Early Corticosteroid Therapy for Mycoplasma pneumoniae Pneumonia Irrespective of Used Antibiotics in Children
Abstract
1. Introduction
2. Patients and Methods
2.1. Patient Selection
2.2. Corticosteroid and Antibiotic Treatment
2.3. Ethics
2.4. Statistical Analysis
3. Results
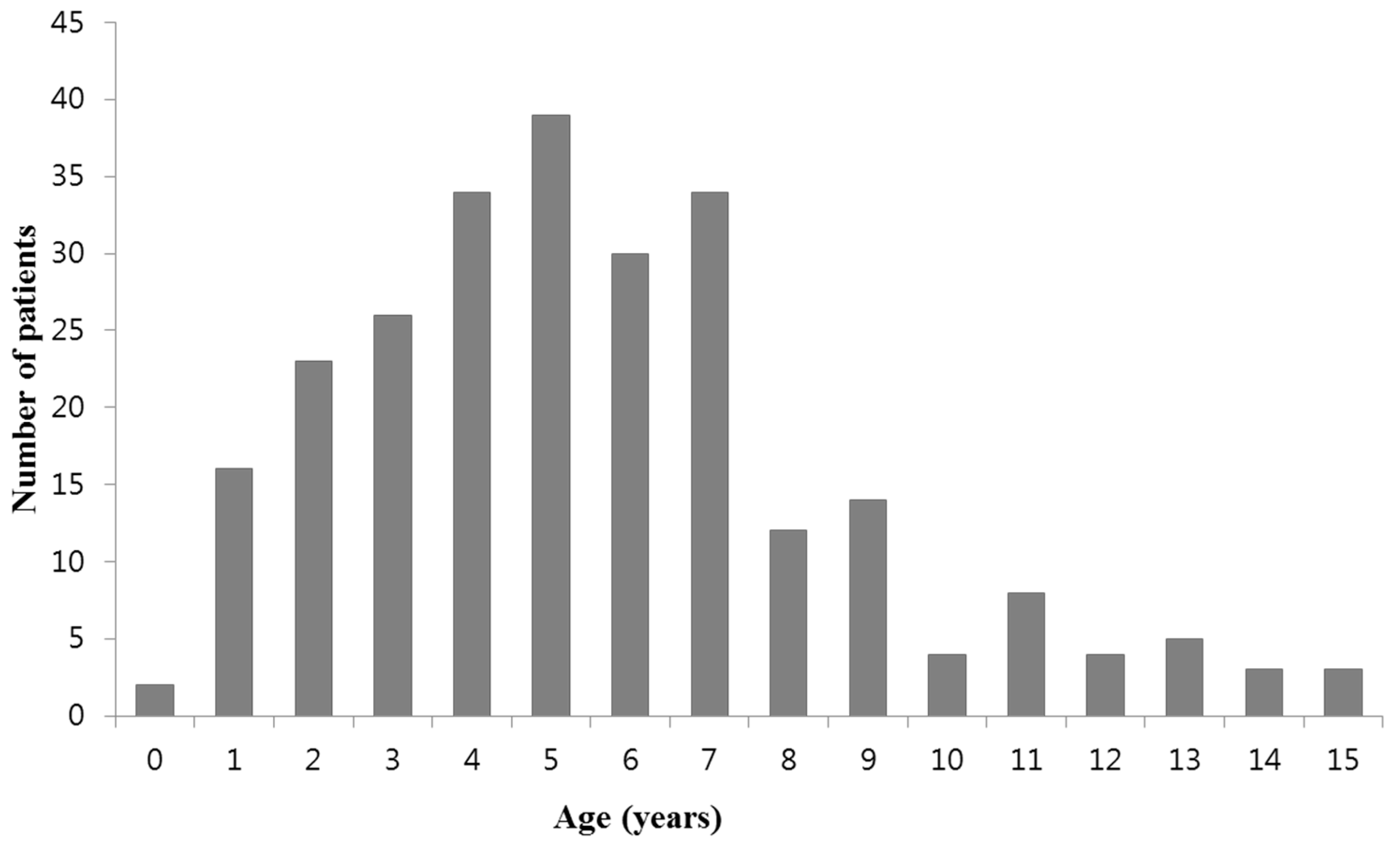
3.1. Demographic, Clinical, and Laboratory Findings of MP Pneumonia Patients
3.2. Comparison of Patients Treated With Macrolide and Those Without
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Lee, K.Y. Pediatric respiratory infections by Mycoplasma pneumoniae. Expert Rev. Anti Infect. Ther. 2008, 6, 509–521. [Google Scholar] [CrossRef] [PubMed]
- Eun, B.W.; Kim, N.H.; Choi, E.H.; Lee, H.J. Mycoplasma pneumoniae in Korean children: The epidemiology of pneumonia over an 18-year period. J. Infect. 2008, 56, 326–331. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.K.; Youn, Y.S.; Rhim, J.W.; Shin, M.S.; Kang, J.H.; Lee, K.Y. Epidemiological comparison of three Mycoplasma pneumoniae pneumonia epidemics in a single hospital over 10 years. Korean J. Pediatr. 2015, 58, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Waites, K.B.; Xiao, L.; Liu, Y.; Balish, M.F.; Atkinson, T.P. Mycoplasma pneumoniae from the respiratory tract and beyond. Clin. Microbiol. Rev. 2017, 30, 747–809. [Google Scholar] [CrossRef] [PubMed]
- Kingston, J.R.; Chanock, R.M.; Musfun, M.A. Eaton agent pneumonia. JAMA 1961, 176, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Rasch, J.R.; Mogabgab, W.J. Therapeutic effect of erythromycin on Mycoplasma pneumoniae pneumonia. Anthmicrob. Agents Chemother. 1965, 5, 633–639. [Google Scholar]
- Stevens, D.; Swift, P.G.; Johnston, P.G.; Kearney, P.J.; Corner, B.D.; Burman, D. Mycoplasma pneumoniae infections in children. Arch. Dis. Child 1978, 53, 38–42. [Google Scholar] [CrossRef]
- Lee, K.Y.; Lee, H.S.; Hong, J.H.; Lee, M.H.; Lee, J.S.; Burgner, D.; Lee, B.C. Role of prednisolone treatment in severe Mycoplasma pneumoniae pneumonia in children. Pediatr. Pulmonol. 2006, 41, 263–268. [Google Scholar] [CrossRef]
- Tamura, A.; Matsubara, K.; Tanaka, T.; Nigami, H.; Yura, K.; Fukaya, T. Methylprednisolone pulse therapy for refractory Mycoplasma pneumoniae pneumonia in children. J. Infect. 2008, 57, 223–228. [Google Scholar] [CrossRef]
- Miyashita, N.; Obase, Y.; Ouchi, K.; Kawasaki, K.; Kawai, Y.; Kobashi, Y.; Oka, M. Clinical features of severe Mycoplasma pneumoniae pneumonia in adults admitted to an intensive care unit. J. Med. Microbiol. 2007, 56, 1625–1629. [Google Scholar] [CrossRef]
- Youn, Y.S.; Lee, K.Y. Mycoplasma pneumoniae pneumonia in children. Korean J. Pediatr. 2012, 55, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Gardiner, S.J.; Gavranich, J.B.; Chang, A.B. Antibiotics for community-acquired lower respiratory tract infections secondary to Mycoplasma pneumoniae in children. Cochrane Database Syst. Rev. 2015, 1, CD004875. [Google Scholar] [CrossRef]
- Spuesens, E.B.; Meyer Sauteur, P.M.; Vink, C.; van Rossum, A.M. Mycoplasma pneumoniae infections; does treatment help? J. Infect. 2014, 69 (Suppl. 1), S42–S46. [Google Scholar] [CrossRef]
- Morozumi, M.; Takahashi, T.; Ubukata, K. Macrolide-resistant Mycoplasma pneumoniae: Characteristics of isolates and clinical aspects of community-acquired pneumonia. J. Infect. Chemother. 2010, 16, 78–86. [Google Scholar] [CrossRef]
- Cao, B.; Zhao, C.J.; Yin, Y.D.; Zhao, F.; Song, S.F.; Bai, L.; Zhang, J.Z.; Liu, Y.M.; Zhang, Y.Y.; Wang, H.; et al. High prevalence of macrolide resistance in Mycoplasma pneumoniae isolates from adult and adolescent patients with respiratory tract infections in China. Clin. Infect. Dis. 2010, 51, 189–194. [Google Scholar] [CrossRef]
- Hong, K.B.; Cho, E.H.; Lee, H.J.; Lee, S.Y.; Cho, E.Y.; Choi, J.H.; Kang, H.M.; Lee, J.; Ahn, Y.M.; Kang, Y.H.; et al. Macrolide resistance of Mycoplasma pneumoniae, South Korea, 2000–2011. Emerg. Infect. Dis. 2013, 19, 1281–1284. [Google Scholar] [CrossRef]
- Lee, E.; Cho, H.J.; Hong, S.J.; Lee, J.; Sung, H.; Yu, J. Prevalence and clinical manifestations of macrolide resistant Mycoplasma pneumoniae pneumonia in Korean children. Korean J. Pediatr. 2017, 60, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, S.; Yamazaki, T.; Narita, M.; Okazaki, N.; Suzuki, I.; Andoh, T.; Matsuoka, M.; Kenri, T.; Arakawa, Y.; Sasaki, T. Clinical evaluation of macrolide-resistant Mycoplasma pneumoniae. Antimicrob. Agents Chemother. 2006, 50, 709–712. [Google Scholar] [CrossRef]
- Matsubara, K.; Morozumi, M.; Okada, T.; Matsushima, T.; Komiyama, O.; Shoji, M.; Ebihara, T.; Ubukata, K.; Sato, Y.; Akita, H.; et al. A comparative clinical study of macrolide-sensitive and macrolide-resistant Mycoplasma pneumoniae infections in pediatric patients. J. Infect. Chemother. 2009, 15, 380–383. [Google Scholar] [CrossRef]
- Zhou, Y.; Zhang, Y.; Sheng, Y.; Zhang, L.; Shen, Z.; Chen, Z. More complications occur in macrolide-resistant than in macrolide-sensitive Mycoplasma pneumoniae pneumonia. Antimicrob. Agents Chemother. 2014, 58, 1034–1038. [Google Scholar] [CrossRef] [PubMed]
- Youn, Y.S.; Lee, K.T.; Hwang, J.Y.; Rhim, J.W.; Kang, J.H.; Lee, J.S.; Kim, J.C. Difference of clinical features in childhood Mycoplasma pneumoniae pneumonia. BMC Pediatr. 2010, 10, 48. [Google Scholar] [CrossRef] [PubMed]
- Youn, Y.S.; Lee, S.C.; Rhim, J.W.; Shin, M.S.; Kang, J.H.; Lee, K.Y. Early additional immune-modulators for Mycoplasma pneumoniae pneumonia in children: An observation study. Infect. Chemother. 2014, 46, 239–247. [Google Scholar] [CrossRef]
- Lee, S.C.; Youn, Y.S.; Rhim, J.W.; Kang, J.H.; Lee, K.Y. Early serologic diagnosis of Mycoplasma pneumoniae pneumonia: An observational study on changes in titers of a specific-IgM antibodies and cold agglutinins. Medicine 2016, 95, e3605. [Google Scholar] [CrossRef]
- Bradley, J.S.; Byington, C.L.; Shah, S.S.; Alverson, B.; Carter, E.R.; Harrison, C.; Kaplan, S.L.; Mace, S.E.; McCracken, G.H., Jr.; Moore, M.R.; et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: Clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin. Infect. Dis. 2011, 53, e25–e76. [Google Scholar] [CrossRef]
- Yamazaki, T.; Kenri, T. Epidemiology of Mycoplasma pneumoniae infections in Japan and therapeutic strategies for macrolide-resistant M. pneumoniae. Front. Microbiol. 2016, 7, 693. [Google Scholar] [CrossRef]
- McCracken, G.H., Jr. Current status of antibiotic treatment for Mycoplasma pneumoniae infections. Pediatr. Infect. Dis. 1986, 5, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Mills, G.D.; Oehley, M.R.; Arrol, B. Effectiveness of beta lactam antibiotics compared with antibiotics active against atypical pathogens in non-severe community acquired pneumonia: Meta-analysis. BMJ 2005, 330, 456. [Google Scholar] [CrossRef] [PubMed]
- Okada, T.; Morozumi, M.; Tajima, T.; Hasegawa, M.; Sakata, H.; Ohnari, S.; Chiba, N.; Iwata, S.; Ubukata, K. Rapid effectiveness of minocycline or doxycycline against macrolide-resistant Mycoplasma pneumoniae infection in a 2011 outbreak among Japanese children. Clin. Infect. Dis. 2012, 55, 1642–1649. [Google Scholar] [CrossRef]
- Kawai, Y.; Miyashita, N.; Kubo, M.; Akaike, H.; Kato, A.; Nishizawa, Y.; Saito, A.; Kondo, E.; Teranishi, H.; Ogita, S.; et al. Therapeutic efficacy of macrolides, minocycline, and tosufloxacin against macrolide-resistant Mycoplasma pneumoniae pneumonia in pediatric patients. Antimicrob. Agents Chemother. 2013, 57, 2252–2258. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Shin, K.S.; Lee, K.H.; Kim, Y.R.; Choi, J.H. Clinical characteristics of macrolide resistant Mycoplasma pneumoniae from children in Jeju. J. Korean Med. Sci. 2017, 32, 1642–1646. [Google Scholar] [CrossRef]
- Yang, D.; Chen, L.; Chen, Z. The timing of azithromycin treatment is not associated with the clinical prognosis of childhood Mycoplasma pneumoniae pneumonia in high macrolide-resistant prevalence settings. PLoS ONE 2018, 13, e0191951. [Google Scholar] [CrossRef]
- Lee, H.; Yun, K.W.; Lee, H.J.; Choi, E.H. Antimicrobial therapy of macrolide-resistant Mycoplasma pneumoniae pneumonia in children. Expert Rev. Anti Infect. Ther. 2018, 16, 23–34. [Google Scholar] [CrossRef]
- Yang, J.H.; Song, D.J.; Shim, J.Y. Mechanism of resistance acquisition and treatment of macrolide-resistant Mycoplamsa pneumoniae pneumonia in children. Korean J. Pediatr. 2017, 60, 167–174. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Walker, M.J.; Barnett, T.C.; McArthur, J.D.; Cole, J.N.; Gillen, C.M.; Henningham, A.; Sriprakash, K.S.; Sanderson-Smith, M.L.; Nizet, V. Disease manifestations and pathogenic mechanisms of Group A Streptococcus. Clin. Microbiol. Rev. 2014, 27, 264–301. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.Y.; Rhim, J.W.; Kang, J.H. Kawasaki disease: Laboratory findings and an immunopathogenesis on the premise of a “protein homeostasis system”. Yonsei Med. J. 2012, 53, 262–275. [Google Scholar] [CrossRef] [PubMed]
- Razin, S.; Yogev, D.; Naot, Y. Molecular biology and pathogenicity of mycoplasmas. Microbiol. Mol. Biol. Rev. 1998, 62, 1094–1156. [Google Scholar]
- Rottem, S. Interaction of mycoplasmas with host cells. Physiol. Rev. 2003, 83, 417–432. [Google Scholar] [CrossRef]
- Hegde, S.; Hegde, S.; Spergser, J.; Brunthaler, R.; Rosengarten, R.; Chopra-Dewasthaly, R. In vitro and in vivo cell invasion and systemic spreading of Mycoplasma Agalactiae in the sheep infection model. Int. J. Med. Microbiol. 2014, 304, 1024–1031. [Google Scholar] [CrossRef]
- Lee, K.Y. A common immunopathogenesis mechanism for infectious diseases: The protein-homeostasis-system hypothesis. Infect. Chemother. 2015, 47, 12–26. [Google Scholar] [CrossRef]
- Lee, K.Y. Pneumonia, acute respiratory distress syndrome, and early immune-modulator therapy. Int. J. Mol. Sci. 2017, 18, 388. [Google Scholar] [CrossRef]
- Lee, K.Y.; Rhim, J.W.; Kang, J.H. Hyperactive immune cells (T cells) may be responsible for acute lung injury in influenza virus infections: A need for early immune-modulators for severe cases. Med. Hypotheses 2011, 76, 64–69. [Google Scholar] [CrossRef]
- Rhim, J.W.; Lee, K.Y.; Youn, Y.S.; Kang, J.H.; Kim, J.C. Epidemiological and clinical characteristics of childhood pandemic 2009 H1N1 virus infection: An observational cohort study. BMC Infect. Dis. 2011, 11, 225. [Google Scholar] [CrossRef]
- Blum, C.A.; Nigro, N.; Briel, M.; Schuetz, P.; Ullmer, E.; Suter-Widmer, I.; Winzeler, B.; Bingisser, R.; Elsaesser, H.; Drozdov, D.; et al. Adjunct prednisone therapy for patients with community-acquired pneumonia: A multicentre, double-blind, randomised, placebo-controlled trial. Lancet 2015, 385, 1511–1518. [Google Scholar] [CrossRef]
- Torres, A.; Sibila, O.; Ferrer, M.; Polverino, E.; Menendez, R.; Mensa, J.; Gabarrús, A.; Sellarés, J.; Restrepo, M.I.; Anzueto, A.; et al. Effect of corticosteroids on treatment failure among hospitalized patients with severe community-acquired pneumonia and high inflammatory response: A randomized clinical trial. JAMA 2015, 313, 677–686. [Google Scholar] [CrossRef] [PubMed]
- You, S.Y.; Jwa, H.J.; Yang, E.A.; Kil, H.R.; Lee, J.H. Effects of methylprednisolone pulse therapy on refractory Mycoplasma pneumoniae pneumonia in children. Allergy Asthma Immunol. Res. 2014, 6, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Kim, J.Y.; Yoo, C.H.; Seo, W.H.; Yoo, Y.; Song, D.J.; Choung, J.T. Macrolide resistance and its impacts on M. pneumoniae pneumonia in children: Comparison of two recent epidemics in Korea. Allergy Asthma Immunol. Res. 2017, 9, 340–346. [Google Scholar] [CrossRef]
- Kil, H.R.; Lee, J.H.; Lee, K.Y.; Rhim, J.W.; Youn, Y.S.; Kang, J.H. Early corticosteroid treatment for severe pneumonia caused by 2009 H1N1 influenza virus. Crit. Care 2011, 15, 413. [Google Scholar] [CrossRef]
| Clinical Characteristics | All | Macrolide (+) | Macrolide (−) | p-Value * |
|---|---|---|---|---|
| (n = 257) | (n = 172) | (n = 85) | ||
| Age (year) | 5.6 ± 3.1 | 5.7 ± 3.5 | 5.4 ± 2.9 | 0.614 |
| Male-female ratio | 130:127 | 86:86 | 44:41 | 0.793 |
| Diagnosis (n, %) † | ||||
| Increased titers | 177 (69) | 121 (70) | 56 (66) | 0.477 |
| Seroconversion | 33 (13) | 15 (9) | 18 (21) | 0.06 |
| High titers ≥1:640 | 47 (18) | 36 (21) | 11 (13) | 0.127 |
| Hospitalization (day) | 6.0 ± 1.8 | 6.1 ± 1.9 | 5.9 ± 1.4 | 0.424 |
| Duration of fever (day) | ||||
| Before admission | 5.1 ± 2.6 | 5.1 ± 2.5 | 5.2 ± 2.9 | 0.683 |
| Total duration | 5.6 ± 2.8 | 5.7 ± 2.8 | 5.5 ± 2.9 | 0.621 |
| Corticosteroids, n (%) | ||||
| Oral prednisolone (1 mg/kg) | 114 (44) | 80 (47) | 34 (40) | 0.352 |
| Intravenous MP (1–2 mg/kg) | 100 (39) | 62 (36) | 38 (45) | 0.221 |
| High-dose MP (5 mg/kg or 10 mg/kg) | 43 (17) | 30 (17) | 13 (15) | 0.619 |
| Additive MP (5 mg/kg or 10 mg/kg) | 8 (3) | 6 (4) | 2 (2) | 0.724 |
| Pneumonic infiltration, n (%) | ||||
| Bronchopneumonia | 68 (26) | 47 (27) | 21 (25) | 0.764 |
| Segmental/lobar pneumonia | 189 (74) | 125 (73) | 63 (75) | 0.882 |
| Laboratory Parameters | All | Macrolide (+) | Macrolide (−) | p-Value |
|---|---|---|---|---|
| (n = 257) | (n = 172) | (n = 85) | ||
| WBC (×103/µL) | 8.2 (1.5–28.5) | 7.9 (1.5–28.5) | 8.3 (4.1–25.4) | 0.202 |
| Neutrophil (%) | 62.9 (16.0–88.5) | 62.4 (18.0–83.9) | 63.6 (16.0–88.5) | 0.786 |
| Lymphocyte (%) | 25.7 (6.4–75.3) | 26.0 (7.0–65.2) | 24.8 (6.4–75.3) | 0.930 |
| Monocyte (%) | 8.1 (0.2–22) | 8.2 (0.2–17) | 8.0 (0.7–22) | 0.731 |
| Hemoglobin (g/dL) | 12.1 (10.1–15.5) | 12.1 (10.1–15.5) | 12.2 (10.6–14.6) | 0.443 |
| ESR (mm/h) | 24 (3–84) | 25 (3–84) | 23 (3–72) | 0.145 |
| CRP (mg/dL) | 2.4 (0.1–19.9) | 2.4 (0.1–14.3) | 2.4 (0.1–19.9) | 0.544 |
| LDH (IU/L) | 287 (23–1600) | 295 (23–748) | 283 (147–1600) | 0.174 |
| ALP (IU/L) | 159 (58–323) | 157 (58–293) | 165 (64–323) | 0.131 |
| AST (IU/L) | 30 (15–908) | 30 (15–299) | 29 (16–908) | 0.855 |
| ALT (IU/L) | 14 (3–1638) | 14 (3–295) | 14 (6–1638) | 0.572 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, E.-A.; Kang, H.-M.; Rhim, J.-W.; Kang, J.-H.; Lee, K.-Y. Early Corticosteroid Therapy for Mycoplasma pneumoniae Pneumonia Irrespective of Used Antibiotics in Children. J. Clin. Med. 2019, 8, 726. https://doi.org/10.3390/jcm8050726
Yang E-A, Kang H-M, Rhim J-W, Kang J-H, Lee K-Y. Early Corticosteroid Therapy for Mycoplasma pneumoniae Pneumonia Irrespective of Used Antibiotics in Children. Journal of Clinical Medicine. 2019; 8(5):726. https://doi.org/10.3390/jcm8050726
Chicago/Turabian StyleYang, Eun-Ae, Hyun-Mi Kang, Jung-Woo Rhim, Jin-Han Kang, and Kyung-Yil Lee. 2019. "Early Corticosteroid Therapy for Mycoplasma pneumoniae Pneumonia Irrespective of Used Antibiotics in Children" Journal of Clinical Medicine 8, no. 5: 726. https://doi.org/10.3390/jcm8050726
APA StyleYang, E.-A., Kang, H.-M., Rhim, J.-W., Kang, J.-H., & Lee, K.-Y. (2019). Early Corticosteroid Therapy for Mycoplasma pneumoniae Pneumonia Irrespective of Used Antibiotics in Children. Journal of Clinical Medicine, 8(5), 726. https://doi.org/10.3390/jcm8050726





