Urinary Epidermal Growth Factor/Creatinine Ratio and Graft Failure in Renal Transplant Recipients: A Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
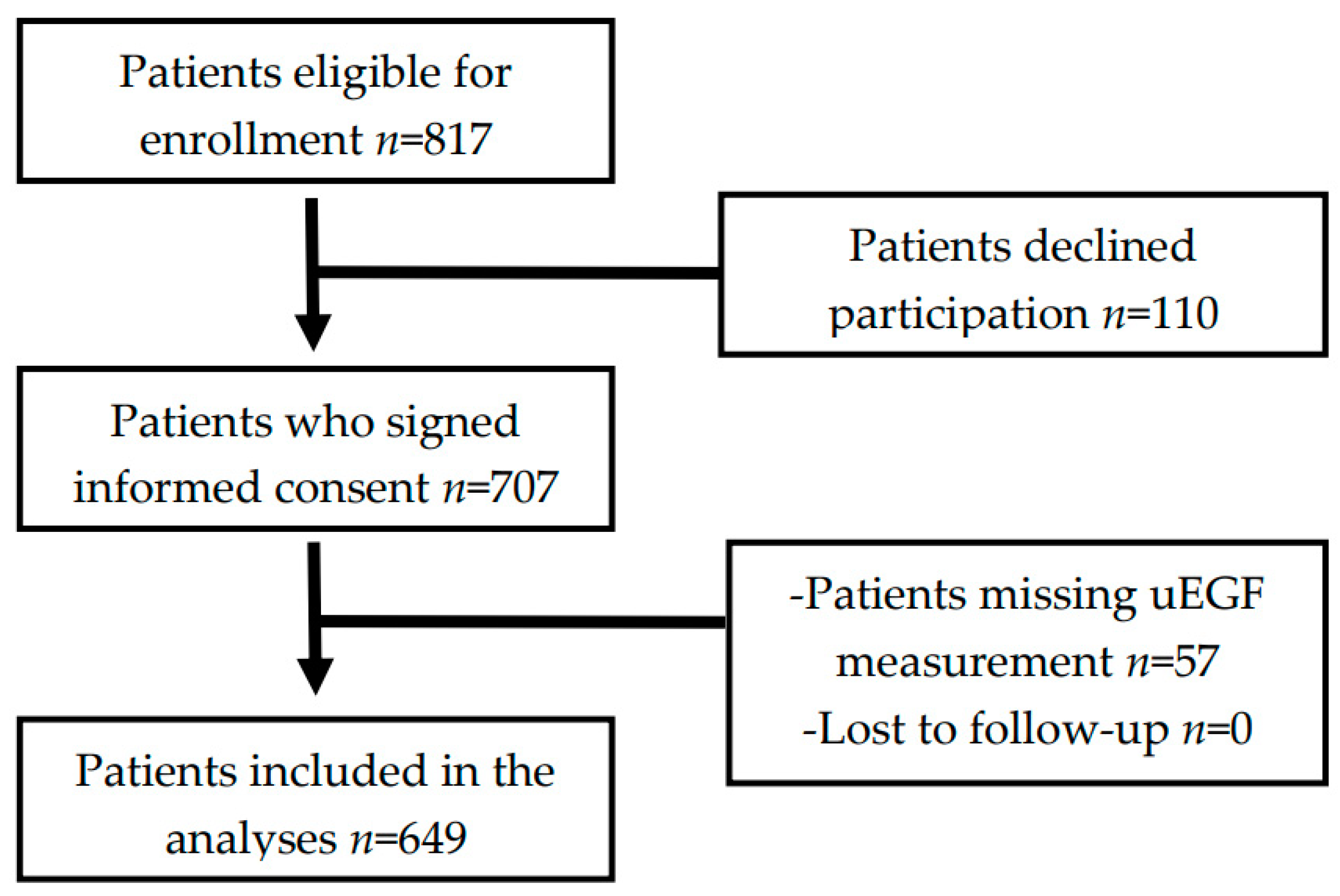
2.1. Study Design and Patient Population
2.2. Data Collection
2.3. Laboratory Measurements and Calculations
2.4. Statistical Analysis
3. Results
3.1. Characteristics at Enrollment
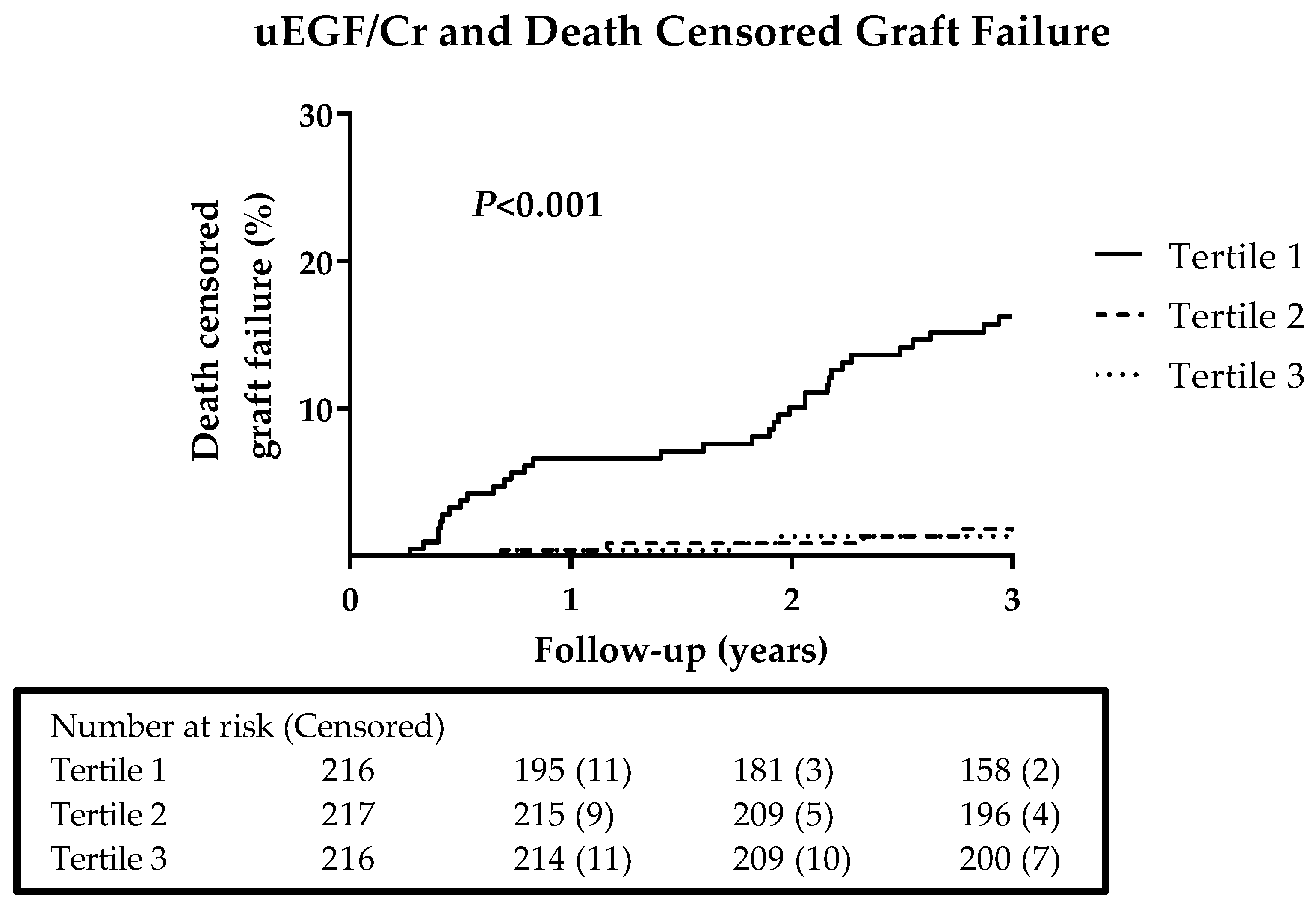
3.2. Prospective Analyses on Graft Failure
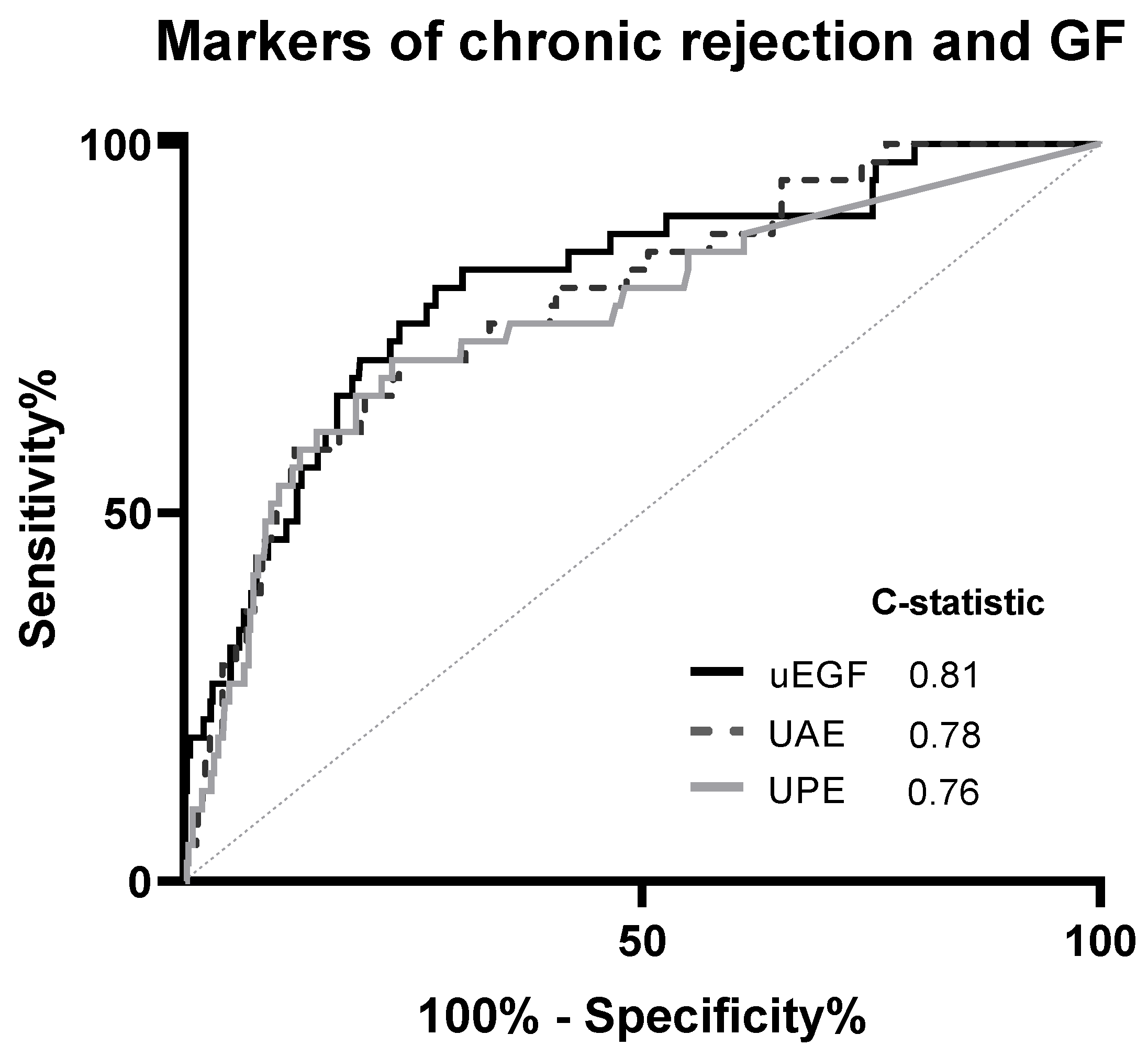
3.3. Secondary and Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Meier-Kriesche, H.-U.; Schold, J.D.; Srinivas, T.R.; Kaplan, B. Lack of Improvement in Renal Allograft Survival Despite a Marked Decrease in Acute Rejection Rates Over the Most Recent Era. Am. J. Transplant. 2004, 4, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Kloc, M.; Ghobrial, R.M. Chronic allograft rejection: A significant hurdle to transplant success. Burn Trauma 2014, 2, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Ponticelli, C. Progression of renal damage in chronic rejection. Kidney Int. 2000, 75, S62–S70. [Google Scholar] [CrossRef]
- Schratzberger, G.; Gert, M. Chronic allograft failure: A disease we don’t understand and can’t cure? Nephrol. Dial. Transplant. 2002, 17, 1384–1390. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McLaren, A.J.; Fuggle, S.V.; Welsh, K.I.; Gray, D.W.R.; Phil, D.; Morris, P.J. Chronic Allograft Failure in Human Renal Transplantation. A Multivariate Risk Factor Analysis. Ann. Surg. 2000, 232, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Nauta, F.L.; Bakker, S.J.L.; van Oeveren, W.; Navis, G.; van der Heide, J.J.H.; van Goor, H.; de Jong, P.E.; Gansevoort, R.T. Albuminuria, proteinuria, and novel urine biomarkers as predictors of long-term allograft outcomes in kidney transplant recipients. Am. J. Kidney Dis. 2011, 57, 733–743. [Google Scholar] [CrossRef] [PubMed]
- Stein-Oakley, A.N.; Tzanidis, A.; Fuller, P.J.; Jablonski, P.; Thomson, N.M. Expression and distribution of epidermal growth factor in acute and chronic renal allograft rejection. Kidney Int. 1994, 46, 1207–1215. [Google Scholar] [CrossRef] [PubMed]
- Worawichawong, S.; Radinahamed, P.; Muntham, D.; Sathirapongsasuti, N.; Nongnuch, A.; Assanatham, M.; Kitiyakara, C. Urine Epidermal Growth Factor, Monocyte Chemoattractant Protein-1 or Their Ratio as Biomarkers for Interstitial Fibrosis and Tubular Atrophy in Primary Glomerulonephritis. Kidney Blood Press Res. 2016, 41, 997–1007. [Google Scholar] [CrossRef]
- Harskamp, L.R.; Gansevoort, R.T.; van Goor, H.; Meijer, E. The epidermal growth factor receptor pathway in chronic kidney diseases. Nat. Rev. Nephrol. 2016, 12, 496. [Google Scholar] [CrossRef]
- Yarden, Y.; Sliwkowski, M.X. Untangling the ErbB signalling network. Nat. Rev. Mol. Cell Biol. 2001, 2, 127. [Google Scholar] [CrossRef]
- Schlessinger, J. Ligand-Induced, Receptor-Mediated Dimerization and Activation of EGF Receptor. Cell 2002, 110, 669–672. [Google Scholar] [CrossRef]
- Klein, J.; Bascands, J.-L.; Buffin-Meyer, B.; Schanstra, J.P. Epidermal growth factor and kidney disease: A long-lasting story. Kidney Int. 2016, 89, 985–987. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.; Liu, N.; Zhuang, S. Role of epidermal growth factor receptor in acute and chronic kidney injury. Kidney Int. 2013, 83, 804–810. [Google Scholar] [CrossRef] [PubMed]
- Isaka, Y. Epidermal growth factor as a prognostic biomarker in chronic kidney diseases. Ann. Transl. Med. 2016, 4 (Suppl. 1), S62. [Google Scholar] [CrossRef]
- Ju, W.; Nair, V.; Smith, S.; Zhu, L.; Shedden, K.; Song, P.X.K.; Mariani, L.H.; Eichinger, F.H.; Berthier, C.C.; Randolph, A.; et al. Tissue transcriptome-driven identification of epidermal growth factor as a chronic kidney disease biomarker. Sci. Transl. Med. 2015, 7, 316ra193. [Google Scholar] [CrossRef] [PubMed]
- van den Berg, E.; Geleijnse, J.M.; Brink, E.J.; van Baak, M.A.; Homan van der Heide, J.J.; Gans, R.O.B.; Navis, G.; Bakker, S.J.L. Sodium intake and blood pressure in renal transplant recipients. Nephrol. Dial. Transplant. 2012, 27, 3352–3359. [Google Scholar] [CrossRef]
- van den Berg, E.; Engberink, M.; Brink, E.; van Baak, M.; Gans, R.; Navis, G.; Bakker, S. Dietary protein, blood pressure and renal function in renal transplant recipients. Br. J. Nutr. 2013, 109, 1463–1470. [Google Scholar] [CrossRef] [PubMed]
- De Vries, A.P.J.; Bakker, S.J.L.; Van Son, W.J.; Van Der Heide, J.J.H.; Ploeg, R.J.; The, H.T.; De Jong, P.E.; Gans, R.O.B. Metabolic Syndrome Is Associated with Impaired Long-term Renal Allograft Function; Not All Component criteria Contribute Equally. Am. J. Transplant. 2004, 4, 1675–1683. [Google Scholar] [CrossRef]
- Du Bois, D.; Du Bois, E.F. A formula to estimate the approximate surface area if height and weight be known. Nutrition 1989, 5, 303–311. [Google Scholar]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F.; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Kok, H.M.; Falke, L.L.; Goldschmeding, R.; Nguyen, T.Q. Targeting CTGF, EGF and PDGF pathways to prevent progression of kidney disease. Nat. Rev. Nephrol 2014, 10, 700–711. [Google Scholar] [CrossRef] [PubMed]
- Amado, J.A.; De-Francisco, A.L.M.; Botana, M.A.; Pesquera, C.; Vázquez-de-Prada, J.A.; Arias, M. Influence of kidney or heart transplantation on the urinary excretion of epidermal growth factor. Transpl. Int. 1994, 7, 127–130. [Google Scholar] [CrossRef] [PubMed]
- Rayego-Mateos, S.; Rodrigues-Diez, R.; Morgado-Pascual, J.L.; Valentijn, F.; Valdivielso, J.M.; Goldschmeding, R.; Ruiz-Ortega, M. Role of Epidermal Growth Factor Receptor (EGFR) and Its Ligands in Kidney Inflammation and Damage. Mediat. Inflamm. 2018, 2018, e8739473. [Google Scholar] [CrossRef] [PubMed]
- Azukaitis, K.; Ju, W.; Kirchner, M.; Nair, V.; Smith, M.; Fang, Z.; Thurn-Valsassina, D.; Bayazit, A.; Niemirska, A.; Canpolat, N.; et al. Low levels of urinary epidermal growth factor predict chronic kidney disease progression in children. Kidney Int. 2019, 96, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Meybosch, S.; De Monie, A.; Anné, C.; Bruyndonckx, L.; Jürgens, A.; De Winter, B.Y.; Trouet, D.; Ledeganck, K.J. Epidermal growth factor and its influencing variables in healthy children and adults. PLoS ONE 2019, 14, e0211212. [Google Scholar] [CrossRef] [PubMed]
- Callegari, C.; Laborde, N.P.; Buenaflor, G.; Nascimento, C.G.; Brasel, J.A.; Fisher, D.A. The source of urinary epidermal growth factor in humans. Eur. J. Appl. Physiol. Occup. Physiol. 1988, 58, 26–31. [Google Scholar] [CrossRef]
- Nath, K.A. Tubulointerstitial Changes as a Major Determinant in the Progression of Renal Damage. Am. J. Kidney Dis. 1992, 20, 1–17. [Google Scholar] [CrossRef]
- Ledeganck, K.J.; Anné, C.; De Monie, A.; Meybosch, S.; Verpooten, G.; Vinckx, M.; Van Hoeck, K.; Van Eyck, A.; De Winter, B.; Trouet, D. Longitudinal Study of the Role of Epidermal Growth Factor on the Fractional Excretion of Magnesium in Children: Effect of Calcineurin Inhibitors. Nutrients 2018, 10, 677. [Google Scholar] [CrossRef]
- Ledeganck, K.J.; De Winter, B.Y.; Van den Driessche, A.; Jurgens, A.; Bosmans, J.-L.; Couttenye, M.M.; Verpooten, G.A. Magnesium loss in cyclosporine-treated patients is related to renal epidermal growth factor downregulation. Nephrol. Dial. Transplant. 2014, 29, 1097–1102. [Google Scholar] [CrossRef]
- Groenestege, W.M.; Thébault, S.; van der Wijst, J.; van den Berg, D.; Janssen, R.; Tejpar, S.; van den Heuvel, L.P.; van Cutsem, E.; Hoenderop, J.G.; Knoers, N.V.; et al. Impaired basolateral sorting of pro-EGF causes isolated recessive renal hypomagnesemia. J. Clin. Investig. 2007, 117, 2260–2267. [Google Scholar] [CrossRef]
- Lev-Ran, A.; Hwang, D.L.; Miller, J.D.; Josefsberg, Z. Excretion of epidermal growth factor (EGF) in diabetes. Clin. Chim. Acta 1990, 192, 201–206. [Google Scholar] [CrossRef]
- Koenig, W.; Sund, M.; Fröhlich, M.; Löwel, H.; Hutchinson, W.L.; Pepys, M.B. Refinement of the Association of Serum C-reactive Protein Concentration and Coronary Heart Disease Risk by Correction for Within-Subject Variation over TimeThe MONICA Augsburg Studies, 1984 and 1987. Am. J. Epidemiol. 2003, 158, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Danesh, J.; Wheeler, J.G.; Hirschfield, G.M.; Eda, S.; Eiriksdottir, G.; Rumley, A.; Lowe, G.D.O.; Pepys, M.B.; Gudnason, V. C-Reactive Protein and Other Circulating Markers of Inflammation in the Prediction of Coronary Heart Disease. N. Engl. J. Med. 2004, 350, 1387–1397. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Collier, C.P.; White, C.A. Interlaboratory Variability in Plasma Creatinine Measurement and the Relation with Estimated Glomerular Filtration Rate and Chronic Kidney Disease Diagnosis. Clin. J. Am. Soc. Nephrol. 2017, 12, 29–37. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Overall RTR (n = 649) | Tertile 1 | Tertile 2 | Tertile 3 | P |
|---|---|---|---|---|---|
| <4.78 ng/mg | 4.78–8.80 ng/mg | >8.80 ng/mg | |||
| uEGF/Cr, ng/mg | 6.43 (4.07–10.77) | 3.18 (2.12–4.07) | 6.43 (5.57–7.45) | 12.91 (10.77–16.08) | — |
| Demographics | |||||
| Age, years | 53 ± 13 | 51 ± 13 | 53 ± 13 | 55 ± 12 | 0.01 |
| Sex (male), n (%) | 373 (57) | 149 (69) | 124 (57) | 100 (46) | <0.001 |
| Caucasian ethnicity, n (%) | 647 (99) | 216 (100) | 216 (100) | 215 (99) | 0.44 |
| Renal allograft function | |||||
| eGFR, mL/min/1.73 m2 a | 52 ± 20 | 37 ± 14 | 53 ± 16 | 68 ± 17 | <0.001 |
| Urinary protein excretion, g/24 h b | 0.20 (0.02–0.34) | 0.25 (0.13–0.63) | 0.19 (0.02–0.32) | 0.08 (0.02–0.26) | <0.001 |
| Urinary albumin excretion, mg/24 h c | 38.27 (10.57–174.38) | 94.00 (20.48–393.77) | 37.52 (10.50–155.20) | 19.35 (7.11–71.08) | <0.001 |
| Renal transplantation characteristics | |||||
| Pre–emptive transplantation, n (%) | 105 (16) | 27 (13) | 35 (16) | 43 (20) | 0.11 |
| Living donor, n (%) d | 230 (35) | 30 (14) | 95 (44) | 75 (35) | 0.002 |
| Age of donor, years e | 43 ± 15 | 47 ± 14 | 45 ± 15 | 37 ± 15 | <0.001 |
| Sex of donor (male), n (%) f | 331 (51) | 97 (45) | 109 (50) | 125 (58) | 0.03 |
| Cold ischemia time, hours g | 15.2 (2.7–21.3) | 15.6 (3.0–22.5) | 14.0 (2.6–21.0) | 15.4 (2.7–22.0) | 0.03 |
| Time since transplantation, years | 5.28 (1.74–12.00) | 5.07 (1.53–12.92) | 5.26 (1.40–12.32) | 5.45 (2.63–10.98) | 0.96 |
| Renal transplantation recipients’ characteristics | |||||
| Delayed graft fuction, n (%) | 47 (7) | 24 (11) | 13 (6) | 10 (5) | 0.02 |
| HLA mismatch with donor, number h | 2 (1–3) | 2 (1–3) | 2 (1–3) | 2 (1–3) | 0.10 |
| Immunosuppressive therapy | |||||
| Cumulative prednisolone dose, g | 17.4 (5.2–36.2) | 17.0 (4.7–38.4) | 16.8 (4.6–36.4) | 18.1 (8.1–32.8) | 0.78 |
| Sirolimus or rapamune use, n (%) i | 13 (2) | 4 (2) | 6 (3) | 3 (1) | 0.57 |
| Type of calcineurin inhibitor | |||||
| Cyclosporine, n (%) | 258 (40) | 90 (42) | 102 (47) | 66 (31) | 0.002 |
| Tacrolimus, n (%) | 120 (18) | 66 (31) | 32 (15) | 22 (10) | <0.001 |
| Type of proliferation inhibitor | |||||
| Mycophenolic acid, n (%) | 424 (65) | 126 (58) | 147 (68) | 151 (70) | 0.03 |
| Azathioprine, n (%) | 112 (17) | 41 (19) | 32 (15) | 39 (18) | 0.47 |
| Acute rejection treatment, n (%) | 172 (27) | 77 (36) | 55 (25) | 40 (19) | <0.001 |
| Body composition | |||||
| Body surface area, m2 | 1.94 ± 0.22 | 1.97 ± 0.23 | 1.94 ± 0.20 | 1.92 ± 0.21 | 0.06 |
| Body mass index, kg/m2 | 26.5 ± 4.7 | 26.4 ± 4.8 | 26.4 ± 4.4 | 26.8 ± 4.9 | 0.53 |
| Cardiovascular history | |||||
| History of cardiovascular disease, n (%) j | 281 (43) | 88 (41) | 96 (44) | 97 (45) | 0.65 |
| Arterial pressure | |||||
| SBP, mmHg a | 136 ± 17 | 138 ± 18 | 135 ± 17 | 135 ± 17 | 0.17 |
| DBP, mmHg a | 82 ± 11 | 84 ± 11 | 82 ± 11 | 82 ± 10 | 0.06 |
| Use of antihypertensives, n (%) | 573 (88) | 202 (94) | 194 (90) | 177 (82) | 0.001 |
| Lifestyle | |||||
| Current smoker, n (%) k | 78 (12) | 31 (14) | 25 (12) | 22 (10) | 0.48 |
| Alcohol intake >30 g/day, n (%) l | 29 (4) | 9 (4) | 11 (5) | 9 (4) | 0.60 |
| SQUASH, intensity x hours | 5050 (1950–8055) | 5190 (1800–9105) | 4750 (1700–7260) | 5408 (2645–7301) | 0.89 |
| Diabetes and glucose homeostasis | |||||
| Diabetes mellitus, n (%) | 160 (25) | 50 (23) | 58 (27) | 52 (24) | 0.53 |
| Plasma glucose, mmol/L a | 5.2 (4.8–6.0) | 5.3 (4.8–5.9) | 5.2 (4.8–6.1) | 5.3 (4.7–6.1) | 0.09 |
| HbA1c, % m | 5.8 (5.5–6.2) | 5.7 (5.4–6.1) | 5.8 (5.5–6.2) | 5.9 (5.6–6.3) | 0.004 |
| Inflammation | |||||
| Leukocyte count, per 109/L b | 8.2 ± 2.7 | 8.1 ± 2.8 | 8.2 ± 2.8 | 8.1 ± 2.4 | 0.97 |
| hs-CRP, mg/L n | 1.6 (0.7–4.6) | 1.7 (0.8–4.9) | 1.4 (0.7–3.7) | 1.6 (0.7–5.1) | 0.71 |
| Models | uEGF/Cr, ng/mg | ||
|---|---|---|---|
| HR | 95% CI | P | |
| Crude | 0.68 | 0.59–0.78 | <0.001 |
| Model 1 | 0.67 | 0.58–0.78 | <0.001 |
| Model 2 | 0.70 | 0.58–0.77 | <0.001 |
| Model 3 | 0.67 | 0.58–0.78 | <0.001 |
| Model 4 | 0.66 | 0.57–0.77 | <0.001 |
| Model 5 | 0.78 | 0.66–0.93 | 0.005 |
| Model 6 | 0.79 | 0.67–0.94 | 0.007 |
| C-Statistic | P * | |
|---|---|---|
| Urinary protein excretion, g/24 h | 0.76 | Ref. |
| + uEGF/Cr, ng/mg | 0.82 | <0.001 |
| Urinary albumin excretion, mg/24 h | 0.78 | Ref. |
| + uEGF/Cr, ng/mg | 0.82 | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yepes-Calderón, M.; Sotomayor, C.G.; Kretzler, M.; Gans, R.O.B.; Berger, S.P.; Navis, G.J.; Ju, W.; Bakker, S.J.L. Urinary Epidermal Growth Factor/Creatinine Ratio and Graft Failure in Renal Transplant Recipients: A Prospective Cohort Study. J. Clin. Med. 2019, 8, 1673. https://doi.org/10.3390/jcm8101673
Yepes-Calderón M, Sotomayor CG, Kretzler M, Gans ROB, Berger SP, Navis GJ, Ju W, Bakker SJL. Urinary Epidermal Growth Factor/Creatinine Ratio and Graft Failure in Renal Transplant Recipients: A Prospective Cohort Study. Journal of Clinical Medicine. 2019; 8(10):1673. https://doi.org/10.3390/jcm8101673
Chicago/Turabian StyleYepes-Calderón, Manuela, Camilo G. Sotomayor, Matthias Kretzler, Rijk O. B. Gans, Stefan P. Berger, Gerjan J. Navis, Wenjun Ju, and Stephan J. L. Bakker. 2019. "Urinary Epidermal Growth Factor/Creatinine Ratio and Graft Failure in Renal Transplant Recipients: A Prospective Cohort Study" Journal of Clinical Medicine 8, no. 10: 1673. https://doi.org/10.3390/jcm8101673
APA StyleYepes-Calderón, M., Sotomayor, C. G., Kretzler, M., Gans, R. O. B., Berger, S. P., Navis, G. J., Ju, W., & Bakker, S. J. L. (2019). Urinary Epidermal Growth Factor/Creatinine Ratio and Graft Failure in Renal Transplant Recipients: A Prospective Cohort Study. Journal of Clinical Medicine, 8(10), 1673. https://doi.org/10.3390/jcm8101673







