Smartphone Apps Targeting Hazardous Drinking Patterns among University Students Show Differential Subgroup Effects over 20 Weeks: Results from a Randomized, Controlled Trial
Abstract
:1. Introduction
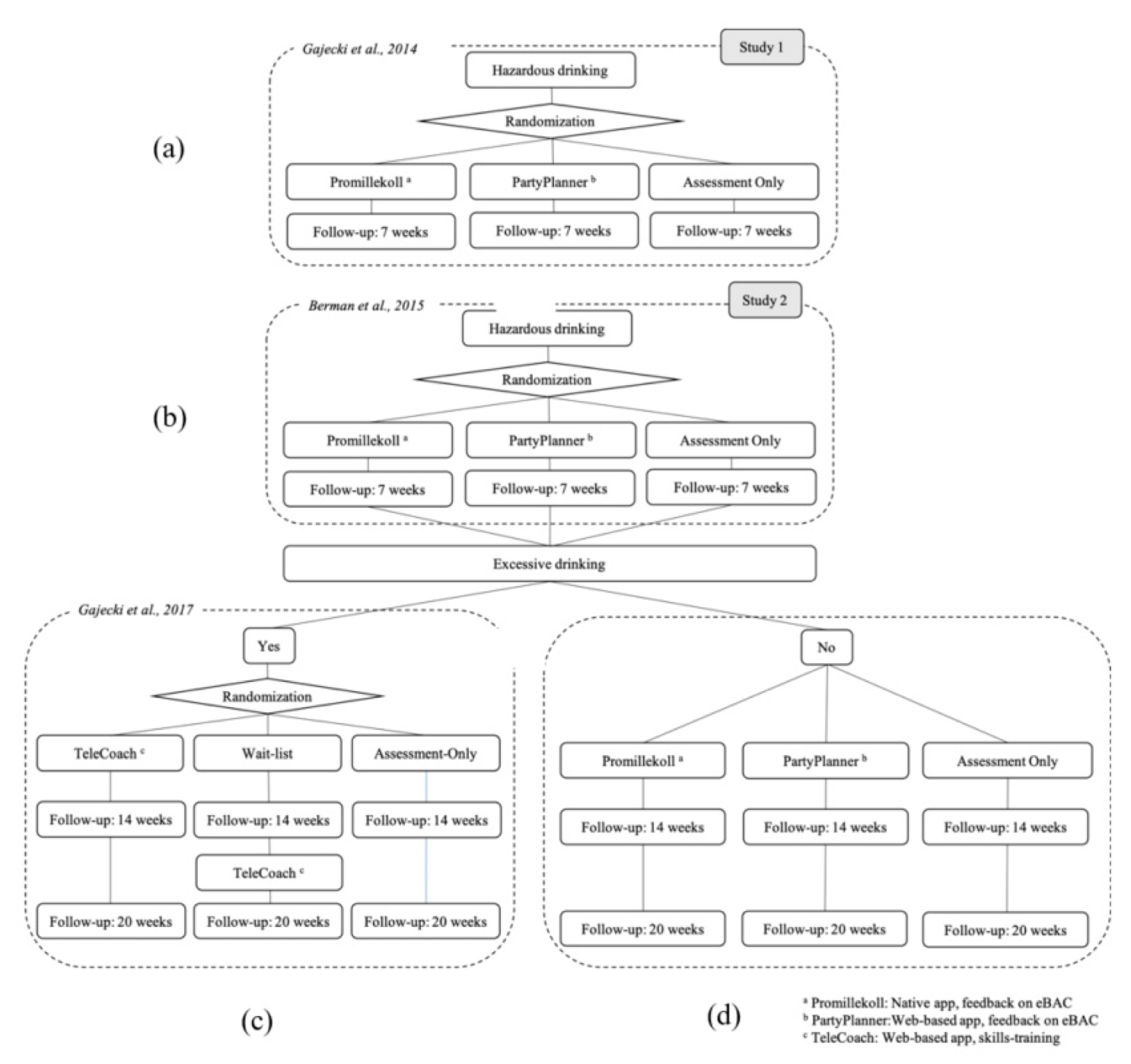
2. Experimental Section
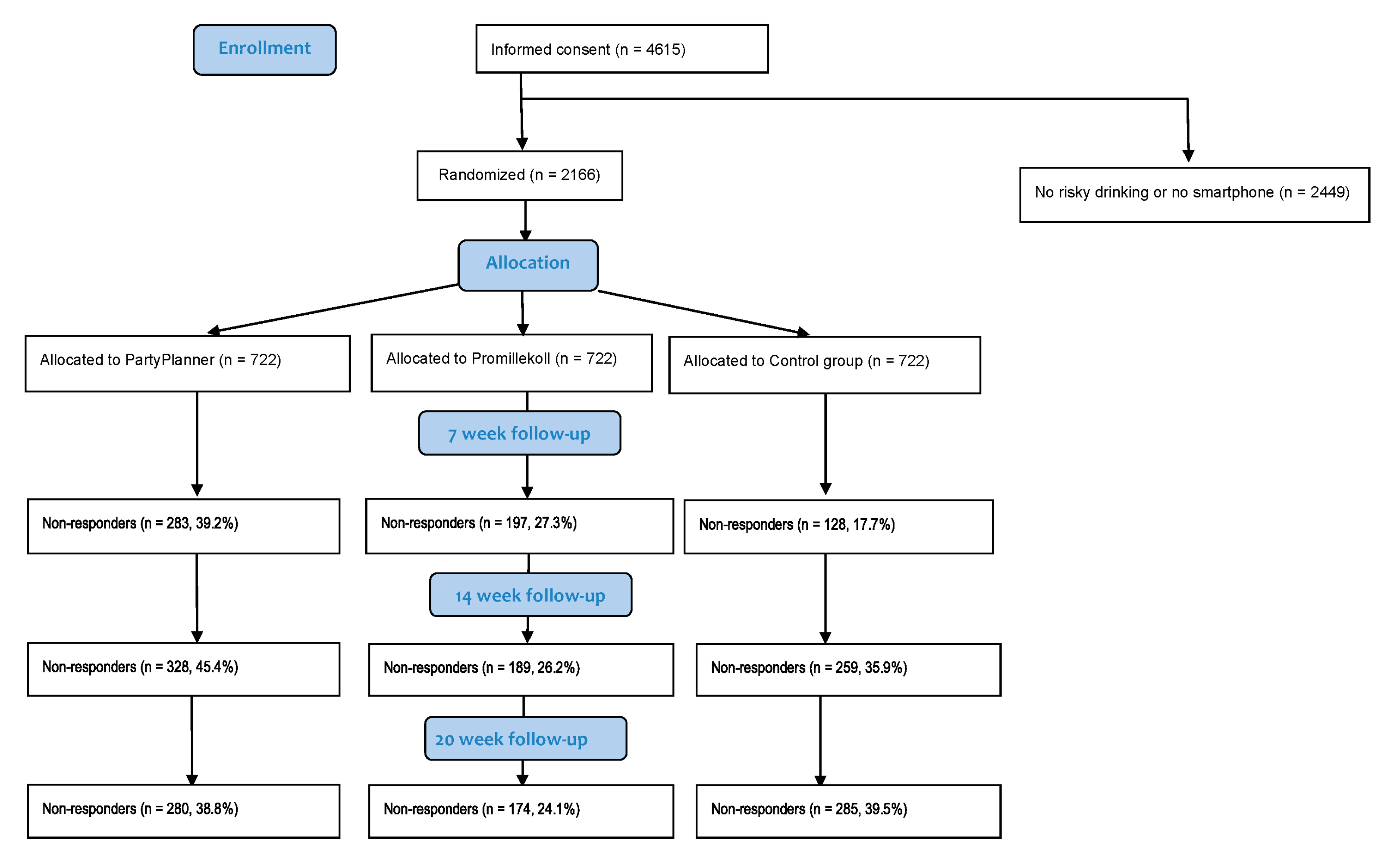
2.1. Procedure
2.2. Interventions
2.3. Statistics
3. Results
3.1. Baseline Characteristics
3.2. 7 Week Follow-up
3.3. 7, 14, and 20 Weeks for Non-Excessive Drinkers
3.4. Motivation to Change
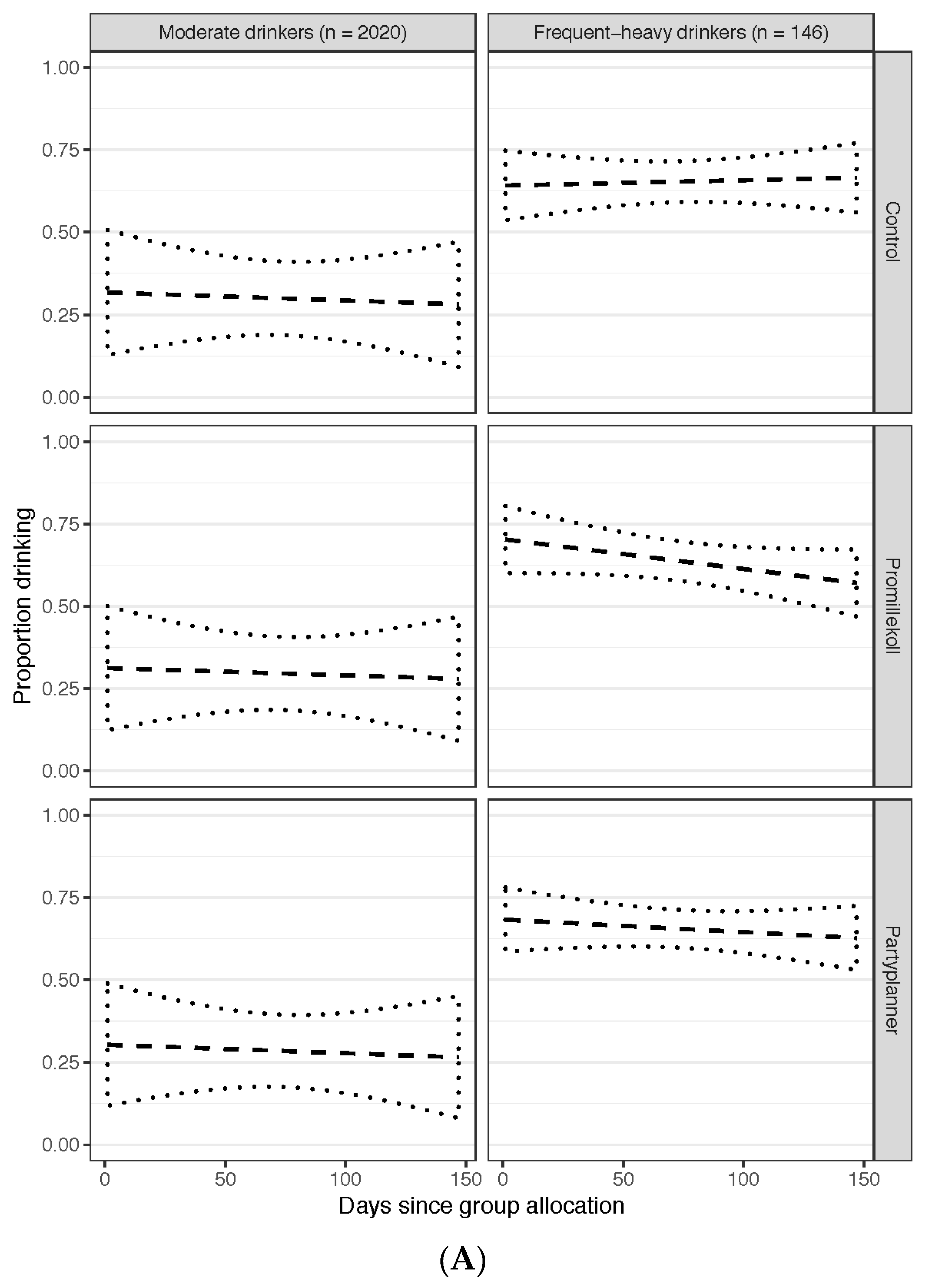
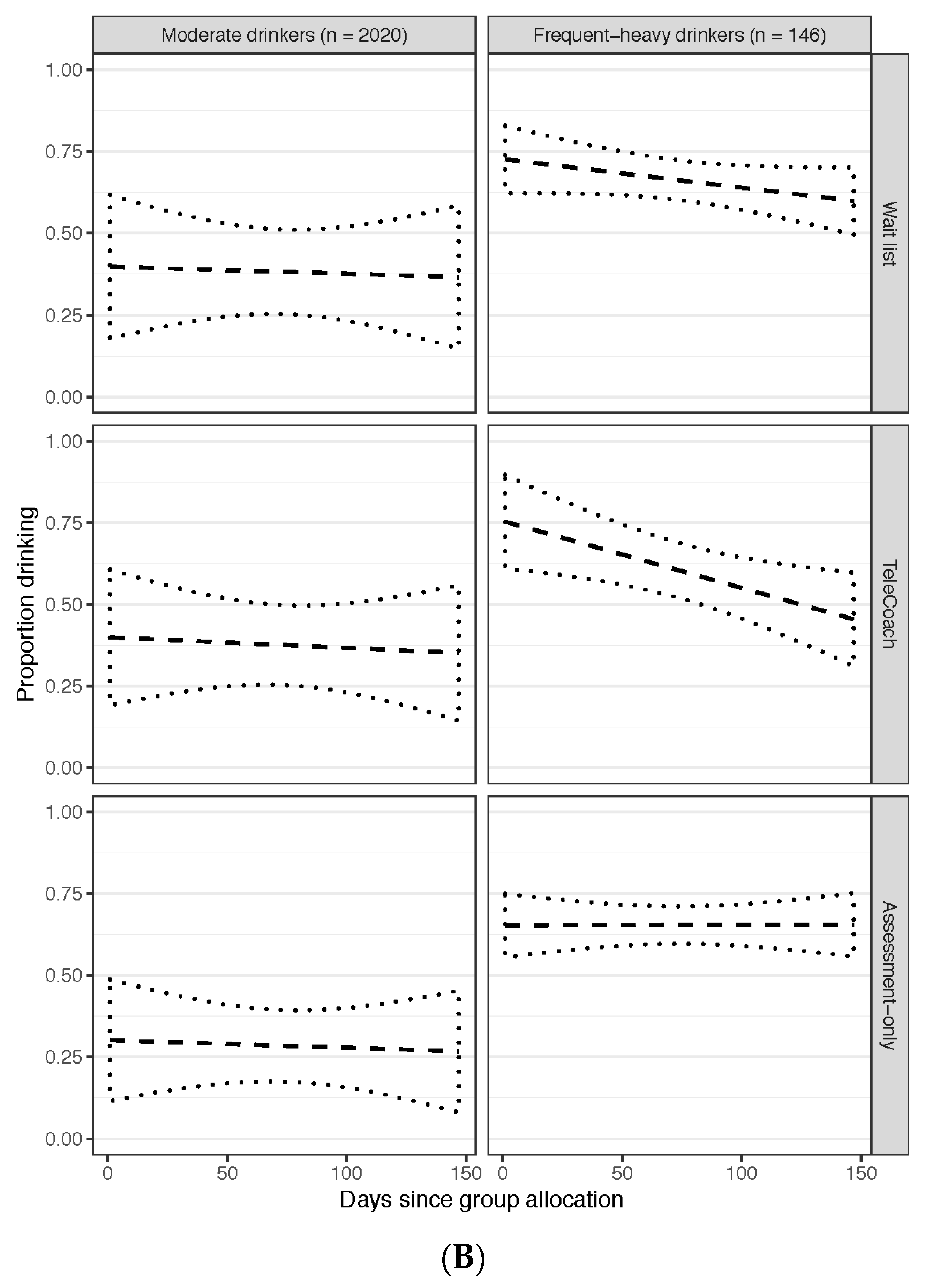
3.5. Hidden Markov Model Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Data Statement
References
- Rehm, J.; Mathers, C.; Popova, S.; Thavorncharoensap, M.; Teerawattananon, Y.; Patra, J. Global burden of disease and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 2009, 373, 2223–2233. [Google Scholar] [CrossRef]
- WHO. Global Status Report on Alcohol 2018; World Health Organisation: Geneva, Switzerland, 2018. [Google Scholar]
- Chisholm, D.; Rehm, J.; Van Ommeren, M.; Monteiro, M. Reducing the global burden of hazardous alcohol use: A comparative cost-effectiveness analysis. J. Stud. Alcohol 2004, 65, 782–793. [Google Scholar] [CrossRef] [PubMed]
- Connor, J.P.; Haber, P.S.; Hall, W.D. Alcohol use disorders. Lancet 2016, 387, 988–998. [Google Scholar] [CrossRef] [Green Version]
- Kaner, E.F.S.; Beyer, F.R.; Garnett, C.; Crane, D.; Brown, J.; Muirhead, C.; Redmore, J.; O’Donnell, A.; Newham, J.J.; de Vocht, F.; et al. Personalised digital interventions for reducing hazardous and harmful alcohol consumption in community-dwelling populations. Cochrane Database Syst. Rev. 2017, 9. [Google Scholar] [CrossRef]
- Grant, B.F.; Goldstein, R.B.; Saha, T.D.; Chou, S.P.; Jung, J.; Zhang, H.; Pickering, R.P.; Ruan, W.J.; Smith, S.M.; Huang, B.; et al. Epidemiology of DSM-5 alcohol use disorder: Results from the national epidemiologic survey on alcohol and related conditions III. JAMA Psychiatry 2015, 72, 757–766. [Google Scholar] [CrossRef]
- Arnett, J.J.; Žukauskienė, R.; Sugimura, K. The new life stage of emerging adulthood at ages 18–29 years: Implications for mental health. Lancet Psychiatry 2014, 1, 569–576. [Google Scholar] [CrossRef]
- Kohn, R.; Saxena, S.; Levav, I.; Saraceno, B. The treatment gap in mental health care. Bull. World Health Organ. 2004, 82, 858–866. [Google Scholar]
- Johnston, L.D.; O’Malley, P.M.; Bachman, J.G.; Schulenberg, J.E. Monitoring the Future: National Survey Results on Drug Use, 1975–2012. Volume 2: College Students and Adults ages 19–50; Institute of Social Research, University of Michigan: Ann Arbor, MI, USA, 2013. [Google Scholar]
- Plant, M.A.; Plant, M.L.; Miller, P.; Gmel, G.; Kuntsche, S. The social consequences of binge drinking: A comparison of young adults in six European countries. J. Addict. Dis. 2009, 28, 294–308. [Google Scholar] [CrossRef]
- O’Neill, S.E.; Parra, G.R.; Sher, K.J. Clinical relevance of heavy drinking during the college years: Cross-sectional and prospective perspectives. Psychol. Addict. Behav. 2001, 15, 350. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.-T.; Pilowsky, D.J.; Schlenger, W.E.; Hasin, D. Alcohol use disorders and the use of treatment services among college-age young adults. Psychiatr. Serv. 2007, 58, 192–200. [Google Scholar] [CrossRef]
- Buscemi, J.; Murphy, J.G.; Martens, M.P.; McDevitt-Murphy, M.E.; Dennhardt, A.A.; Skidmore, J.R. Help-seeking for alcohol-related problems in college students: Correlates and preferred resources. Psychol. Addict. Behav. 2010, 24, 571. [Google Scholar] [CrossRef] [PubMed]
- Cronce, J.M.; Larimer, M.E. Individual-focused approaches to the prevention of college student drinking. Alcohol Res. Health 2011, 34, 210. [Google Scholar] [PubMed]
- Sundström, C.; Blankers, M.; Khadjesari, Z. Computer-based interventions for problematic alcohol use: A review of systematic reviews. Int. J. Behav. Med. 2016, 24, 646–658. [Google Scholar] [CrossRef] [PubMed]
- Riper, H.; Hoogendoorn, A.; Cuijpers, P.; Karyotaki, E.; Boumparis, N.; Mira, A.; Andersson, G.; Berman, A.H.; Bertholet, N.; Bischof, G.; et al. Effectiveness and treatment moderators of internet interventions for adult problem drinking: An individual patient data meta-analysis of 19 randomised controlled trials. PLoS Med. 2018, 15, e1002714. [Google Scholar] [CrossRef] [PubMed]
- Carey, K.B.; Scott-Sheldon, L.A.; Elliott, J.C.; Garey, L.; Carey, M.P. Face-to-face versus computer-delivered alcohol interventions for college drinkers: A meta-analytic review, 1998 to 2010. Clin. Psychol. Rev. 2012, 32, 690–703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carey, K.B.; Scott-Sheldon, L.A.; Elliott, J.C.; Bolles, J.R.; Carey, M.P. Computer-delivered interventions to reduce college student drinking: A meta-analysis. Addiction 2009, 104, 1807–1819. [Google Scholar] [CrossRef] [PubMed]
- Berman, A.H.; Gajecki, M.; Sinadinovic, K.; Andersson, C. Mobile interventions targeting risky drinking among university students: A review. Curr. Addict. Rep. 2016, 3, 166–174. [Google Scholar] [CrossRef]
- Andersson, C. Comparison of WEB and Interactive Voice Response (IVR) methods for delivering brief alcohol interventions to hazardous-drinking university students: A randomized controlled trial. Eur. Addict. Res. 2015, 21, 240–252. [Google Scholar] [CrossRef]
- Witkiewitz, K.; Desai, S.A.; Bowen, S.; Leigh, B.C.; Kirouac, M.; Larimer, M.E. Development and evaluation of a mobile intervention for heavy drinking and smoking among college students. Psychol. Addict. Behav. 2014, 28, 639. [Google Scholar] [CrossRef]
- Schulenberg, J.E.; Maggs, J.L. A developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. J. Stud. Alcohol Suppl. 2002, 14, 54–70. [Google Scholar] [CrossRef]
- Reiskin, H.; Wechsler, H. Drinking among college students using a campus mental health center. J. Stud. Alcohol 1981, 42, 716–724. [Google Scholar] [CrossRef] [PubMed]
- Larimer, M.E.; Cronce, J.M. Identification, prevention, and treatment revisited: Individual-focused college drinking prevention strategies 1999–2006. Addict. Behav. 2007, 32, 2439–2468. [Google Scholar] [CrossRef] [PubMed]
- Gajecki, M.; Berman, A.H.; Sinadinovic, K.; Rosendahl, I.; Andersson, C. Mobile phone brief intervention applications for risky alcohol use among university students: A randomized controlled study. Addict. Sci. Clin. Pract. 2014, 9, 11. [Google Scholar] [CrossRef] [PubMed]
- Berman, A.H.; Gajecki, M.; Fredriksson, M.; Sinadinovic, K.; Andersson, C. Smartphone applications for university students with hazardous alcohol use: Study protocol for two consecutive randomized controlled trials. JMIR Res. Protoc. 2015, 4, e139. [Google Scholar] [CrossRef]
- Gajecki, M.; Andersson, C.; Rosendahl, I.; Sinadinovic, K.; Fredriksson, M.; Berman, A.H. Skills training via smartphone app for university students with excessive alcohol consumption: A randomized controlled trial. Int. J. Behav. Med. 2017, 24, 778–788. [Google Scholar] [CrossRef]
- Witkiewitz, K.; Dearing, R.L.; Maisto, S.A. Alcohol use trajectories among non-treatment-seeking heavy drinkers. J. Stud. Alcohol Drugs 2014, 75, 415–422. [Google Scholar] [CrossRef]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; de la Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Bergman, H.; Källmén, H. Alcohol use among Swedes and a psychometric evaluation of the Alcohol Use Disorders Identification Test. Alcohol Alcohol. 2002, 37, 245–251. [Google Scholar] [CrossRef]
- Andréasson, S.; Allebeck, P. Alkohol och hälsa: En Kunskapsöversikt om Alkoholens Positiva och Negativa Effekter på Vår Hälsa; [Alcohol and Health: A Knowledge-Based Overview of the Positive and Negative Effects of Alcohol on Our Health]; R 2005:11; Statens Folkhälsoinstitut: Stockholm, Sweden, 2005. [Google Scholar]
- Collins, R.L.; Parks, G.A.; Marlatt, G.A. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. J. Consult. Clin. Psychol. 1985, 53, 189. [Google Scholar] [CrossRef]
- Bertholet, N.; Cheng, D.M.; Palfai, T.P.; Samet, J.H.; Saitz, R. Does readiness to change predict subsequent alcohol consumption in medical inpatients with unhealthy alcohol use? Addict. Behav. 2009, 34, 636–640. [Google Scholar] [CrossRef] [Green Version]
- Craig, D.W.; Perkins, H.W. Accuracy of estimated blood alcohol concentration norms from college student drinking survey data: Verification using matched late-night breath measurements. J. Stud. Alcohol Drugs 2018, 79, 455–464. [Google Scholar] [CrossRef] [PubMed]
- Martens, M.P.; Ferrier, A.G.; Cimini, M.D. Do protective behavioral strategies mediate the relationship between drinking motives and alcohol use in college students? J. Stud. Alcohol Drugs 2007, 68, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Bartolucci, F.; Farcomeni, A.; Pennoni, F. Latent Markov models: A review of a general framework for the analysis of longitudinal data with covariates. Test 2014, 23, 433–465. [Google Scholar] [CrossRef]
- Rabiner, L.; Juang, B. An introduction to hidden Markov models. IEEE ASSP Mag. 1986, 3, 4–16. [Google Scholar] [CrossRef]
- Jurafsky, D.; Martin, J.H. Hidden Markov and maximum entropy models. In Speech And Language Processing: An Introduction to Natural Language Processing, Computational Linguistics, and Speech Recognition, 2nd ed.; Pearson Education: New York, NY, USA, 2006. [Google Scholar]
- Donders, A.R.; van der Heijden, G.J.; Stijnen, T.; Moons, K.G. Review: A gentle introduction to imputation of missing values. J. Clin. Epidemiol. 2006, 59, 1087–1091. [Google Scholar] [CrossRef]
- Tucker, J.S.; D’Amico, E.J.; Ewing, B.A.; Miles, J.N.; Pedersen, E.R. A group-based motivational interviewing brief intervention to reduce substance use and sexual risk behavior among homeless young adults. J. Subst. Abus. Treat. 2017, 76, 20–27. [Google Scholar] [CrossRef] [Green Version]
- Song, T.; Qian, S.; Yu, P. Mobile health interventions for self-control of unhealthy alcohol use: Systematic review. JMIR Mhealth Uhealth 2019, 7, e10899. [Google Scholar] [CrossRef]
- Sinadinovic, K.; Wennberg, P.; Johansson, M.; Berman, A.H. Targeting individuals with problematic alcohol use via Internet-based cognitive-behavioral self-help modules, personalized screening feedback or assessment only: A randomized controlled trial. Eur. Addict. Res. 2014, 20, 305–318. [Google Scholar] [CrossRef]
- Johansson, M.; Sinadinovic, K.; Hammarberg, A.; Sundström, C.; Hermansson, U.; Andreasson, S.; Berman, A.H. Web-based self-help for problematic alcohol use: A large naturalistic study. Int. J. Behav. Med. 2017, 24, 749–759. [Google Scholar] [CrossRef]
- Walters, S.T.; Vader, A.M.; Harris, T.R.; Field, C.A.; Jouriles, E.N. Dismantling motivational interviewing and feedback for college drinkers: A randomized clinical trial. J. Consult. Clin. Psychol. 2009, 77, 64–73. [Google Scholar] [CrossRef]
- Andersson, G.; Titov, N.; Dear, B.F.; Rozental, A.; Carlbring, P. Internet-delivered psychological treatments: From innovation to implementation. World Psychiatry 2019, 18, 20–28. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Total (n = 2166) | PartyPlanner (n = 722) | Promillekoll (n = 722) | Control (n = 722) | p-Values a |
|---|---|---|---|---|---|
| Gender: M (%)/F (%) | 704 (32.5)/1462 (67.5) | 206 (31.3)/496 (68.7) | 226 (31.2)/497 (68.8) | 253 (35.0)/469 (65.0) | 0.203 |
| Age: mean (SD) | 25.84 (6.57) | 25.73 (6.38) | 25.84 (6.36) | 25.93 (6.94) | 0.844 |
| Measures of alcohol consumption: means (SD) | |||||
| Alcohol Use Disorders Identification Test (AUDIT) score (scale 0–40) | 10.98 (4.33) | 10.98 (4.40) | 10.96 (4.21) | 10.99 (4.38) | 0.992 |
| Quantity (standard glasses/week) | 9.40 (6.69) | 9.24 (6.57) | 9.24 (6.44) | 9.71 (7.05) | 0.309 |
| Frequency (drinking occasions/week) | 2.39 (1.23) | 2.31 (1.21) | 2.37 (1.25) | 2.48 (1.24) | 0.026 b |
| Binge occasions (no. per week) | 1.04 (0.91) | 1.03 (0.90) | 1.04 (0.91) | 1.04 (0.94) | 0.985 |
| Average estimated blood alcohol concentration (eBAC) c per week | 0.018 (0.023) | 0.019 (0.017) | 0.018 (0.020) | 0.017 (0.030) | 0.487 |
| Peak eBAC d within past month | 1.35 (0.89) | 1.40 (0.93) | 1.33 (0.87) | 1.32 (0.86) | 0.197 |
| Percent (%) over weekly recommended level | 31.0 | 30.3 | 30.5 | 32.1 | 0.709 |
| Motivation to change drinking behavior (scale 0–10) | 4.07 (2.61) | 4.06 (2.63) | 4.17 (2.67) | 3.97 (2.54) | 0.358 |
| Measures of Alcohol consumption in Means (SD); N = 2166 | Control | PartyPlanner | PartyPlanner Compared to Control Linear Mixed Models c | Promillekoll | Promillekoll Compared to Control Linear Mixed Models d | |||
|---|---|---|---|---|---|---|---|---|
| Baseline (n = 722) | Follow-up (n = 594) | Baseline (n = 722) | Follow-up (n = 439) | Time*Group p-Value | Baseline n = 722) | Follow-up (n = 525) | Time*Group p-Value | |
| Quantity (standard glasses/week) | 9.601 (6.669) | 8.634 (6.313) | 9.268 (6.277) | 8.351 (5.838) | 0.828 | 9.283 (6.149) | 8.875 (6.559) | 0.135 |
| Frequency (drinking occasions/week) | 2.472 (1.211) | 2.390 (1.306) | 2.310 (1.192) | 2.238 (1.201) | 0.799 | 2.367 (1.234) | 2.349 (1.210) | 0.101 |
| Binge occasions (no. per week) | 1.032 (0.919) | 0.833 (0.841) | 1.033 (0.881) | 0.863 (0.880) | 0.778 | 1.044 (0.891) | 0.879 (0.884) | 0.726 |
| eBAC a/week | 0.019 (0.018) | 0.017 (0.016) | 0.019 (0.017) | 0.017 (0.017) | 0.765 | 0.019 (0.018) | 0.018 (0.018) | 0.208 |
| Peak eBAC b/month | 1.331 (0.821) | 1.238 (0.842) | 1.393 (0.903) | 1.266 (0.915) | 0.419 | 1.331 (0.843) | 1.270 (0.904) | 0.694 |
| Risk for excessive weekly drinking | 0.322 (0.467) | 0.244 (0.420) | 0.302 (0.458) | 0.253 (0.412) | Odds ratio (OR) 1.33 n.s.e | 0.305 (0.460) | 0.284 (0.431) | OR 1.83 ** |
| Measures of Alcohol Consumption in Means (SD) N = 2166 a | Control | PartyPlanner | PartyPlanner Compared to Control Linear Mixed Models | Promillekoll | Promillekoll Compared to Control Linear Mixed Models | |||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | Time*Group p-Value | Baseline | Follow-up | Time*Group p-Value | |
| 7 week follow-up for hazardous drinkers, n = 1157 | (n = 450) | (n = 450) | (n = 335) | (n = 335) | (n = 372) | (n = 372) | ||
| Quantity (standard glasses/week) | 7.540 (4.454) | 5.790 (3.228) | 7.081 (4.082) | 5.380 (3.137 | 0.860 | 7.161 (4.184) | 5.489 (2.961) | 0.686 |
| Frequency (drinking occasions/week) | 2.227 (1.115) | 2.013 (1.141) | 2.002 (1.035) | 1.827 (1.103) | 0.064 | 2.093 (1.157) | 1.937 (1.081) | 0.085 |
| Binge occasions (no. per week) | 0.782 (0.755) | 0.487 (0.562) | 0.804 (0.707) | 0.524 (0.595) | 0.062 | 0.765 (0.718) | 0.452 (0.562) | 0.040 * |
| eBAC b/week | 0.014 (0.012) | 0.011 (0.009) | 0.014 (0.012) | 0.010 (0.008) | 0.001 *** | 0.014 (0.010) | 0.010 (0.008) | 0.001 *** |
| Peak eBAC c/month | Model did not converge | |||||||
| Risk for excessive weekly drinking | Model did not converge | |||||||
| 14 week follow-up for hazardous drinkers, n = 984 | (n = 401) | (n = 266) | (n = 317) | |||||
| Quantity (standard glasses/week) | 6.672 (6.317) | 5.950 (4.024) | 0.128 | 6.014 (4.830) | 0.072 | |||
| Frequency (drinking occasions/week) | 2.007 (1.320) | 1.872 (1.142) | 0.100 | 2.012 (1.324) | 0.107 | |||
| Binge occasions (no. per week) | 0.630 (0.793) | 0.599 (0.661) | 0.046 * | 0.543 (0.712) | 0.022 * | |||
| eBAC b/week | 0.013 (0.015) | 0.012 (0.012) | 0.001 *** | 0.011 (0.012) | 0.001 *** | |||
| 20 week follow-up for hazardous drinkers, n = 975 | (n = 400) | (n = 262) | (n = 313) | |||||
| Quantity (standard glasses/week) | 6.320 (4.306) | 5.764 (3.992) | 0.088 | 5.868 (3.885) | 0.112 | |||
| Frequency (drinking occasions/week) | 1.922 (1.155) | 1.805 (1.088) | 0.093 | 1.847 (1.088) | 0.093 | |||
| Binge occasions (no. per week) | 0.599 (0.762) | 0.611 (0.676) | 0.061 | 0.541 (0.674) | 0.043 * | |||
| eBAC b/week | 0.012 (0.012) | 0.011 (0.011) | 0.001 *** | 0.010 (0.010) | 0.001 *** | |||
| Characteristic | Continual Frequent-Heavy Drinkers (n = 119) a | Itinerant Frequent-Heavy Drinkers (n = 27) a | Total Frequent-Heavy Drinkers (n = 146) | Total Moderate b Drinkers (n = 2020) | t/Z | pc |
|---|---|---|---|---|---|---|
| Gender: M (%)/W (%) | M = 63 (52.9%)/W = 56 (47.1%) | M = 13 (48.1%)/W = 14 (51.9%) | M = 76 (52.1%)/W = 70 (47.9%) | M = 628 (31.1%)/W = 1392 (68.9%) | Z = −5.2231 | <0.0001 |
| Age: mean (SD) | 30.4 (10.2) | 25.7 (4.1) | 29.5 (9.5) | 25.6 (6.2) | t = 4.9661 (df = 154.06) | <0.0001 |
| Measures of alcohol consumption: means (SD) | ||||||
| AUDIT score (scale 0–40) | 14.1 (6.1) | 12.4 (4.3) | 13.8 (5.8) | 10.8 (4.1) | t = 6.206 (df = 155.82) | <0.0001 |
| Quantity (standard glasses/week) | 17.3 (10.6) | 12.4 (8.5) | 16.4 (10.4) | 8.9 (6.0) | t = 8.63 (df = 152.1) | <0.0001 |
| Frequency (drinking occasions/week) | 5.0 (1.2) | 3.2 (1.3) | 4.6 (1.4) | 2.2 (1.0) | t = 20.801 (df = 157.46) | <0.0001 |
| Binge occasions (no. per week) | 1.5 (1.4) | 1.2 (1.1) | 1.4 (1.4) | 1.0 (0.86) | t = 3.6129 (df = 153.12) | 0.0004 |
| Average eBAC d per week | 0.033 (0.028) | 0.019 (0.017) | 0.031 (0.027) | 0.018 (0.017) | t = 5.5123 (df = 153.36) | <0.0001 |
| Peak eBAC e within past month | 1.53 (1.09) | 1.48 (0.78) | 1.52 (1.04) | 1.34 (0.87) | t = 2.0771 (df = 160.1) | 0.004 |
| Percent (%) over weekly recommended level | 81 (68.1%) | 13 (48.1%) | 94 (64.4%) | 575 (28.5%) | Z = 9.0714 | <0.0001 |
| Motivation to change drinking behavior (scale 0–10) | 5.1 (2.7) | 3.9 (3.0) | 4.8 (2.7) | 4.0 (2.6) | t = 3.5199 (df = 164.37) | 0.0006 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berman, A.H.; Andersson, C.; Gajecki, M.; Rosendahl, I.; Sinadinovic, K.; Blankers, M. Smartphone Apps Targeting Hazardous Drinking Patterns among University Students Show Differential Subgroup Effects over 20 Weeks: Results from a Randomized, Controlled Trial. J. Clin. Med. 2019, 8, 1807. https://doi.org/10.3390/jcm8111807
Berman AH, Andersson C, Gajecki M, Rosendahl I, Sinadinovic K, Blankers M. Smartphone Apps Targeting Hazardous Drinking Patterns among University Students Show Differential Subgroup Effects over 20 Weeks: Results from a Randomized, Controlled Trial. Journal of Clinical Medicine. 2019; 8(11):1807. https://doi.org/10.3390/jcm8111807
Chicago/Turabian StyleBerman, Anne H., Claes Andersson, Mikael Gajecki, Ingvar Rosendahl, Kristina Sinadinovic, and Matthijs Blankers. 2019. "Smartphone Apps Targeting Hazardous Drinking Patterns among University Students Show Differential Subgroup Effects over 20 Weeks: Results from a Randomized, Controlled Trial" Journal of Clinical Medicine 8, no. 11: 1807. https://doi.org/10.3390/jcm8111807
APA StyleBerman, A. H., Andersson, C., Gajecki, M., Rosendahl, I., Sinadinovic, K., & Blankers, M. (2019). Smartphone Apps Targeting Hazardous Drinking Patterns among University Students Show Differential Subgroup Effects over 20 Weeks: Results from a Randomized, Controlled Trial. Journal of Clinical Medicine, 8(11), 1807. https://doi.org/10.3390/jcm8111807





