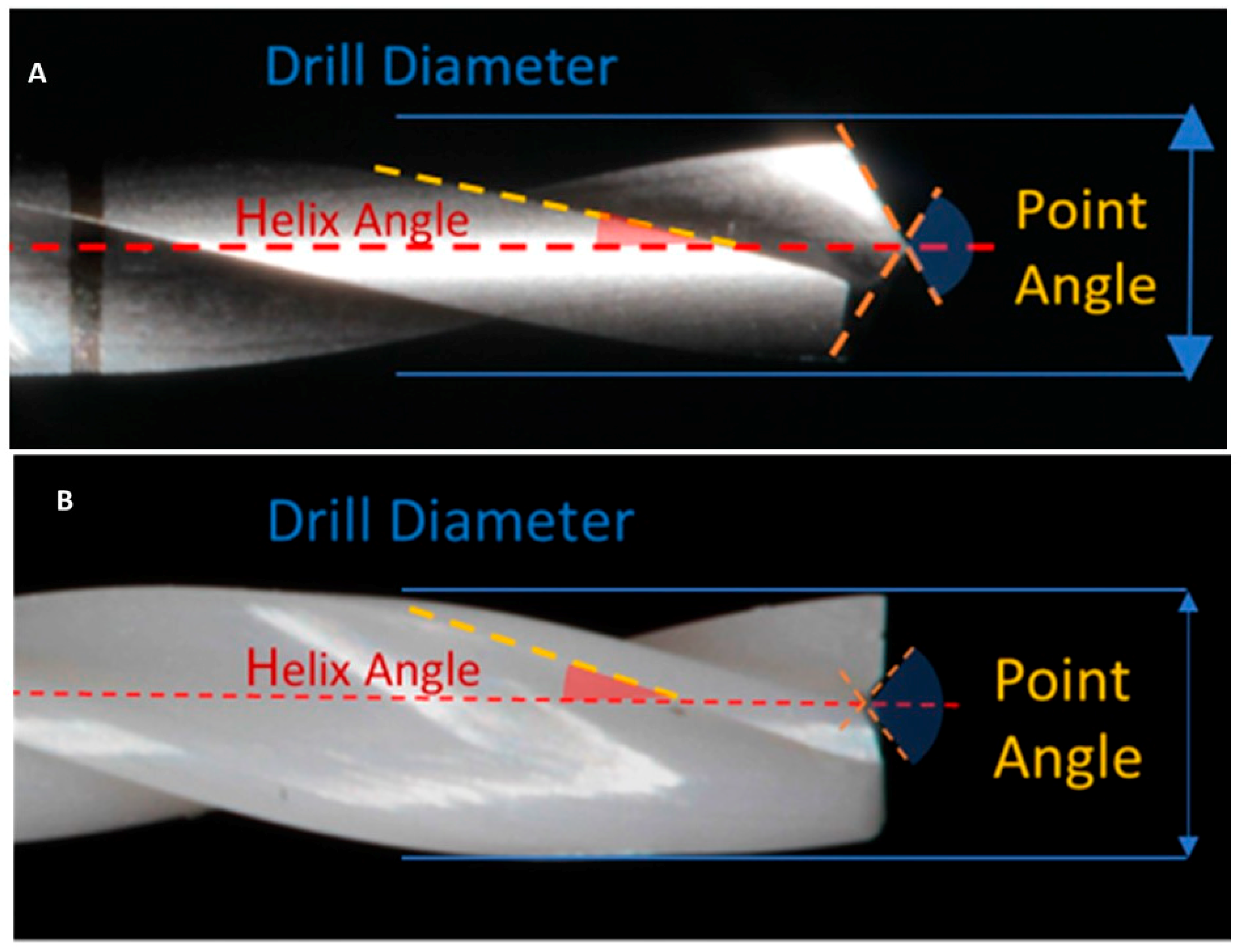
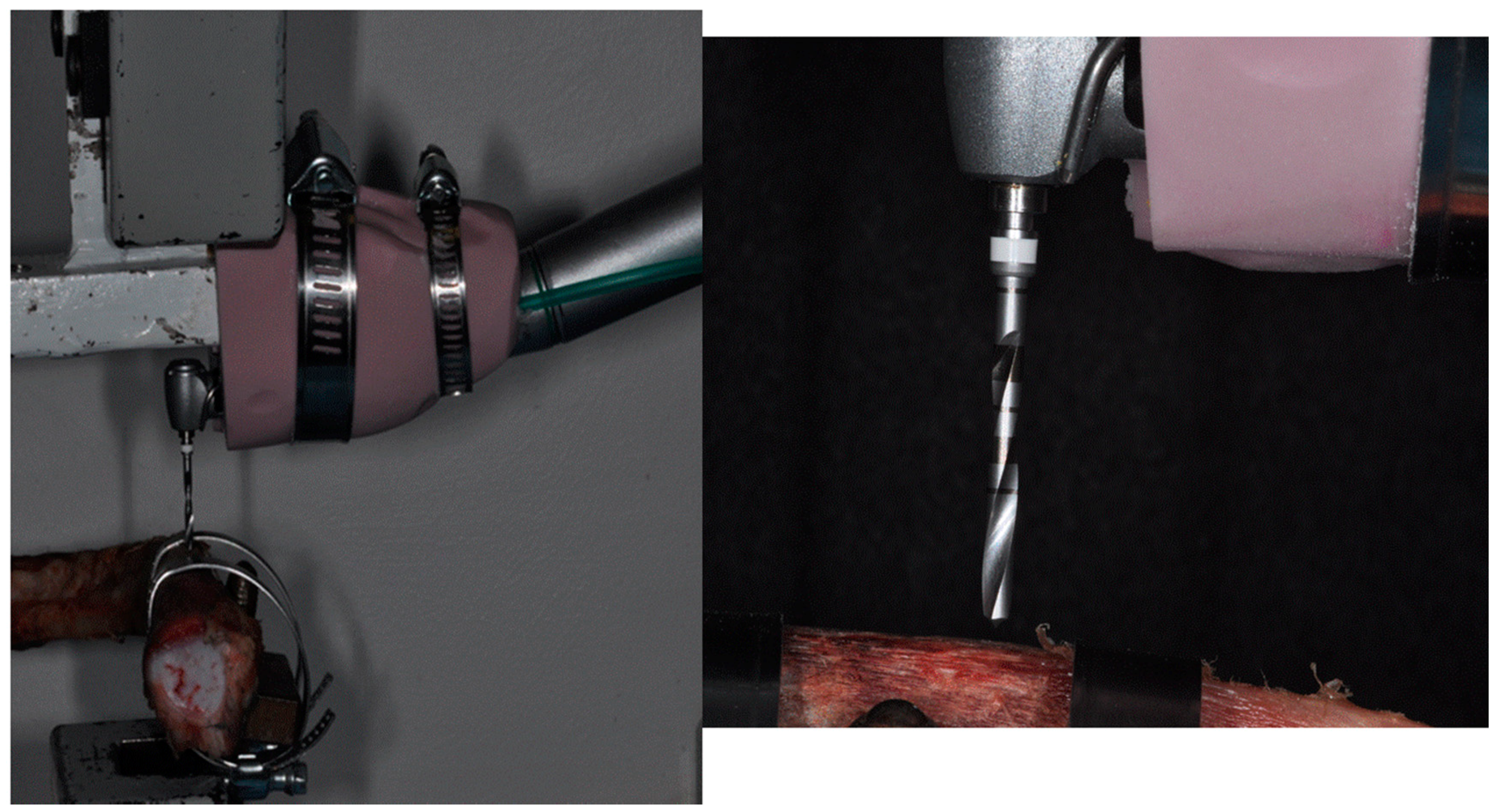
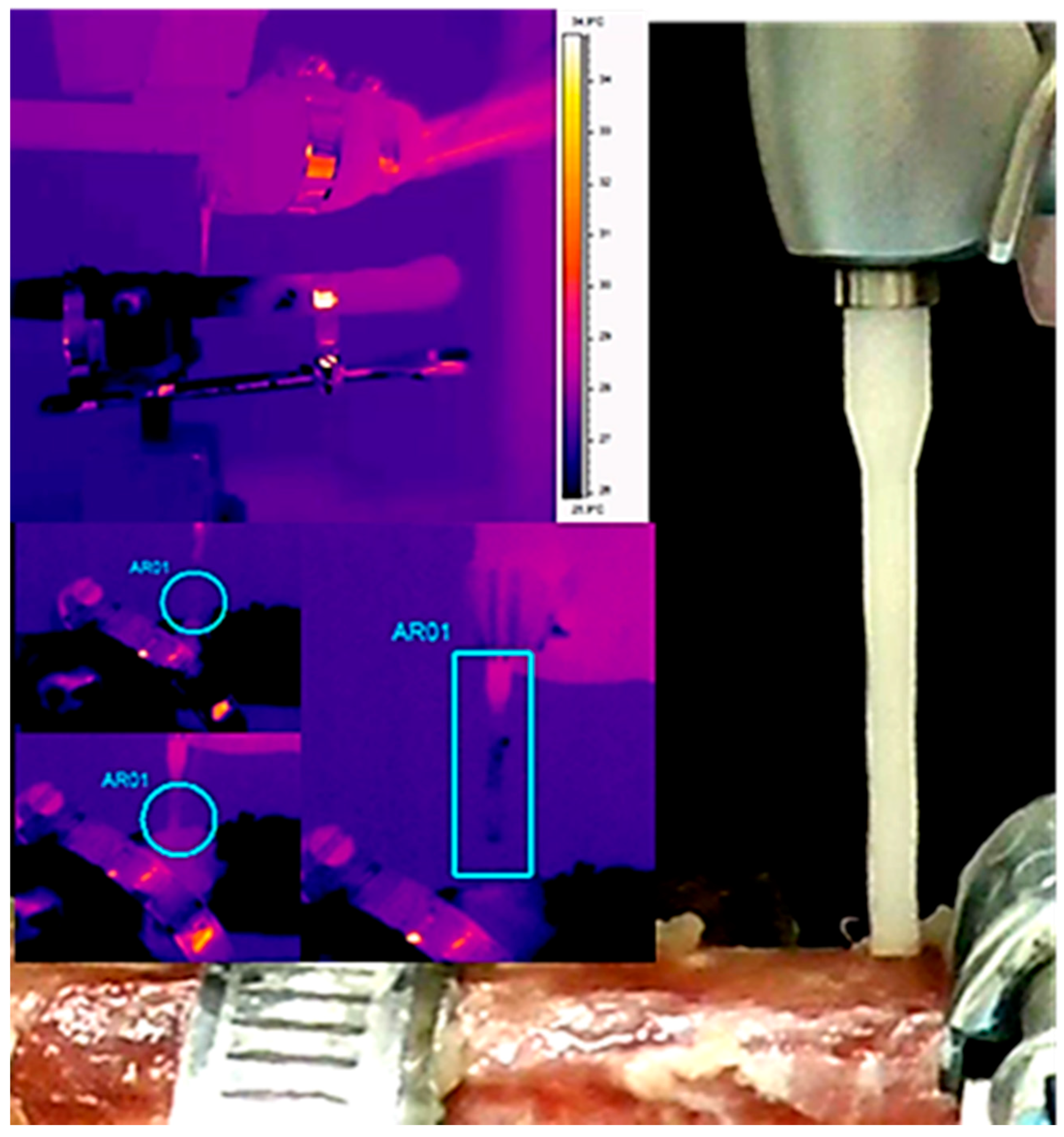
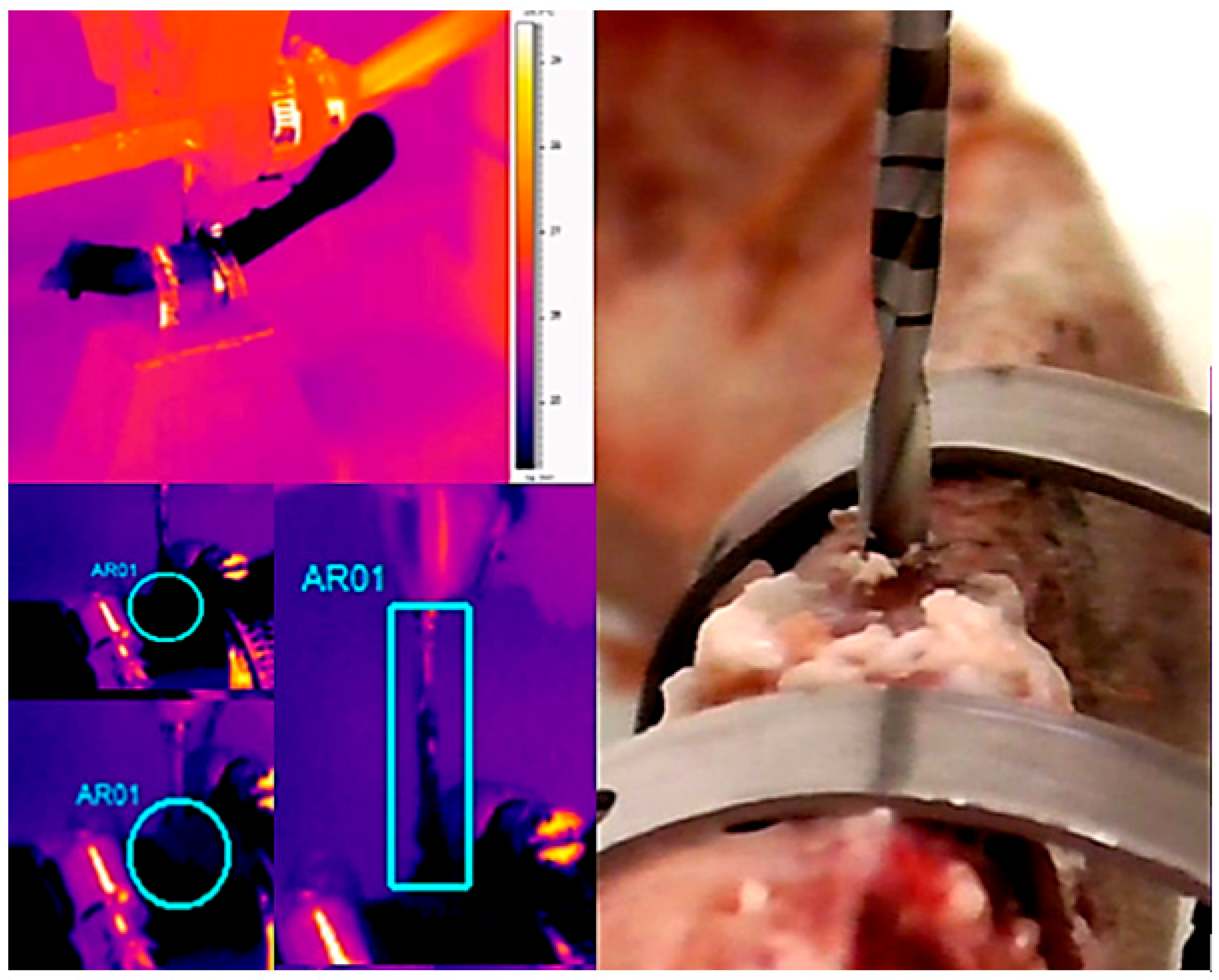
2. Materials and Methods
Statistical Evaluation
3. Results
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Eriksson, R.A.; Albrektsson, T.; Magnusson, B. Assessment of bone viability after heat trauma. A histological, histochemical and vital microscopic study in the rabbit. Scand. J. Plast. Reconstr. Surg. 1984, 18, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Janner, S.F.M.; Wittneben, J.-G.; Brägger, U.; Ramseier, C.A.; Salvi, G.E. 10-year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: A retrospective study in 303 partially edentulous patients. Clin. Implant Dent. Relat. Res. 2012, 14, 839–851. [Google Scholar] [CrossRef] [PubMed]
- Albrektsson, T.; Lekholm, U. Osseointegration: Current state of the art. Dent. Clin. N. Am. 1989, 33, 537–554. [Google Scholar] [PubMed]
- Hochscheidt, C.J.; Shimizu, R.H.; Andrighetto, A.R.; Moura, L.M.; Golin, A.L.; Hochscheidt, R.C. Thermal Variation During Osteotomy With Different Dental Implant Drills: A Standardized Study in Bovine Ribs. Implant Dent. 2017, 26, 73–79. [Google Scholar] [CrossRef]
- Lucchiari, N.; Frigo, A.C.; Stellini, E.; Coppe, M.; Berengo, M.; Bacci, C. In Vitro Assessment with the Infrared Thermometer of Temperature Differences Generated During Implant Site Preparation: The Traditional Technique Versus the Single-Drill Technique. Clin. Implant Dent. Relat. Res. 2016, 18, 182–191. [Google Scholar] [CrossRef] [PubMed]
- Marković, A.; Mišić, T.; Miličić, B.; Calvo-Guirado, J.L.; Aleksić, Z.; Ðinić, A. Heat generation during implant placement in low-density bone: Effect of surgical technique, insertion torque and implant macro design. Clin. Oral Implant. Res. 2013, 24, 798–805. [Google Scholar] [CrossRef]
- Scarano, A.; Lorusso, F.; Orsini, T.; Morra, M.; Iviglia, G.; Valbonetti, L. Biomimetic Surfaces Coated with Covalently Immobilized Collagen Type I: An X-ray Photoelectron Spectroscopy, Atomic Force Microscopy, Micro-CT and Histomorphometrical Study in Rabbits. Int. J. Mol. Sci. 2019, 20, 724. [Google Scholar] [CrossRef]
- Slaets, E.; Carmeliet, G.; Naert, I.; Duyck, J. Early trabecular bone healing around titanium implants: A histologic study in rabbits. J. Periodontol. 2007, 78, 510–517. [Google Scholar] [CrossRef]
- Yeniyol, S.; Jimbo, R.; Marin, C.; Tovar, N.; Janal, M.N.; Coelho, P.G. The effect of drilling speed on early bone healing to oral implants. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 116, 550–555. [Google Scholar] [CrossRef]
- Guazzi, P.; Grandi, T.; Grandi, G. Implant site preparation using a single bur versus multiple drilling steps: 4-month post-loading results of a multicenter randomised controlled trial. Eur. J. Oral Implantol. 2015, 8, 283–290. [Google Scholar]
- Bogovič, V.; Svete, A.; Bajsić, I. Effects of a drill diameter on the temperature rise in a bone during implant site preparation under clinical conditions. Proc. Inst. Mech. Eng. 2016, 230, 907–917. [Google Scholar] [CrossRef] [PubMed]
- Strbac, G.D.; Unger, E.; Donner, R.; Bijak, M.; Watzek, G.; Zechner, W. Thermal effects of a combined irrigation method during implant site drilling. A standardized in vitro study using a bovine rib model. Clin. Oral Implant. Res. 2014, 25, 665–674. [Google Scholar] [CrossRef] [PubMed]
- Stelzle, F.; Frenkel, C.; Riemann, M.; Knipfer, C.; Stockmann, P.; Nkenke, E. The effect of load on heat production, thermal effects and expenditure of time during implant site preparation—An experimental ex vivo comparison between piezosurgery and conventional drilling. Clin. Oral Implant. Res. 2014, 25, e140–e148. [Google Scholar] [CrossRef] [PubMed]
- Ercoli, C.; Funkenbusch, P.D.; Lee, H.-J.; Moss, M.E.; Graser, G.N. The influence of drill wear on cutting efficiency and heat production during osteotomy preparation for dental implants: A study of drill durability. Int. J. Oral Maxillofac. Implant. 2004, 19, 335–349. [Google Scholar]
- Berglundh, T.; Abrahamsson, I.; Lang, N.P.; Lindhe, J. De novo alveolar bone formation adjacent to endosseous implants. Clin. Oral Implant. Res. 2003, 14, 251–262. [Google Scholar] [CrossRef]
- Leunig, M.; Hertel, R. Thermal necrosis after tibial reaming for intramedullary nail fixation. A report of three cases. J. Bone Jt. Surg. Br. 1996, 78, 584–587. [Google Scholar] [CrossRef]
- Piattelli, A.; Piattelli, M.; Mangano, C.; Scarano, A. A histologic evaluation of eight cases of failed dental implants: Is bone overheating the most probable cause. Biomaterials 1998, 19, 683–690. [Google Scholar] [CrossRef]
- Albrektsson, T.; Eriksson, A. Thermally induced bone necrosis in rabbits: Relation to implant failure in humans. Clin. Orthop. Relat. Res. 1985, 195, 311–312. [Google Scholar] [CrossRef]
- Scarano, A.; Iezzi, G.; Perrotti, V.; Tetè, S.; Staiti, G.; Mortellaro, C.; Cappucci, C. Ultrasonic versus drills implant site preparation: A histologic analysis in bovine ribs. J. Craniofacial Surg. 2014, 25, 814–817. [Google Scholar] [CrossRef]
- Scarano, A.; Carinci, F.; Quaranta, A.; Di Iorio, D.; Assenza, B.; Piattelli, A. Effects of bur wear during implant site preparation: An in vitro study. Int. J. Immunopathol. Pharmacol. 2007, 20, 23–26. [Google Scholar] [CrossRef]
- Frösch, L.; Mukaddam, K.; Filippi, A.; Zitzmann, N.U.; Kühl, S. Comparison of heat generation between guided and conventional implant surgery for single and sequential drilling protocols—An in vitro study. Clin. Oral Implant. Res. 2019, 30, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Stacchi, C.; Vercellotti, T.; Torelli, L.; Furlan, F.; Di Lenarda, R. Changes in implant stability using different site preparation techniques: Twist drills versus piezosurgery. A single-blinded, randomized, controlled clinical trial. Clin. Implant Dent. Relat. Res. 2013, 15, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Carinci, F.; Lorusso, F.; Festa, F.; Bevilacqua, L.; Santos de Oliveira, P.; Maglione, M. Ultrasonic vs Drill Implant Site Preparation: Post-Operative Pain Measurement Through VAS, Swelling and Crestal Bone Remodeling: A Randomized Clinical Study. Materials 2018, 11, 2516. [Google Scholar] [CrossRef] [PubMed]
- Agabiti, I.; Botticelli, D. Two-Stage Ridge Split at Narrow Alveolar Mandibular Bone Ridges. J. Oral Maxillofac. Surg. 2017, 75, 2115. [Google Scholar] [CrossRef]
- Manicone, P.F.; Rossi Iommetti, P.; Raffaelli, L. An overview of zirconia ceramics: Basic properties and clinical applications. J. Dent. 2007, 35, 819–826. [Google Scholar] [CrossRef]
- Scarano, A.; Stoppaccioli, M.; Casolino, T. Zirconia crowns cemented on titanium bars using CAD/CAM: A five-year follow-up prospective clinical study of 9 patients. BMC Oral Health 2019, 19, 286. [Google Scholar] [CrossRef]
- Scarano, A.; Piattelli, A.; Assenza, B.; Carinci, F.; Di Donato, L.; Romani, G.L.; Merla, A. Infrared thermographic evaluation of temperature modifications induced during implant site preparation with cylindrical versus conical drills. Clin. Implant Dent. Relat. Res. 2011, 13, 319–323. [Google Scholar] [CrossRef]
- Brisman, D.L. The effect of speed, pressure, and time on bone temperature during the drilling of implant sites. Int. J. Oral Maxillofac. Implant. 1996, 11, 35–37. [Google Scholar]
- Jacob, C.H.; Berry, J.T. A study of the bone machining process—Drilling. J. Biomech. 1976, 9, 343–349. [Google Scholar] [CrossRef]
- Lughmani, W.A.; Bouazza-Marouf, K.; Ashcroft, I. Drilling in cortical bone: A finite element model and experimental investigations. J. Mech. Behav. Biomed. Mater. 2015, 42, 32–42. [Google Scholar] [CrossRef]
- Lee, J.; Gozen, B.A.; Ozdoganlar, O.B. Modeling and experimentation of bone drilling forces. J. Biomech. 2012, 45, 1076–1083. [Google Scholar] [CrossRef] [PubMed]
- Alam, K.; Muhammad, R.; Shamsuzzoha, A.; AlYahmadi, A.; Ahmed, N. Quantitative analysis of force and torque in bone drilling. J. Eng. Res. 2017, 14, 39–48. [Google Scholar] [CrossRef]
- Favero, V.; Sakuma, S.; Apaza Alccayhuaman, K.A.; Benedetto, G.A.; Bengazi, F.; Botticelli, D. Healing at sites prepared using different drilling protocols. An experimental study in the tibiae of sheep. PLoS ONE 2018, 13, e0202957. [Google Scholar] [CrossRef] [PubMed]
- Agren, E.; Arwill, T. High-speed or conventional dental equipment for the removal of bone in oral surgery. 3. A histologic and microradiographic study on bone repair in the rabbit. Acta Odontol. Scand. 1968, 26, 223–246. [Google Scholar] [CrossRef]
- Wiggins, K.L.; Malkin, S. Drilling of bone. J. Biomech. 1976, 9, 553–559. [Google Scholar] [CrossRef]
- Jacobs, C.H.; Pope, M.H.; Berry, J.T.; Hoaglund, F. A study of the bone machining process-orthogonal cutting. J. Biomech. 1974, 7, 131–136. [Google Scholar] [CrossRef]
- Chacon, G.E.; Bower, D.L.; Larsen, P.E.; McGlumphy, E.A.; Beck, F.M. Heat production by 3 implant drill systems after repeated drilling and sterilization. J. Oral Maxillofac. Surg. 2006, 64, 265–269. [Google Scholar] [CrossRef]
- Matthews, L.S.; Hirsch, C. Temperatures measured in human cortical bone when drilling. J Bone Jt. Surg. Am. 1972, 54, 297–308. [Google Scholar] [CrossRef]
- Benington, I.C.; Biagioni, P.A.; Briggs, J.; Sheridan, S.; Lamey, P.-J. Thermal changes observed at implant sites during internal and external irrigation. Clin. Oral Implant. Res. 2002, 13, 293–297. [Google Scholar] [CrossRef]
- Eriksson, R.A.; Adell, R. Temperatures during drilling for the placement of implants using the osseointegration technique. J. Oral Maxillofac. Surg. 1986, 44, 4–7. [Google Scholar] [CrossRef]
- Albrektsson, T.; Bra-nemark, P.-I.; Zarb, G.A. Tissue-integrated prostheses: Osseointegration in clinical dentistry. Plast. Reconstr. Surg. 1986, 77, 496–497. [Google Scholar]
- Akiba, Y.; Eguchi, K.; Akiba, N.; Uoshima, K. Biological Evaluation of Implant Drill Made from Zirconium Dioxide. Clin. Implant Dent. Relat. Res. 2017, 19, 306–315. [Google Scholar] [CrossRef]
- Oliveira, N.; Alaejos-Algarra, F.; Mareque-Bueno, J.; Ferrés-Padró, E.; Hernández-Alfaro, F. Thermal changes and drill wear in bovine bone during implant site preparation. A comparative in vitro study: Twisted stainless steel and ceramic drills. Clin. Oral Implant. Res. 2012, 23, 963–969. [Google Scholar] [CrossRef]
- Piattelli, A.; Scarano, A.; Piattelli, M. Histologic observations on 230 retrieved dental implants: 8 years’ experience (1989–1996). J. Periodontol. 1998, 69, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Baumgart, F.; Kohler, G.; Ochsner, P.E. The physics of heat generation during reaming of the medullary cavity. Injury 1998, 29, B11–B25. [Google Scholar] [CrossRef]
- Harder, S.; Egert, C.; Wenz, H.J.; Jochens, A.; Kern, M. Influence of the drill material and method of cooling on the development of intrabony temperature during preparation of the site of an implant. Br. J. Oral Maxillofac. Surg. 2013, 51, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Koo, K.-T.; Kim, M.-H.; Kim, H.-Y.; Wikesjö, U.M.E.; Yang, J.-H.; Yeo, I.-S. Effects of implant drill wear, irrigation, and drill materials on heat generation in osteotomy sites. J. Oral Implantol. 2015, 41, e19–e23. [Google Scholar] [CrossRef]
- Sumer, M.; Misir, A.F.; Telcioglu, N.T.; Guler, A.U.; Yenisey, M. Comparison of heat generation during implant drilling using stainless steel and ceramic drills. J. Oral Maxillofac. Surg. 2011, 69, 1350–1354. [Google Scholar] [CrossRef]
- Di Fiore, A.; Sivolella, S.; Stocco, E.; Favero, V.; Stellini, E. Experimental Analysis of Temperature Differences during Implant Site Preparation: Continuous Drilling Technique versus Intermittent Drilling Technique. J. Oral Implantol. 2018, 44, 46–50. [Google Scholar] [CrossRef]
- Garbey, M.; Sun, N.; Merla, A.; Pavlidis, I. Contact-free measurement of cardiac pulse based on the analysis of thermal imagery. IEEE Trans. Biomed. Eng. 2007, 54, 1418–1426. [Google Scholar] [CrossRef]
- Mariotti, A.; Di Carlo, L.; Orlando, G.; Corradini, M.L.; Di Donato, L.; Pompa, P.; Iezzi, R.; Cotroneo, A.R.; Romani, G.L.; Merla, A. Scrotal thermoregulatory model and assessment of the impairment of scrotal temperature control in varicocele. Ann. Biomed. Eng. 2011, 39, 664–673. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Lavery, L.A.; Liswood, P.J.; Todd, W.F.; Tredwell, J.A. Infrared dermal thermometry for the high-risk diabetic foot. Phys. Ther. 1997, 77, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Perpetuini, D.; Cardone, D.; Chiarelli, A.M.; Filippini, C.; Croce, P.; Zappasodi, F.; Rotunno, L.; Anzoletti, N.; Zito, M.; Merla, A. Autonomic impairment in Alzheimer’s disease is revealed by complexity analysis of functional thermal imaging signals during cognitive tasks. Physiol. Meas. 2019, 40. [Google Scholar] [CrossRef] [PubMed]
- Bahramian, F.; Mojra, A. Analysis of thyroid thermographic images for detection of thyroid tumor: An experimental-numerical study. Int. J. Numer. Methods Biomed. Eng. 2019, 35, e3192. [Google Scholar] [CrossRef] [PubMed]
- Augustin, G.; Davila, S.; Udiljak, T.; Vedrina, D.S.; Bagatin, D. Determination of spatial distribution of increase in bone temperature during drilling by infrared thermography: Preliminary report. Arch. Orthop. Trauma Surg. 2009, 129, 703–709. [Google Scholar] [CrossRef] [PubMed]
- Augustin, G.; Zigman, T.; Davila, S.; Udilljak, T.; Staroveski, T.; Brezak, D.; Babic, S. Cortical bone drilling and thermal osteonecrosis. Clin. Biomech. 2012, 27, 313–325. [Google Scholar] [CrossRef]
- Zelenov, E.S. Experimental investigation of the thermophysical properties of compact bone. Mech. Compos. Mater. 1986, 21, 759–762. [Google Scholar] [CrossRef]
- Field, J.R.; Sumner-Smith, G. Bone blood flow response to surgical trauma. Injury 2002, 33, 447–451. [Google Scholar] [CrossRef]

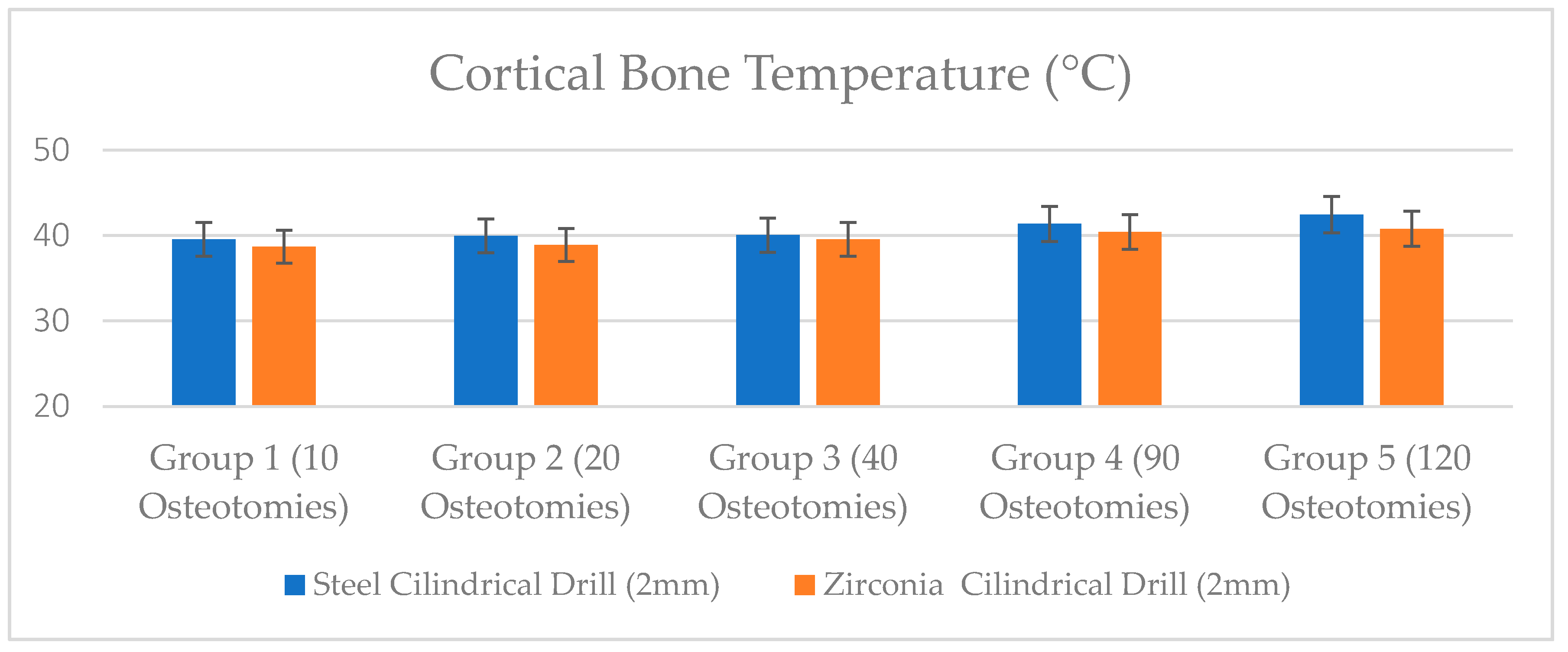
| Bone Temperature (°C) | Group 1 (10 Osteotomies) | Group 2 (20 Osteotomies) | Group 3 (40 Osteotomies) | Group 4 (90 Osteotomies) | Group 5 (120 Osteotomies) |
|---|---|---|---|---|---|
| Steel Cylindrical Drill (2 mm) | 39.55 ± 0.98 | 39.97 ± 0.92 | 40.06 ± 1.26 | 41.37 ± 1.81 | 42.45 ± 1.70 |
| Zirconia Cylindrical Drill (2 mm) | 38.70 ± 0.83 | 38.9 ± 1.36 | 39.55 ± 1.79 | 40.43 ± 1.82 | 40.80 ± 0.85 |
| p Value | p = 0.54 | p = 0.25 | p = 0.031 (*) | p = 0.0033 (**) | p = 0.0004 (**) |
| Apical Drill Temperature (°C) | Group 1 (10 Osteotomies) | Group 2 (20 Osteotomies) | Group 3 (40 Osteotomies) | Group 4 (90 Osteotomies) | Group 5 (120 Osteotomies) |
|---|---|---|---|---|---|
| Steel Cylindrical Drill (2 mm) | 40.51 ± 0.88 | 40.63 ± 0.97 | 41.66 ± 0.55 | 41.96 ± 1.51 | 42.15 ± 1.14 |
| Zirconia Cylindrical Drill (2 mm) | 39.68 ± 1.10 | 39.75 ± 0.89 | 40.14 ± 1.01 | 40.20 ± 0.85 | 40.62 ± 1.00 |
| p Value | p = 0.33 | p = 0.025 (*) | p = 0.028 (*) | p = 0.0003 (**) | p = 0.0001 (**) |
| Drilling Time (Sec) | Group 1 (10 Osteotomies) | Group 2 (20 Osteotomies) | Group 3 (40 Osteotomies) | Group 4 (90 Osteotomies) | Group 5 (120 Osteotomies) |
|---|---|---|---|---|---|
| Steel Cylindrical Drill (2 mm diameter) | 11.05 ± 0.91 | 11.08 ± 1.09 | 11.56 ± 0.56 | 12.15 ± 0.70 | 12.88 ± 1.34 |
| Zirconia Cylindrical Drill (2 mm diameter) | 9.62 ± 0.75 | 9.79 ± 0.52 | 10.02 ± 0.62 | 10.44 ± 0.62 | 10.53 ± 1.09 |
| p Value | p = 0.0067 (**) | p = 0.0003 (**) | p = 0.0001 (**) | p = 0.00003 (**) | p = 0.000001 (**) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scarano, A.; Lorusso, F.; Noumbissi, S. Infrared Thermographic Evaluation of Temperature Modifications Induced during Implant Site Preparation with Steel vs. Zirconia Implant Drill. J. Clin. Med. 2020, 9, 148. https://doi.org/10.3390/jcm9010148
Scarano A, Lorusso F, Noumbissi S. Infrared Thermographic Evaluation of Temperature Modifications Induced during Implant Site Preparation with Steel vs. Zirconia Implant Drill. Journal of Clinical Medicine. 2020; 9(1):148. https://doi.org/10.3390/jcm9010148
Chicago/Turabian StyleScarano, Antonio, Felice Lorusso, and Sammy Noumbissi. 2020. "Infrared Thermographic Evaluation of Temperature Modifications Induced during Implant Site Preparation with Steel vs. Zirconia Implant Drill" Journal of Clinical Medicine 9, no. 1: 148. https://doi.org/10.3390/jcm9010148
APA StyleScarano, A., Lorusso, F., & Noumbissi, S. (2020). Infrared Thermographic Evaluation of Temperature Modifications Induced during Implant Site Preparation with Steel vs. Zirconia Implant Drill. Journal of Clinical Medicine, 9(1), 148. https://doi.org/10.3390/jcm9010148







