Uncharted Waters: Treating Trauma Symptoms in the Context of Early Psychosis
Abstract
1. Introduction
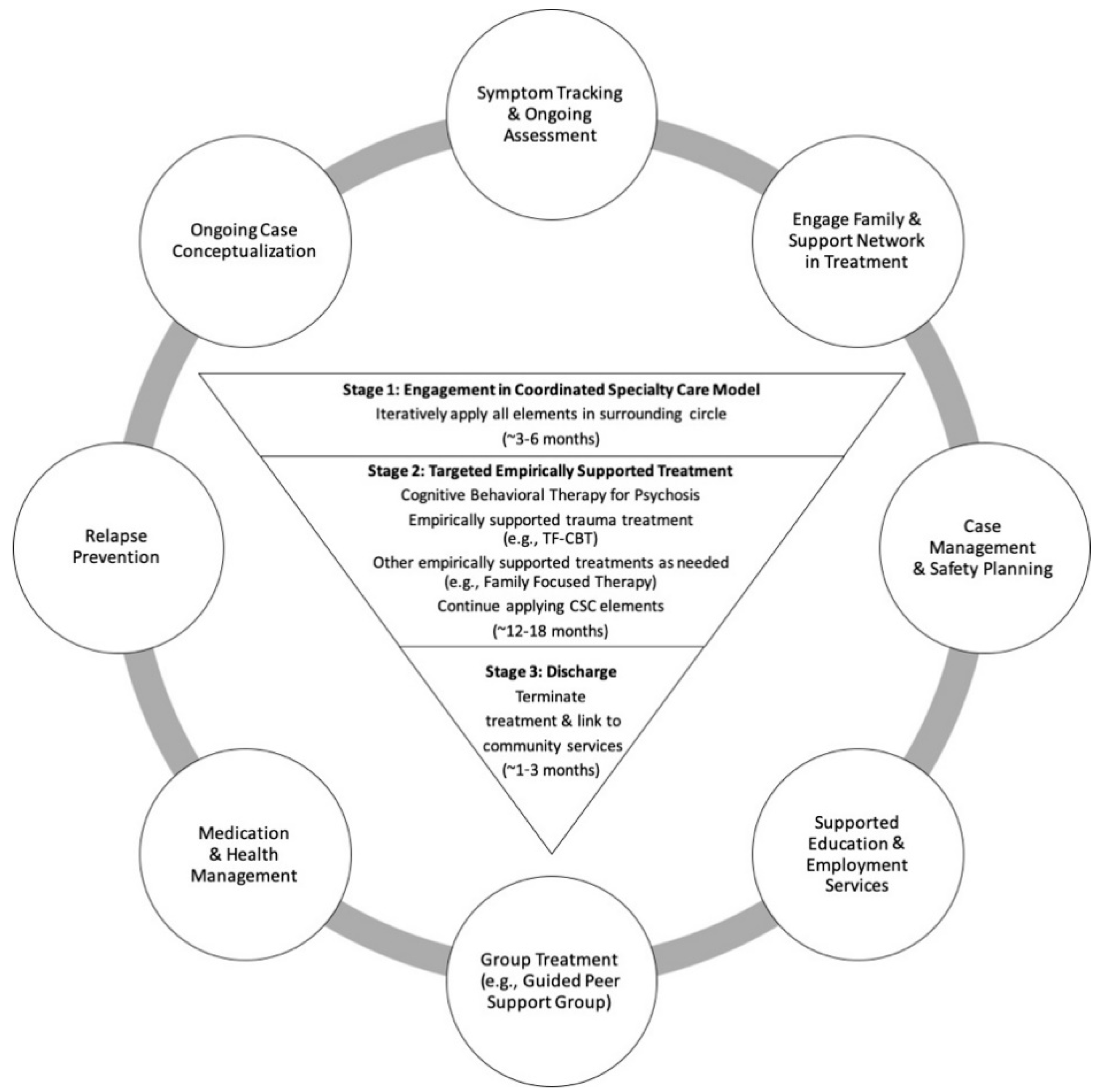
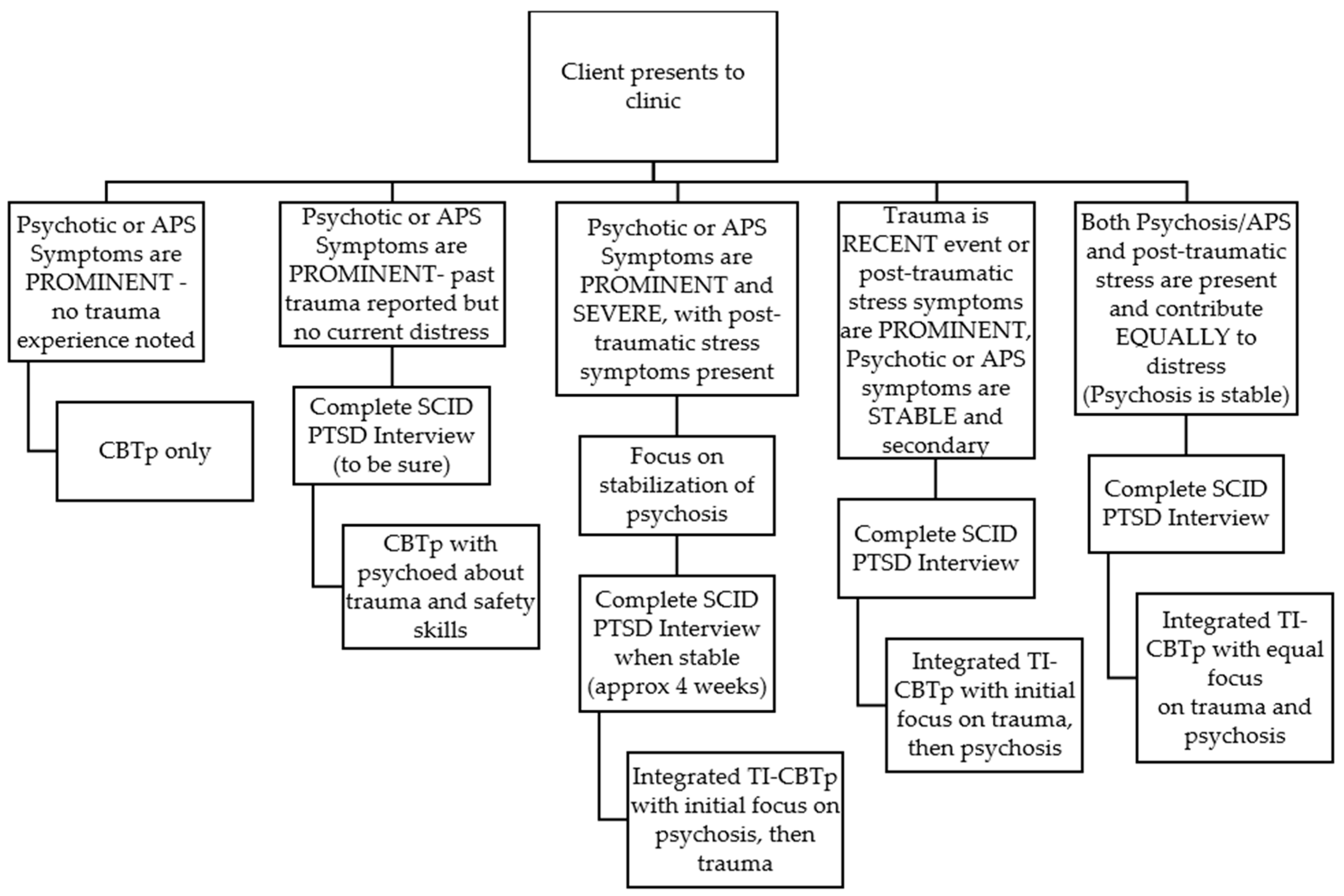
2. The Current Approach: TI-CBTp
3. Experimental Section
3.1. Participants and Study Design
3.2. Analysis
4. Results
4.1. Sample Characteristics
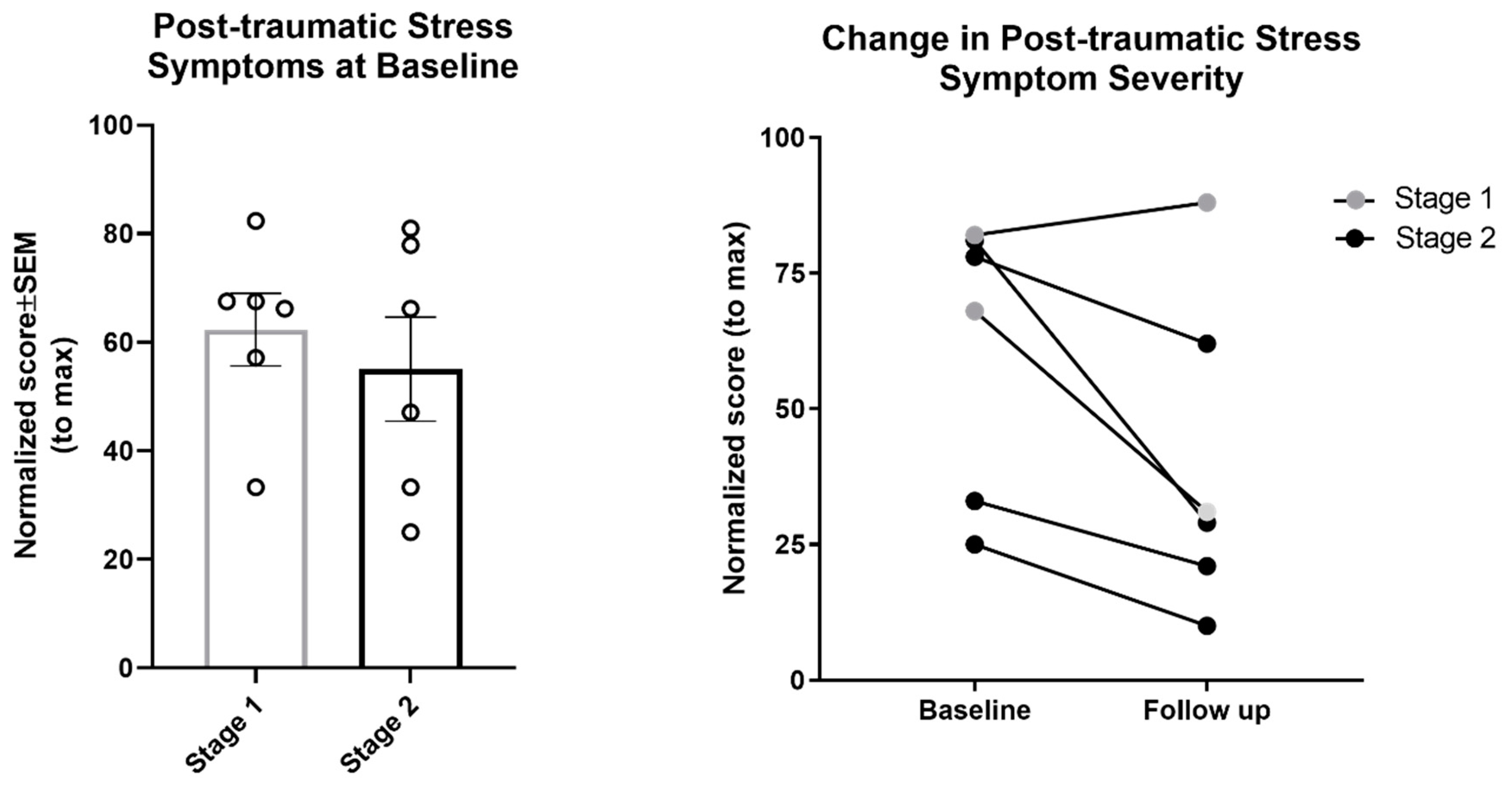
4.2. Outcomes
5. Discussion
5.1. Limitations and Future Directions
5.2. Challenges of Treating Trauma in Early Psychosis
5.1.1. Cognitive Symptoms
5.1.2. Negative Symptoms
5.1.3. Recurrent Crises
5.1.4. Reality of Incident
5.1.5. Clinician Skepticism
5.1.6. Secondary Traumatic Stress
5.1.7. Training Recommendations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Murray, R.M.; Bhavsar, V.; Tripoli, G.; Howes, O. 30 Years on: How the Neurodevelopmental Hypothesis of Schizophrenia Morphed into the Developmental Risk Factor Model of Psychosis. Schizophr. Bull. 2017, 43, 1190–1196. [Google Scholar] [CrossRef] [PubMed]
- Holtzman, C.W.; Trotman, H.D.; Goulding, S.M.; Ryan, A.T.; MacDonald, A.N.; Shapiro, D.I.; Brasfield, J.L.; Walker, E.F. Stress and Neurodevelopmental Processes in the Emergence of Psychosis. Neuroscience 2013, 249, 172–191. [Google Scholar] [CrossRef]
- Mayo, D.; Corey, S.; Kelly, L.H.; Yohannes, S.; Youngquist, A.L.; Stuart, B.K.; Niendam, T.A.; Loewy, R.L. The Role of Trauma and Stressful Life Events among Individuals at Clinical High Risk for Psychosis: A Review. Front. Psychiatry 2017, 8, 1–17. [Google Scholar] [CrossRef]
- Read, J.; Van Os, J.; Morrison, A.P.; Ross, C.A. Childhood Trauma, Psychosis and Schizophrenia: A Literature Review with Theoretical and Clinical Implications. Acta Psychiatr. Scand. 2005, 112, 330–350. [Google Scholar] [CrossRef] [PubMed]
- Heins, M.; Simons, C.; Lataster, T.; Pfeifer, S.; Versmissen, D.; Lardinois, M.; Marcelis, M.; Delespaul, P.; Krabbendam, L.; Van Os, J.; et al. Childhood Trauma and Psychosis: A Case-Control and Case-Sibling Comparison across Different Levels of Genetic Liability, Psychopathology, and Type of Trauma. Am. J. Psychiatry 2011, 168, 1286–1294. [Google Scholar] [CrossRef]
- Schenkel, L.S.; Spaulding, W.D.; Dilillo, D.; Silverstein, S.M. Histories of Childhood Maltreatment in Schizophrenia: Relationships with Premorbid Functioning, Symptomatology, and Cognitive Deficits. Schizophr. Res. 2005, 76, 273–286. [Google Scholar] [CrossRef] [PubMed]
- Kilcommons, A.; Morrison, A. Relationships Between Trauma and Psychosis: An Exploration of Cognitive and Dissociative Factors. Acta Psychiatr. Scand. 2005, 112, 351–359. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, M.H.; Yildirim, E.A.; Kaser, M.; Guduk, M.; Fistikci, N.; Cinar, O. The Relationship Between Adulthood Traumatic Experiences and Psychotic Symptoms in Female Patients with Schizophrenia. Compr. Psychiatry 2014, 55, 1847–1854. [Google Scholar] [CrossRef] [PubMed]
- Grubaugh, A.L.; Zinzow, H.M.; Paul, L.; Egede, L.E.; Frueh, B.C. Trauma Exposure and Posttraumatic Stress Disorder in Adults with Severe Mental Illness: A Critical Review. Clin. Psychol. Rev. 2012, 31, 883–899. [Google Scholar] [CrossRef]
- Neria, Y.; Bromet, E.J.; Sievers, S.; Lavelle, J.; Fochtmann, L.J. Trauma Exposure and Posttraumatic Stress Disorder in Psychosis: Findings from a First-Admission Cohort. J. Consult. Clin. Psychol. 2002, 70, 246–251. [Google Scholar] [CrossRef]
- Cragin, C.A.; Straus, M.B.; Blacker, D.; Tully, L.M.; Niendam, T.A. Early Psychosis and Trauma-Related Disorders: Clinical Practice Guidelines and Future Directions. Front. Psychiatry 2017, 8, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Miller, T.J.; McGlashan, T.H.; Rosen, J.L.; Cadenhead, K.; Ventura, J.; McFarlane, W.; Perkins, D.O.; Pearlson, G.D.; Woods, S.W. Prodromal Assessment with the Structured Interview for Prodromal Syndromes and the Scale of Prodromal Symptoms: Predictive Validity, Interrater Reliability, and Training to Reliability. Schizophr. Bull. 2003, 29, 703–715. [Google Scholar] [CrossRef] [PubMed]
- Heinssen, R.K.; Goldstein, A.B.; Azrin, S.T. Evidence-Based Treatments for First Episode Psychosis: Components of Coordinated Specialty Care; National Institute of Mental Health: Bethesda, MD, USA, 2014. [Google Scholar]
- Mueser, K.T.; Deavers, F.; Penn, D.L.; Cassisi, J.E. Psychosocial Treatments for Schizophrenia. Annu. Rev. Clinincal Psychochology 2013, 9, 465–497. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.A.; Mannarino, A.P.; Deblinger, E. Treating Trauma and Traumatic Grief in Children and Adolescents; Guilford Press: New York, NY, USA, 2017. [Google Scholar]
- Foa, E.B.; Hembree, E.A.; Rothbaum, B. Prolonged Exposure Therapy for PTSD; Oxford University: New York, NY, USA, 2007. [Google Scholar]
- Resick, P.A.; Schnicke, M. Cognitive Processing Therapy for Rape Victims: A Treatment Manual; Sage Publications: Newbury Park, CA, USA, 1993. [Google Scholar]
- Haro, J.M.; Kamath, S.A.; Ochoa, S.; Novick, D.; Rele, K.; Fargas, A.; Rodriguez, M.J.; Rele, R.; Orta, J.; Kharbeng, A.; et al. The Clinical Global Impression-Schizophrenia Scale: A Simple Instrument to Measure the Diversity of Symptoms Present in Schizophrenia. Acta Psychiatr. Scand. 2003, 107, 16–23. [Google Scholar] [CrossRef]
- Hutton, P.; Taylor, P.J. Cognitive Behavioural Therapy for Psychosis Prevention: A Systematic Review and Meta-Analysis. Psychol. Med. 2014, 44, 449–468. [Google Scholar] [CrossRef] [PubMed]
- Morrison, A.P.; French, P.; Walford, L.; Lewis, S.W.; Kilcommons, A.; Green, J.; Parker, S.; Bentall, R.P. Cognitive Therapy for the Prevention of Psychosis in People at Ultra-High Risk: Randomised Controlled Trial. Br. J. Psychiatry 2004, 185, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Van der Gaag, M.; Valmaggia, L.R.; Smit, F. The Effects of Individually Tailored Formulation-Based Cognitive Behavioural Therapy in Auditory Hallucinations and Delusions: A Meta-Analysis. Schizophr. Res. 2014, 156, 30–37. [Google Scholar] [CrossRef]
- First, M.B.; Williams, J.B.W.; Karg, R.S.; Spitzer, R.L. Structured Clinical Interview for DSM-5—Research Version; American Psychiatric Association: Arlington, VA, USA, 2015. [Google Scholar]
- First, M.B.; Spitzer, T.L.; Gibbon, M.; Williams, J. Structured Clinical Interview for DSM-IV Axis I Disorders; Biometrics Research Department: New York, NY, USA, 1997. [Google Scholar]
- Spearing, M.K.; Post, R.M.; Leverich, G.S.; Brandt, D.; Nolen, W. Modification of the Clinical Global Impressions (CGI) Scale for use in bipolar illness (BP): The CGI-BP. Psychiatry Res. 1997, 73, 159–171. [Google Scholar] [CrossRef]
- Cornblatt, B.A.; Auther, A.A.; Niendam, T.; Smith, C.W.; Zinberg, J.; Bearden, C.E.; Cannon, T.D. Preliminary Findings for Two New Measures of Social and Role Functioning in the Prodromal Phase of Schizophrenia. Schizophr. Bull. 2007, 33, 688–702. [Google Scholar] [CrossRef]
- Hall, R.C. Global Assessment of Functioning: A Modified scale. Psychosomatics 1995, 36, 267–275. [Google Scholar] [CrossRef]
- Kay, S.R.; Fiszbein, A.; Opler, L.A. The Positive and Negative Syndrome Scale (PANSS) for Schizophrenia. Schizophr. Bull. 1987, 13, 261–276. [Google Scholar] [CrossRef] [PubMed]
- Posner, K.; Brown, G.K.; Stanley, B.; Brent, D.A.; Yershova, K.V.; Oquendo, M.A.; Currier, G.W.; Glenn Melvin, M.A.; Greenhill, L.; Shen, S.; et al. The Columbia–Suicide Severity Rating Scale: Initial Validity and Internal Consistency Findings from Three Multisite Studies with Adolescents and Adults. Am. J. Psychiatry 2011, 168, 1266–1277. [Google Scholar] [CrossRef] [PubMed]
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD Checklist for Dsm-5 (Pcl-5). Scale Available from the National Center for PTSD. Available online: www.ptsd.va.gov (accessed on 1 July 2019).
- Steinberg, A.M.; Brymer, M.J.; Kim, S.; Briggs, E.C.; Ippen, C.G.; Ostrowski, S.A.; Gully, K.J.; Pynoos, R.S. Psychometric Properties of the UCLA PTSD Reaction Index: Part I. J. Trauma Stress 2013, 26, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sachser, C.; Berliner, L.; Holt, T.; Jensen, T.K.; Jungbluth, N.; Risch, E.; Rosner, R.; Goldbeck, L. International Development and Psychometric Properties of the Child and Adolescent Trauma Screen (CATS). J. Affect. Disord. 2017, 210, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Heinrichs, R.W.; Zakzanis, K.K. Neurocognitive Deficit in Schizophrenia: A Quantitative Review of the Evidence. Neuropsychology 1998, 12, 426–445. [Google Scholar] [CrossRef] [PubMed]
- McGurk, S.R.; Twamley, E.W.; Sitzer, D.I.; McHugo, G.J.; Mueser, K.T. A Meta-Analysis of Cognitive Remediation in Schizophrenia. Am. J. Psychiatry 2007, 164, 1791–1802. [Google Scholar] [CrossRef] [PubMed]
- De Bont, P.A.J.M.; Van Minnen, A.; De Jongh, A. Treating Ptsd in Patients with Psychosis: A within-Group Controlled Feasibility Study Examining the Efficacy and Safety of Evidence-Based Pe and EMDR Protocols. Behav. Ther. 2013, 44, 717–730. [Google Scholar] [CrossRef] [PubMed]
- Frueh, C.B.; Grubaugh, A.L.; Cusack, K.J.; Kimble, M.O.; Elhai, J.D.; Knapp, R.G. Exposure-Based Cognitive-Behavioral Treatment of PTSD in Adults with Schizophrenia or Schizoaffective Disorder: A Pilot Study. J. Anxiety Disord. 2009, 23, 665–675. [Google Scholar] [CrossRef]
- Van Den Berg, D.P.G.; Van Der Gaag, M. Treating Trauma in Psychosis with EMDR: A Pilot Study. J. Behav. Ther. Exp. Psychiatry 2012, 43, 664–671. [Google Scholar] [CrossRef] [PubMed]
- The National Child Traumatic Stress Network. Available online: https://www.nctsn.org (accessed on 15 July 2019).

| Stage 1 N = 12 | Stage 2 N = 10 | ||
|---|---|---|---|
| Age at assessment M (SD) | Years | 19.1 (5.4) | 16.8 (4.9) |
| Sex N (%) | Female | 7 (58%) | 7 (70%) |
| Male | 5 (42%) | 3 (30%) | |
| Race N (%) | Black | 6(50%) | 4 (40%) |
| White | 2 (17%) | 2 (20%) | |
| Other Asian | 0 (0%) | 1 (10%) | |
| Other Pacific Islander | 1 (8%) | 0 (0%) | |
| Other Race | 3 (25%) | 3 (30%) | |
| Ethnicity N (%) | Other Hispanic/Latino | 4 (33%) | 3 (30%) |
| Not Hispanic | 8 (67%) | 7 (70%) | |
| Primary Language N (%) | English | 12 (100%) | 10 (100%) |
| Diagnosis N (%) | Mood with Psychotic Features | 5 (42%) | 3 (30%) |
| Schizophrenia Spectrum Disorders | 7 (58%) | 3 (30%) | |
| Other Specified/Not Otherwise Specified Schizophrenia Spectrum | 0 (0%) | 4 (40%) | |
| PTSD Diagnosis N (%) | PTSD Dx | 7 (58%) | 6 (60%) |
| Post-traumatic Stress Symptom Severity M (SD) | Normalized Score | 62.3 (16.4) | 55.1 (23.5) |
| Psychosis Diagnosis N (%) | Recent Onset | 12 (100%) | 7 (70%) |
| Clinical High Risk | 0 (0%) | 3 (30%) | |
| Substance Use N (%) | Lifetime | 6 (50%) | 3 (30%) |
| Current | 5 (42%) | 2 (20%) | |
| Suicidal Ideation M (SD) | Lifetime | 3.3 (2.0) | 2.2 (2.4) |
| Current | 1.0 (1.3) | 0.4 (1.0) | |
| Suicidal Behavior N (%) | Lifetime | 5 (42%) | 4 (40%) |
| Current | 0 (0%) | 1 (10%) | |
| Non-Suicidal Self-Injury N (%) | Lifetime | 5 (42%) | 4 (40%) |
| Current | 1 (8%) | 2 (20%) | |
| Insight M (SD) | Current | 3.0 (1.1) | 2.0 (1.3) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
B. Folk, J.; Tully, L.M.; Blacker, D.M.; Liles, B.D.; Bolden, K.A.; Tryon, V.; Botello, R.; Niendam, T.A. Uncharted Waters: Treating Trauma Symptoms in the Context of Early Psychosis. J. Clin. Med. 2019, 8, 1456. https://doi.org/10.3390/jcm8091456
B. Folk J, Tully LM, Blacker DM, Liles BD, Bolden KA, Tryon V, Botello R, Niendam TA. Uncharted Waters: Treating Trauma Symptoms in the Context of Early Psychosis. Journal of Clinical Medicine. 2019; 8(9):1456. https://doi.org/10.3390/jcm8091456
Chicago/Turabian StyleB. Folk, Johanna, Laura M. Tully, Dawn M. Blacker, Brandi D. Liles, Khalima A. Bolden, Valerie Tryon, Renata Botello, and Tara A. Niendam. 2019. "Uncharted Waters: Treating Trauma Symptoms in the Context of Early Psychosis" Journal of Clinical Medicine 8, no. 9: 1456. https://doi.org/10.3390/jcm8091456
APA StyleB. Folk, J., Tully, L. M., Blacker, D. M., Liles, B. D., Bolden, K. A., Tryon, V., Botello, R., & Niendam, T. A. (2019). Uncharted Waters: Treating Trauma Symptoms in the Context of Early Psychosis. Journal of Clinical Medicine, 8(9), 1456. https://doi.org/10.3390/jcm8091456





