Anxiety and Depression in Patients with Obstructive Sleep Apnoea before and after Continuous Positive Airway Pressure: The ADIPOSA Study
Abstract
1. Introduction
2. Experimental Section
2.1. Study Protocol and Participant’s Enrolment
2.2. Procedures
2.2.1. Overnight Sleep Study
2.2.2. Daytime Sleepiness, Depression and Anxiety
2.3. CPAP Usage
2.4. Sample Size Calculation
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Senaratna, C.V.; Perret, J.L.; Lodge, C.J.; Lowe, A.J.; Campbell, B.E.; Matheson, M.C.; Hamilton, G.S.; Dharmage, S.C. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med. Rev. 2017, 34, 70–81. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 15 October 2019).
- Carneiro-Barrera, A.; Díaz-Román, A.; Guillén-Riquelme, A.; Buela-Casal, G. Weight loss and lifestyle interventions for obstructive sleep apnoea in adults: Systematic review and meta-analysis. Obes. Rev. 2019, 20, 750–762. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.S.; McSharry, D.G.; Malhotra, A. Adult obstructive sleep apnoea. Lancet 2014, 383, 736–747. [Google Scholar] [CrossRef]
- Chopra, S.; Rathore, A.; Younas, H.; Pham, L.V.; Gu, C.; Beselman, A.; Kim, I.Y.; Wolfe, R.R.; Perin, J.; Polotsky, V.Y.; et al. Obstructive sleep apnea dynamically increases nocturnal plasma free fatty acids, glucose, and cortisol during sleep. J. Clin. Endocrinol. Metab. 2017, 102, 3172–3181. [Google Scholar] [CrossRef]
- Hoyos, C.M.; Drager, L.F.; Patel, S.R. OSA and cardiometabolic risk: What’s the bottom line? Respirology 2017, 22, 420–429. [Google Scholar] [CrossRef]
- Aurora, R.N.; Punjabi, N.M. Obstructive sleep apnoea and type 2 diabetes mellitus: A bidirectional association. Lancet Respir. Med. 2013, 1, 329–338. [Google Scholar] [CrossRef]
- Holingue, C.; Wennberg, A.; Berger, S.; Polotsky, V.Y.; Spira, A.P. Disturbed sleep and diabetes: A potential nexus of dementia risk. Metabolism 2018, 84, 85–93. [Google Scholar] [CrossRef]
- Bradley, T.D.; Floras, J.S. Obstructive sleep apnoea and its cardiovascular consequences. Lancet 2009, 373, 82–93. [Google Scholar] [CrossRef]
- Jackson, M.L.; McEvoy, R.D.; Banks, S.; Barnes, M. Neurobehavioral impairment and CPAP treatment response in mild-moderate obstructive sleep apnea. J. Clin. Sleep Med. 2018, 14, 47–56. [Google Scholar] [CrossRef]
- Rezaeitalab, F.; Moharrari, F.; Saberi, S.; Asadpour, H.; Rezaeetalab, F. The correlation of anxiety and depression with obstructive sleep apnea syndrome. J. Res. Med. Sci. 2014, 19, 205–210. [Google Scholar]
- Fu, Y.; Xia, Y.; Yi, H.; Xu, H.; Guan, J.; Yin, S. Meta-analysis of all-cause and cardiovascular mortality in obstructive sleep apnea with or without continuous positive airway pressure treatment. Sleep Breath. 2017, 21, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Tregear, S.; Reston, J.; Schoelles, K.; Phillips, B. Obstructive sleep apnea and risk of motor vehicle crash: Systematic review and meta-analysis. J. Clin. Sleep Med. 2009, 5, 573–581. [Google Scholar] [PubMed]
- Jurado-Gámez, B.; Guglielmi, O.; Gude, F.; Buela-Casal, G. Workplace accidents, absenteeism and productivity in patients with sleep apnea. Arch. Bronconeumol. 2015, 51, 213–218. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Sleep Medicine. International Classification of Sleep Disorders, 3rd ed.; American Academy of Sleep Medicine: Darien, IL, USA, 2014. [Google Scholar]
- Sharafkhaneh, A.; Giray, N.; Richardson, P.; Young, T.; Hirshkowitz, M. Association of psychiatric disorders and sleep apnea in a large cohort. Sleep 2005, 28, 1405–1411. [Google Scholar] [CrossRef]
- Ohayon, M.M. The effects of breathing-related sleep disorders on mood disturbances in the general population. J. Clin. Psychiatry 2003, 64, 1195–1200. [Google Scholar] [CrossRef]
- Douglas, N.; Young, A.; Roebuck, T.; Ho, S.; Miller, B.R.; Kee, K.; Dabscheck, E.J.; Naughton, M.T. Prevalence of depression in patients referred with snoring and obstructive sleep apnoea. Intern. Med. J. 2013, 43, 630–634. [Google Scholar] [CrossRef]
- Scott, K.M. Depression, anxiety and incident cardiometabolic diseases. Curr. Opin. Psychiatry 2014, 27, 289–293. [Google Scholar] [CrossRef]
- Kjelsberg, F.N.; Ruud, E.A.; Stavem, K. Predictors of symptoms of anxiety and depression in obstructive sleep apnea. Sleep Med. 2005, 6, 341–346. [Google Scholar] [CrossRef]
- Knechtle, B.; Economou, N.T.; Nikolaidis, P.T.; Velentza, L.; Kallianos, A.; Steiropoulos, P.; Koutsompolis, D.; Rosemann, T.; Trakada, G. Clinical characteristics of obstructive sleep apnea in psychiatric disease. J. Clin. Med. 2019, 8, 534. [Google Scholar] [CrossRef]
- Epstein, L.J.; Kristo, D.; Strollo, P.J.; Friedman, N.; Malhotra, A.; Patil, S.P.; Ramar, K.; Rogers, R.; Schwab, R.J.; Weaver, E.M.; et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J. Clin. Sleep Med. 2009, 5, 263–276. [Google Scholar]
- Shokoueinejad, M.; Fernandez, C.; Carroll, E.; Wang, F.; Levin, J.; Rusk, S.; Glattard, N.; Mulchrone, A.; Zhang, X.; Xie, A.; et al. Sleep apnea: A review of diagnostic sensors, algorithms, and therapies. Physiol. Meas. 2017, 38, R204–R252. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, A.I.; Martínez, P.; Miró, E.; Bardwell, W.A.; Buela-Casal, G. CPAP and behavioral therapies in patients with obstructive sleep apnea: Effects on daytime sleepiness, mood, and cognitive function. Sleep Med. Rev. 2009, 13, 223–233. [Google Scholar] [CrossRef] [PubMed]
- Jurado-Gámez, B.; Guglielmi, O.; Gude-Sampedro, F.; Buela-Casal, G. Effect of CPAP therapy on job productivity and psychosocial occupational health in patients with moderate to severe sleep apnea. Sleep Breath. 2015, 19, 1293–1299. [Google Scholar] [CrossRef] [PubMed]
- Jurado-Gámez, B.; Guglielmi, O.; Gude, F.; Buela-Casal, G. Effects of continuous positive airway pressure treatment on cognitive functions in patients with severe obstructive sleep apnoea. Neurologia 2016, 31, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.Y.; Wang, R.; Gleason, K.J.; Lewis, E.F.; Quan, S.F.; Toth, C.M.; Morrical, M.; Rueschman, M.; Weng, J.; Ware, J.H.; et al. Effect of continuous positive airway pressure treatment on health-related quality of life and sleepiness in high cardiovascular risk individuals with sleep apnea: Best apnea interventions for research (Best AIR) trial. Sleep 2017, 40, zsx040. [Google Scholar] [CrossRef] [PubMed]
- Loube, D.I.; Loube, A.A.; Erman, M.K. Continuous positive airway pressure treatment results in weight less in obese and overweight patients with obstructive sleep apnea. J. Am. Diet Assoc. 1997, 97, 896–897. [Google Scholar] [CrossRef]
- Redenius, R.; Murphy, C.; O’Neill, E.; Al-Hamwi, M.; Zallek, S.N. Does CPAP lead to change in BMI? J. Clin. Sleep Med. 2008, 4, 205–209. [Google Scholar]
- Drager, L.F.; Brunoni, A.R.; Jenner, R.; Lorenzi-Filho, G.; Bensenor, I.M.; Lotufo, P.A. Effects of CPAP on body weight in patients with obstructive sleep apnoea: A meta-analysis of randomised trials. Thorax 2015, 70, 258–264. [Google Scholar] [CrossRef]
- Shechter, A.; Airo, M.; Valentin, J.; Dugas, N.C.; Abdalla, M.; St-Onge, M.P.; Louh, I.K. Effects of continuous positive airway pressure on body composition in individuals with obstructive sleep apnea: A non-randomized, matched before-after study. J. Clin. Med. 2019, 8, 1195. [Google Scholar] [CrossRef]
- Morgenthaler, T.I.; Kapen, S.; Lee-Chiong, T.; Alessi, C.; Boehlecke, B.; Brown, T.; Coleman, J.; Friedman, L.; Kapur, V.; Owens, J.; et al. Practice parameters for the medical therapy of obstructive sleep apnea. Sleep 2006, 29, 1031–1035. [Google Scholar]
- Carneiro-Barrera, A.; Amaro-Gahete, F.J.; Díaz-Román, A.; Guillén-Riquelme, A.; Jurado-Fasoli, L.; Sáez-Roca, G.; Martín-Carrasco, C.; Ruiz, J.R.; Buela-Casal, G. Interdisciplinary weight loss and lifestyle intervention for obstructive sleep apnoea in adults: Rationale, design and methodology of the INTERAPNEA study. Nutrients 2019, 11, 2227. [Google Scholar] [CrossRef] [PubMed]
- Harris, M.; Glozier, N.; Ratnavadivel, R.; Grunstein, R.R. Obstructive sleep apnea and depression. Sleep Med. Rev. 2009, 13, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, A.I.; Buela-Casal, G.; Bermúdez, M.P.; Casas-Maldonado, F. The effects of continuous positive air pressure treatment on anxiety and depression levels in apnea patients. Psychiatry Clin. Neurosci. 2001, 55, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Bucks, R.S.; Nanthakumar, S.; Starkstein, S.S.; Hillman, D.R.; James, A.; McArdle, N.; Hatch, K.; Skinner, T.C. Discerning depressive symptoms in patients with obstructive sleep apnea: The effect of continuous positive airway pressure therapy on Hamilton Depression Rating Scale symptoms. Sleep 2018, 41, zsy178. [Google Scholar] [CrossRef] [PubMed]
- Bhat, S.; Gupta, D.; Akel, O.; Polos, P.G.; DeBari, V.A.; Akhtar, S.; McIntyre, A.; Ming, S.X.; Upadhyay, H.; Chokroverty, S. The relationships between improvements in daytime sleepiness, fatigue and depression and psychomotor vigilance task testing with CPAP use in patients with obstructive sleep apnea. Sleep Med. 2018, 49, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Campos-Rodriguez, F.; Asensio-Cruz, M.I.; Cordero-Guevara, J.; Jurado-Gamez, B.; Carmona-Bernal, C.; Gonzalez-Martinez, M.; Troncoso, M.F.; Sanchez-Lopez, V.; Arellano-Orden, E.; Garcia-Sanchez, M.I.; et al. Effect of continuous positive airway pressure on inflammatory, antioxidant, and depression biomarkers in women with obstructive sleep apnea: A randomized controlled trial. Sleep 2019, 42, zsz145. [Google Scholar] [CrossRef]
- Haensel, A.; Norman, D.; Natarajan, L.; Bardwell, W.A.; Ancoli-Israel, S.; Dimsdale, J.E. Effect of a 2 week CPAP treatment on mood states in patients with obstructive sleep apnea: A double-blind trial. Sleep Breath. 2007, 11, 239–244. [Google Scholar] [CrossRef]
- Gagnadoux, F.; Le Vaillant, M.; Goupil, F.; Pigeanne, T.; Chollet, S.; Masson, P.; Bizieux-Thaminy, A.; Humeau, M.P.; Meslier, N. Depressive symptoms before and after long-term CPAP therapy in patients with sleep apnea. Chest 2014, 145, 1025–1031. [Google Scholar] [CrossRef]
- Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 56–62. [Google Scholar] [CrossRef]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef]
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An inventory for measuring clinical anxiety: Psychometric properties. J. Consult. Clin. Psychol. 1988, 56, 893–897. [Google Scholar] [CrossRef] [PubMed]
- Kapur, V.K.; Auckley, D.H.; Chowdhuri, S.; Kuhlmann, D.C.; Mehra, R.; Ramar, K.; Harrod, C.G. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2017, 13, 479–504. [Google Scholar] [CrossRef] [PubMed]
- Masa, J.F.; Corral, J.; Pereira, R.; Duran-Cantolla, J.; Cabello, M.; Hernández-Blasco, L.; Monasterio, C.; Alonso, A.; Chiner, E.; Rubio, M.; et al. Effectiveness of home respiratory polygraphy for the diagnosis of sleep apnoea and hypopnoea syndrome. Thorax 2011, 66, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Berry, R.B.; Budhiraja, R.; Gottlieb, D.J.; Gozal, D.; Iber, C.; Kapur, V.K.; Marcus, C.L.; Mehra, R.; Parthasarathy, S.; Quan, S.F.; et al. Rules for scoring respiratory events in sleep: Update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American Academy of Sleep Medicine. J. Clin. Sleep Med. 2012, 8, 597–619. [Google Scholar] [CrossRef] [PubMed]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef]
- Chiner, E.; Arriero, J.M.; Signes-Costa, J.; Marco, J.; Fuentes, I. Validation of the Spanish version of the Epworth Sleepiness Scale in patients with a sleep apnea syndrome. Arch. Bronconeumol. 1999, 35, 422–427. [Google Scholar] [CrossRef]
- Beck, A.T.; Guth, D.; Steer, R.A.; Ball, R. Screening for major depression disorders in medical inpatients with the Beck Depression Inventory for Primary Care. Behav. Res. Ther. 1997, 35, 785–791. [Google Scholar] [CrossRef]
- Sanz, J.; Izquierdo, A.; García-Vera, M.P. Departamento de I+D Pearson Clinical & Talent Assessment. In BDI-FS, Inventario de Depresión de Beck Para Pacientes Médicos; Pearson: Madrid, Spain, 2011. [Google Scholar]
- Spielberger, C.D.; Agudelo, D.; Buela-Casal, G. Inventario de Depresión Estado/Rasgo (IDER); TEA Ediciones: Madrid, Spain, 2008. [Google Scholar]
- Law, M.; Naughton, M.T.; Dhar, A.; Barton, D.; Dabscheck, E. Validation of two depression screening instruments in a sleep disorders clinic. J. Clin. Sleep Med. 2014, 10, 683–688. [Google Scholar] [CrossRef]
- Poole, H.; Bramwell, R.; Murphy, P. The utility of the Beck Depression Inventory Fast Screen (BDI-FS) in a pain clinic population. Eur. J. Pain 2009, 13, 865–869. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gorsuch, R.; Lushene, R. Manual for the State-Trait Anxiety Inventory; Consulting Psychologist Press: Palo Alto, CA, USA, 1970. [Google Scholar]
- Buela-Casal, G.; Guillén-Riquelme, A.; Seisdedos-Cubero, N. Cuestionario de Ansiedad Estado-Rasgo: Adaptación española, 9th ed.; TEA Ediciones: Madrid, Spain, 2016. [Google Scholar]
- Polysomnography Task Force; American Sleep Disorders Association Standards of Practice Committee. Practice parameters for the indications for polysomnography and related procedures. Sleep 1997, 20, 406–422. [Google Scholar] [CrossRef]
- Shaffer, M.L.; Chinchilli, V.M. Including multiple imputation in a sensitivity analysis for clinical trials with treatment failures. Contemp. Clin. Trials 2007, 28, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Morris, S.B. Distribution of the standardized mean change effect size for meta-analysis on repeated measures. Br. J. Math. Stat. Psychol. 2000, 53, 17–29. [Google Scholar] [CrossRef] [PubMed]
- Nanthakumar, S.; Bucks, R.S.; Skinner, T.C. Are we overestimating the prevalence of depression in chronic illness using questionnaires? Meta-analytic evidence in obstructive sleep apnoea. Health Psychol. 2016, 35, 423–432. [Google Scholar] [CrossRef] [PubMed]
- Watson, D.; Clark, L.A.; Carey, G. Positive and negative affectivity and their relation to anxiety and depressive disorders. J. Abnorm. Psychol. 1988, 97, 346–353. [Google Scholar] [CrossRef]
- Copur, A.S.; Erik Everhart, D.; Zhang, C.; Chen, Z.; Shekhani, H.; Mathevosian, S.; Loveless, J.; Watson, E.; Kadri, I.; Wallace, L.; et al. Effect of personality traits on adherence with positive airway pressure therapy in obstructive sleep apnea patients. Sleep Breath. 2018, 22, 369–376. [Google Scholar] [CrossRef]
- Schenk, H.M.; Jeronimus, B.F.; van der Krieke, L.; Bos, E.H.; de Jonge, P.; Rosmalen, J.G.M. Associations of positive affect and negative affect with allostatic load: A lifelines cohort study. Psychosom. Med. 2018, 80, 160–166. [Google Scholar] [CrossRef]
- Steptoe, A.; O’Donnell, K.; Badrick, E.; Kumari, M.; Marmot, M. Neuroendocrine and inflammatory factors associated with positive affect in healthy men and women: The Whitehall II study. Am. J. Epidemiol. 2008, 167, 96–102. [Google Scholar] [CrossRef]
- Steptoe, A.; Gibson, E.L.; Hamer, M.; Wardle, J. Neuroendocrine and cardiovascular correlates of positive affect measured by ecological momentary assessment and by questionnaire. Psychoneuroendocrinology 2007, 32, 56–64. [Google Scholar] [CrossRef]
- Mehra, R.; Teodorescu, M. Sleep, circadian disruption, and microbial-immune interactions: A new frontier. Chest 2018, 154, 740–742. [Google Scholar] [CrossRef]
- Juster, R.P.; McEwen, B.S.; Lupien, S.J. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci. Biobehav. Rev. 2010, 35, 2–16. [Google Scholar] [CrossRef]
- Aloia, M.S.; Arnedt, J.T.; Smith, L.; Skrekas, J.; Stanchina, M.; Millman, R.P. Examining the construct of depression in obstructive sleep apnea syndrome. Sleep Med. 2005, 6, 115–121. [Google Scholar] [CrossRef]
- Kawahara, S.; Akashiba, T.; Akahoshi, T.; Horie, T. Nasal CPAP improves the quality of life and lessens the depressive symptoms in patients with obstructive sleep apnea syndrome. Intern. Med. 2005, 44, 422–427. [Google Scholar] [CrossRef]
- Garbarino, S.; Bardwell, W.A.; Guglielmi, O.; Chiorri, C.; Bonanni, E.; Magnavita, N. Association of anxiety and depression in obstructive sleep apnea patients: A systematic review and meta-analysis. Behav. Sleep Med. 2018, 19, 1–23. [Google Scholar] [CrossRef]
- Moussavi, S.; Chatterji, S.; Verdes, E.; Tandon, A.; Patel, V.; Ustun, B. Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. Lancet 2007, 370, 851–858. [Google Scholar] [CrossRef]
- Wersebe, H.; Lieb, R.; Meyer, A.H.; Miche, M.; Mikoteit, T.; Imboden, C.; Hoyer, J.; Bader, K.; Hatzinger, M.; Gloster, A.T. Well-being in major depression and social phobia with and without comorbidity. Int. J. Clin. Health Psychol. 2018, 18, 201–208. [Google Scholar] [CrossRef]
- Becker, N.B.; de Jesus, S.N.; Viseu, J.N.; Stobäus, C.D.; Guerreiro, M.; Domingues, R.B. Depression and quality of life in older adults: Mediation effect of sleep quality. Int. J. Clin. Health Psychol. 2018, 18, 8–17. [Google Scholar] [CrossRef]
| N | All | N | Men | N | Women | ||||
|---|---|---|---|---|---|---|---|---|---|
| Age (years) | 48 | 54.5 | (13.1) | 33 | 51.0 | (12.0) | 15 | 62.0 | (12.6) * |
| Body mass index (kg/m2) | 48 | 32.8 | (6.8) | 33 | 33.5 | (7.3) | 15 | 31.2 | (5.4) |
| Smokers (n, %) | 48 | 8 | (16.7) | 33 | 7 | (21.2) | 15 | 1 | (6.7) |
| Alcohol consumers (n, %) | 48 | 5 | (10.4) | 33 | 5 | (15.2) | 15 | 0 | (0.0) |
| OSA severity classification | |||||||||
| Moderate OSA (n, %) | 48 | 13 | (27.1) | 33 | 8 | (24.2) | 15 | 5 | (33.3) |
| Severe OSA (n, %) | 48 | 35 | (72.9) | 33 | 25 | (75.8) | 15 | 10 | (66.7) |
| Apnoea-hypopnoea index (n) | 48 | 44.2 | (22.5) | 33 | 47.0 | (23.3) | 15 | 38.0 | (19.9) |
| CPAP use (h) | 48 | 5.7 | (1.8) | 33 | 5.9 | (1.6) | 15 | 5.3 | (2.2) |
| CPAP pressure (mmHg) | 48 | 9.7 | (1.8) | 33 | 9.5 | (2.0) | 15 | 9.9 | (1.2) |
| Epworth questionnaire | |||||||||
| Epworth sleepiness score | 47 | 9.85 | (5.27) | 32 | 9.94 | (5.16) | 15 | 9.67 | (5.69) |
| BDI-FS questionnaire | |||||||||
| BDI-FS score | 48 | 2.92 | (3.05) | 33 | 2.82 | (2.90) | 15 | 3.13 | (3.44) |
| Sadness | 48 | 0.25 | (0.48) | 33 | 0.24 | (0.44) | 15 | 0.27 | (0.59) |
| Pessimism | 48 | 0.50 | (0.74) | 33 | 0.52 | (0.76) | 15 | 0.47 | (0.74) |
| Past failure | 48 | 0.29 | (0.65) | 33 | 0.27 | (0.52) | 15 | 0.33 | (0.9) |
| Loss of pleasure | 48 | 0.54 | (0.74) | 33 | 0.55 | (0.75) | 15 | 0.53 | (0.74) |
| Self-dislike | 48 | 0.48 | (0.83) | 33 | 0.45 | (0.75) | 15 | 0.53 | (0.99) |
| Self-criticalness | 48 | 0.77 | (0.72) | 33 | 0.70 | (0.81) | 15 | 0.93 | (0.46) |
| Suicidal thoughts | 48 | 0.08 | (0.28) | 33 | 0.09 | (0.29) | 15 | 0.07 | (0.26) |
| STAI questionnaire | |||||||||
| STAI-State score | 46 | 20.11 | (12.57) | 31 | 18.03 | (12.82) | 15 | 24.40 | (11.24) |
| STAI-State score percentile a | 46 | 57.50 | (33.90) | 31 | 53.26 | (37.24) | 15 | 66.27 | (24.49) |
| STAI-Trait score | 45 | 21.60 | (11.06) | 30 | 20.97 | (11.81) | 15 | 22.87 | (9.64) |
| STAI-Trait score percentile a | 45 | 51.62 | (32.07) | 30 | 53.50 | (34.37) | 15 | 47.87 | (27.61) |
| IDER questionnaire | |||||||||
| IDER-State score | 48 | 19.56 | (5.67) | 33 | 18.82 | (5.86) | 15 | 21.20 | (5.03) |
| IDER-State score percentile a | 48 | 61.37 | (26.17) | 33 | 58.52 | (28.28) | 15 | 67.67 | (20.25) |
| IDER-State euthymia score | 48 | 12.71 | (3.51) | 33 | 12.21 | (3.60) | 15 | 13.80 | (3.14) |
| IDER-State dysthymia score | 48 | 6.85 | (2.59) | 33 | 6.61 | (2.67) | 15 | 7.40 | (2.38) |
| IDER-Trait score | 48 | 18.42 | (5.62) | 33 | 18.06 | (5.33) | 15 | 19.20 | (6.35) |
| IDER-Trait score percentile a | 48 | 50.21 | (32.09) | 33 | 50.88 | (32.25) | 15 | 48.73 | (32.82) |
| IDER-Trait euthymia score | 48 | 11.46 | (3.99) | 33 | 11.27 | (3.83) | 15 | 11.87 | (4.44) |
| IDER-Trait dysthymia score | 48 | 6.96 | (2.13) | 33 | 6.79 | (1.98) | 15 | 7.33 | (2.47) |
| All (n = 48) | Men (n = 33) | Women (n = 15) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre Mean (SD) | Post Mean (SD) | d (95%CI) | Pre Mean (SD) | Post Mean (SD) | d (95%CI) | Pre Mean (SD) | Post Mean (SD) | d (95%CI) | |
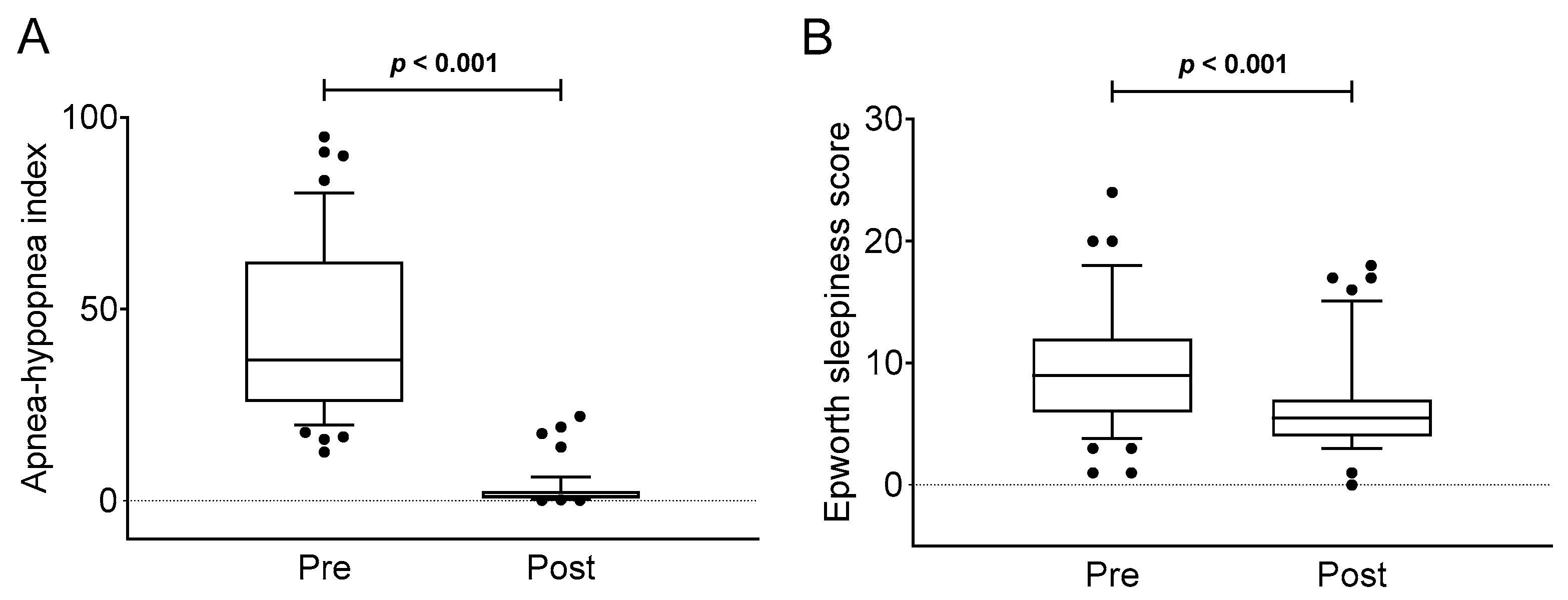
| Apnoea-hypopnoea index (n) | 44.17 (22.51) | 2.78 (4.90) | 1.809 (1.262 to 2.344) | 46.99 (23.35) | 2.49 (4.78) | 1.875 (1.319 to 2.420) | 37.95 (19.89) | 3.41 (5.27) | 1.708 (1.175 to 2.230) |
| Epworth sleepiness score | 9.85 (5.27) | 6.57 (4.14) | 0.612 (0.190 to 1.027) | 9.94 (5.16) | 6.28 (4.46) | 0.699 (0.272 to 1.120) | 9.67 (5.69) | 7.20 (3.41) | 0.427 (0.016 to 0.834) |
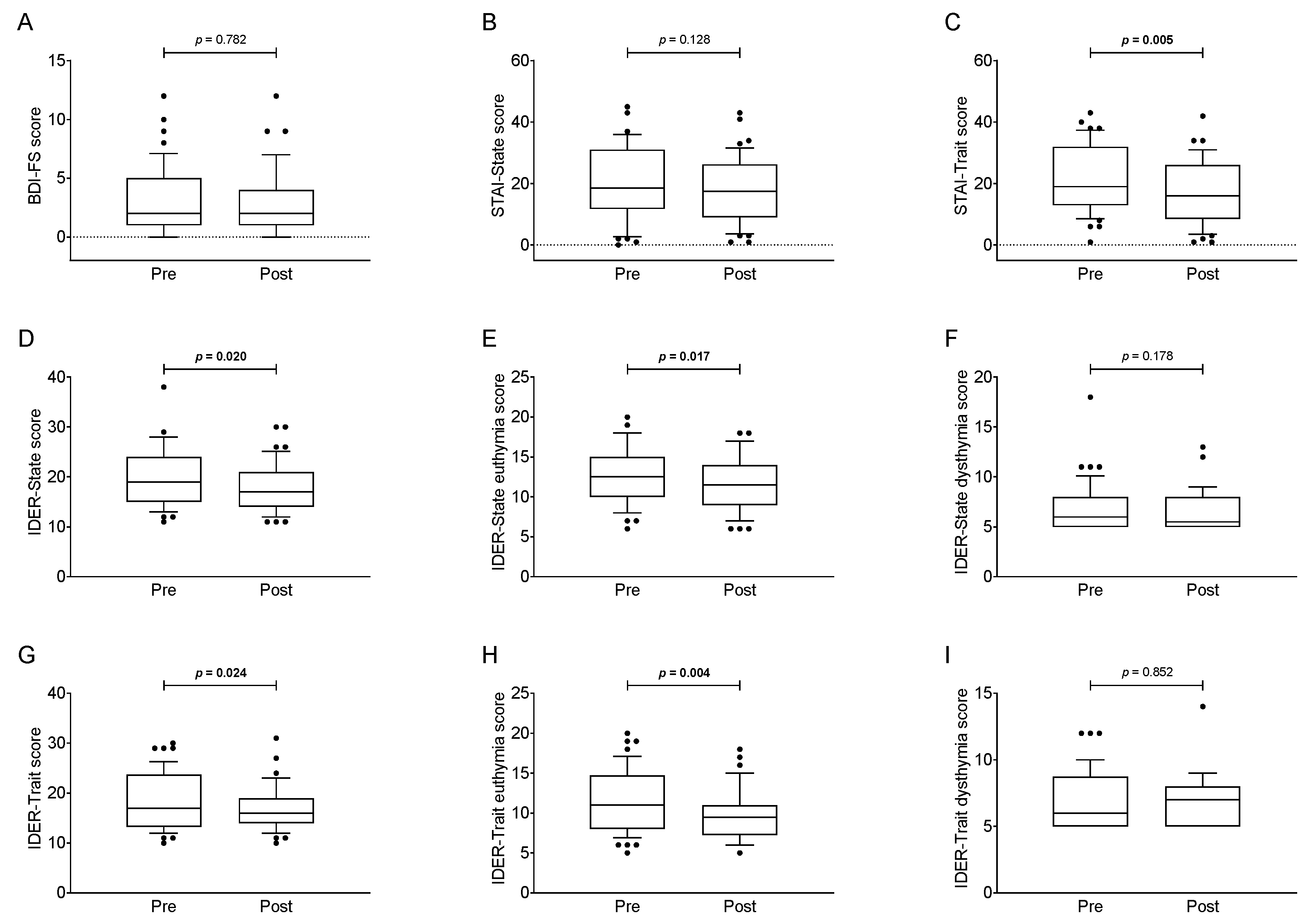
| BDI-FS score | 2.92 (3.05) | 2.79 (2.82) | 0.042 (−0.358 to 0.442) | 2.82 (2.90) | 2.67 (3.12) | 0.051 (−0.349 to 0.451) | 3.13 (3.44) | 3.07 (2.09) | 0.017 (−0.383 to 0.417) |
| STAI-State score | 20.11 (12.57) | 17.80 (10.74) | 0.181 (−0.222 to 0.582) | 18.03 (12.82) | 15.29 (9.98) | 0.21 (−0.193 to 0.611) | 24.40 (11.24) | 23.00 (10.71) | 0.123 (−0.278 to 0.523) |
| STAI-Trait score | 21.60 (11.06) | 16.96 (10.26) | 0.413 (0.002 to 0.820) | 20.97 (11.81) | 14.23 (9.07) | 0.562 (0.143 to 0.975) | 22.87 (9.64) | 22.40 (10.62) | 0.048 (−0.352 to 0.448) |
| IDER-State score | 19.56 (5.67) | 17.98 (4.86) | 0.274 (−0.131 to 0.676) | 18.82 (5.86) | 17.15 (4.79) | 0.281 (−0.125 to 0.684) | 21.20 (5.03) | 19.80 (4.66) | 0.274 (−0.131 to 0.676) |
| IDER-State euthymia score | 12.71 (3.51) | 11.54 (3.34) | 0.328 (−0.079 to 0.732) | 12.21 (3.60) | 10.88 (3.32) | 0.364 (−0.045 to 0.769) | 13.80 (3.14) | 13.00 (2.98) | 0.250 (−0.155 to 0.652) |
| IDER-State dysthymia score | 6.85 (2.59) | 6.44 (1.91) | 0.156 (−0.246 to 0.556) | 6.61 (2.67) | 6.27 (1.79) | 0.125 (−0.276 to 0.525) | 7.40 (2.38) | 6.80 (2.18) | 0.248 (−0.156 to 0.650) |
| IDER-Trait score | 18.42 (5.62) | 16.73 (4.23) | 0.296 (−0.110 to 0.699) | 18.06 (5.33) | 16.55 (4.79) | 0.279 (−0.126 to 0.682) | 19.20 (6.35) | 17.13 (2.72) | 0.321 (−0.086 to 0.725) |
| IDER-Trait euthymia score | 11.46 (3.99) | 9.83 (3.09) | 0.402 (−0.008 to 0.808) | 11.27 (3.83) | 9.76 (3.44) | 0.388 (−0.022 to 0.794) | 11.87 (4.44) | 10.00 (2.24) | 0.415 (0.004 to 0.822) |
| IDER-Trait dysthymia score | 6.96 (2.13) | 6.90 (1.81) | 0.028 (−0.372 to 0.428) | 6.79 (1.98) | 6.79 (1.97) | 0.001 (−0.399 to 0.401) | 7.33 (2.47) | 7.13 (1.46) | 0.080 (−0.321 to 0.480) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carneiro-Barrera, A.; Amaro-Gahete, F.J.; Sáez-Roca, G.; Martín-Carrasco, C.; R. Ruiz, J.; Buela-Casal, G. Anxiety and Depression in Patients with Obstructive Sleep Apnoea before and after Continuous Positive Airway Pressure: The ADIPOSA Study. J. Clin. Med. 2019, 8, 2099. https://doi.org/10.3390/jcm8122099
Carneiro-Barrera A, Amaro-Gahete FJ, Sáez-Roca G, Martín-Carrasco C, R. Ruiz J, Buela-Casal G. Anxiety and Depression in Patients with Obstructive Sleep Apnoea before and after Continuous Positive Airway Pressure: The ADIPOSA Study. Journal of Clinical Medicine. 2019; 8(12):2099. https://doi.org/10.3390/jcm8122099
Chicago/Turabian StyleCarneiro-Barrera, Almudena, Francisco J. Amaro-Gahete, Germán Sáez-Roca, Carlos Martín-Carrasco, Jonatan R. Ruiz, and Gualberto Buela-Casal. 2019. "Anxiety and Depression in Patients with Obstructive Sleep Apnoea before and after Continuous Positive Airway Pressure: The ADIPOSA Study" Journal of Clinical Medicine 8, no. 12: 2099. https://doi.org/10.3390/jcm8122099
APA StyleCarneiro-Barrera, A., Amaro-Gahete, F. J., Sáez-Roca, G., Martín-Carrasco, C., R. Ruiz, J., & Buela-Casal, G. (2019). Anxiety and Depression in Patients with Obstructive Sleep Apnoea before and after Continuous Positive Airway Pressure: The ADIPOSA Study. Journal of Clinical Medicine, 8(12), 2099. https://doi.org/10.3390/jcm8122099






