Comparative Study between an Immediate Loading Protocol Using the Digital Workflow and a Conventional Protocol for Dental Implant Treatment: A Randomized Clinical Trial
Abstract
:1. Introduction
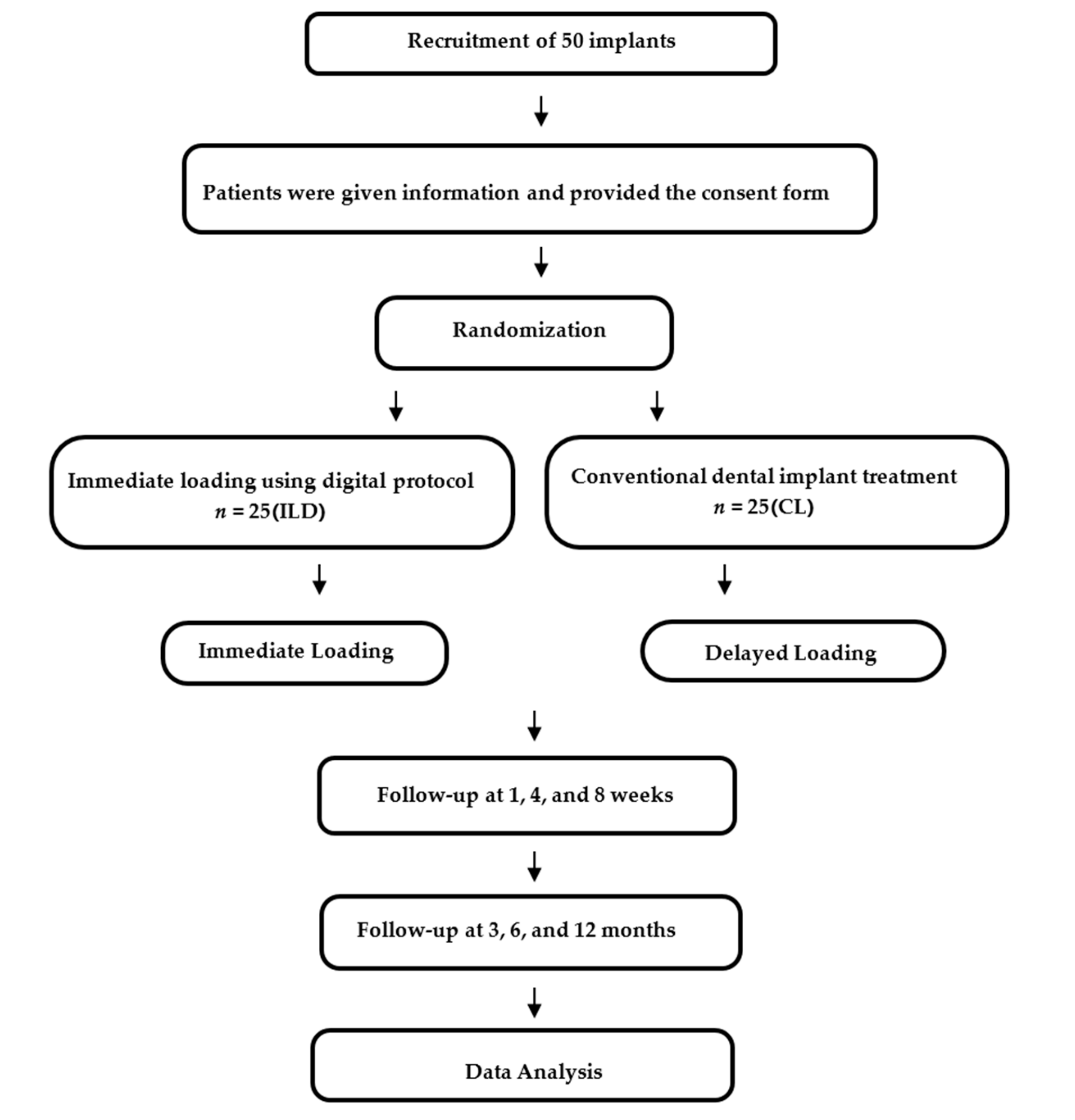
2. Experimental Section
2.1. Patients Selection
2.2. Surgical Procedures
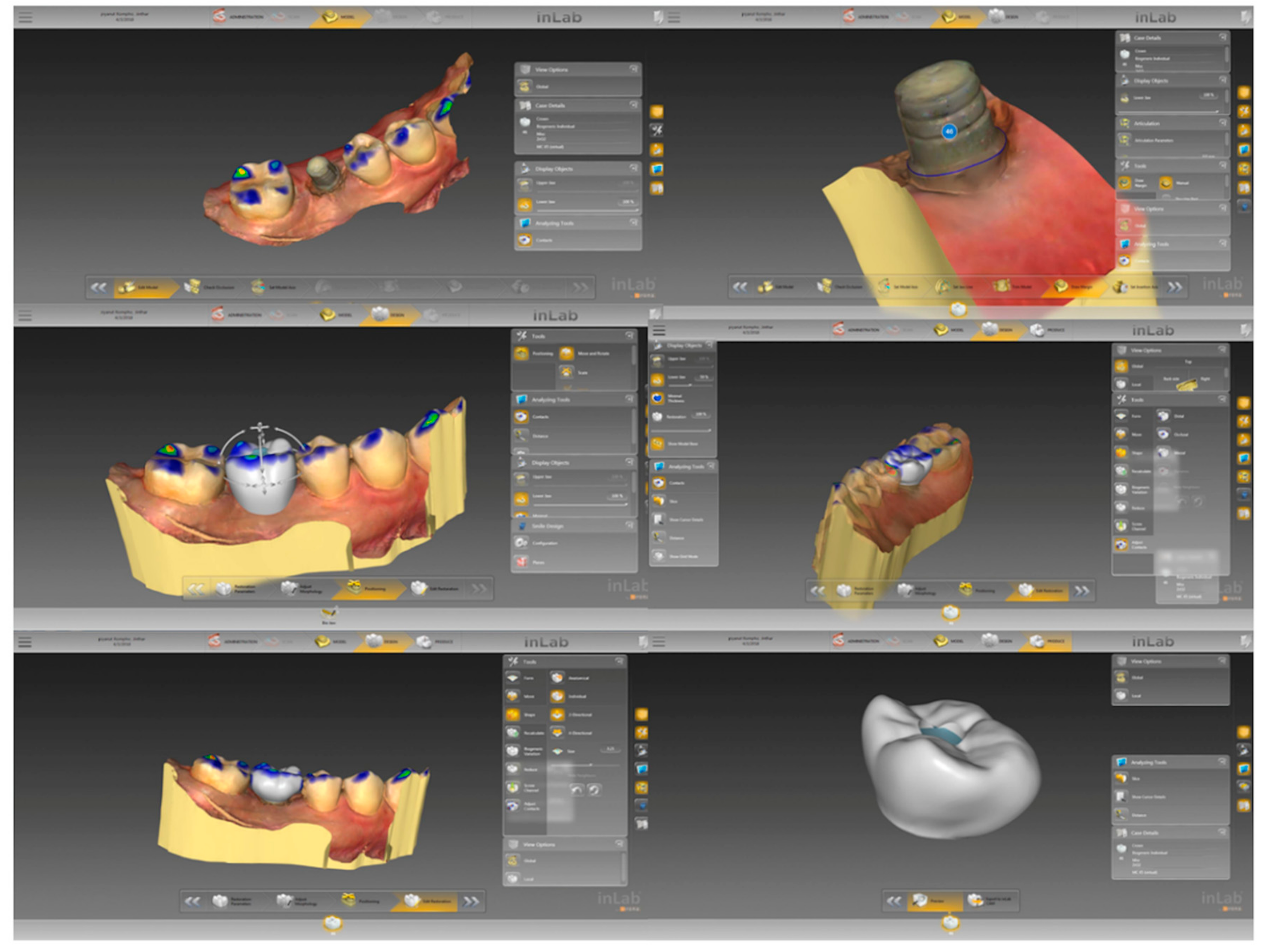
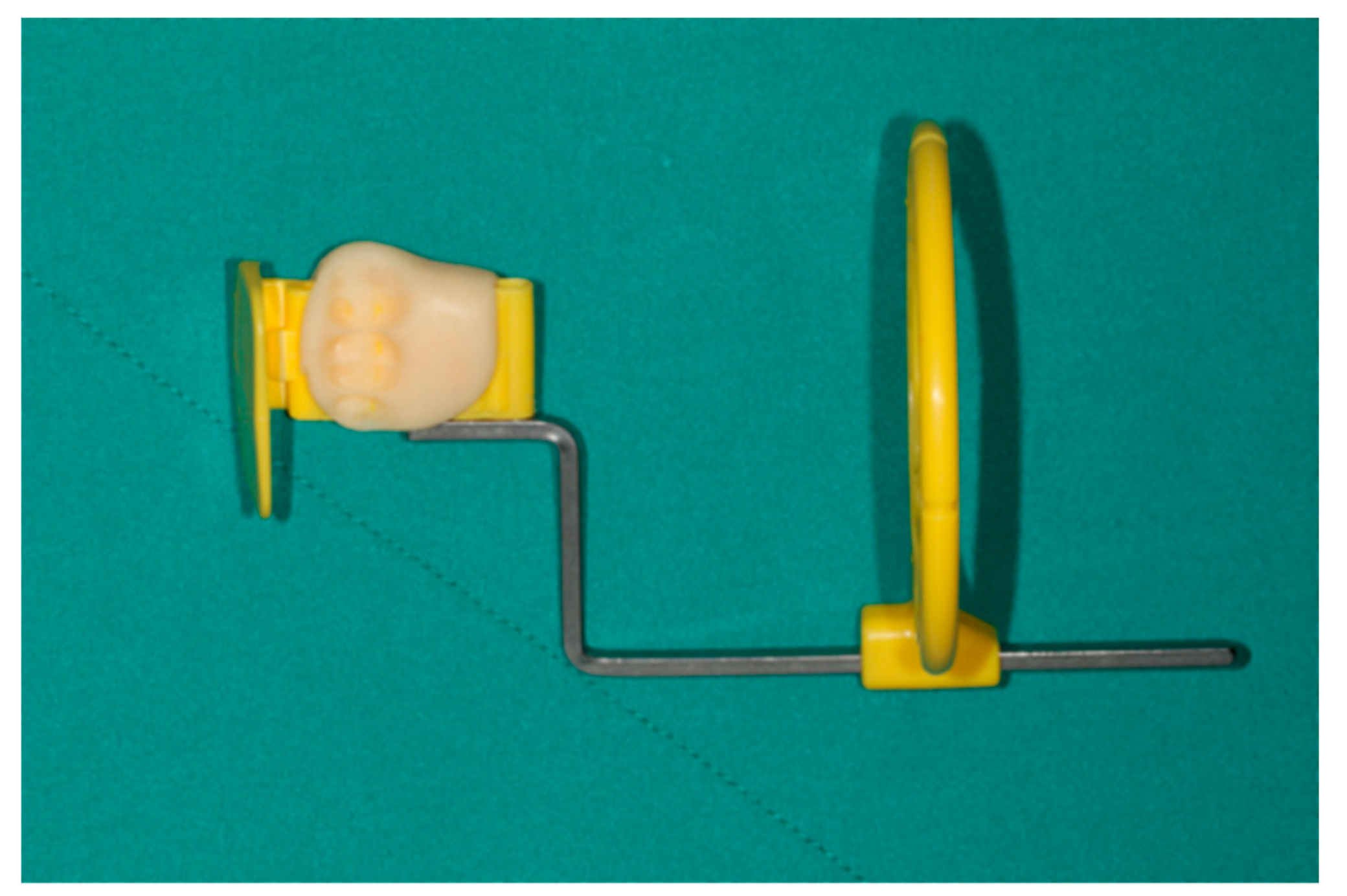
2.3. Prosthetic Procedures
2.4. Parameters for Measurement
- functionality without pain or tenderness;
- zero mobility;
- radiographic bone loss resulting from surgery not exceeding 2 mm; and,
- absence of exudate history.
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Albrektsson, T.; Zarb, G.; Worthington, P.; Eriksson, A.R. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int. J. Oral Maxillofac. Implant. 1986, 1, 11–25. [Google Scholar]
- Henry, P.J.; Laney, W.R.; Jemt, T.; Harris, D.; Krogh, P.H.; Polizzi, G.; A Zarb, G.; Herrmann, I. Osseointegrated implants for single-tooth replacement: A prospective 5-year multicenter study. Int. J. Oral Implant. 1996, 11, 450–455. [Google Scholar]
- Becker, W.; Becker, B.E.; Israelon, H.; Lucchini, J.P.; Handelsman, M.; Ammons, W.; Rosenberg, E.; Rose, L.; Tucker, L.M.; Lekholm, U. One-step surgical placement of Brånemark implants: A prospective multicenter clinical study. Int. J. Oral Maxillofac. Implant. 1967, 12, 454–462. [Google Scholar]
- Buser, D.; Bernard, J.P.; Behneke, A.; Behneke, N.; Hirt, H.P.; Mericske-Stern, R.; Belser, U.C.; Lang, N.P. Long-term evaluation of non-submerged ITI implants. Part I: 8-year lift table analysis of a prospective multicenter study with 2359 implants. Clin. Oral Implant. Res. 1997, 8, 161–172. [Google Scholar] [CrossRef]
- Arvidson, K.; Bystedt, H.; Frykholm, A.; Von Konow, L.; Lothigius, E. Five-year prospective follow-up report of the Astra Tech Dental Implant System in the treatment of edentulous mandibles. Clin. Oral Implant. Res. 1998, 9, 225–234. [Google Scholar] [CrossRef]
- Branemark, P.I.; Hansson, B.O.; Adell, R.; Breine, U.; Lindstrom, J.; Hallen, O.; Ohman, A. Osseointegratated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand. J. Plast. Reconstr. Surg. Suppl. 1977, 16, 1–132. [Google Scholar]
- Albrektsson, T. On long-term maintenance of the osseointegrated response. Aust. Prosthodont. J. 1993, 7, 15–24. [Google Scholar] [PubMed]
- Åstrand, P.; Almfeldt, I.; Brunell, G.; Hamp, S.-E.; Hellem, S.; Karlsson, U. Non-submerged implants in the treatment of the edentulous lower jaw. A 2-year longitudinal study. Clin. Oral Implant. 1996, 7, 337–344. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Thoma, D.; Jung, R.; Zwahlen, M.; Zembic, A. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin. Oral Implant. 2012, 23, 22–38. [Google Scholar]
- Weber, H.-P.; Morton, D.; O Gallucci, G.; Roccuzzo, M.; Cordaro, L.; Grutter, L. Consensus statements and recommended clinical procedures regarding loading protocols. Int. J. Oral Implant. 2009, 24, 180–183. [Google Scholar]
- Esposito, M.; Willings, M.; Coulthard, P.; Worthington, H.V.; Grusovin, M.G. The effectiveness of immediate, early and conventional loading of dental implants: a Cochrane systemic review of randomized controlled clinical trials. Int. J. Oral Maxillofac. Implant. 2007, 22, 893–904. [Google Scholar]
- Linkow, L.I.; Miller, R.J. Immediate Loading of Endosseous Implants Is Not New. J. Oral Implant. 2004, 30, 314–317. [Google Scholar] [CrossRef] [PubMed]
- Moraschini, V.; Barboza, E.P. Immediate versus conventional loaded single implants in the posterior mandible: a meta-analysis of randomized controlled trials. Int. J. Oral Surg. 2016, 45, 85–92. [Google Scholar] [CrossRef]
- Duret, F.; Blouin, J.L.; Duret, B. CAD/CAM in dentistry. J. Am. Dent. Assoc. 1988, 117, 715–720. [Google Scholar] [CrossRef] [PubMed]
- Priest, G. Virtual-Designed and Computer-Milled Implant Abutments. J. Oral Surg. 2005, 63, 22–32. [Google Scholar] [CrossRef]
- Joda, T.; Braqqer, U. Complete digital workflow for the production of implant-supported single-unit monolithic crowns. Clin. Oral Implant. Res. 2014, 25, 1304–1306. [Google Scholar] [CrossRef]
- Misch, C.E.; Perel, M.L.; Wang, H.L.; Sammartino, G.; Galindo-Moreno, P.; Trisi, P.; Steigmann, M.; Rebaudi, A.; Palti, A.; Pikos, M.A.; et al. Implant success, survival, and failure: The International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant. Dent. 2008, 17, 5–15. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Karoussis, I.; Bürgin, W.; Bragger, U.; Lang, N.P. Patients’ satisfaction following implant therapy. A 10-year prospective cohort study. Clin. Oral Implant. 2005, 16, 185–193. [Google Scholar] [CrossRef]
- Strub, J.R.; Jurdzik, B.A.; Tuna, T. Prognosis of immediately loaded implants and their restorations: A systematic literature review. J. Oral Rehabil. 2012, 39, 704–717. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, R.B.; Albrektsson, T.; Wennerberg, A. Immediate non functional versus immediate functional loading and dental implant failure rates: A systematic review and meta-analysis. J. Dent. 2014, 42, 1052–1059. [Google Scholar] [CrossRef]
- Guidetti, L.; Monnazzi, M.; Piveta, A.; Gabrielli, M.; Gabrielli, M.; Filho, V.P. Evaluation of single implants placed in the posterior mandibular area under immediate loading: A prospective study. Int. J. Oral Surg. 2015, 44, 1411–1415. [Google Scholar] [CrossRef] [PubMed]
- Engelhardt, S.; Papacosta, P.; Rathe, F.; Özen, J.; Jansen, J.A.; Junker, R. Annual failure rates and marginal bone-level changes of immediate compared to conventional loading of dental implants. A systematic review of the literature and meta-analysis. Clin. Oral Implant. Res. 2015, 26, 671–687. [Google Scholar] [CrossRef]
- Giacomel, M.; Camati, P.; Souza, J.; Deliberador, T. Comparison of Marginal Bone Level Changes of Immediately Loaded Implants, Delayed Loaded Nonsubmerged Implants, and Delayed Loaded Submerged Implants: A Randomized Clinical Trial. Int. J. Oral Implant. 2017, 32, 661–666. [Google Scholar] [CrossRef]
- Joda, T.; Brägger, U. Time-efficientcy analysis of the treatment with monolithic implant crowns in digital workflow: A randomized control trial. Clin. Oral Implant. Res. 2016, 27, 1401–1416. [Google Scholar] [CrossRef]
- Zembic, A.; Bösch, A.; Jung, R.E.; Hämmerle, C.H.; Sailer, I. Five-year results of a randomized controlled clinical trial comparing zirconia and titanium abutments supporting single-implant crowns in canine and posterior regions. Clin. Oral Implant. Res. 2013, 24, 384–390. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.J.; Yuan, J.C.-C.; Hedger, P.J.; Taylor, E.J.; Harlow, R.F.; Knoernschild, K.L.; Campbell, S.D.; Sukotjo, C. Patient Perception and Satisfaction with Implant Therapy in a Predoctoral Implant Education Program: A Preliminary Study. J. Prosthodont. 2015, 24, 525–531. [Google Scholar] [CrossRef] [PubMed]


| Inclusion Criteria | Exclusion Criteria |
|---|---|
| General Criteria | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |
| |
| |
| Dental Implant Criteria | |
| |
| |
| |
| 1. | Does your dental implant and crown allow good functional use? |
| 2. | Which are better for chewing: the dental implant, or natural teeth? |
| 3. | Are you able to speak normally? |
| 4. | Are you satisfied with the way you look? |
| 5. | Are you able to clean the implant easily? |
| 6. | Is it easier to clean the dental implant than natural teeth? |
| 7. | Is it faster to clean the dental implant, or the natural teeth? |
| 8. | Has the dental implant treatment performed as expected? |
| 9. | Compared to the opportunity to wear dentures, would you prefer to undergo the dental implant treatment? |
| 10. | Would you encourage friends or family to have the dental implant treatment? |
| 11. | Do you believe that the dental implant price is suitable? |
| Patient Demographic | Immediate Loading Using Digital Workflow | Conventional Loading |
|---|---|---|
| Male/Female | 4/21 | 8/17 |
| Mean age | 49.16 ± 11.07 | 51.60 ± 16.44 |
| First molar/second molar | 25/0 | 24/1 |
| Implant Stability Measurements | ILD Group (n = 25) | CL Group (n = 25) |
|---|---|---|
| Mean ± SD | Mean ± SD | |
| ISQ | 78.26 ± 4.09 | 73.74 ± 5.14 |
| Insertion torque | 36.60 ± 12.64 | 38.80 ± 12.19 |
| Questionnaires | Group | Mean ± SD | t-test p Value |
|---|---|---|---|
| Question 1 | CL | 94.76 ± 9.45 | 0.004 |
| ILD | 86.34 ± 10.34 | ||
| Question 2 | CL | 63.15 ± 24.20 | 0.756 |
| ILD | 65.12 ± 20.55 | ||
| Question 3 | CL | 85.54 ± 22.44 | 0.832 |
| ILD | 86.79 ± 18.93 | ||
| Question 4 | CL | 87.07 ± 17.61 | 0.946 |
| ILD | 87.39 ± 14.49 | ||
| Question 5 | CL | 76.25 ± 18.26 | 0.923 |
| ILD | 76.76 ± 19.47 | ||
| Question 6 | CL | 64.23 ± 26.78 | 0.975 |
| ILD | 64.01 ± 21.59 | ||
| Question 7 | CL | 77.13 ± 23.20 | 0.146 |
| ILD | 68.41 ± 18.25 | ||
| Question 8 | CL | 95.05 ± 8.56 | 0.161 |
| ILD | 91.97 ± 10.32 | ||
| Question 9 | CL | 94.32 ± 8.61 | 0.363 |
| ILD | 92.02 ± 8.87 | ||
| Question 10 | CL | 94.99 ± 9.05 | 0.450 |
| ILD | 93.11 ± 9.39 | ||
| Question 11 | CL | 75.07 ± 20.98 | 0.271 |
| ILD | 68.51 ± 20.73 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rattanapanich, P.; Aunmeungtong, W.; Chaijareenont, P.; Khongkhunthian, P. Comparative Study between an Immediate Loading Protocol Using the Digital Workflow and a Conventional Protocol for Dental Implant Treatment: A Randomized Clinical Trial. J. Clin. Med. 2019, 8, 622. https://doi.org/10.3390/jcm8050622
Rattanapanich P, Aunmeungtong W, Chaijareenont P, Khongkhunthian P. Comparative Study between an Immediate Loading Protocol Using the Digital Workflow and a Conventional Protocol for Dental Implant Treatment: A Randomized Clinical Trial. Journal of Clinical Medicine. 2019; 8(5):622. https://doi.org/10.3390/jcm8050622
Chicago/Turabian StyleRattanapanich, Piyanut, Weerapan Aunmeungtong, Pisaisit Chaijareenont, and Pathawee Khongkhunthian. 2019. "Comparative Study between an Immediate Loading Protocol Using the Digital Workflow and a Conventional Protocol for Dental Implant Treatment: A Randomized Clinical Trial" Journal of Clinical Medicine 8, no. 5: 622. https://doi.org/10.3390/jcm8050622
APA StyleRattanapanich, P., Aunmeungtong, W., Chaijareenont, P., & Khongkhunthian, P. (2019). Comparative Study between an Immediate Loading Protocol Using the Digital Workflow and a Conventional Protocol for Dental Implant Treatment: A Randomized Clinical Trial. Journal of Clinical Medicine, 8(5), 622. https://doi.org/10.3390/jcm8050622





