Admission Hyperglycemia as a Predictor of Mortality in Acute Heart Failure: Comparison between the Diabetics and Non-Diabetics
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Echocardiographic Measurements
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Echocardiographic Findings
3.3. Prescribed Medications
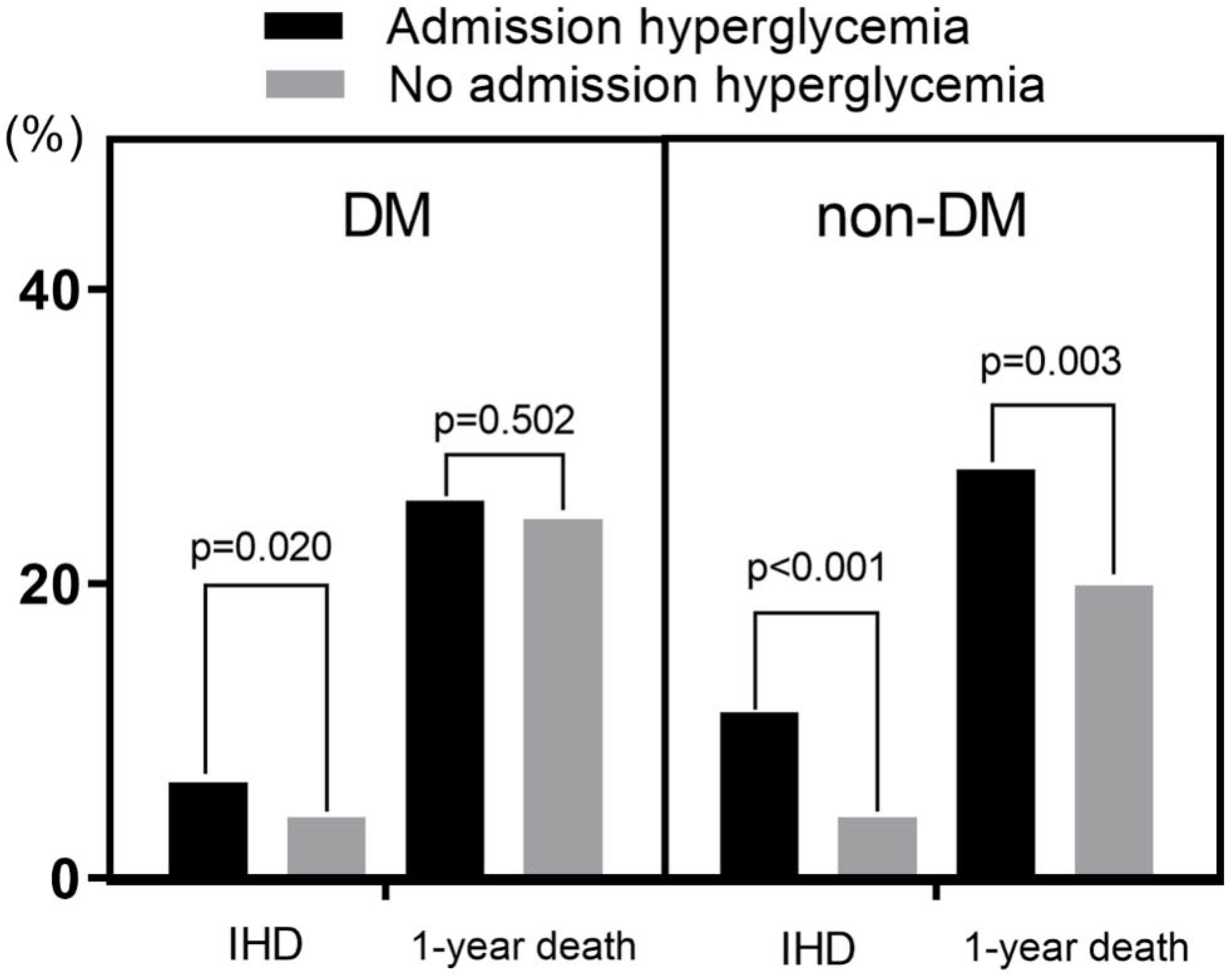
Impacts of DM and Admission HGL on IHD and 1-Year Death
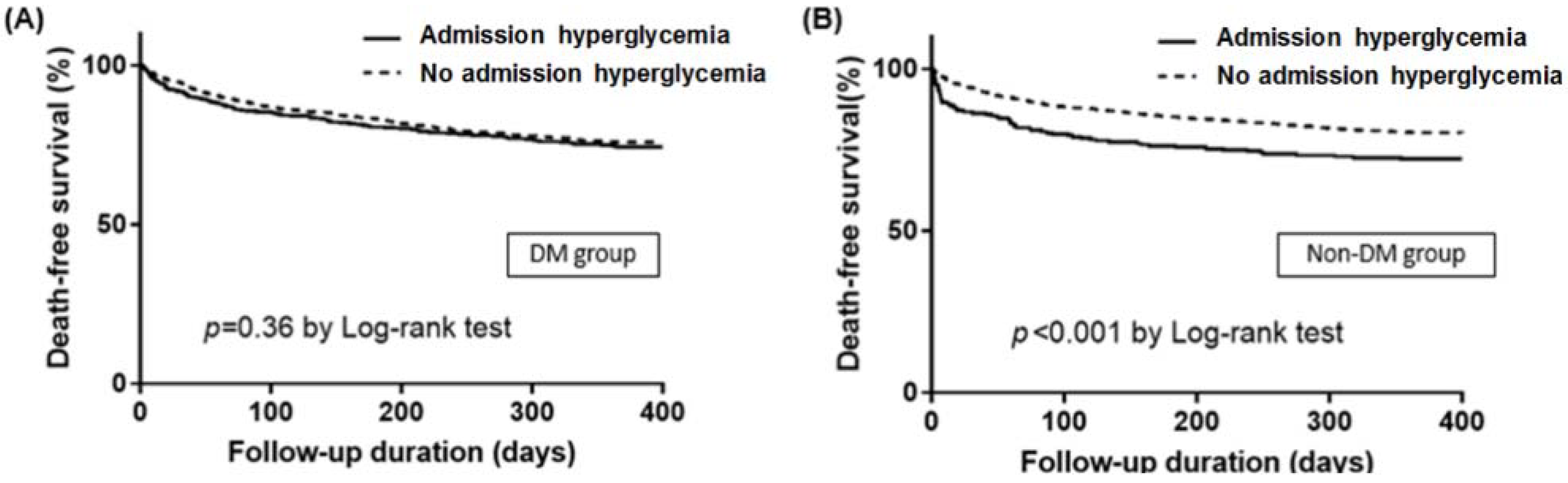
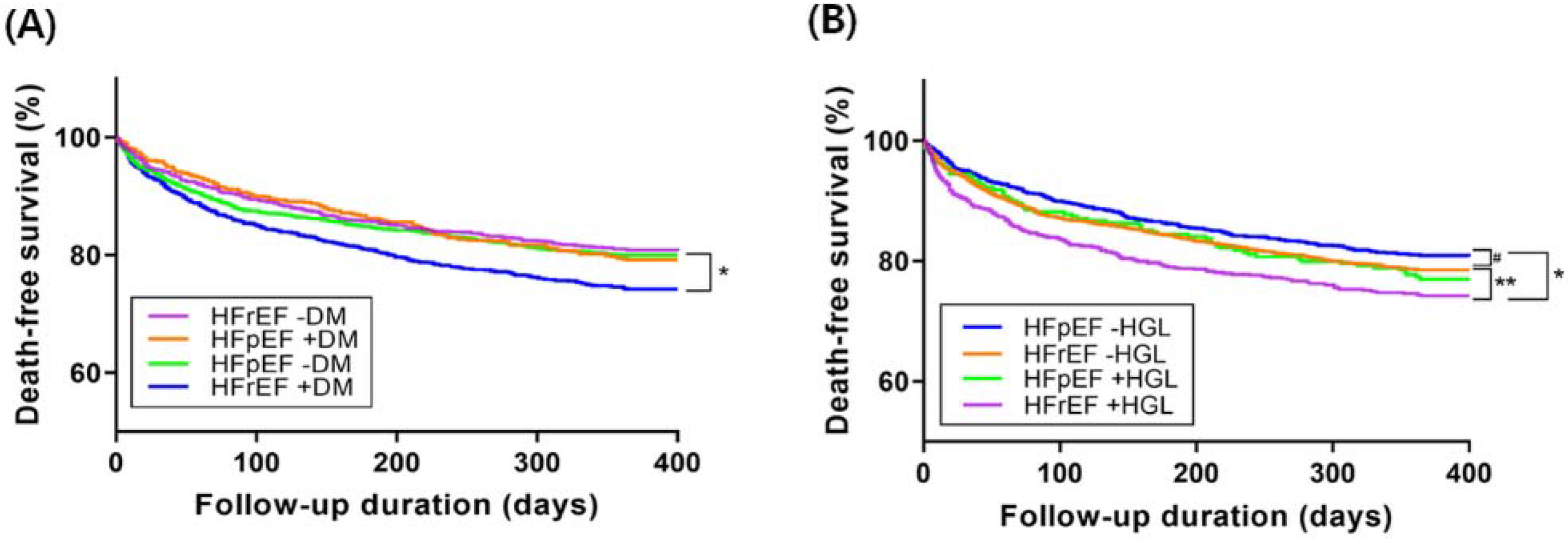
3.4. Impacts of DM and Admission HGL on 1-Year Mortality According to HF Subtypes
4. Discussion
4.1. Admission HGL or DM and IHD
4.2. Admission HGL or DM and 1-Year Death
4.3. HGL and Increased SNS Affecting HF Mortality
4.4. Impacts of DM and Admission HGL on 1-Year Mortality According to HF Subtypes
5. Study Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Hao, Y.; Lu, Q.; Li, T.; Yang, G.; Hu, P.; Ma, A. Admission hyperglycemia and adverse outcomes in diabetic and non-diabetic patients with non-ST-elevation myocardial infarction undergoing percutaneous coronary intervention. BMC Cardiovasc. Disord. 2017, 17, 6. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.F.; Burt, M.G.; Heilbronn, L.K.; Mangoni, A.A.; Wong, V.W.; McLean, M.; Cheung, N.W. Relative hyperglycemia is associated with complications following an acute myocardial infarction: A post-hoc analysis of HI-5 data. Cardiovasc. Diabetol. 2017, 16, 157. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.J.; Jeong, M.H.; Kim, J.H.; Ahn, T.H.; Seung, K.B.; Oh, D.J.; Kim, H.S.; Gwon, H.C.; Seong, I.W.; Hwang, K.K.; et al. Clinical impact of admission hyperglycemia on in-hospital mortality in acute myocardial infarction patients. Int. J. Cardiol. 2017, 236, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Ishihara, M.; Kagawa, E.; Inoue, I.; Kawagoe, T.; Shimatani, Y.; Kurisu, S.; Nakama, Y.; Maruhashi, T.; Ookawa, K.; Dai, K.; et al. Impact of admission hyperglycemia and diabetes mellitus on short- and long-term mortality after acute myocardial infarction in the coronary intervention era. Am. J. Cardiol. 2007, 99, 1674–1679. [Google Scholar] [CrossRef]
- Mann, D.L.; Zipes, D.P.; Libby, P.; Bonow, R.O.; Braunwald, E. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine; Elsevier/Saunders: Philadelphia, PA, USA, 2015. [Google Scholar]
- Porte, D., Jr.; Robertson, R.P. Control of insulin secretion by catecholamines, stress, and the sympathetic nervous system. Fed. Proc. 1973, 32, 1792–1796. [Google Scholar]
- Kattel, S.; Kasai, T.; Matsumoto, H.; Yatsu, S.; Murata, A.; Kato, T.; Suda, S.; Hiki, M.; Takagi, A.; Daida, H. Association between elevated blood glucose level on admission and long-term mortality in patients with acute decompensated heart failure. J. Cardiol. 2017, 69, 619–624. [Google Scholar] [CrossRef]
- Helfand, B.K.; Maselli, N.J.; Lessard, D.M.; Yarzebski, J.; Gore, J.M.; McManus, D.D.; Saczynski, J.S.; Goldberg, R.J. Elevated serum glucose levels and survival after acute heart failure: A population-based perspective. Diab. Vasc. Dis. Res. 2015, 12, 119–125. [Google Scholar] [CrossRef]
- Kosiborod, M.; Inzucchi, S.E.; Spertus, J.A.; Wang, Y.; Masoudi, F.A.; Havranek, E.P.; Krumholz, H.M. Elevated admission glucose and mortality in elderly patients hospitalized with heart failure. Circulation 2009, 119, 1899–1907. [Google Scholar] [CrossRef]
- Nieminen, M.S.; Bohm, M.; Cowie, M.R.; Drexler, H.; Filippatos, G.S.; Jondeau, G.; Hasin, Y.; Lopez-Sendon, J.; Mebazaa, A.; Metra, M.; et al. Executive summary of the guidelines on the diagnosis and treatment of acute heart failure: The Task Force on Acute Heart Failure of the European Society of Cardiology. Eur. Heart J. 2005, 26, 384–416. [Google Scholar]
- Lee, S.E.; Cho, H.J.; Lee, H.Y.; Yang, H.M.; Choi, J.O.; Jeon, E.S.; Kim, M.S.; Kim, J.J.; Hwang, K.K.; Chae, S.C.; et al. A multicentre cohort study of acute heart failure syndromes in Korea: Rationale, design, and interim observations of the Korean Acute Heart Failure (KorAHF) registry. Eur. J. Heart Fail. 2014, 16, 700–708. [Google Scholar] [CrossRef]
- Lee, S.E.; Lee, H.Y.; Cho, H.J.; Choe, W.S.; Kim, H.; Choi, J.O.; Jeon, E.S.; Kim, M.S.; Kim, J.J.; Hwang, K.K.; et al. Clinical characteristics and outcome of acute heart failure in Korea: Results from the Korean Acute Heart Failure Registry (KorAHF). Korean Circ. J. 2017, 47, 341–353. [Google Scholar] [CrossRef] [PubMed]
- Chouihed, T.; Buessler, A.; Bassand, A.; Jaeger, D.; Virion, J.M.; Nace, L.; Barbe, F.; Salignac, S.; Rossignol, P.; Zannad, F.; et al. Hyponatraemia, hyperglycaemia and worsening renal function at first blood sample on emergency department admission as predictors of in-hospital death in patients with dyspnoea with suspected acute heart failure: Retrospective observational analysis of the PARADISE cohort. BMJ Open 2018, 8, e019557. [Google Scholar] [PubMed]
- Kataja, A.; Tarvasmaki, T.; Lassus, J.; Cardoso, J.; Mebazaa, A.; Kober, L.; Sionis, A.; Spinar, J.; Carubelli, V.; Banaszewski, M.; et al. The association of admission blood glucose level with the clinical picture and prognosis in cardiogenic shock—Results from the CardShock Study. Int. J. Cardiol. 2017, 226, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Mebazaa, A.; Gayat, E.; Lassus, J.; Meas, T.; Mueller, C.; Maggioni, A.; Peacock, F.; Spinar, J.; Harjola, V.P.; Van Kimmenade, R.; et al. Association between elevated blood glucose and outcome in acute heart failure: Results from an international observational cohort. J. Am. Coll. Cardiol. 2013, 61, 820–829. [Google Scholar] [CrossRef]
- Sud, M.; Wang, X.; Austin, P.C.; Lipscombe, L.L.; Newton, G.E.; Tu, J.V.; Vasan, R.S.; Lee, D.S. Presentation blood glucose and death, hospitalization, and future diabetes risk in patients with acute heart failure syndromes. Eur. Heart J. 2015, 36, 924–931. [Google Scholar] [CrossRef]
- Targher, G.; Dauriz, M.; Laroche, C.; Temporelli, P.L.; Hassanein, M.; Seferovic, P.M.; Drozdz, J.; Ferrari, R.; Anker, S.; Coats, A.; et al. In-hospital and 1-year mortality associated with diabetes in patients with acute heart failure: Results from the ESC-HFA Heart Failure Long-Term Registry. Eur. J. Heart Fail. 2017, 19, 54–65. [Google Scholar] [CrossRef]
- Parissis, J.T.; Rafouli-Stergiou, P.; Mebazaa, A.; Ikonomidis, I.; Bistola, V.; Nikolaou, M.; Meas, T.; Delgado, J.; Vilas-Boas, F.; Paraskevaidis, I.; et al. Acute heart failure in patients with diabetes mellitus: Clinical characteristics and predictors of in-hospital mortality. Int. J. Cardiol. 2012, 157, 108–113. [Google Scholar] [CrossRef]
- Jia, Q.; Wang, Y.R.; He, P.; Huang, X.L.; Yan, W.; Mu, Y.; He, K.L.; Tian, Y.P. Prediction model of in-hospital mortality in elderly patients with acute heart failure based on retrospective study. J. Geriatr. Cardiol. 2017, 14, 669–678. [Google Scholar]
- Aljohar, A.; Alhabib, K.F.; Kashour, T.; Hersi, A.; Al Habeeb, W.; Ullah, A.; Elasfar, A.; Almasood, A.; Ghabashi, A.; Mimish, L.; et al. The prognostic impact of hyperglycemia on clinical outcomes of acute heart failure: Insights from the heart function assessment registry trial in Saudi Arabia. J. Saudi Heart Assoc. 2018, 30, 319–327. [Google Scholar] [CrossRef]
- Targher, G.; Dauriz, M.; Tavazzi, L.; Temporelli, P.L.; Lucci, D.; Urso, R.; Lecchi, G.; Bellanti, G.; Merlo, M.; Rossi, A.; et al. Prognostic impact of in-hospital hyperglycemia in hospitalized patients with acute heart failure: Results of the IN-HF (Italian Network on Heart Failure) Outcome registry. Int. J. Cardiol. 2016, 203, 587–593. [Google Scholar] [CrossRef]
- Barsheshet, A.; Garty, M.; Grossman, E.; Sandach, A.; Lewis, B.S.; Gottlieb, S.; Shotan, A.; Behar, S.; Caspi, A.; Schwartz, R.; et al. Admission blood glucose level and mortality among hospitalized nondiabetic patients with heart failure. Arch. Intern. Med. 2006, 166, 1613–1619. [Google Scholar] [CrossRef] [PubMed]
- Lazzeri, C.; Valente, S.; Attana, P.; Chiostri, M.; Picariello, C.; Gensini, G.F. Acute hyperglycemia and insulin resistance in acute heart failure syndromes without previously known diabetes. Intern. Emerg. Med. 2012, 7, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, R.; Norrelund, H.; Kampmann, U.; Botker, H.E.; Moller, N.; Wiggers, H. Effect of acute hyperglycemia on left ventricular contractile function in diabetic patients with and without heart failure: Two randomized cross-over studies. PLoS ONE 2013, 8, e53247. [Google Scholar] [CrossRef] [PubMed]
- Devedjian, J.C.; Pujol, A.; Cayla, C.; George, M.; Casellas, A.; Paris, H.; Bosch, F. Transgenic mice overexpressing alpha2A-adrenoceptors in pancreatic beta-cells show altered regulation of glucose homeostasis. Diabetologia 2000, 43, 899–906. [Google Scholar] [CrossRef][Green Version]
- Trico, D.; Baldi, S.; Frascerra, S.; Venturi, E.; Marraccini, P.; Neglia, D.; Natali, A. Abnormal glucose tolerance is associated with a reduced myocardial metabolic flexibility in patients with dilated cardiomyopathy. J. Diabetes Res. 2016, 2016, 3906425. [Google Scholar] [CrossRef][Green Version]
- Nikolaidis, L.A.; Sturzu, A.; Stolarski, C.; Elahi, D.; Shen, Y.T.; Shannon, R.P. The development of myocardial insulin resistance in conscious dogs with advanced dilated cardiomyopathy. Cardiovasc. Res. 2004, 61, 297–306. [Google Scholar] [CrossRef]
- MacDonald, M.R.; Petrie, M.C.; Varyani, F.; Ostergren, J.; Michelson, E.L.; Young, J.B.; Solomon, S.D.; Granger, C.B.; Swedberg, K.; Yusuf, S.; et al. Impact of diabetes on outcomes in patients with low and preserved ejection fraction heart failure: An analysis of the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) programme. Eur. Heart J. 2008, 29, 1377–1385. [Google Scholar] [CrossRef]
- De Boer, R.A.; Doehner, W.; Van Der Horst, I.C.; Anker, S.D.; Babalis, D.; Roughton, M.; Coats, A.J.; Flather, M.D.; Van Veldhuisen, D.J.; Investigators, S. Influence of diabetes mellitus and hyperglycemia on prognosis in patients > or =70 years old with heart failure and effects of nebivolol (data from the Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors with heart failure [SENIORS]). Am. J. Cardiol. 2010, 106, 78–86. [Google Scholar]

| Variables | DM (n = 2125) | No DM (n = 3416) | ||||
|---|---|---|---|---|---|---|
| Admission HGL (n = 799) | No Admission HGL (n = 1326) | p | Admission HGL (n = 248) | No Admission HGL (n = 3168) | p | |
| Age (years) | 70.8 ± 11.3 | 70.2 ± 11.5 | 0.223 | 72.9 ± 12.9 | 67.0 ± 16.1 | <0.001 |
| Male sex (%) | 400 (50.1) | 757 (57.1) | 0.002 | 115 (46.4) | 1670 (52.7) | 0.054 |
| Body mass index (kg/m2) | 23.6 ± 3.6 | 24.0 ± 4.0 | 0.017 | 22.5 ± 3.3 | 23.0 ± 3.9 | 0.014 |
| Systolic blood pressure (mmHg) | 138.1 ± 33.0 | 132.1 ± 29.3 | <0.001 | 139.0 ± 36.6 | 128.5 ± 29.1 | <0.001 |
| Diastolic blood pressure (mmHg) | 79.9 ± 19.7 | 78.1 ± 17.6 | 0.035 | 82.3 ± 20.3 | 78.2 ± 18.8 | 0.003 |
| Heart rate (bpm) | 98.2 ± 26.9 | 90.4 ± 23.9 | <0.001 | 102.3 ± 28.8 | 91.5 ± 26.0 | <0.001 |
| Hypertension | 586 (73.3) | 985 (74.3) | 0.632 | 145 (58.5) | 1564 (49.4) | 0.006 |
| Heart failure history | 326 (40.8) | 660 (49.8) | <0.001 | 84 (33.9) | 1338 (42.2) | 0.010 |
| Dyslipidemia | 645 (52.9) | 443 (59.8) | 0.003 | 97 (44.7) | 984 (34.7) | 0.003 |
| Smoking history | 304 (38.0) | 550 (41.5) | 0.118 | 99 (39.9) | 1187 (37.5) | 0.443 |
| Alcohol history | 278 (34.8) | 502 (37.9) | 0.156 | 78 (31.5) | 1264 (39.9) | 0.009 |
| Valvular heart disease | 72 (9.0) | 165 (12.4) | 0.015 | 21 (8.5) | 542 (17.1) | <0.001 |
| Cerebrovascular disease | 139 (17.4) | 253 (19.1) | 0.333 | 34 (13.7) | 414 (13.1) | 0.775 |
| Ischemic heart disease | 304 (38.0) | 535 (40.3) | 0.294 | 68 (27.4) | 654 (20.7) | 0.012 |
| Chronic kidney disease | 169 (21.2) | 302 (22.8) | 0.383 | 19 (7.7) | 304 (9.6) | 0.316 |
| Atrial fibrillation | 145 (18.1) | 392 (29.6) | <0.001 | 54 (21.8) | 941 (29.7) | 0.008 |
| Serum glucose (mg/dL) | 291.1 ± 87.3 | 137.1 ± 36.0 | <0.001 | 259.1 ± 61.2 | 120.8 ± 27.8 | <0.001 |
| Hb A1c (%) | 8.0 ± 1.6 | 6.9 ± 1.0 | <0.001 | 5.8 ± 0.3 | 5.8 ± 0.4 | 0.764 |
| Serum creatinine (mg/dL) | 1.8 ± 1.6 | 1.7 ± 1.6 | 0.373 | 1.5 ± 1.4 | 1.3 ± 1.4 | 0.132 |
| Glomerular filtration rate (ml/min) | 61.0 ± 36.1 | 66.0 ± 39.9 | 0.004 | 67.1 ± 33.7 | 79.6 ± 40.0 | <0.001 |
| High-sensitivity C-reactive protein* | 1.02 (0.26–3.71) | 0.67 (0.23–2.24) | <0.001 | 0.88 (0.24–2.41) | 0.58 (0.18–2.00) | 0.684 |
| Brain natriuretic peptide* | 993.8 (617.3–1845.5) | 893.3 (470.0–1685.8) | 0.213 | 1004.4 (521.5–2120.0) | 884.3 (447.1–1732.1) | 0.188 |
| N-terminal Pro-B type natriuretic peptide* | 6198.3 (2441.5–15,835.3) | 5365.0 (2344.0–13,443.0) | 0.186 | 5983.0 (2361.0–13,833.0) | 4497.0 (2031.0–10,416.0) | 0.166 |
| Troponin-I* | 0.13 (0.05–1.20) | 0.06 (0.03–0.21) | 0.189 | 0.11 (0.05–0.76) | 0.05 (0.03–0.19) | 0.301 |
| Variables | DM (n = 2125) | No DM (n = 3416) | ||||
|---|---|---|---|---|---|---|
| Admission HGL (n = 799) | No Admission HGL (n = 1326) | p | Admission HGL (n = 248) | No Admission HGL (n = 3168) | p | |
| LVEDD (mm) | 56.2 ± 8.9 | 57.9 ± 9.2 | <0.001 | 55.9 ± 9.7 | 57.5 ± 10.7 | 0.018 |
| LVESD (mm) | 44.1 ± 11.0 | 45.8 ± 11.6 | 0.001 | 43.5 ± 11.3 | 45.1 ± 13.0 | 0.047 |
| LVEF (%) | 36.8 ± 14.5 | 36.8 ± 15.1 | 0.996 | 37.0 ± 14.5 | 38.7 ± 16.1 | 0.081 |
| LA dimension (mm) | 45.7 ± 8.3 | 48.7 ± 9.0 | <0.001 | 45.8 ± 10.6 | 48.7 ± 10.3 | <0.001 |
| E (m/s) | 0.93 ± 0.35 | 0.96 ± 0.36 | 0.156 | 0.82 ± 0.33 | 0.95 ± 0.41 | <0.001 |
| DT (msec) | 162.4 ± 59.5 | 167.5 ± 70.7 | 0.157 | 171.3 ± 69.7 | 172.1 ± 89.9 | 0.900 |
| E’ (cm/s) | 4.8 ± 3.4 | 4.7 ± 1.9 | 0.746 | 4.7 ± 1.9 | 5.2 ± 2.2 | 0.003 |
| S’ (cm/s) | 4.8 ± 1.8 | 5.1 ± 1.9 | 0.020 | 5.2 ± 2.0 | 5.1 ± 2.1 | 0.835 |
| E/E’ | 22.3 ± 11.0 | 22.8 ± 12.6 | 0.401 | 19.1 ± 8.5 | 20.5 ± 11.3 | 0.039 |
| SPAP (mmHg) | 44.2 ± 14.6 | 45.2 ± 15.5 | 0.237 | 41.2 ± 14.3 | 43.5 ± 15.0 | 0.056 |
| Variables | DM (n = 2125) | Non-DM (n = 3416) | ||||
|---|---|---|---|---|---|---|
| Odd Ratio | 95% CI | p | Odd Ratio | 95% CI | p | |
| Age > 75 years | 1.72 | 1.07–2.79 | 0.026 | 0.92 | 0.65–1.30 | 0.625 |
| Male sex | 1.08 | 0.67–1.75 | 0.739 | 1.43 | 1.02–2.01 | 0.036 |
| History of hypertension | 0.98 | 0.59–1.62 | 0.927 | 0.94 | 0.67–1.33 | 0.740 |
| Systolic blood pressure < 100 mmHg | 3.59 | 2.17–5.93 | <0.001 | 2.88 | 2.06–4.05 | <0.001 |
| Renal insufficiency (initial GFR < 60 mL/min) | 1.70 | 1.05–2.76 | 0.030 | 2.14 | 1.53–2.99 | <0.001 |
| Admission hyperglycemia | 1.84 | 1.11–3.05 | 0.017 | 2.26 | 1.47–3.48 | <0.001 |
| Hb A1c | 0.83 | 0.68–1.02 | 0.080 | |||
| Ischemic etiology | 1.88 | 1.16–3.04 | 0.010 | 1.91 | 1.37–2.68 | 0.74 |
| Variables | Hazard Ratio | 95% CI | p |
|---|---|---|---|
| Age > 75 years | 1.94 | 1.65–2.29 | <0.001 |
| Male sex | 1.41 | 1.21–1.64 | <0.001 |
| Systolic blood pressure < 100 mmHg | 1.84 | 1.54–2.20 | <0.001 |
| Renal insufficiency (initial GFR < 60 mL/min) | 1.82 | 1.55–2.13 | <0.001 |
| Admission HGL | 1.32 | 1.03–1.69 | 0.030 |
| No RAS inhibitors | 2.13 | 1.78–2.55 | <0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, J.Y.; Kim, K.H.; Lee, S.E.; Cho, H.-J.; Lee, H.-Y.; Choi, J.-O.; Jeon, E.-S.; Kim, M.-S.; Kim, J.-J.; Hwang, K.-K.; et al. Admission Hyperglycemia as a Predictor of Mortality in Acute Heart Failure: Comparison between the Diabetics and Non-Diabetics. J. Clin. Med. 2020, 9, 149. https://doi.org/10.3390/jcm9010149
Cho JY, Kim KH, Lee SE, Cho H-J, Lee H-Y, Choi J-O, Jeon E-S, Kim M-S, Kim J-J, Hwang K-K, et al. Admission Hyperglycemia as a Predictor of Mortality in Acute Heart Failure: Comparison between the Diabetics and Non-Diabetics. Journal of Clinical Medicine. 2020; 9(1):149. https://doi.org/10.3390/jcm9010149
Chicago/Turabian StyleCho, Jae Yeong, Kye Hun Kim, Sang Eun Lee, Hyun-Jai Cho, Hae-Young Lee, Jin-Oh Choi, Eun-Seok Jeon, Min-Seok Kim, Jae-Joong Kim, Kyung-Kuk Hwang, and et al. 2020. "Admission Hyperglycemia as a Predictor of Mortality in Acute Heart Failure: Comparison between the Diabetics and Non-Diabetics" Journal of Clinical Medicine 9, no. 1: 149. https://doi.org/10.3390/jcm9010149
APA StyleCho, J. Y., Kim, K. H., Lee, S. E., Cho, H.-J., Lee, H.-Y., Choi, J.-O., Jeon, E.-S., Kim, M.-S., Kim, J.-J., Hwang, K.-K., Chae, S. C., Baek, S. H., Kang, S.-M., Choi, D.-J., Yoo, B.-S., Ahn, Y., Park, H.-Y., Cho, M.-C., & Oh, B.-H. (2020). Admission Hyperglycemia as a Predictor of Mortality in Acute Heart Failure: Comparison between the Diabetics and Non-Diabetics. Journal of Clinical Medicine, 9(1), 149. https://doi.org/10.3390/jcm9010149






