Evaluation of Concomitant Orbital Floor Fractures in Patients with Head Trauma Using Conventional Head CT Scan: A Retrospective Study at a Level II Trauma Center
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting and Selection of Participants
2.2. Imaging Protocol of CT Scans
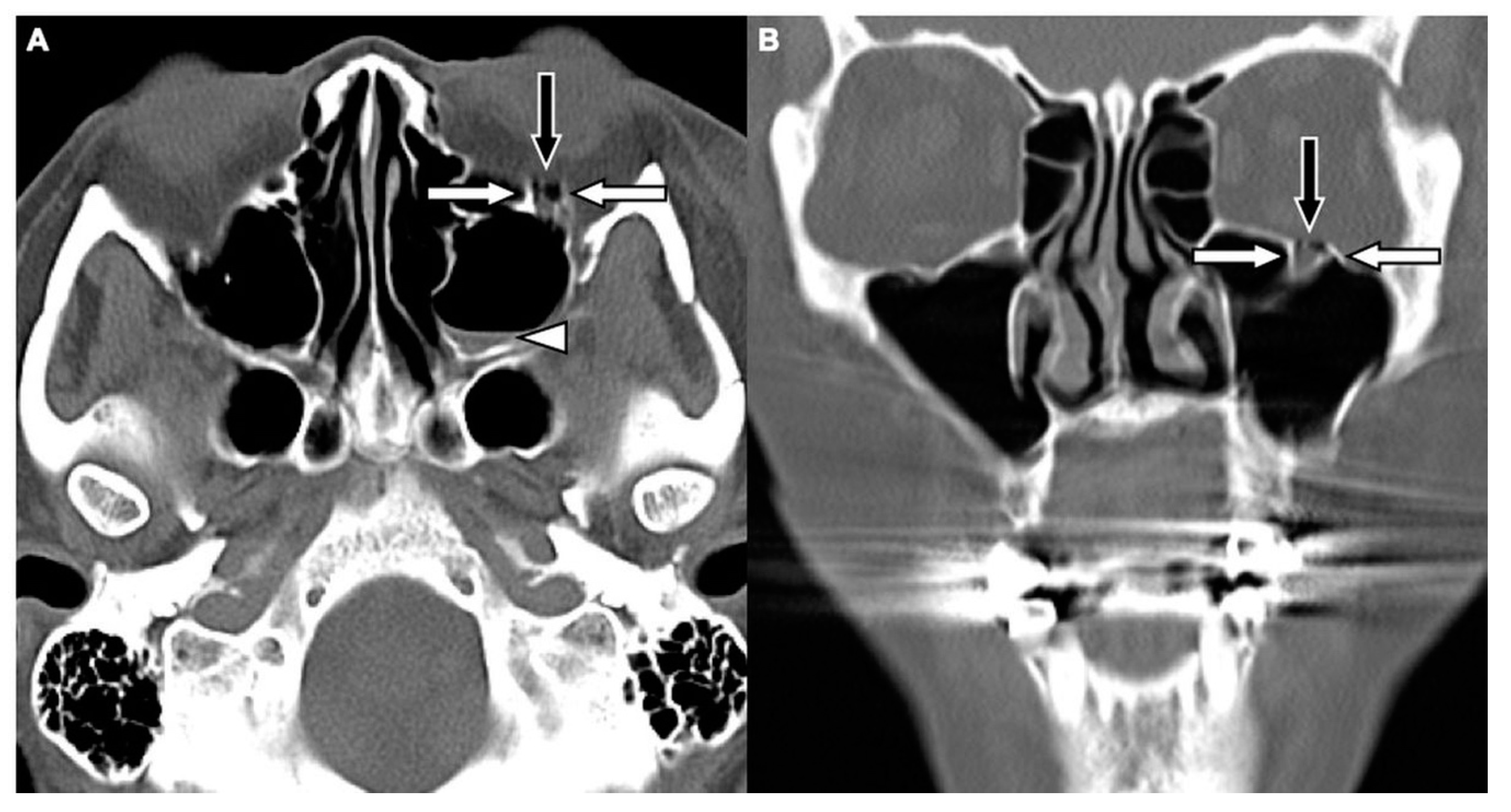
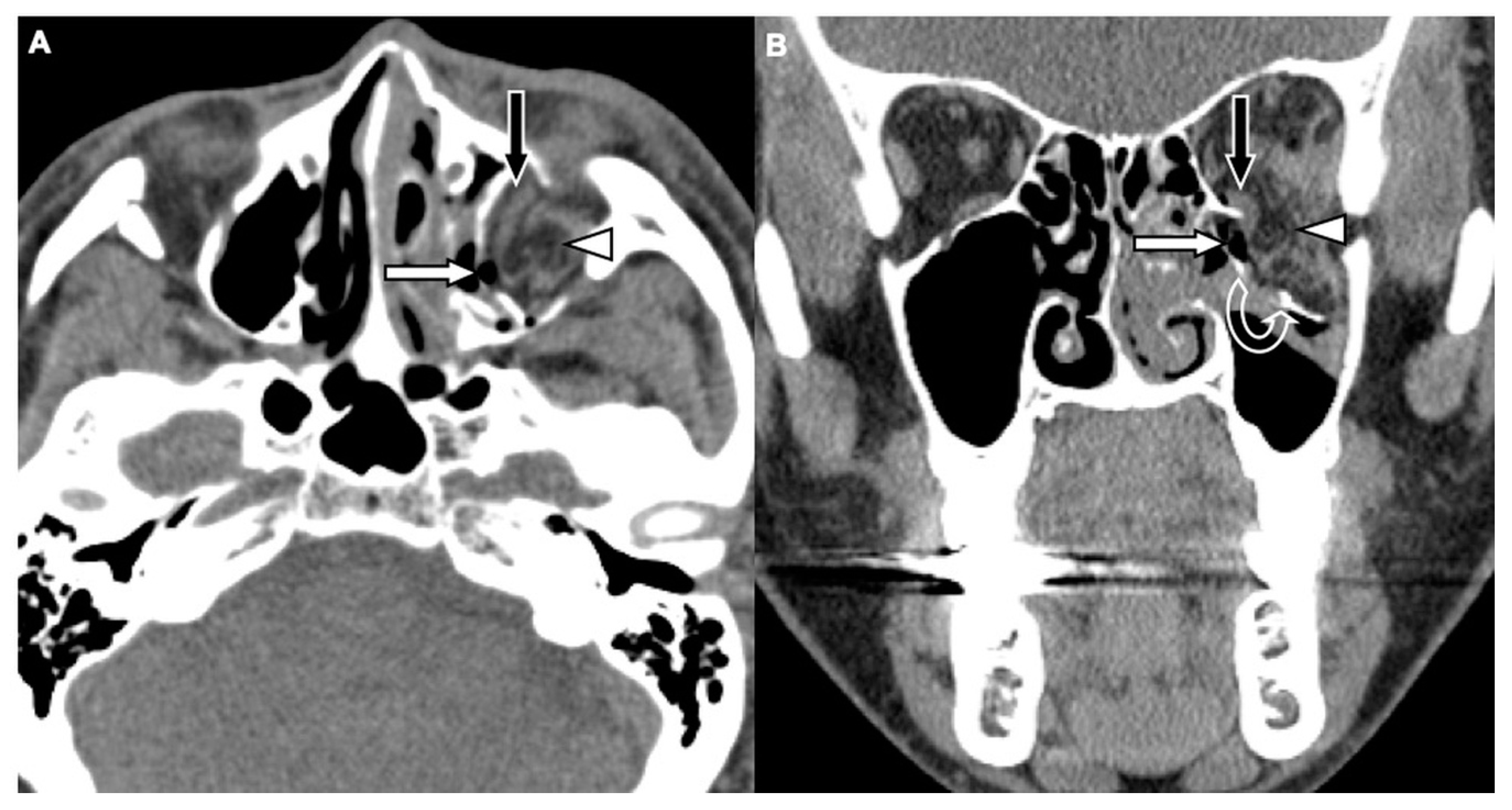
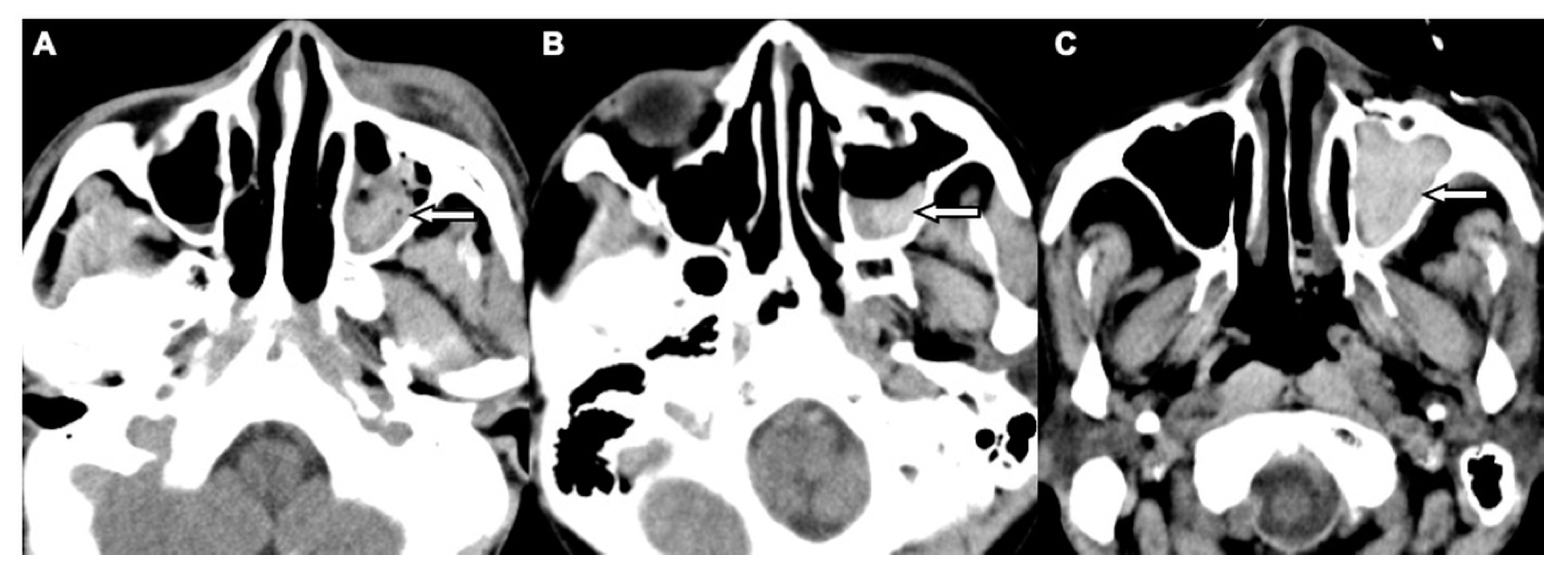
2.3. Image Analysis
2.4. Clinical Data Assessment
2.5. Statistical Analysis
3. Results
3.1. Comparison of Patients with and without OFFs
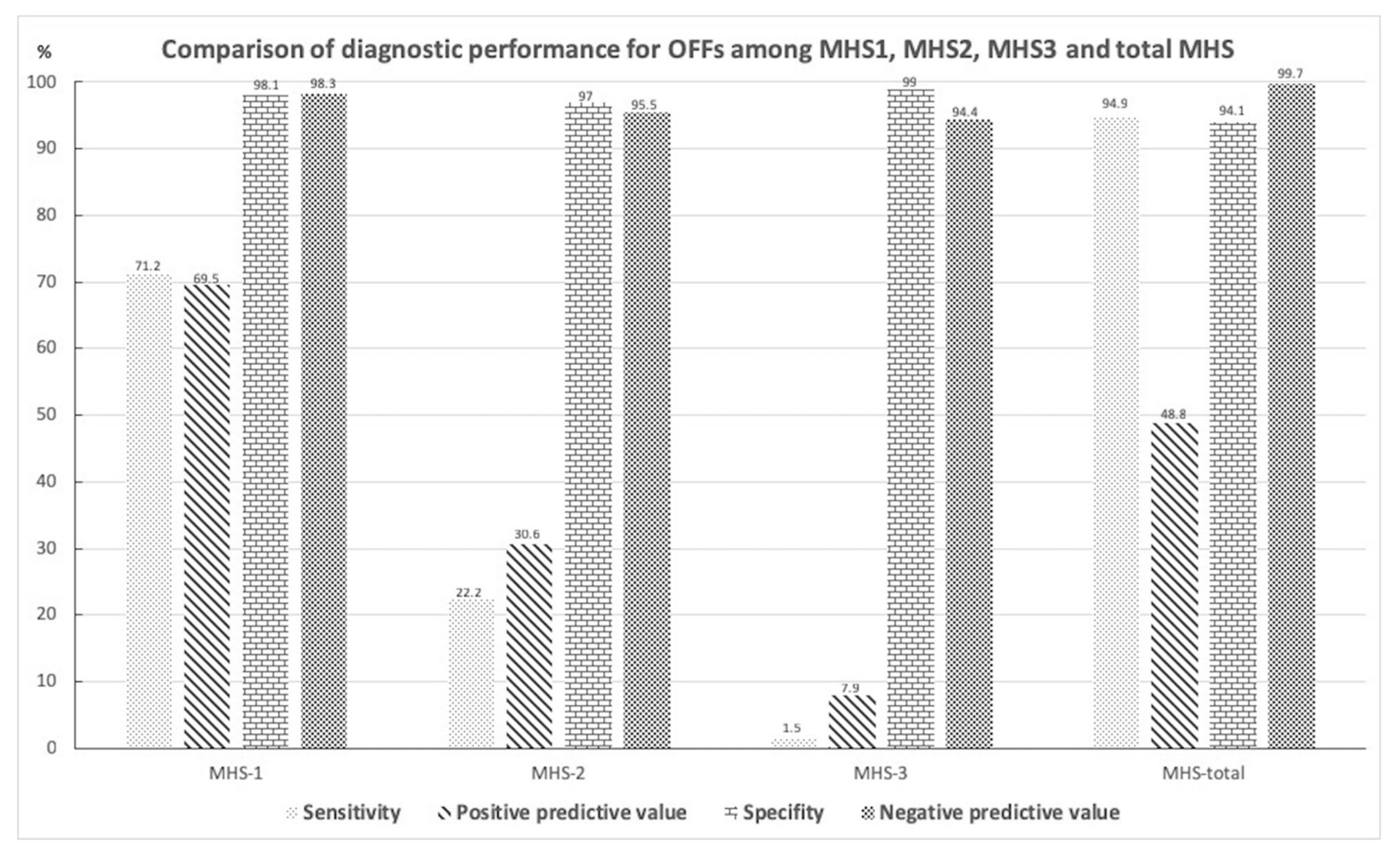
3.2. Diagnostic Performance of MHS
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Zandi, M.; Seyed Hoseini, S.R. The relationship between head injury and facial trauma: A case-control study. Oral Maxillofac. Surg. 2013, 17, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Blaszczyk, B.; Studziński, M.; Ladziński, P. Coincidence of craniocerebral and craniofacial injuries. J. Cranio-Maxillofac. Surg. 2019, 47, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.K.; Wang, H.H.; Tu, H.F.; Fu, C.Y. Simultaneous head and facial computed tomography scans for assessing facial fractures in patients with traumatic brain injury. Injury 2017, 48, 1417–1422. [Google Scholar] [CrossRef] [PubMed]
- Almousa, R.; Amrith, S.; Mani, A.H.; Liang, S.; Sundar, G. Radiological signs of periorbital trauma–the Singapore experience. Orbit 2010, 29, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Smith, H.L.; Chrischilles, E.; Janus, T.J.; Sidwell, R.A.; Ramirez, M.; Peek-Asa, C.; Sahr, S.M. Clinical indicators of midface fracture in patients with trauma. Dent. Traumatol. 2013, 29, 313–318. [Google Scholar] [CrossRef] [PubMed]
- Ludi, E.K.; Rohatgi, S.; Zygmont, M.E.; Khosa, F.; Hanna, T.N. Do Radiologists and Surgeons Speak the Same Language? A Retrospective Review of Facial Trauma. Am. J. Roentgenol. 2016, 207, 1070–1076. [Google Scholar] [CrossRef]
- He, Y.; Zhang, Y.; An, J.G. Correlation of types of orbital fracture and occurrence of enophthalmos. J. Craniofac. Surg. 2012, 23, 1050–1053. [Google Scholar] [CrossRef]
- Cellina, M.; Floridi, C.; Panzeri, M.; Giancarlo, O. The role of computed tomography (CT) in predicting diplopia in orbital blowout fractures (BOFs). Emerg. Radiol. 2018, 25, 13–19. [Google Scholar] [CrossRef]
- Winegar, B.A.; Murillo, H.; Tantiwongkosi, B. Spectrum of critical imaging findings in complex facial skeletal trauma. Radiographics 2013, 33, 3–19. [Google Scholar] [CrossRef]
- Exadaktylos, A.K.; Sclabas, G.M.; Smolka, K.; Rahal, A.; Andres, R.H.; Zimmermann, H.; Iizuka, T. The value of computed tomographic scanning in the diagnosis and management of orbital fractures associated with head trauma: A prospective, consecutive study at a level I trauma center. J. Trauma 2005, 58, 336–341. [Google Scholar] [CrossRef]
- Currie, S.; Saleem, N.; Straiton, J.A.; Macmullen-Price, J.; Warren, D.J.; Craven, I.J. Imaging assessment of traumatic brain injury. Postgrad. Med. J. 2016, 92, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Bodanapally, U.K.; Sours, C.; Zhuo, J.; Shanmuganathan, K. Imaging of Traumatic Brain Injury. Radiol. Clin. N. Am. 2015, 53, 695–715. [Google Scholar] [CrossRef] [PubMed]
- Davis, P.C. Head trauma. Am. J. Neuroradiol. 2007, 28, 1619–1621. [Google Scholar] [PubMed]
- Haydel, M.J.; Preston, C.A.; Mills, T.J.; Luber, S.; Blaudeau, E.; DeBlieux, P.M. Indications for computed tomography in patients with minor head injury. N. Engl. J. Med. 2000, 343, 100–105. [Google Scholar] [CrossRef]
- Lubner, M.; Menias, C.; Rucker, C.; Bhalla, S.; Peterson, C.M.; Wang, L.; Gratz, B. Blood in the belly: CT findings of hemoperitoneum. Radiographics 2007, 27, 109–125. [Google Scholar] [CrossRef]
- Lambert, D.M.; Mirvis, S.E.; Shanmuganathan, K.; Tilghman, D.L. Computed tomography exclusion of osseous paranasal sinus injury in blunt trauma patients: The "clear sinus" sign. J. Oral Maxillofac. Surg. 1997, 55, 1207–1210. [Google Scholar] [CrossRef]
- Teasdale, G.; Jennett, B. Assessment of coma and impaired consciousness. A practical scale. Lancet 1974, 2, 81–84. [Google Scholar] [CrossRef]
- Ingebrigtsen, T.; Romner, B.; Kock-Jensen, C. Scandinavian guidelines for initial management of minimal, mild, and moderate head injuries. The Scandinavian Neurotrauma Committee. J. Trauma 2000, 48, 760–766. [Google Scholar] [CrossRef]
- Foletti, J.M.; Martinez, V.; Graillon, N.; Godio-Raboutet, Y.; Thollon, L.; Guyot, L. Development and validation of an optimized finite element model of the human orbit. J. Stomatol. Oral Maxillofac. Surg. 2019, 120, 16–20. [Google Scholar] [CrossRef]
- Huempfner-Hierl, H.; Schaller, A.; Hierl, T. Maxillofacial fractures and craniocerebral injuries–stress propagation from face to neurocranium in a finite element analysis. Scand. J. Trauma, Resusc. Emerg. Med. 2015, 23, 35. [Google Scholar] [CrossRef][Green Version]
- Lane, K.; Penne, R.B.; Bilyk, J.R. Evaluation and management of pediatric orbital fractures in a primary care setting. Orbit 2007, 26, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.I.; Ahn, K.J.; Chung, Y.A.; Kim, B.S. A new reference line for the brain CT: The tuberculum sellae-occipital protuberance line is parallel to the anterior/posterior commissure line. Am. J. Neuroradiol. 2009, 30, 1704–1708. [Google Scholar] [CrossRef] [PubMed]
- Hammerschlag, S.B.; O’Reilly, G.V.; Naheedy, M.H. Computed tomography of the optic canals. Am. J. Neuroradiol. 1981, 2, 593–594. [Google Scholar] [PubMed]
- Hunts, J.H.; Patrinely, J.R.; Holds, J.B.; Anderson, R.L. Orbital emphysema. Staging and acute management. Ophthalmology 1994, 101, 960–966. [Google Scholar] [CrossRef]
- Fleishman, J.A.; Beck, R.W.; Hoffman, R.O. Orbital emphysema as an ophthalmologic emergency. Ophthalmology 1984, 91, 1389–1391. [Google Scholar] [CrossRef]
- Moon, H.; Kim, Y.; Wi, J.M.; Chi, M. Morphological characteristics and clinical manifestations of orbital emphysema caused by isolated medial orbital wall fractures. Eye 2016, 30, 582–587. [Google Scholar] [CrossRef]
- Lewandowski, R.J.; Rhodes, C.A.; McCarroll, K.; Hefner, L. Role of routine nonenhanced head computed tomography scan in excluding orbital, maxillary, or zygomatic fractures secondary to blunt head trauma. Emerg. Radiol. 2004, 10, 173–175. [Google Scholar] [CrossRef]
- Friedman, A.; Burns, J.; Scheinfeld, M.H. Significance of post-traumatic maxillary sinus fluid, or lack of fluid, in a level II trauma population. Emerg. Radiol. 2015, 22, 661–666. [Google Scholar] [CrossRef]
- Gwaltney, J.M., Jr.; Phillips, C.D.; Miller, R.D.; Riker, D.K. Computed tomographic study of the common cold. N. Engl. J. Med. 1994, 330, 25–30. [Google Scholar] [CrossRef]
- Chen, H.J.; Chen, H.S.; Chang, Y.L.; Huang, Y.C. Complete unilateral maxillary sinus opacity in computed tomography. J. Formos. Med. Assoc. 2010, 109, 709–715. [Google Scholar] [CrossRef]
| Variables | With OFFs (n = 198) | Without OFFs (n = 3336) | p-Value | Odds Ratio of OFF a (95% CI) |
|---|---|---|---|---|
| General demographics | ||||
| Age (years) | 46.8 ± 21.5 | 58.6 ± 21.0 | <0.001 b | 0.98 (0.97–0.99) |
| Male (n, %) | 137 (69.2) | 1810 (54.3) | <0.001 c | 1.64 (1.14–2.37) |
| Clinical information | ||||
| ILOC (n, %) | 98 (49.5) | 985 (29.5) | <0.001c | NS |
| Specific mechanism of injury (n, %) | ||||
| Fall from elevation | 11 (5.6) | 96 (2.9) | 0.033 c | 3.22 (1.38–7.54) |
| Motorcycle collision | 116 (58.6) | 880 (26.4) | <0.001c | 1.72 (1.17–2.52) |
| Evaluation in emergency department | ||||
| GCS at ED (scale) | 13.7 ± 3.0 | 14.6 ± 1.7 | <0.001 b | NS |
| LOC (GCS < 14) (n, %) | 47 (23.7) | 259 (7.8) | <0.001 c | NS |
| Deep coma (GCS < 8) (n, %) | 19 (9.6) | 81 (2.4) | <0.001 c | NS |
| Physical findings (n, %) | ||||
| Blepharohematoma | 159 (80.3) | 535 (16.0) | <0.001 c | 14.78 (9.94–21.98) |
| Facial wound | 179 (90.4) | 1139 (34.1) | <0.001 c | 6.68 (4.02–11.11) |
| Epistaxis | 26 (13.1) | 95 (2.8) | <0.001c | 2.47 (1.39–4.39) |
| Variables | With OFFs (n = 198) | Without OFFs (n = 3336) | p-Value a |
|---|---|---|---|
| CT variables related to the cranium (n, %) | |||
| ICH | 52 (26.3) | 463 (13.9) | <0.001 |
| Skull fracture | 37 (18.7) | 150 (4.5) | <0.001 |
| CT variables related to OFFs (n, %) | |||
| Orbital floor discontinuity | 181 (91.4) | 0 (0) | <0.001 |
| Gas bubbles entrapped between floor fragments | 156 (78.8) | 0 (0) | <0.001 |
| Orbital fat herniation into the maxillary sinus | 31 (15.7) | 0 (0) | <0.001 |
| Inferior extraconal emphysema | 98 (49.5) | 15 (0.4) | <0.001 |
| MHS | 188 (94.9) | 197 (5.9) | <0.001 |
| CT Variables | With OFFs (n = 188) | Without OFFs a (n = 102) | p-Value b | Odds Ratio c (95% CI) |
|---|---|---|---|---|
| MHS type 1 | 141 (75.0) | 7 (6.9) | <0.001 | 47.50 (8.26–273.05) |
| MHS type 2 | 44 (23.4) | 63 (61.8) | <0.001 | - |
| MHS type 3 | 3 (1.6) | 32 (31.4) | <0.001 | - |
| Orbital floor discontinuity | 172 (91.5) | 0 (0) | <0.001 | NS |
| Gas bubbles entrapped between floor fragments | 149 (79.3) | 0 (0) | <0.001 | NS |
| Orbital fat herniation into the maxillary sinus | 27 (14.4) | 0 (0) | <0.001 | NS |
| Inferior extraconal emphysema | 94 (50.0) | 0 (0) | <0.001 | NS |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, L.-K.; Tu, H.-F.; Jiang, L.-D.; Chen, Y.-Y.; Fu, C.-Y. Evaluation of Concomitant Orbital Floor Fractures in Patients with Head Trauma Using Conventional Head CT Scan: A Retrospective Study at a Level II Trauma Center. J. Clin. Med. 2019, 8, 1852. https://doi.org/10.3390/jcm8111852
Huang L-K, Tu H-F, Jiang L-D, Chen Y-Y, Fu C-Y. Evaluation of Concomitant Orbital Floor Fractures in Patients with Head Trauma Using Conventional Head CT Scan: A Retrospective Study at a Level II Trauma Center. Journal of Clinical Medicine. 2019; 8(11):1852. https://doi.org/10.3390/jcm8111852
Chicago/Turabian StyleHuang, Li-Kuo, Hsi-Feng Tu, Liang-De Jiang, Ying-Yuan Chen, and Chih-Yuan Fu. 2019. "Evaluation of Concomitant Orbital Floor Fractures in Patients with Head Trauma Using Conventional Head CT Scan: A Retrospective Study at a Level II Trauma Center" Journal of Clinical Medicine 8, no. 11: 1852. https://doi.org/10.3390/jcm8111852
APA StyleHuang, L.-K., Tu, H.-F., Jiang, L.-D., Chen, Y.-Y., & Fu, C.-Y. (2019). Evaluation of Concomitant Orbital Floor Fractures in Patients with Head Trauma Using Conventional Head CT Scan: A Retrospective Study at a Level II Trauma Center. Journal of Clinical Medicine, 8(11), 1852. https://doi.org/10.3390/jcm8111852




