Obstructive Sleep Apnea: Emerging Treatments Targeting the Genioglossus Muscle
Abstract
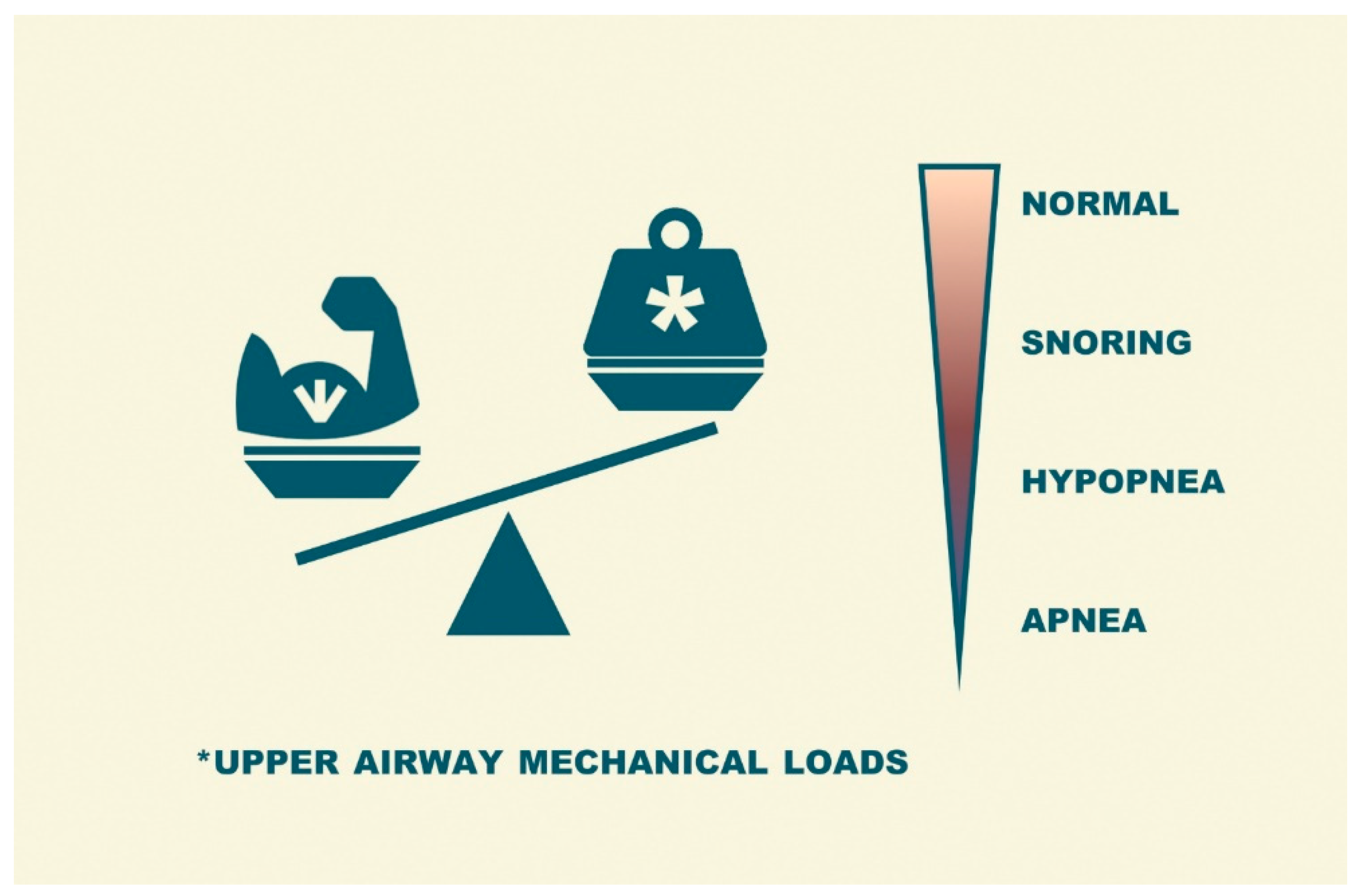
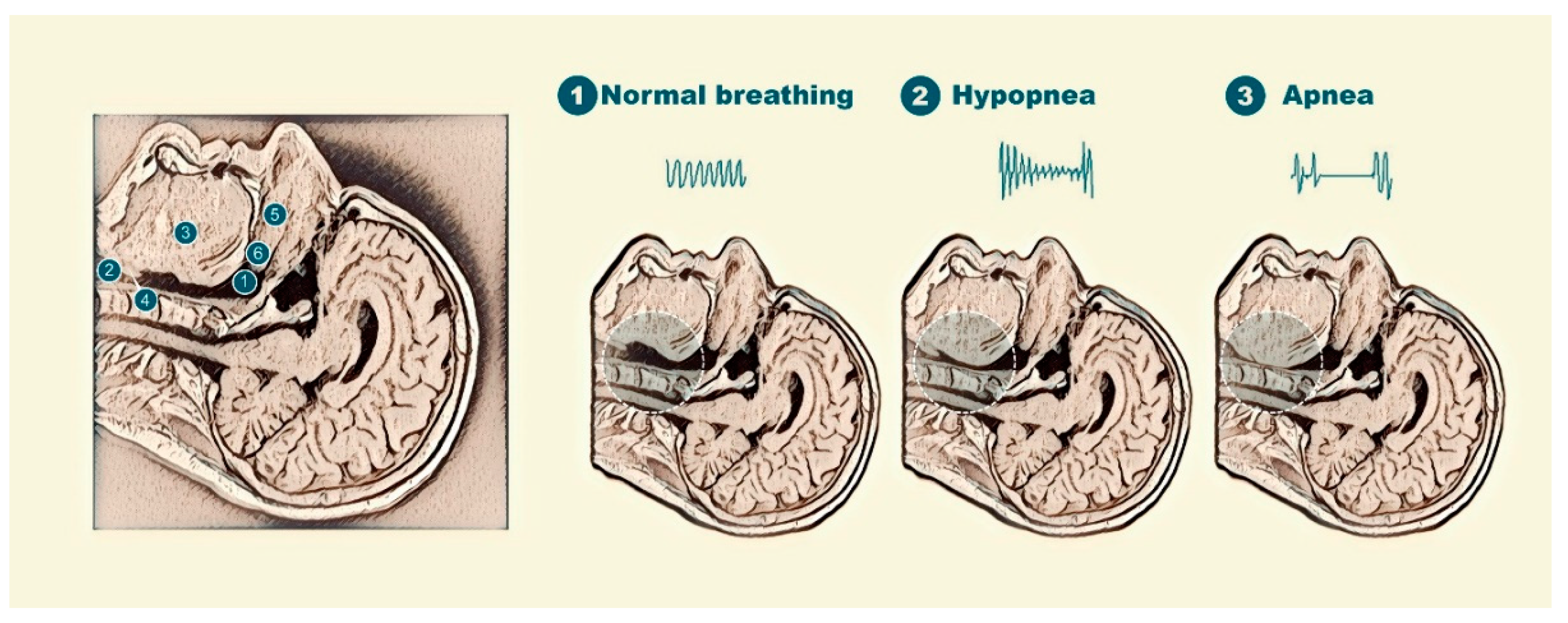
1. Introduction
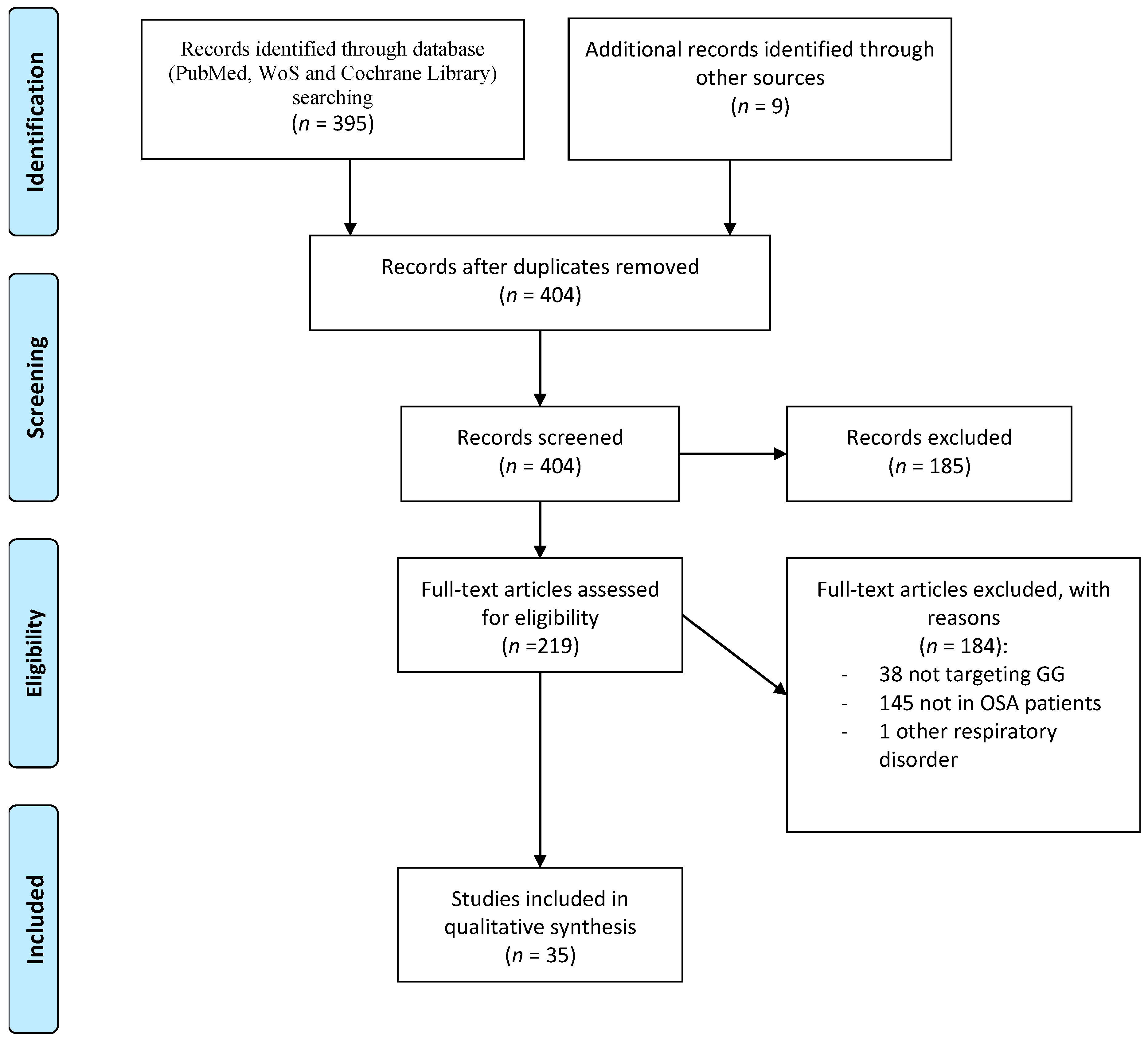
2. Search Strategy and Study Selection
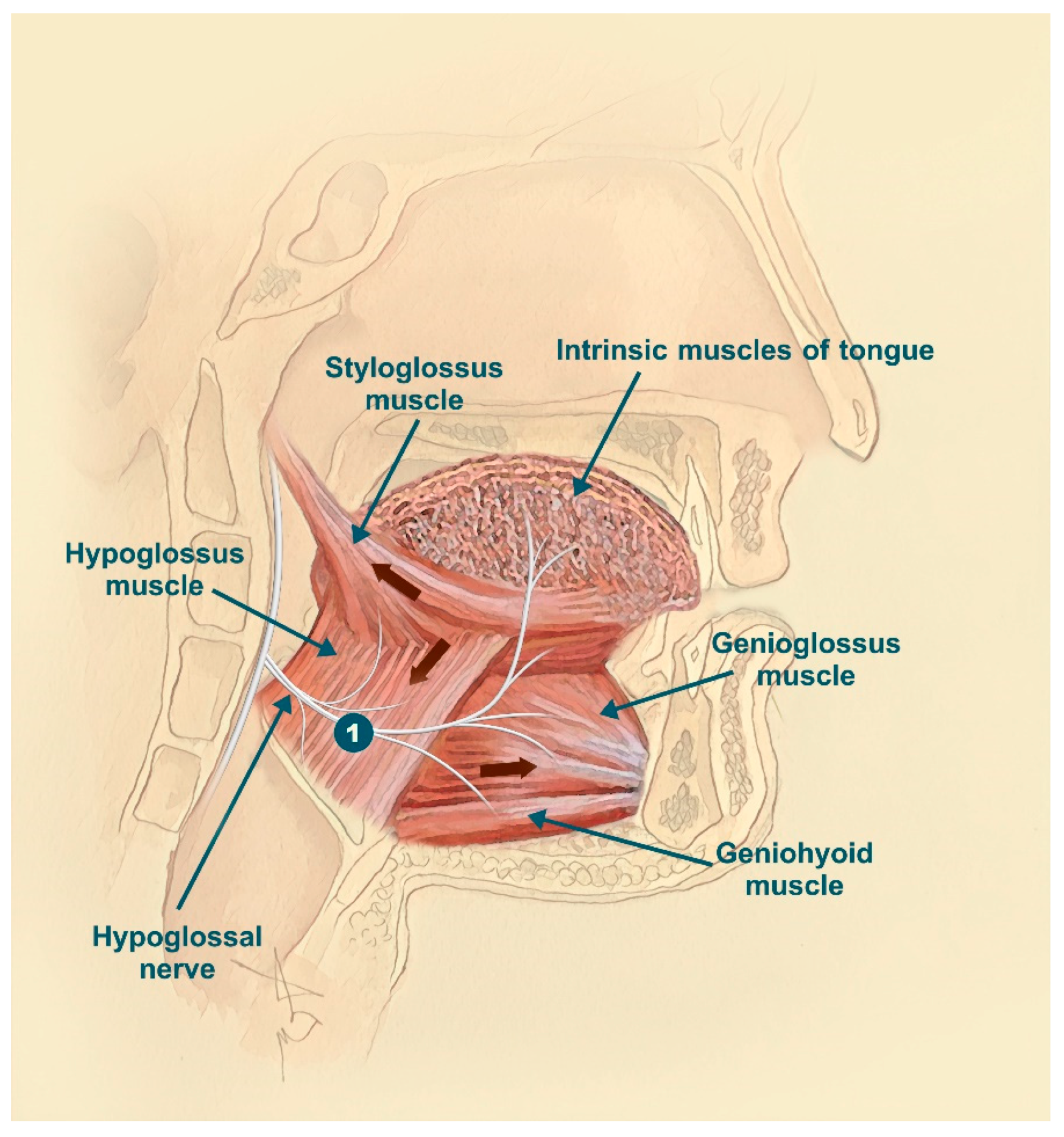
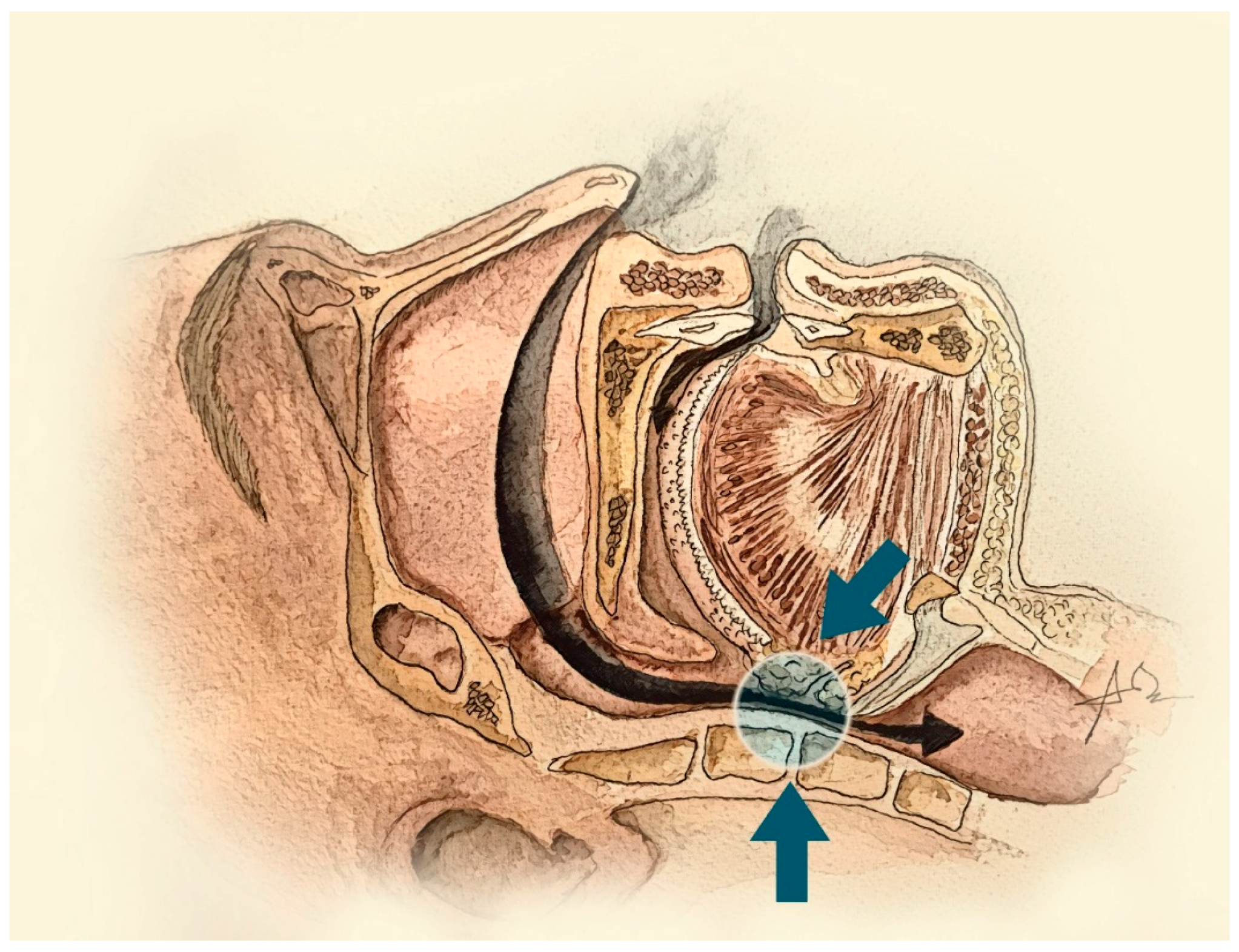
3. The Genioglossus Muscle
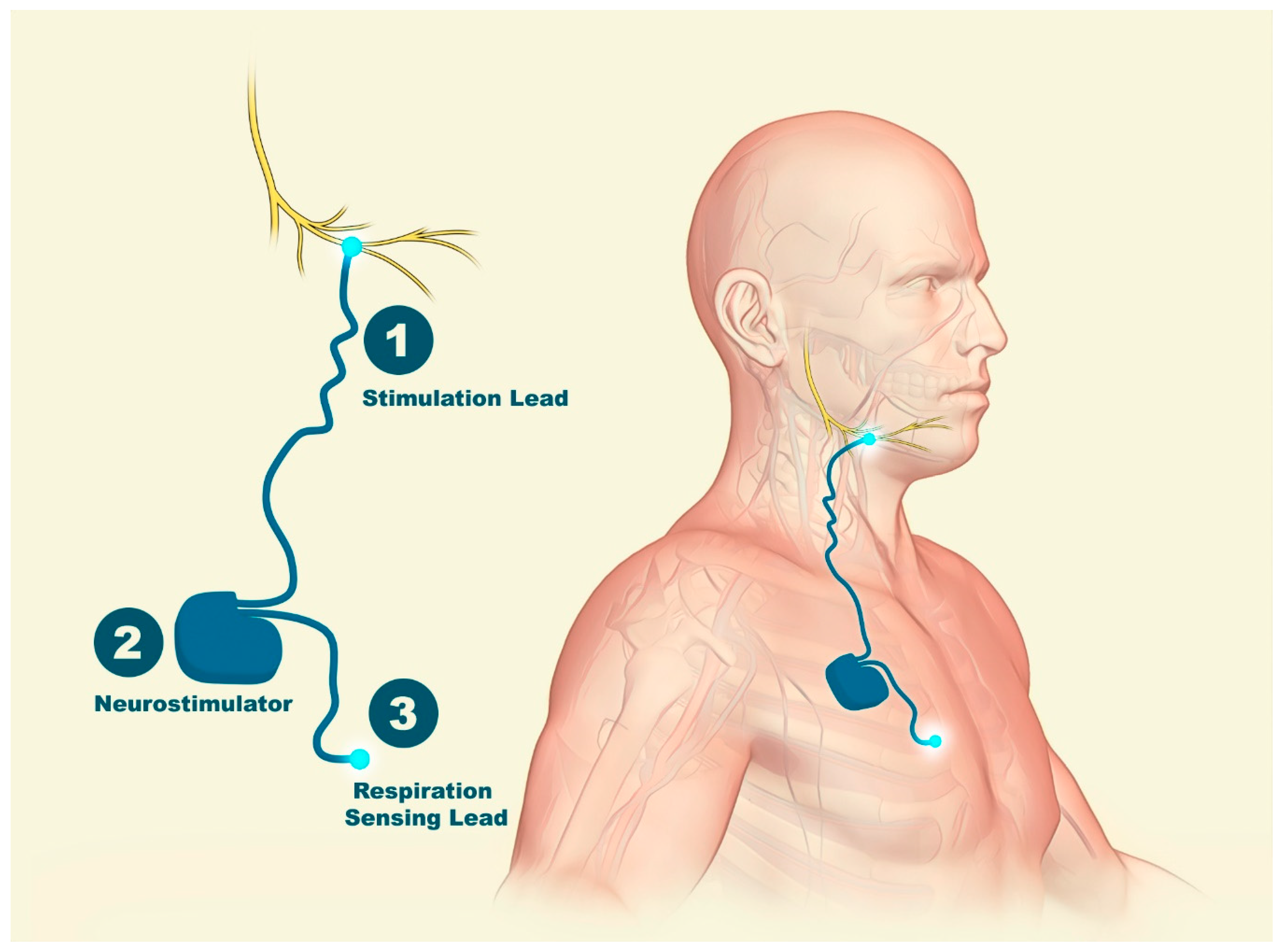
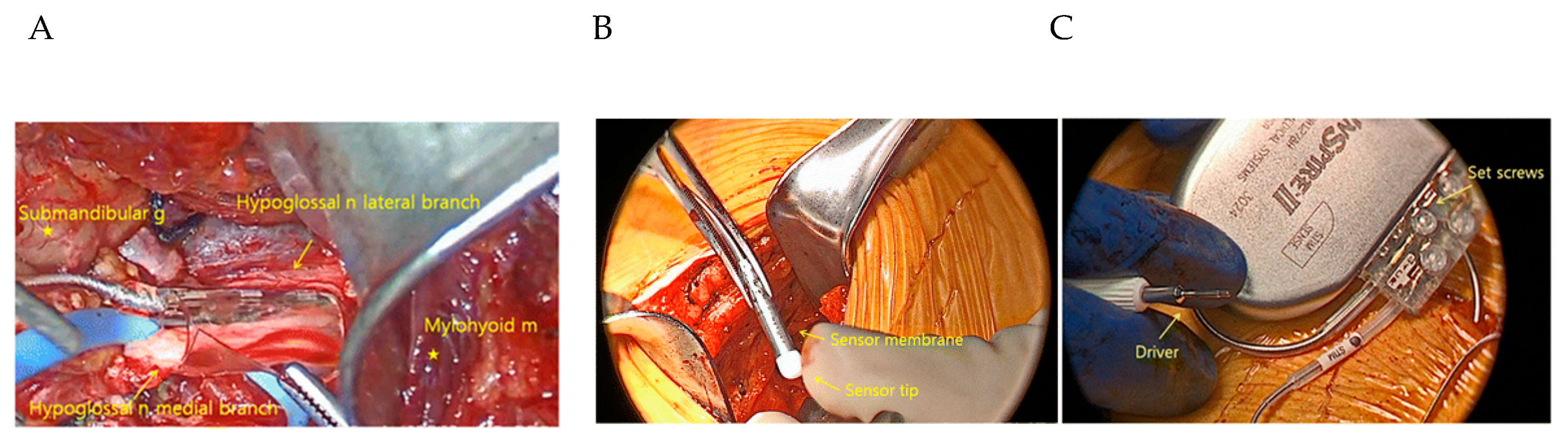
4. Nerve Electrical Stimulation
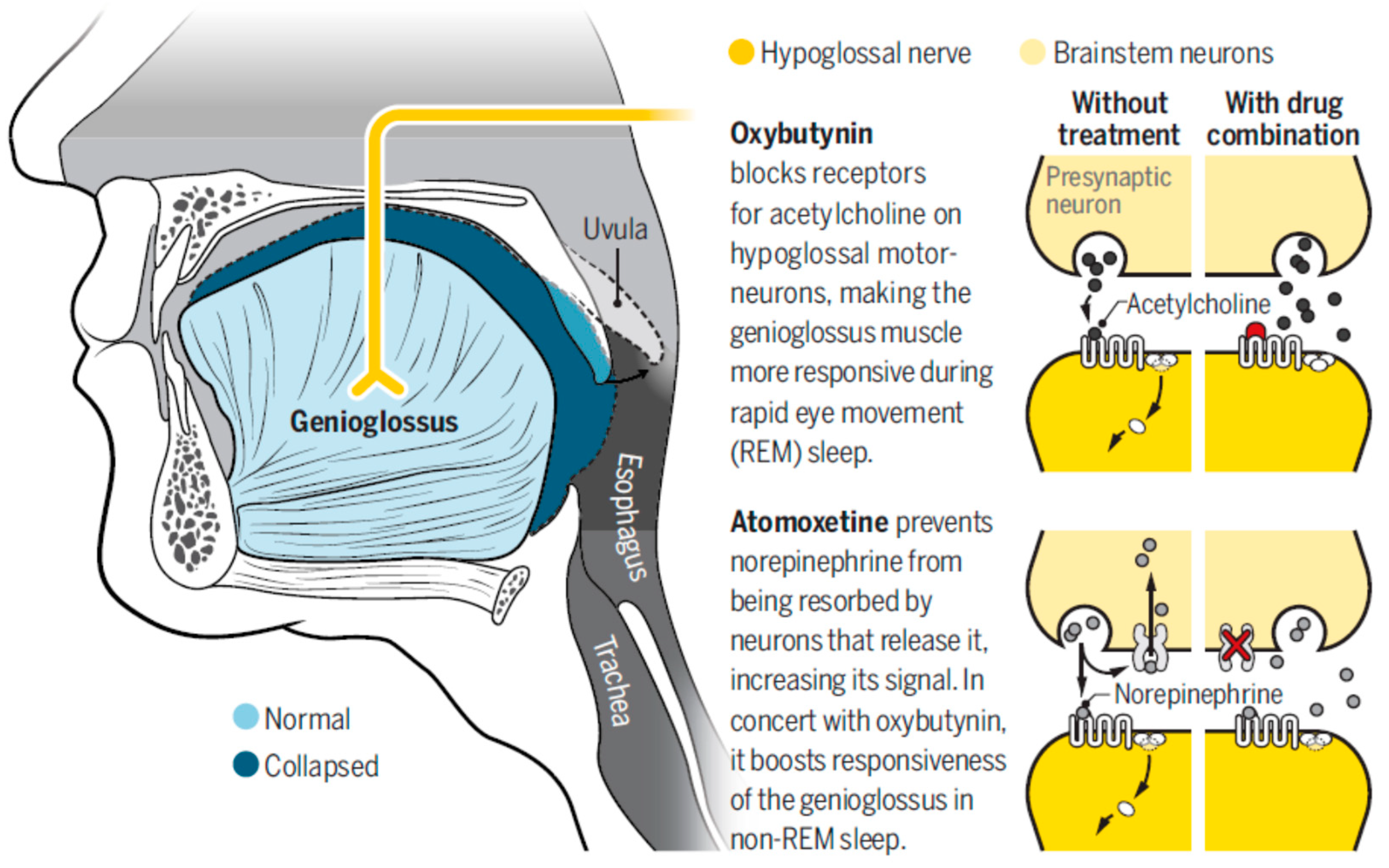
5. Pharmacological Treatment
6. Myofunctional Therapy (MT)
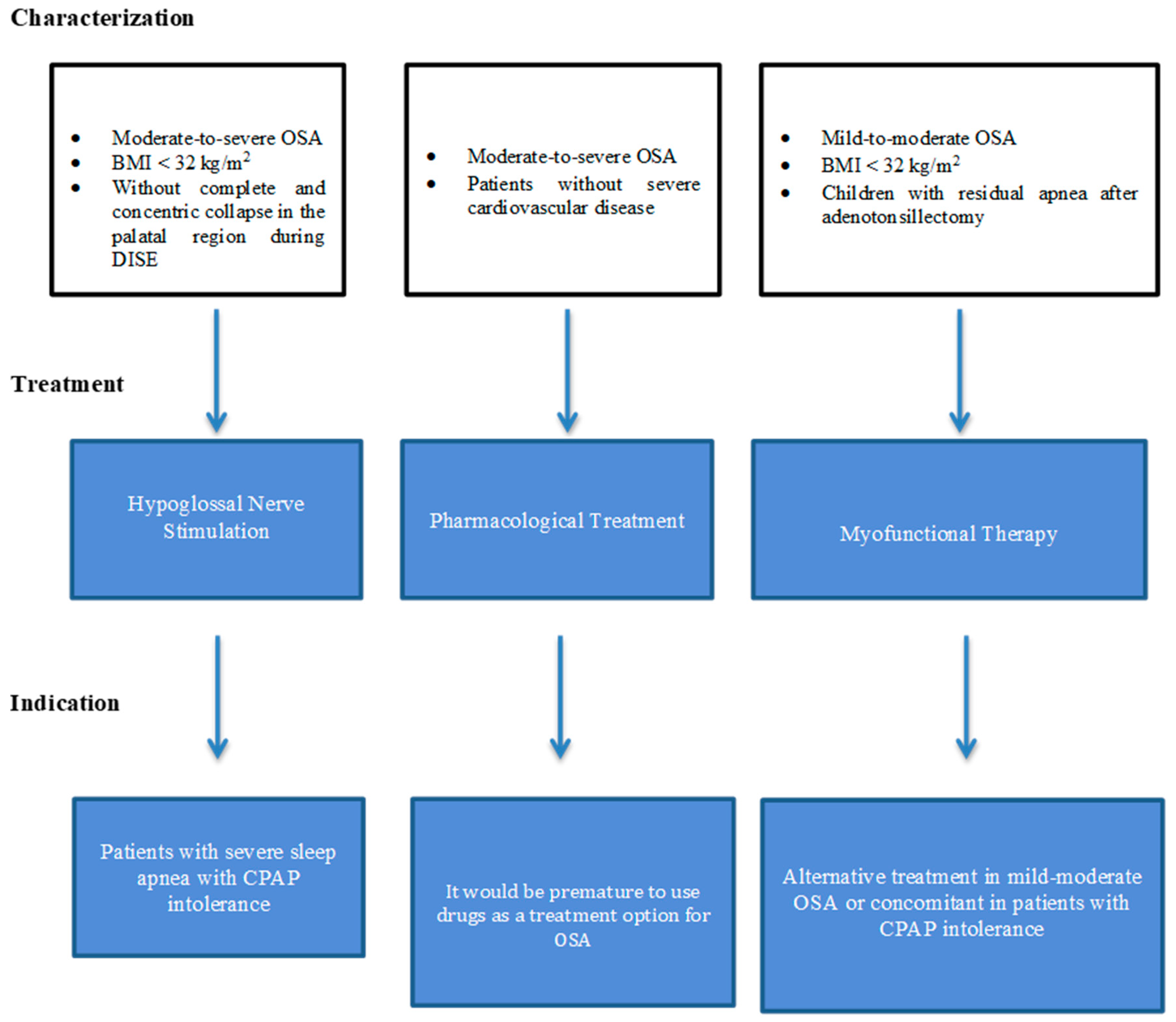
7. Clinical Applicability
8. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Dempsey, J.A.; Veasey, S.C.; Morgan, B.J.; O’Donnell, C.P. Pathophysiology of sleep apnea. Phys. Rev. 2010, 90, 47–112. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.P.; Schneider, H.; Schwartz, A.R.; Smith, P.L. Adult obstructive sleep apnea: Pathophysiology and diagnosis. Chest 2007, 132, 325–337. [Google Scholar] [CrossRef] [PubMed]
- Peppard, P.E.; Young, T.; Barnet, J.H.; Palta, M.; Hagen, E.W.; Hla, K.M. Increased prevalence of sleep-disordered breathing in adults. Am. J. Epidemiol. 2013, 177, 1006–1014. [Google Scholar] [CrossRef] [PubMed]
- Stepnowsky, C.; Sarmiento, K.F.; Bujanover, S.; Villa, K.F.; Li, V.W.; Flores, N.M. Comorbidities, Health-Related Quality of Life, and Work Productivity Among People with Obstructive Sleep Apnea with Excessive Sleepiness: Findings From the 2016 US National Health and Wellness Survey. J. Clin. Sleep Med. 2019, 15, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Terán-Santos, J.; Jiménez-Gómez, A.; Cordero-Guevara, J. The association between sleep apnea and the risk of traffic accidents. Cooperative Group Burgos-Santander. N. Engl. J. Med. 1999, 340, 847–851. [Google Scholar] [CrossRef]
- Marin, J.M.; Carrizo, S.J.; Vicente, E.; Agusti, A.G. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: An observational study. Lancet 2005, 365, 1046–1053. [Google Scholar] [CrossRef]
- Mediano, O.; Cano-Pumarega, I.; Sánchez-de-la-Torre, M.; Alonso-Álvarez, M.L.; Troncoso, M.F.; García-Río, F.; Egea, C.; the Spanish Sleep Network. Upcoming Scenarios for the Comprehensive Management of Obstructive Sleep Apnea: An Overview of the Spanish Sleep Network. Arch. Bronconeumol. 2019. [Google Scholar] [CrossRef]
- Davies, R.J.; Stradling, J.R. The relationship between neck circumference, radiographic pharyngeal anatomy, and the obstructive sleep apnoea syndrome. Eur. Respir. J. 1990, 3, 509–514. [Google Scholar]
- Montserrat, J.M.; Ferrer, M.; Hernandez, L.; Farré, R.; Vilagut, G.; Navajas, D.; Badia, J.R.; Carrasco, E.; De Pablo, J.; Ballester, E. Effectiveness of CPAP treatment in daytime function in sleep apnea syndrome: A randomized controlled study with an optimized placebo. Am. J. Respir. Crit. Care Med. 2001, 164, 608–613. [Google Scholar] [CrossRef]
- McEvoy, R.D.; Antic, N.A.; Heeley, E.; Luo, Y.; Ou, Q.; Zhang, X.; Mediano, O.; Chen, R.; Drager, L.F.; Liu, Z.; et al. SAVE Investigators and Coordinators. CPAP for Prevention of Cardiovascular Events in Obstructive Sleep Apnea. N. Engl. J. Med. 2016, 375, 919–931. [Google Scholar] [CrossRef]
- Parra, O.; Sánchez-Armengol, Á.; Capote, F.; Bonnin, M.; Arboix, A.; Campos-Rodríguez, F.; Pérez-Ronchel, J.; Durán-Cantolla, J.; Martínez-Null, C.; de la Peña, M.; et al. Efficacy of continuous positive airway pressure treatment on 5-year survival in patients with ischaemic stroke and obstructive sleep apnea: A randomized controlled trial. J. Sleep Res. 2015, 24, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, M.; Acosta, L.; Hung, Y.L.; Padilla, M.; Enciso, R. Effects of CPAP and mandibular advancement device treatment in obstructive sleep apnea patients: A systematic review and meta-analysis. Sleep Breath. 2018, 22, 555–568. [Google Scholar] [CrossRef] [PubMed]
- Cori, J.M.; O’Donoghue, F.J.; Jordan, A.S. Sleeping tongue: Current perspectives of genioglossus control in healthy individuals and patients with obstructive sleep apnea. Nat. Sci. Sleep 2018, 10, 169–179. [Google Scholar] [CrossRef] [PubMed]
- Berkovitz, B.K.B.; Holland, G.R.; Moxham, B. Chapter 3: Regional topography of the mouth and related areas. In Oral Anatomy, Histology and Embryology, 5th ed.; Elsevier: Edinburgh, UK, 2018; pp. 70–91. [Google Scholar]
- Worsnop, C.J.; Kay, A.; Pierce, R.J.; Kim, Y.; Trinder, J. Activity of respiratory pump and upper airway muscles during sleep onset. J. Appl. Physiol. 1998, 85, 908–920. [Google Scholar] [CrossRef] [PubMed]
- Remmers, J.E.; deGroot, W.J.; Sauerland, E.K.; Anch, A.M. Pathogenesis of upper airway occlusion during sleep. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 1978, 44, 931–938. [Google Scholar] [CrossRef]
- Certal, V.F.; Zaghi, S.; Riaz, M.; Vieira, A.S.; Pinheiro, C.T.; Kushida, C.; Capasso, R.; Camacho, M. Hypoglossal nerve stimulation in the treatment of obstructive sleep apnea: A systematic review and meta-analysis. Laryngoscope 2015, 125, 1254–1264. [Google Scholar] [CrossRef]
- Miki, H.; Hida, W.; Chonan, T.; Kikuchi, Y.; Takishima, T. Effects of submental electrical stimulation during sleep on upper airway patency in patients with obstructive sleep apnea. Am. Rev. Respir. Dis. 1989, 140, 1285–1289. [Google Scholar] [CrossRef]
- Schwartz, A.R.; Thut, D.C.; Russ, B.; Seelagy, M.; Yuan, X.; Brower, R.G.; Permutt, S.; Wise, R.A.; Smith, P.L. Effect of electrical stimulation of the hypoglossal nerve on airflow mechanics in the isolated upper airway. Am. Rev. Respir. Dis. 1993, 147, 1144–1150. [Google Scholar] [CrossRef]
- Schwartz, A.R.; Bennett, M.L.; Smith, P.L.; De Backer, W.; Hedner, J.; Boudewyns, A.; Van de Heyning, P.; Ejnell, H.; Hochban, W.; Knaack, L.; et al. Therapeutic electrical stimulation of the hypoglossal nerve in obstructive sleep apnea. Arch. Otolaryngol. Head Neck Surg. 2001, 127, 1216–1223. [Google Scholar] [CrossRef]
- Safiruddin, F.; Vanderveken, O.M.; de Vries, N.; Maurer, J.T.; Lee, K.; Ni, Q.; Strohl, K.P. Effect of upper-airway stimulation for obstructive sleep apnoea on airway dimensions. Eur. Respir. J. 2015, 45, 129–138. [Google Scholar] [CrossRef]
- Lorenzi-Filho, G.; Almeida, F.R.; Strollo, P.J. Treating OSA: Current and emerging therapies beyond CPAP. Respirology 2017, 22, 1500–1507. [Google Scholar] [CrossRef] [PubMed]
- Heiser, C.; Hofauer, B.; Lozier, L.; Woodson, B.T.; Stark, T. Nerve monitoring-guided selective hypoglossal nerve stimulation in obstructive sleep apnea patients. Laryngoscope 2016, 126, 2852–2858. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.O.; Chen, Y.F.; Jung, J.; Kwon, Y.D.; Liu, S.Y.C. Hypoglossal nerve stimulation for treatment of obstructive sleep apnea (OSA): a primer for oral and maxillofacial surgeons. Maxillofac. Plast. Reconstr. Surg. 2017, 39, 27. [Google Scholar] [CrossRef] [PubMed]
- Bisogni, V.; Pengo, M.F.; De Vito, A.; Maiolino, G.; Rossi, G.P.; Moxham, J.; Steier, J. Electrical stimulation for the treatment of obstructive sleep apnoea: A review of the evidence. Expert Rev. Respir. Med. 2017, 11, 711–720. [Google Scholar] [CrossRef] [PubMed]
- Eastwood, P.R.; Barnes, M.; Walsh, J.H.; Hee, G.; Schwartz, A.R.; Smith, P.L.; Malhotra, A.; McEvoy, R.D.; Wheatley, J.R.; O’Donoghue, F.J.; et al. Treating obstructive sleep apnea with hypoglossal nerve stimulation. Sleep 2011, 34, 1479–1486. [Google Scholar] [CrossRef]
- Goding, G.S., Jr.; Tesfayesus, W.; Kezirian, E.J. Hypoglossal nerve stimulation and airway changes under fluoroscopy. Otolaryngol. Head Neck Surg. 2012, 146, 1017–1022. [Google Scholar] [CrossRef]
- Mwenge, G.B.; Rombaux, P.; Dury, M.; Lengelé, B.; Rodenstein, D. Targeted hypoglossal neurostimulation for obstructive sleep apnoea: A 1-year pilot study. Eur. Respir. J. 2013, 41, 360–367. [Google Scholar] [CrossRef]
- Van de Heyning, P.H.; Badr, M.S.; Baskin, J.Z.; Cramer Bornemann, M.A.; De Backer, W.A.; Dotan, Y.; Woodson, B.T. Implanted upper airway stimulation device for obstructive sleep apnea. Laryngoscope 2012, 122, 1626–1633. [Google Scholar] [CrossRef]
- Vanderveken, O.M.; Beyers, J.; Op de Beeck, S.; Dieltjens, M.; Willemen, M.; Verbraecken, J.A.; De Backer, W.A.; Van de Heyning, P.H. Development of a Clinical Pathway and Technical Aspects of Upper Airway Stimulation Therapy for Obstructive Sleep Apnea. Front. Neurosci. 2017, 11, 523. [Google Scholar] [CrossRef]
- Strollo, P.J., Jr.; Soose, R.J.; Maurer, J.T.; de Vries, N.; Cornelius, J.; Froymovich, O.; Hanson, R.D.; Padhya, T.A.; Steward, D.L.; Gillespie, M.B.; et al. Upper-airway stimulation for obstructive sleep apnea. STAR Trial Group N. Engl. J. Med. 2014, 370, 139–149. [Google Scholar] [CrossRef]
- Woodson, B.T.; Soose, R.J.; Gillespie, M.B.; Strohl, K.P.; Maurer, J.T.; de Vries, N.; Steward, D.L.; Baskin, J.Z.; Badr, M.S.; Lin, H.S.; et al. Three-year outcomes of cranial nerve stimulation for obstructive sleep apnea: The STAR trial. Otolaryngol. Head Neck Surg. 2016, 154, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, M.B.; Soose, R.J.; Woodson, B.T.; Strohl, K.P.; Maurer, J.T.; de Vries, N.; Steward, D.L.; Baskin, J.Z.; Badr, M.S.; Lin, H.S.; et al. Upper airway stimulation for obstructive sleep apnea: Patient-reported outcomes after 48 months of follow-up. Otolaryngol. Head Neck Surg. 2017, 156, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Fleury Curado, T.; Oliven, A.; Sennes, L.U.; Polotsky, V.Y.; Eisele, D.; Schwartz, A.R. Neurostimulation Treatment of OSA. Chest 2018, 154, 1435–1447. [Google Scholar] [CrossRef] [PubMed]
- Veasey, S.C. Serotonin agonists and antagonists in obstructive sleep apnea: Therapeutic potential. Am. J. Respir. Med. 2003, 2, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Fenik, V.B.; Davies, R.O.; Kubin, L. REM sleep-like atonia of hypoglossal (XII) motoneurons is caused by loss of noradrenergic and serotonergic inputs. Am. J. Respir. Crit. Care Med. 2005, 172, 1322–1330. [Google Scholar] [CrossRef]
- Berry, R.B.; Yamaura, E.M.; Gill, K.; Reist, C. Acute effects of paroxetine on genioglossus activity in obstructive sleep apnea. Sleep 1999, 22, 1087–1092. [Google Scholar] [CrossRef][Green Version]
- Prasad, B.; Radulovacki, M.; Olopade, C.; Herdegen, J.J.; Logan, T.; Carley, D.W. Prospective trial of efficacy and safety of ondansetron and fluoxetine in patients with obstructive sleep apnea syndrome. Sleep 2010, 33, 982–989. [Google Scholar] [CrossRef][Green Version]
- Chan, E.; Steenland, H.W.; Liu, H.; Horner, R.L. Endogenous excitatory drive modulating respiratory muscle activity across sleep–wake states. Am. J. Respir. Crit. Care Med. 2006, 174, 1264–1273. [Google Scholar] [CrossRef]
- Taranto-Montemurro, L.; Edwards, B.A.; Sands, S.A.; Marques, M.; Eckert, D.J.; White, D.P.; Wellman, A. Desipramine Increases Genioglossus Activity and Reduces Upper Airway Collapsibility during Non-REM Sleep in Healthy Subjects. Am. J. Respir. Crit. Care Med. 2016, 194, 878–885. [Google Scholar] [CrossRef]
- Taranto-Montemurro, L.; Sands, S.A.; Edwards, B.A.; Azarbarzin, A.; Marques, M.; de Melo, C.; Eckert, D.J.; White, D.P.; Wellman, A. Desipramine improves upper airway collapsibility and reduces OSA severity in patients with minimal muscle compensation. Eur. Respir. J. 2016, 48, 1340–1350. [Google Scholar] [CrossRef]
- Grace, K.P.; Hughes, S.W.; Horner, R.L. Identification of the mechanism mediating genioglossus muscle suppression in REM sleep. Am. J. Respir. Crit. Care Med. 2013, 187, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Taranto-Montemurro, L.; Messineo, L.; Sands, S.A.; Azarbarzin, A.; Marques, M.; Edwards, B.A.; Eckert, D.J.; White, D.P.; Wellman, A. The Combination of Atomoxetine and Oxybutynin Greatly Reduces Obstructive Sleep Apnea Severity: A Randomized, Placebo-Controlled, Double-Blind Crossover Trial. Am. J. Respir. Crit. Care Med. 2019, 199, 1267–1276. [Google Scholar] [CrossRef] [PubMed]
- Wadman, M. Drug pair shows promise for treating sleep apnea. Science 2018, 361, 1174–1175. [Google Scholar] [CrossRef] [PubMed]
- Eckert, D.J.; White, D.P.; Jordan, A.S.; Malhotra, A.; Wellman, A. Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets. Am. J. Crit. Care Med. 2013, 188, 996–1004. [Google Scholar] [CrossRef]
- Guilleminault, C.; Huang, Y.S. From oral facial dysfunction to dysmorphism and the onset of pediatric OSA. Sleep Med. Rev. 2018, 40, 203–214. [Google Scholar] [CrossRef]
- Genta, P.R.; Sands, S.A.; Butler, J.P.; Loring, S.H.; Katz, E.S.; Demko, B.G.; Kezirian, E.J.; White, D.P.; Wellman, A. Airflow shape is associated with the pharyngeal structure causing OSA. Chest 2017, 152, 537–546. [Google Scholar] [CrossRef]
- Hirata, R.P.; Schorr, F.; Kayamori, F.; Moriya, H.T.; Romano, S.; Insalaco, G.; Gebrim, E.M.; de Oliveira, L.V.; Genta, P.R.; Lorenzi-Filho, G. Upper airway collapsibility assessed by negative expiratory pressure while awake is associated with upper airway anatomy. J. Clin. Sleep Med. 2016, 12, 1339–1346. [Google Scholar] [CrossRef]
- Guimarães, K.C.; Drager, L.F.; Genta, P.R.; Marcondes, B.F.; Lorenzi-Filho, G. Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. Am. J. Respir. Crit. Care Med. 2009, 179, 962–966. [Google Scholar] [CrossRef]
- Rogers, A.P. Exercises for the development of muscles of face with view to increasing their functional activity. Dent. Cosm. LX 1918, 59, 857–876. [Google Scholar] [CrossRef]
- Guimarães, K.C. Soft tissue changes of the oropharynx in patients with obstructive sleep apnea. J. Bras. Fonoaudiol. 1999, 1, 69–75. [Google Scholar]
- Guilleminault, C.; Huang, Y.S.; Monteyrol, P.J.; Sato, R.; Quo, S.; Lin, C.H. Critical role of myofascial reeducation in pediatric sleep-disordered breathing. Sleep Med. 2013, 14, 518–525. [Google Scholar] [CrossRef] [PubMed]
- Steele, C.M. On the plausibility of upper airway remodeling as an outcome of orofacial exercise. Am. J. Respir. Crit. Care Med. 2009, 179, 858–859. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Watanabe, A.; Akihiro, Y.; Takao, M.; Ikematsu, T.; Kimoto, S.; Asano, T.; Kawara, M. Pilot study to assess the potential of oral myofunctional therapy for improving respiration during sleep. J. Prosthodont. Res. 2013, 57, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Diaferia, G.; Badke, L.; Santos-Silva, R.; Bommarito, S.; Tufik, S.; Bittencourt, L. Effect of speech therapy as adjunct treatment to continuous positive airway pressure on the quality of life of patients with obstructive sleep apnea. Sleep Med. 2013, 14, 628–635. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, E.; Tonisi, G.A.B.R.; Vecina, A.L.C.; Inocêncio, L.B.; Guimarães, K.C.C.; Nemr, N.K. A percepção do acompanhante e do indivíduo com ronco/saos antes e após fonoterapia [Perception of the bed partner and the individual suffering from SNORING/OSAS before and after speech therapy]. Rev. CEFAC 2014, 16, 907–916. [Google Scholar] [CrossRef]
- Diaféria, G.; Santos-Silva, R.; Truksinas, E.; Haddad, F.L.M.; Santos, R.; Bommarito, S.; Gregório, L.C.; Tufik, S.; Bittencourt, L. Myofunctional therapy improves adherence to continuous positive airway pressure treatment. Sleep Breath. 2017, 21, 387–395. [Google Scholar] [CrossRef]
- Ieto, V.; Kayamori, F.; Montes, M.I.; Hirata, R.P.; Gregório, M.G.; Alencar, A.M.; Drager, L.F.; Genta, P.R.; Lorenzi-Filho, G. Effects of oropharyngeal exercises on snoring: A randomized trial. Chest 2015, 148, 683–691. [Google Scholar] [CrossRef]
- Camacho, M.; Certal, V.; Abdullatif, J.; Zaghi, S.; Ruoff, C.M.; Capasso, R.; Kushida, C.A. Myofunctional therapy to treat obstructive sleep apnea: A systematic review and meta-analysis. Sleep 2015, 38, 669–675. [Google Scholar] [CrossRef]
- Baz, H.; Elshafey, M.; Elmorsy, S.; Abu-Samra, M. The role of oral myofunctional therapy in managing patients with mild to moderate obstructive sleep apnea. PAN Arab J. Rhinol. 2012, 2, 17–22. [Google Scholar]
- Verma, R.K.; Johnson, J., Jr.; Goyal, M.; Banumathy, N.; Goswami, U.; Panda, N.K. Oropharyngeal exercises in the treatment of obstructive sleep apnoea: Our experience. Sleep Breath. 2016, 20, 1193–1201. [Google Scholar] [CrossRef]
- Mohamed, A.S.; Sharshar, R.S.; Elkolaly, R.M.; Serageldin, M. Upper airway muscle exercises outcome in patients with obstructive sleep apnea syndrome. Egypt J. Chest Dis. Tuberc. 2017, 66, 121–125. [Google Scholar] [CrossRef]
- Felício, C.M.; Silva Dias, F.V.; Trawitzki, L.V.V. Obstructive sleep apnea: Focus on myofunctional therapy. Nat. Sci. Sleep 2018, 10, 271–286. [Google Scholar] [CrossRef] [PubMed]
- Villa, M.P.; Brasili, L.; Ferretti, A.; Vitelli, O.; Rabasco, J.; Mazzotta, A.R.; Pietropaoli, N.; Martella, S. Oropharyngeal exercises to reduce symptoms of OSA after AT. Sleep Breath. 2015, 19, 281–289. [Google Scholar] [CrossRef] [PubMed]
| Reference | Severity | n | Treatment | Follow-Up | Main Effect | Conclusion |
|---|---|---|---|---|---|---|
| Hypoglossal Nerve Electrical Stimulation | ||||||
| Strollo, 2014 [31] | Moderate to severe OSA | 126 | Inspire II Upper Airway Stimulation | 12 months | Decreases AHI 68% (from 29.3 to 9.0 events/h). Decreases ODI score 70% (from 25.4 to 7 events/h). Improve EDS and quality of life. | (1) Safe and effective for the treatment of moderate to severe OSA. (2) Could be an alternative to CPAP. (3) Significant improvements in objective (AHI) and subjective measurements. (4) Its invasive nature limits its application. |
| Woodson, 2016 [32] | Moderate to severe OSA | 116 | Inspire II Upper Airway Stimulation | 36 months | Decreases AHI > 50% (from 28.2 to 6.2 events/h). Improves quality of life. | |
| Gillespie, 2017 [33] | Moderate to severe OSA | 91 | Inspire II Upper Airway Stimulation | 48 months | Improves ESS and quality of life. | |
| Pharmacological Treatment | ||||||
| Berri, 1999 [37] | Severe OSA | 8 | Paroxetine | Single dose | Increases peak inspiratory GG activity during NREM. Does not improve AHI. | (1) Exciting new possibilities for OSA treatment. (2) Probably suitable for a determined phenotype of patients and/or in combination with another treatments. (3) It would be premature to use this combination as a treatment option for OSA at present. |
| Prasad, 2010 [38] | AHI > 10 | 35 | Ondansetron + fluoxetine | Days 7, 14 and 28 | Decreases AHI 40% at high dose (12.9 events/h reduction in AHI). Does not improve EDS. | |
| Taranto-Montemurro, 2016 [41] | AHI > 15 | 14 | Desipramine | Single dose | Decreases pharyngeal collapsibility (Pcrit). Very little effect on AHI. | |
| Taranto-Montemurro, 2019 [43] | 15/20 patients with OSA on placebo (AHI>10 events/h) | 20 | Atomoxetine + oxybutynin | Single dose | Median AHI change of 63% (from 28.5 to 7.5 events/h). Increases nadir oxygen saturation. Increases GG responsiveness. | |
| Myofunctional Therapy | ||||||
| Guimarães, 2009 [49] | Moderate OSA | 31 | Upper airway exercises | 3 months | Decreases AHI from 22.4 to 13.7/h. Increases nadir oxygen saturation. Improves EDS. | (1) It could be a useful tool in nonobese patients with mild to moderate OSA. (2) Can improve the effectiveness or patient adherence of CPAP treatment by reducing the absolute pressure required. (3) One of the most important limitation is that it requires high patient adherence to the therapy. |
| Diaferia, 2013 [55] | Moderate to severe OSA | 100 | Speech therapy | 3 months | Improves quality of life. | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mediano, O.; Romero-Peralta, S.; Resano, P.; Cano-Pumarega, I.; Sánchez-de-la-Torre, M.; Castillo-García, M.; Martínez-Sánchez, A.B.; Ortigado, A.; García-Río, F. Obstructive Sleep Apnea: Emerging Treatments Targeting the Genioglossus Muscle. J. Clin. Med. 2019, 8, 1754. https://doi.org/10.3390/jcm8101754
Mediano O, Romero-Peralta S, Resano P, Cano-Pumarega I, Sánchez-de-la-Torre M, Castillo-García M, Martínez-Sánchez AB, Ortigado A, García-Río F. Obstructive Sleep Apnea: Emerging Treatments Targeting the Genioglossus Muscle. Journal of Clinical Medicine. 2019; 8(10):1754. https://doi.org/10.3390/jcm8101754
Chicago/Turabian StyleMediano, Olga, Sofia Romero-Peralta, Pilar Resano, Irene Cano-Pumarega, Manuel Sánchez-de-la-Torre, María Castillo-García, Ana Belén Martínez-Sánchez, Ana Ortigado, and Francisco García-Río. 2019. "Obstructive Sleep Apnea: Emerging Treatments Targeting the Genioglossus Muscle" Journal of Clinical Medicine 8, no. 10: 1754. https://doi.org/10.3390/jcm8101754
APA StyleMediano, O., Romero-Peralta, S., Resano, P., Cano-Pumarega, I., Sánchez-de-la-Torre, M., Castillo-García, M., Martínez-Sánchez, A. B., Ortigado, A., & García-Río, F. (2019). Obstructive Sleep Apnea: Emerging Treatments Targeting the Genioglossus Muscle. Journal of Clinical Medicine, 8(10), 1754. https://doi.org/10.3390/jcm8101754





