Structured Cognitive-Motor Dual Task Training Compared to Single Mobility Training in Persons with Multiple Sclerosis, a Multicenter RCT
Abstract
1. Introduction
2. Experimental Section
2.1. Participants
2.2. Study Design and Procedure
2.3. Intervention
2.4. Measures
2.4.1. Primary Outcome Measures
2.4.2. Descriptive and Secondary Outcome Measures
2.5. Statistical Analysis
3. Results
3.1. Primary Outcome Measures
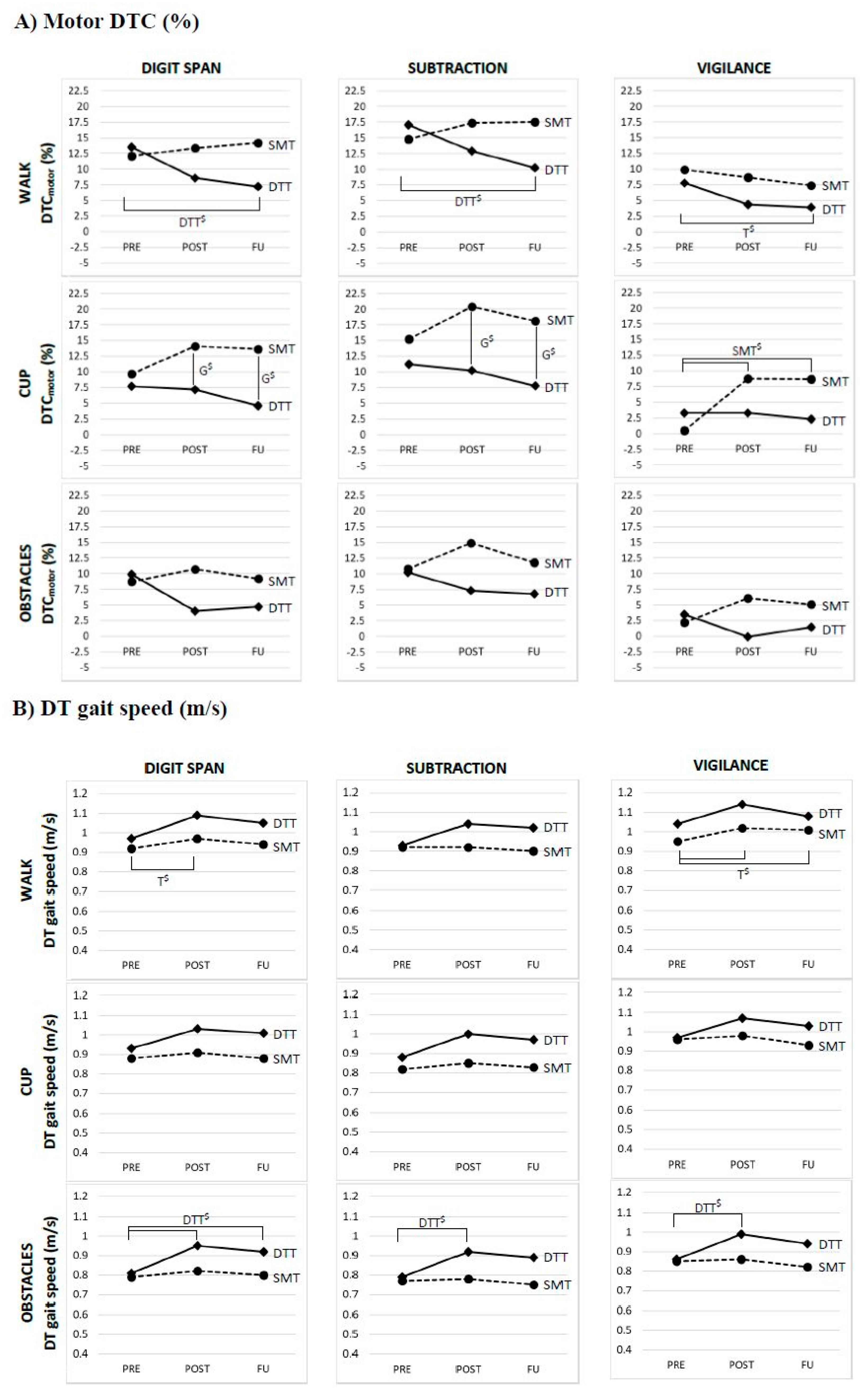
3.1.1. Motor Task Performance in the Dual Task Conditions
3.1.2. Cognitive Task Performance in the Dual Task Conditions
3.2. Secondary Outcome Measures
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rao, S.M.; Leo, G.J.; Bernardin, L.; Unverzagt, F. Cognitive dysfunction in multiple sclerosis. I. Frequency, patterns, and prediction. Neurology 1991, 41, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Peyser, J.M.; Edwards, K.R.; Poser, C.M.; Filskov, S.B. Cognitive function in patients with multiple sclerosis. Arch. Neurol. 1980, 37, 577–579. [Google Scholar] [CrossRef] [PubMed]
- Chiaravalloti, N.D.; DeLuca, J. Cognitive impairment in multiple sclerosis. Lancet Neurol. 2008, 7, 1139–1151. [Google Scholar] [CrossRef]
- Larocca, N.G. Impact of walking impairment in multiple sclerosis: Perspectives of patients and care partners. Patient 2011, 4, 189–201. [Google Scholar] [CrossRef]
- McIntosh-Michaelis, S.A.; Roberts, M.H.; Wilkinson, S.M.; Diamond, I.D.; McLellan, D.L.; Martin, J.P.; Spackman, A.J. The prevalence of cognitive impairment in a community survey of multiple sclerosis. Br. J. Clin. Psychol. 1991, 30, 333–348. [Google Scholar] [CrossRef]
- Leone, C.; Patti, F.; Feys, P. Measuring the cost of cognitive-motor dual tasking during walking in multiple sclerosis. Mult. Scler. 2015, 21, 123–131. [Google Scholar] [CrossRef]
- Learmonth, Y.C.; Ensari, I.; Motl, R.W. Cognitive Motor Interference in Multiple Sclerosis: Insights from a Systematic Quantitative Review. Arch. Phys. Med. Rehabil. 2017, 98, 1229–1240. [Google Scholar] [CrossRef]
- Postigo-Alonso, B.; Galvao-Carmona, A.; Benitez, I.; Conde-Gavilan, C.; Jover, A.; Molina, S.; Pena-Toledo, M.A.; Aguera, E. Cognitive-motor interference during gait in patients with Multiple Sclerosis: A mixed methods Systematic Review. Neurosci. Biobehav. Rev. 2018, 94, 126–148. [Google Scholar] [CrossRef]
- Etemadi, Y. Dual task cost of cognition is related to fall risk in patients with multiple sclerosis: A prospective study. Clin. Rehabil. 2017, 31, 278–284. [Google Scholar] [CrossRef]
- Castelli, L.; De Luca, F.; Marchetti, M.R.; Sellitto, G.; Fanelli, F.; Prosperini, L. The dual task-cost of standing balance affects quality of life in mildly disabled MS people. Neurol. Sci. 2016, 37, 673–679. [Google Scholar] [CrossRef]
- Ruthruff, E.; Van Selst, M.; Johnston, J.C.; Remington, R. How does practice reduce dual-task interference: Integration, automatization, or just stage-shortening? Psychol. Res. 2006, 70, 125–142. [Google Scholar] [CrossRef] [PubMed]
- Silsupadol, P.; Lugade, V.; Shumway-Cook, A.; van Donkelaar, P.; Chou, L.S.; Mayr, U.; Woollacott, M.H. Training-related changes in dual-task walking performance of elderly persons with balance impairment: A double-blind, randomized controlled trial. Gait Posture 2009, 29, 634–639. [Google Scholar] [CrossRef] [PubMed]
- Wajda, D.A.; Mirelman, A.; Hausdorff, J.M.; Sosnoff, J.J. Intervention modalities for targeting cognitive-motor interference in individuals with neurodegenerative disease: A systematic review. Expert Rev Neurother. 2017, 17, 251–261. [Google Scholar] [CrossRef] [PubMed]
- Fritz, N.E.; Cheek, F.M.; Nichols-Larsen, D.S. Motor-Cognitive Dual-Task Training in Persons with Neurologic Disorders: A Systematic Review. J. Neurol. Phys. Ther. 2015, 39, 142–153. [Google Scholar] [CrossRef]
- Ghai, S.; Ghai, I.; Effenberg, A.O. Effects of dual tasks and dual-task training on postural stability: A systematic review and meta-analysis. Clin. Interv. Aging 2017, 12, 557–577. [Google Scholar] [CrossRef]
- Sosnoff, J.J.; Wajda, D.A.; Sandroff, B.M.; Roeing, K.L.; Sung, J.; Motl, R.W. Dual task training in persons with Multiple Sclerosis: A feasability randomized controlled trial. Clin. Rehabil. 2017, 31, 1322–1331. [Google Scholar] [CrossRef]
- Monjezi, S.; Negahban, H.; Tajali, S.; Yadollahpour, N.; Majdinasab, N. Effects of dual-task balance training on postural performance in patients with Multiple Sclerosis: A double-blind, randomized controlled pilot trial. Clin. Rehabil. 2017, 31, 234–241. [Google Scholar] [CrossRef]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Strouwen, C.; Molenaar, E.A.; Keus, S.H.; Munks, L.; Munneke, M.; Vandenberghe, W.; Bloem, B.R.; Nieuwboer, A. Protocol for a randomized comparison of integrated versus consecutive dual task practice in Parkinson’s disease: The DUALITY trial. BMC Neurol. 2014, 14, 61. [Google Scholar] [CrossRef]
- Tacchino, A.; Veldkamp, R.; Coninx, K.; Brulmans, J.; Palmaers, S.; Hamalainen, P.; D’hooge, M.; Vanzeir, E.; Kalron, A.; Brichetto, G.; et al. Cognitive-motor interference in people with Multiple Sclerosis: Design, development and testing of CMI-APP for dual task assessment and training. JMIR Preprints 2019. In review. [Google Scholar]
- Veldkamp, R.; Romberg, A.; Hamalainen, P.; Giffroy, X.; Moumdjian, L.; Leone, C.; Feys, P.; Baert, I. Test-Retest Reliability of Cognitive-Motor Interference Assessments in Walking With Various Task Complexities in Persons With Multiple Sclerosis. Neurorehabilit. Neural Repair 2019. [Google Scholar] [CrossRef] [PubMed]
- Iverson, G.L.; Tulsky, D.S. Detecting malingering on the WAIS-III. Unusual Digit Span performance patterns in the normal population and in clinical groups. Arch. Clin. Neuropsychol. 2003, 18, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Smith, A. The serial sevens subtraction test. Arch. Neurol. 1967, 17, 78–80. [Google Scholar] [CrossRef] [PubMed]
- Washabaugh, E.P.; Kalyanaraman, T.; Adamczyk, P.G.; Claflin, E.S.; Krishnan, C. Validity and repeatability of inertial measurement units for measuring gait parameters. Gait Posture 2017, 55, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Boringa, J.B.; Lazeron, R.H.; Reuling, I.E.; Ader, H.J.; Pfennings, L.; Lindeboom, J.; de Sonneville, L.M.; Kalkers, N.F.; Polman, C.H. The brief repeatable battery of neuropsychological tests: Normative values allow application in multiple sclerosis clinical practice. Mult. Scler. 2001, 7, 263–267. [Google Scholar] [CrossRef]
- Fischer, J.S.; Jak, A.J.; Kniker, J.E.; Rudick, R.A.; Cutter, G. Multiple Sclerosis Functional Composite Administration and Scoring Manual; National Multiple Sclerosis Society: New York, NY, USA, 2001. [Google Scholar]
- Podsiadlo, D.; Richardson, S. The timed Up & Go: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar]
- Shumway-Cook, A.; Woollacott, M.H. Motor Control Theory and Applications; William and Wilkins: Baltimore, MD, USA, 1995. [Google Scholar]
- Goldman, M.D.; Marrie, R.A.; Cohen, J.A. Evaluation of the six-minute walk in multiple sclerosis subjects and healthy controls. Mult. Scler. 2008, 14, 383–390. [Google Scholar] [CrossRef]
- Hobart, J.C.; Riazi, A.; Lamping, D.L.; Fitzpatrick, R.; Thompson, A.J. Measuring the impact of MS on walking ability: The 12-Item MS Walking Scale (MSWS-12). Neurology 2003, 60, 31–36. [Google Scholar] [CrossRef]
- Yardley, L.; Beyer, N.; Hauer, K.; Kempen, G.; Piot-Ziegler, C.; Todd, C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 2005, 34, 614–619. [Google Scholar] [CrossRef]
- Hobart, J.; Lamping, D.; Fitzpatrick, R.; Riazi, A.; Thompson, A. The Multiple Sclerosis Impact Scale (MSIS-29): A new patient-based outcome measure. Brain 2001, 124, 962–973. [Google Scholar] [CrossRef] [PubMed]
- Kos, D.; Kerckhofs, E.; Ketelaer, P.; Duportail, M.; Nagels, G.; D’Hooghe, M.; Nuyens, G. Self-report assessment of fatigue in multiple sclerosis: A critical evaluation. Occup. Ther. Health Care 2004, 17, 45–62. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.J.; Greenfield, E.; Wilson, B.A.; Bateman, A. Walking and talking therapy: Improving cognitive-motor dual-tasking in neurological illness. J. Int. Neuropsychol. Soc. 2009, 15, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Kal, E.; Winters, M.; van der Kamp, J.; Houdijk, H.; Groet, E.; van Bennekom, C.; Scherder, E. Is Implicit Motor Learning Preserved after Stroke? A Systematic Review with Meta-Analysis. PLoS ONE 2016, 11, e0166376. [Google Scholar] [CrossRef]
- Yogev-Seligmann, G.; Hausdorff, J.M.; Giladi, N. Do we always prioritize balance when walking? Towards an integrated model of task prioritization. Mov. Disord. 2012, 27, 765–770. [Google Scholar] [CrossRef]
- Lofgren, N.; Conradsson, D.; Rennie, L.; Moe-Nilssen, R.; Franzen, E. The effects of integrated single- and dual-task training on automaticity and attention allocation in Parkinson’s disease: A secondary analysis from a randomized trial. Neuropsychology 2019, 33, 147–156. [Google Scholar] [CrossRef]
- Baert, I.; Freeman, J.; Smedal, T.; Dalgas, U.; Romberg, A.; Kalron, A.; Conyers, H.; Elorriaga, I.; Gebara, B.; Gumse, J.; et al. Responsiveness and clinically meaningful improvement, according to disability level, of five walking measures after rehabilitation in multiple sclerosis: A European multicenter study. Neurorehabil. Neural Repair 2014, 28, 621–631. [Google Scholar] [CrossRef]
- Strouwen, C.; Molenaar, E.; Munks, L.; Broeder, S.; Ginis, P.; Bloem, B.R.; Nieuwboer, A.; Heremans, E. Determinants of Dual-Task Training Effect Size in Parkinson Disease: Who Will Benefit Most? J. Neurol. Phys. Ther. 2019, 43, 3–11. [Google Scholar] [CrossRef]

| DTT (n = 20) | SMT (n = 20) | p-value DTT vs. SMT | Drop-out (n = 7) | p-value Drop-out vs. Remained | |
|---|---|---|---|---|---|
| Age (years) | 51.4 ± 9.3 | 53.4 ± 9.2 | 0.507 | 49.5 ± 8.5 | 0.436 |
| Gender (F/M, %) | 60/40 | 55/45 | 1.00 | 85.7/14.3 | 0.225 |
| Type of MS (RR/SP/PP%) | 65/20/15 | 65/15/20 | 0.867 | 100/0/0 a | 0.221 |
| EDSS (0–10) Min—Max | 3.4 ± 1.0 2—5 | 3.7 ± 1.2 2—6 | 0.404 | 3.9 ± 1.1 a | 0.456 |
| Years since diagnosis | 9.6 ± 7.7 | 11.4 ± 9.8 | 0.627 | 12.4 ± 10.1 a | 0.525 |
| Walking aid (yes/no, %) | 35/65 | 15/85 | 0.273 | 16.7/83.3 a | 1.00 |
| MMSE (0–30) | 28.5 ± 1.3 | 28.8 ± 1.2 | 0.478 | 28.8 ± 1.8 a | 0.434 |
| DT Screening list (0–13) | 5.3 ± 2.7 a | 4.1 ± 3.3 | 0.218 | 4.6 ± 2.7 a | 0.949 |
| SRT Long term (0–72) | 40.1 ± 13.5 | 36.1 ± 17.1 | 0.412 | 50.9 ± 9.4 | 0.040 * |
| SRT Consistent (0–72) | 29.8 ± 17.6 | 27.2 ± 17.4 | 0.635 | 38.0 ± 16.8 | 0.075 |
| SRT Delay (0–12) | 8.1 ± 2.8 | 7.9 ± 2.6 | 0.772 | 8.4 ± 3.9 | 0.702 |
| SPART (0–30) | 18.9 ± 6.2 | 18.3 ± 8.2 | 0.779 b | 22.4 ± 5.8 | 0.150 |
| SPART Delay (0–10) | 6.4 ± 2.5 | 6.6 ± 2.5 | 0.904 | 8.3 ± 2.1 | 0.092 |
| WLG (n) | 22.8 ± 5.1 | 23.2 ± 5.2 | 0.854 | 26.3 ± 8.4 | 0.239 |
| Group | Digit Span (mean ± SD) | Subtraction (mean ± SD) | Vigilance (mean ± SD) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Fu | Pre | Post | Fu | Pre | Post | Fu | ||
| Walk DTCmotor (%) | DTT | 13.5 ± 7.6 (n = 18) | 8.6 ± 7.8 (n = 18) | 7.2 ± 10.0 (n = 19) | 17.1 ± 9.5 (n = 18) | 12.9 ± 10.0 (n = 18) | 10.2 ± 7.1 (n = 19) | 7.8 ± 5.6 (n = 17) | 4.4 ± 5.2 (n = 18) | 3.9 ± 7.0 (n = 19) |
| SMT | 12.1 ± 10.5 (n = 19) | 13.4 ± 9.5 (n = 18) | 14.2 ± 8.6 (n = 19) | 14.8 ± 8.3 (n = 18) | 17.4 ± 8.8 (n = 18) | 17.5 ± 9.5 (n = 19) | 9.9 ± 9.7 (n = 19) | 8.7 ± 6.5 (n = 18) | 7.4 ± 6.7 (n = 19) | |
| p-values | T: 0.286 | G: 0.171 | T*G: 0.015 * | T: 0.129 | G: 0.169 | T*G: 0.006* | T: 0.026* | G: 0.090 | T*G: 0.699 | |
| Walk Speed (m/s) | DTT | 0.97 ± 0.23 (n = 19) | 1.09 ± 0.22 (n = 18) | 1.05 ± 0.24 (n = 20) | 0.93 ± 0.23 (n = 19) | 1.04 ± 0.23 (n = 18) | 1.02 ± 0.24 (n = 20) | 1.04 ± 0.25 (n = 18) | 1.14 ± 0.22 (n = 18) | 1.08 ± 0.26 (n = 20) |
| SMT | 0.92 ± 0.26 (n = 20) | 0.97 ± 0.24 (n = 18) | 0.94 ± 0.23 (n = 20) | 0.92 ± 0.25 (n = 18) | 0.92 ± 0.23 (n = 18) | 0.90 ± 0.24 (n = 20) | 0.95 ± 0.26 (n = 20) | 1.02 ± 0.23 (n = 18) | 1.01 ± 0.25 (n = 20) | |
| p-values | T: 0.021* | G: 0.175 | T*G: 0.081 | T: 0.059 | G: 0.158 | T*G: 0.077 | T: 0.019 * | G: 0.200 | T*G: 0.237 | |
| Cup DTCmotor (%) | DTT | 7.7 ± 9.0 (n = 17) | 7.2 ± 9.1 (n = 18) | 4.6 ± 12.6 (n = 19) | 11.2 ± 11.8 (n = 16) | 10.1 ± 8.2 (n = 18) | 7.8 ± 11.7 (n = 18) | 3.3 ± 6.6 (n = 17) | 3.3 ± 8.3 (n = 18) | 2.3 ± 7.4 (n = 19) |
| SMT | 9.7 ± 14.7 (n = 19) | 14.1 ± 9.0 (n = 18) | 13.6 ± 6.3 (n = 19) | 15.2 ± 17.0 (n = 19) | 20.4 ± 10.5 (n = 18) | 18.1 ± 8.0 (n = 19) | 0.5 ± 11.3 (n = 19) | 8.8 ± 8.4 (n = 18) | 8.7 ± 6.5 (n = 19) | |
| p-values | T: 0.675 | G: 0.026 * | T*G: 0.227 | T: 0.501 | G: 0.011 * | T*G: 0.340 | T: 0.033 * | G: 0.126 | T*G: 0.013 * | |
| Cup Speed (m/s) | DTT | 0.93 ± 0.26 (n = 19) | 1.03 ± 0.27 (n = 18) | 1.01 ± 0.29 (n = 20) | 0.88 ± 0.26 (n = 18) | 1.00 ± 0.27 (n = 18) | 0.97 ± 0.28 (n = 19) | 0.97 ± 0.28 (n = 19) | 1.07 ± 0.25 (n = 18) | 1.03 ± 0.26 (n = 20) |
| SMT | 0.88 ± 0.26 (n = 20) | 0.91 ± 0.24 (n = 18) | 0.88 ± 0.26 (n = 20) | 0.82 ± 0.25 (n = 20) | 0.85 ± 0.24 (n = 18) | 0.83 ± 0.26 (n = 20) | 0.96 ± 0.26 (n = 20) | 0.98 ± 0.28 (n = 18) | 0.93 ± 0.27 (n = 20) | |
| p-values | T: 0.126 | G: 0.164 | T*G: 0.115 | T: 0.113 | G: 0.087 | T*G: 0.155 | T: 0.622 | G: 0.347 | T*G: 0.101 | |
| Obstacles DTCmotor (%) | DTT | 9.9 ± 9.9 (n = 17) | 4.0 ± 7.7 (n=18) | 4.7 ± 10.0 (n = 18) | 10.2 ± 7.4 (n = 17) | 7.3 ± 8.5 (n = 18) | 6.8 ± 9.4 (n = 19) | 3.5 ± 9.5 (n = 18) | −0.1 ± 5.1 (n = 18) | 1.4 ± 8.1 (n = 19) |
| SMT | 8.7 ± 7.9 (n = 19) | 10.7 ± 11.5 (n = 18) | 9.2 ± 7.8 (n = 19) | 10.8 ± 10.4 (n = 19) | 14.9 ± 9.3 (n = 18) | 11.8 ± 12.3 (n = 19) | 2.2 ± 6.7 (n = 19) | 6.1 ± 8.8 (n = 18) | 5.1 ± 4.1 (n = 19) | |
| p-values | T: 0.329 | G: 0.189 | T*G: 0.072 | T: 0.576 | G: 0.090 | T*G: 0.211 | T: 0.957 | G: 0.101 | T*G: 0.064 | |
| Obstacles Speed (m/s) | DTT | 0.81 ± 0.24 (n = 18) | 0.95 ± 0.22 (n = 18) | 0.92 ± 0.24 (n = 19) | 0.79 ± 0.21 (n = 18) | 0.92 ± 0.23 (n = 18) | 0.89 ± 0.24 (n = 20) | 0.86 ± 0.26 (n = 19) | 0.99 ± 0.23 (n = 18) | 0.94 ± 0.25 (n = 20) |
| SMT | 0.79 ± 0.26 (n = 20) | 0.82 ± 0.22 (n = 18) | 0.80 ± 0.23 (n = 19) | 0.77 ± 0.24 (n = 20) | 0.78 ± 0.22 (n = 18) | 0.75 ± 0.24 (n = 20) | 0.85 ± 0.25 (n = 20) | 0.86 ± 0.23 (n = 18) | 0.82 ± 0.24 (n = 20) | |
| p-values | T: 0.017* | G: 0.162 | T*G: 0.004* | T: 0.156 | G: 0.100 | T*G: 0.031* | T: 0.105 | G: 0.179 | T*G: 0.006 * | |
| DTCmotor (%) | Effect of | Post-hoc analysis p-values a | ||
| Walk-Digit Span | Time*Group | DTTPRE-POST: 0.022 SMTPRE-POST: - PREDTT-SMT: - | DTTPRE-FU: 0.003 $ SMTPRE-FU: - POSTDTT-SMT: - | DTTPOST-FU: - SMTPOST-FU: - FUDTT-SMT: 0.019 |
| Walk-Subtraction | Time*Group | DTTPRE-POST: 0.024 SMTPRE-POST: - PREDTT-SMT: - | DTTPRE-FU: <0.001 $ SMTPRE-FU: - POSTDTT-SMT: - | DTTPOST-FU: - SMTPOST-FU: - FUDTT-SMT: 0.017 |
| Walk-Vigilance | Time | PRE-POST: 0.043 | PRE-FU: 0.010 $ | POST-FU: - |
| Cup-Digit Span | Group | PREDTT-SMT: - | POSTDTT-SMT: 0.042 $ | FUDTT-SMT: 0.011 $ |
| Cup-Subtraction | Group | PREDTT-SMT: - | POSTDTT-SMT: 0.009 $ | FUDTT-SMT: 0.010 $ |
| Cup-Vigilance | Time*Group | DTTPRE-POST: - SMTPRE-POST:<0.001 $ PREDTT-SMT: - | DTTPRE-FU: - SMTPRE-FU: <0.001 $ POSTDTT-SMT: 0.043 | DTTPOST-FU: - SMTPOST-FU: - FUDTT-SMT: 0.021 |
| DT gait speed (m/s) | Effect of | Post-hoc analysis p-values a | ||
| Walk-Digit Span | Time | PRE-POST: 0.009 $ | PRE-FU: 0.034 | POST-FU: - |
| Walk-Vigilance | Time | PRE-POST: 0.013 $ | PRE-FU: 0.017 $ | POST-FU: - |
| Obstacles-Digit Span | Time*Group | DTTPRE-POST: <0.001 $ SMTPRE-POST: - PREDTT-SMT: - | DTTPRE-FU: 0.002 $ SMTPRE-FU: - POSTDTT-SMT: 0.040 | DTTPOST-FU: - SMTPOST-FU: - FUDTT-SMT: - |
| Obstacles-Subtraction | Time*Group | DTTPRE-POST: 0.003 $ SMTPRE-POST: - PREDTT-SMT: - | DTTPRE-FU: 0.023 SMTPRE-FU: - POSTDTT-SMT: 0.033 | DTTPOST-FU: - SMTPOST-FU: - FUDTT-SMT: 0.069 |
| Obstacles-Vigilance | Time*Group | DTTPRE-POST: <0.001 $ SMTPRE-POST: - PREDTT-SMT: - | DTTPRE-FU: 0.026 SMTPRE-FU: - POSTDTT-SMT: 0.054 | DTTPOST-FU: - SMTPOST-FU: - FUDTT-SMT: - |
| Dtt | Smt | p-value | Multiple Comparisons p-value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Fu | Pre | Post | Fu | Time a | Pre-post | Pre-fu | Post-fu | |
| Mobility (mean ± SD) | ||||||||||
| T25FW (s) | 6.2 ± 1.5 | 5.3 ± 1.2 | 5.5 ± 1.4 | 6.4 ± 2.6 | 6.0 ± 2.5 | 5.7 ± 1.8 | 0.006 * | 0.010 $ | 0.003 $ | 0.649 |
| TUG (s) | 8.6 ± 2.2 | 7.6 ± 1.7 | 8.3 ± 2.6 | 8.8 ± 3.3 | 8.0 ± 2.7 | 8.5 ± 2.8 | 0.004 * | 0.001 $ | 0.204 | 0.036 |
| MSWS-12 (0–100) | 37.6 ± 21.4 | 36.6 ± 23.0 | 32.2 ± 22.2 | 40.7 ± 23.9 | 30.8 ± 26.6 | 34.0 ± 29.3 | 0.033 * | 0.031 | 0.018 | 0.846 |
| DGI (0–24) | 19.2 ± 4.3 | 21.1 ± 2.6 | 21.9 ± 2.1 | 20.3 ± 3.2 | 21.4 ± 3.5 | 21.7 ± 2.9 | <0.001 * | <0.001 $ | <0.001 $ | 0.129 |
| FES-I (16–64) | 30.9 ± 11.7 | 28.2 ± 8.6 | 27.7 ± 9.0 | 28.3 ± 9.5 | 26.8 ± 9.4 | 29.1 ± 10.6 | 0.224 | |||
| 2MWT (m) | 144.1 ± 42.1 | 157.0± 33.6 | 150.4± 45.6 | 141.1± 37.1 | 147.9± 40.3 | 143.9± 39.4 | 0.033 * | 0.010 $ | 0.135 | 0.247 |
| Cognitive (mean ± SD) | ||||||||||
| SDMT (0–110) | 46.8 ± 11.6 | 48.8 ± 14.7 | 46.0 ± 14.7 | 44.7 ± 12.2 | 48.2 ± 10.5 | 45.5 ± 10.3 | 0.023 * | 0.017 $ | 1.00 | 0.017 $ |
| PASAT-3s (0–60) | 42.2 ± 12.8 | 47.4 ± 12.0 | 48.2 ± 12.4 | 46.9 ± 9.8 | 49.4 ± 7.7 | 49.2 ± 12.4 | <0.001 * | 0.001 $ | <0.001 $ | 0.927 |
| PASAT-2s (0–60) | 34.0 ± 12.1 | 37.7 ± 12.6 | 40.2 ± 12.5 | 40.0 ± 11.5 | 41.0 ± 11.7 | 41.6 ± 11.6 | 0.078 | - | ||
| Patient-reported (mean ± SD) | ||||||||||
| DTQ (0–40) | 13.8 ± 8.7 | 11.8 ± 6.8 | 12.5 ± 9.0 | 13.0 ± 9.1 | 11.8 ± 6.9 | 12.15 ± 7.6 | 0.154 | - | ||
| MSIS-29 Phys (0–100) | 30.4 ± 21.9 | 27.6 ± 18.6 | 26.4 ± 20.7 | 26.0 ± 17.8 | 22.9 ± 16.8 | 24.6 ± 19.2 | 0.106 | |||
| MSIS-29 Psycho (0–100) | 29.7 ± 21.3 | 28.5 ± 23.4 | 28.9 ± 23.6 | 33.2 ± 24.3 | 29.0 ± 21.7 | 31.5 ± 20.3 | 0.416 | |||
| MFIS Total (0–84) | 35.5 ± 19.0 | 34.7 ± 20.4 | 34.5 ± 20.3 | 29.8 ± 19.1 | 27.8 ± 18.7 | 28.0 ± 18.2 | 0.403 | |||
| MFIS Phys (0–36) | 17.1 ± 8.5 | 16.8 ± 9.0 | 16.6 ± 9.8 | 14.5 ± 8.6 | 13.8 ± 8.5 | 13.9 ± 8.9 | 0.739 | |||
| MFIS Psycho (0–8) | 3.1 ± 2.4 | 3.0 ± 2.6 | 3.2 ± 2.6 | 2.2 ± 2.3 | 2.2 ± 2.2 | 2.0 ± 2.2 | 0.805 | |||
| MFIS Cognitive (0–40) | 15.4 ± 10.9 | 14.8 ± 10.5 | 14.8 ± 9.9 | 13.2 ± 9.8 | 11.9 ± 9.7 | 12.2 ± 9.1 | 0.247 | |||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Veldkamp, R.; Baert, I.; Kalron, A.; Tacchino, A.; D’hooge, M.; Vanzeir, E.; Van Geel, F.; Raats, J.; Goetschalckx, M.; Brichetto, G.; et al. Structured Cognitive-Motor Dual Task Training Compared to Single Mobility Training in Persons with Multiple Sclerosis, a Multicenter RCT. J. Clin. Med. 2019, 8, 2177. https://doi.org/10.3390/jcm8122177
Veldkamp R, Baert I, Kalron A, Tacchino A, D’hooge M, Vanzeir E, Van Geel F, Raats J, Goetschalckx M, Brichetto G, et al. Structured Cognitive-Motor Dual Task Training Compared to Single Mobility Training in Persons with Multiple Sclerosis, a Multicenter RCT. Journal of Clinical Medicine. 2019; 8(12):2177. https://doi.org/10.3390/jcm8122177
Chicago/Turabian StyleVeldkamp, Renee, Ilse Baert, Alon Kalron, Andrea Tacchino, Mieke D’hooge, Ellen Vanzeir, Fanny Van Geel, Joke Raats, Mieke Goetschalckx, Giampaolo Brichetto, and et al. 2019. "Structured Cognitive-Motor Dual Task Training Compared to Single Mobility Training in Persons with Multiple Sclerosis, a Multicenter RCT" Journal of Clinical Medicine 8, no. 12: 2177. https://doi.org/10.3390/jcm8122177
APA StyleVeldkamp, R., Baert, I., Kalron, A., Tacchino, A., D’hooge, M., Vanzeir, E., Van Geel, F., Raats, J., Goetschalckx, M., Brichetto, G., Shalmoni, N., Hellinckx, P., De Weerdt, N., De Wilde, D., & Feys, P. (2019). Structured Cognitive-Motor Dual Task Training Compared to Single Mobility Training in Persons with Multiple Sclerosis, a Multicenter RCT. Journal of Clinical Medicine, 8(12), 2177. https://doi.org/10.3390/jcm8122177






