Percutaneous Computed Tomography-Guided Coaxial Core Biopsy for the Diagnosis of Pancreatic Tumors
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
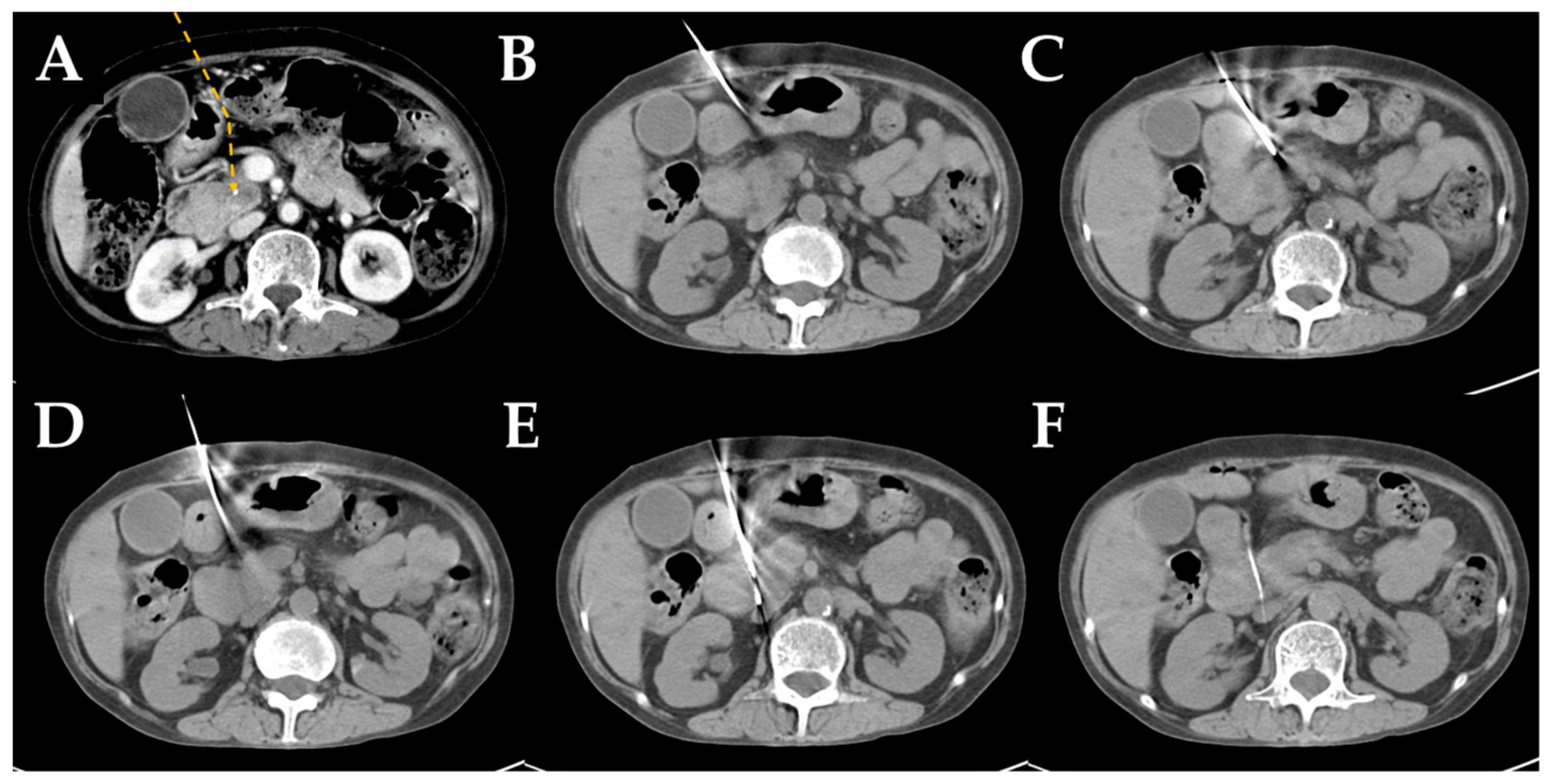
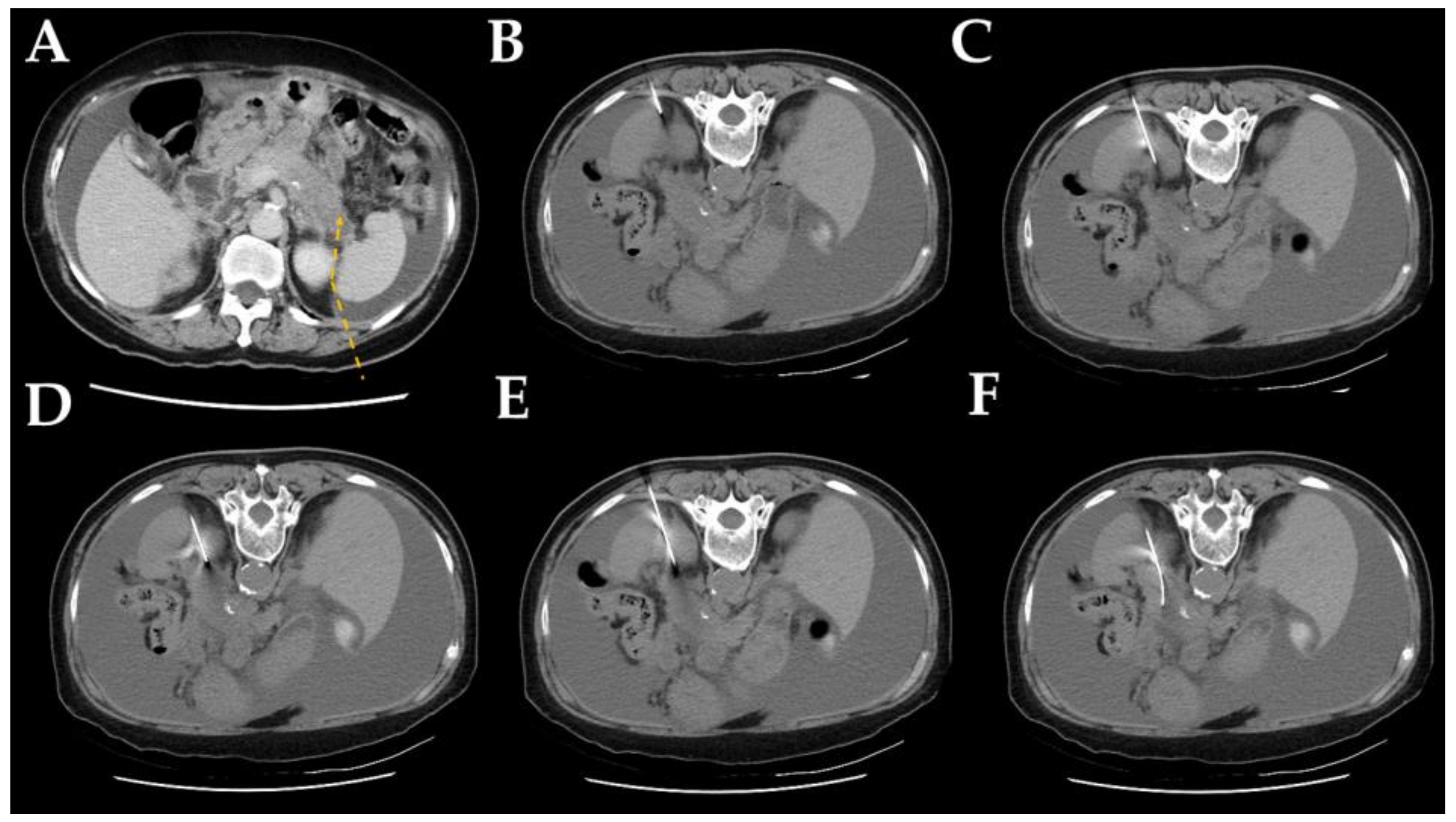
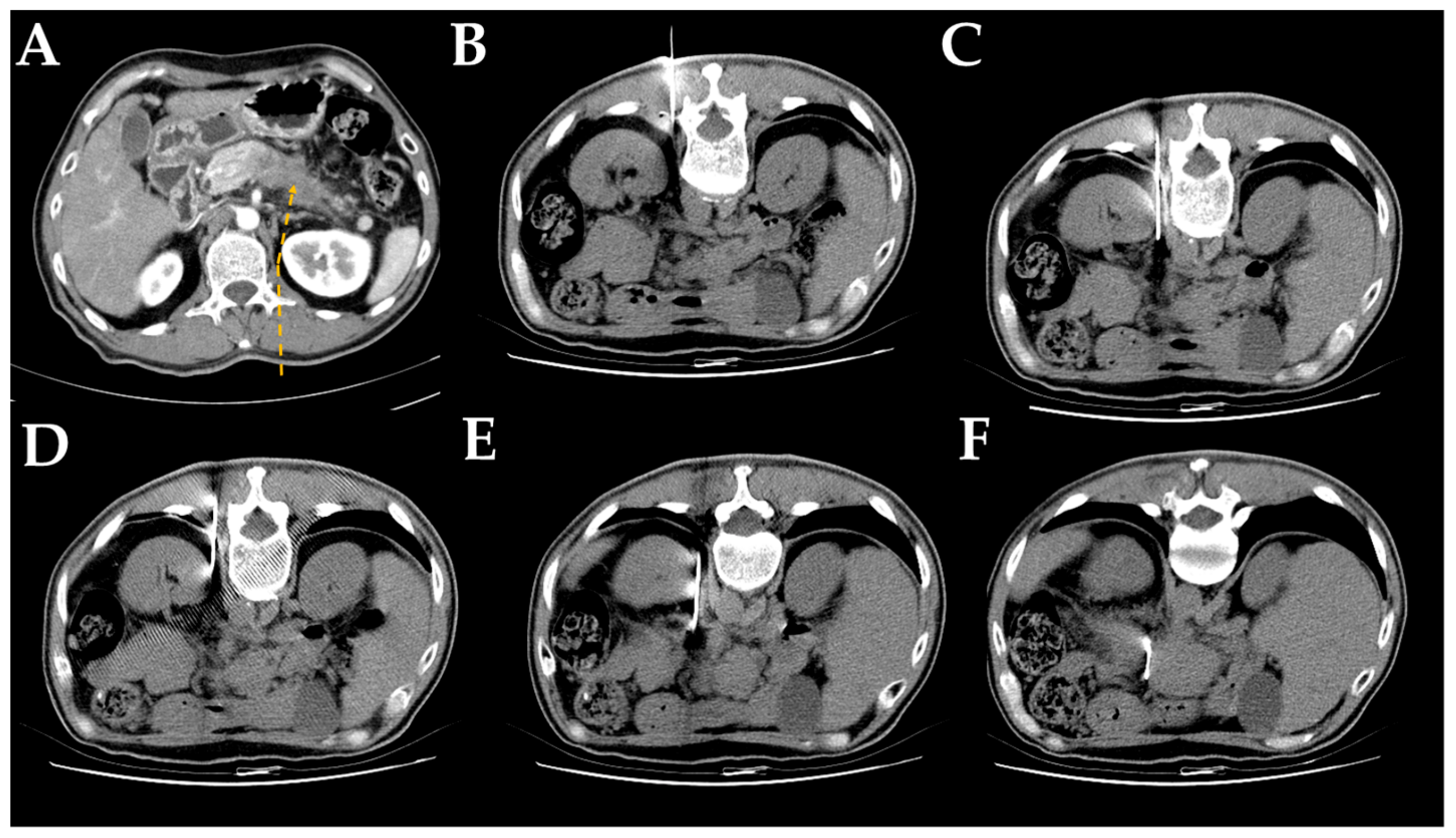
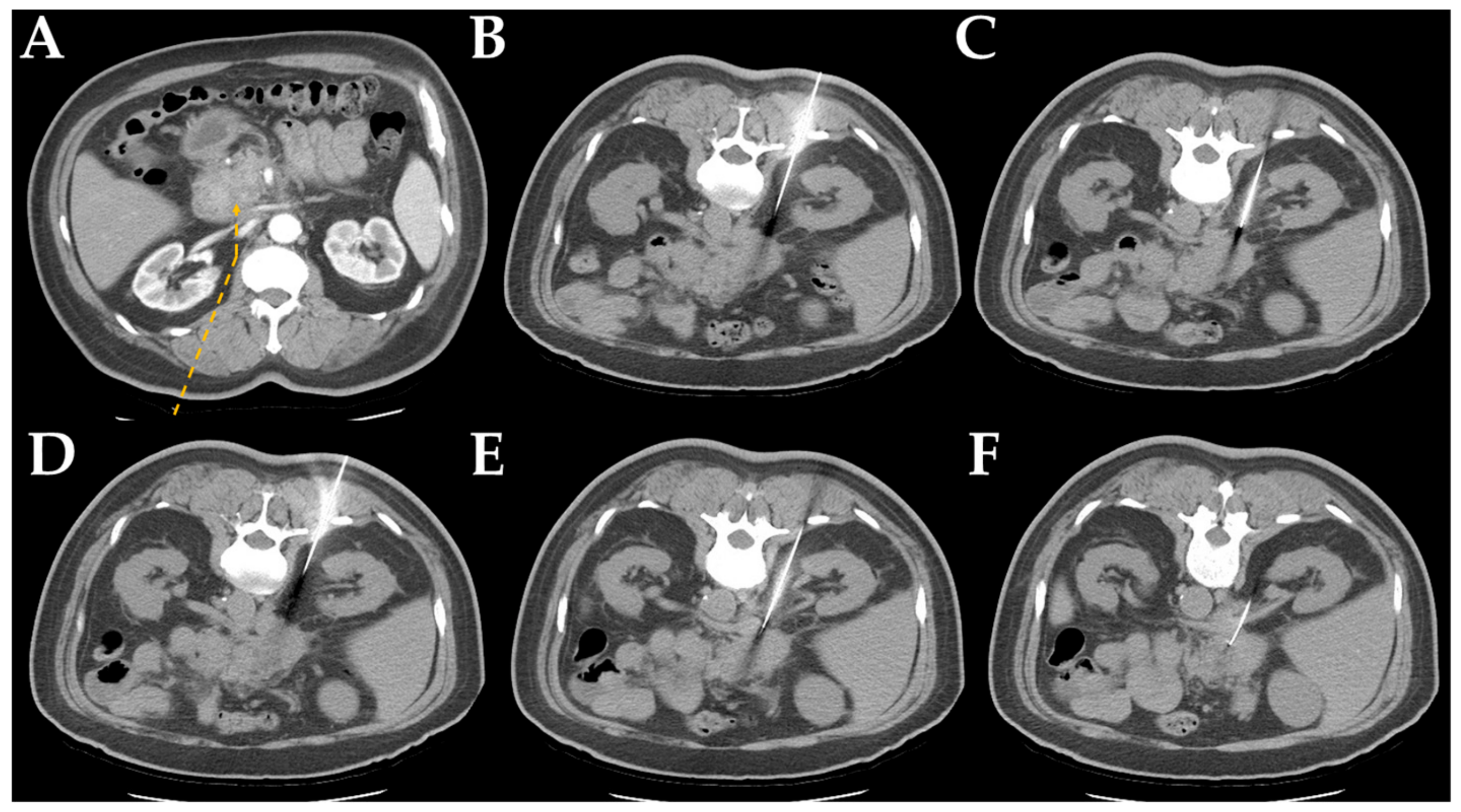
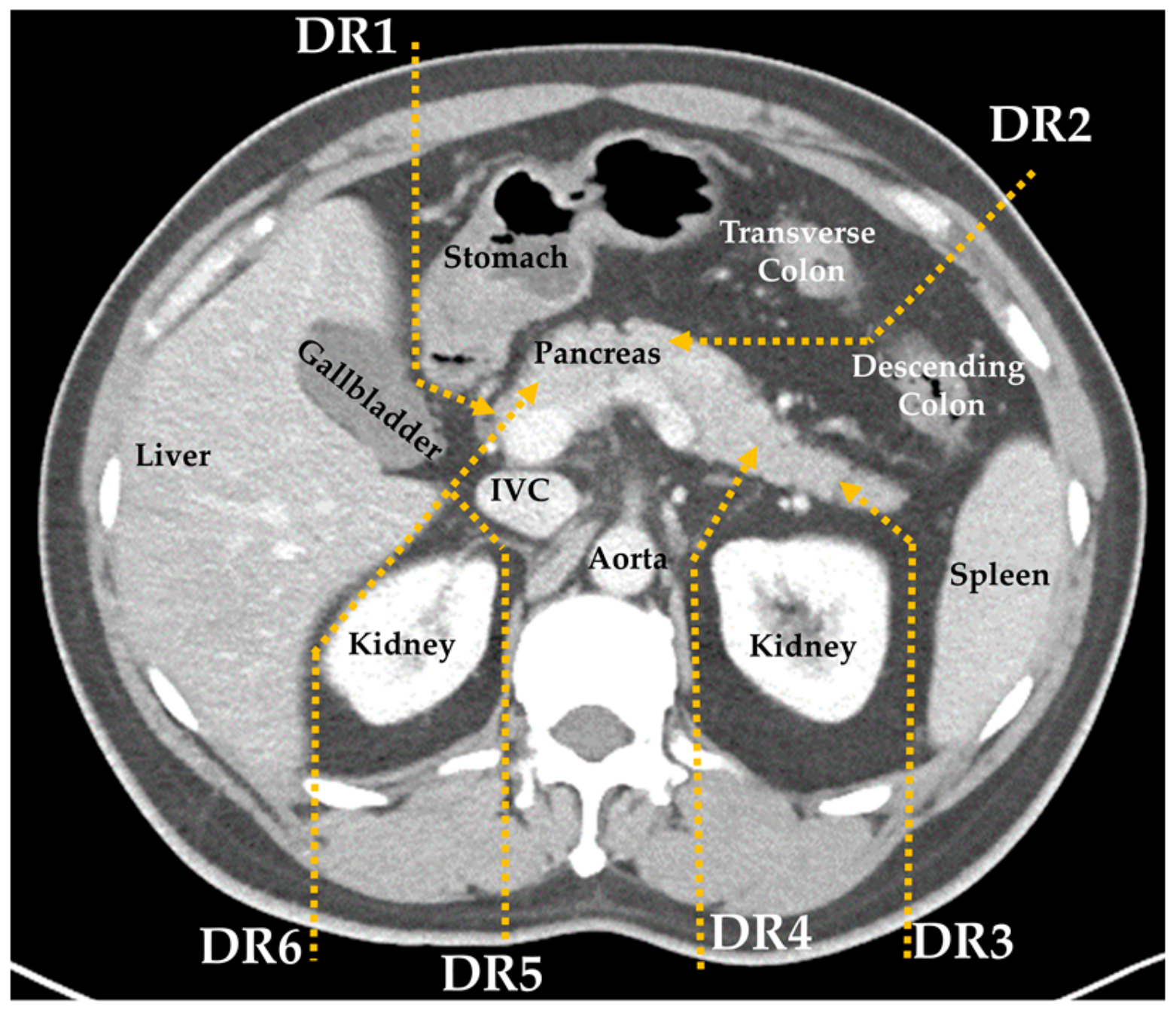
2.2. Computed Tomography-Guided Core Needle Biopsy Technique
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Final Diagnosis and Diagnostic Performance
3.3. Safety Profiles
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
Appendix A

| Cases | Procedure Time Median (range), Minutes | |
|---|---|---|
| Location | ||
| Head | 213 | 30 (14–54) |
| Body | 130 | 28 (14–50) |
| Tail | 90 | 25 (12–41) |
| Access | ||
| Detour route 1 | 169 | 29 (14–54) |
| Detour route 2 | 169 | 28 (12–51) |
| Detour route 3 | 26 | 28.5 (17–42) |
| Detour route 4 | 19 | 29 (16–41) |
| Detour route 5 | 26 | 29.5 (19–40) |
| Detour route 6 | 11 | 28 (19–38) |
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2018. CA Cancer J. Clin. 2018, 68, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Rahib, L.; Smith, B.D.; Aizenberg, R.; Rosenzweig, A.B.; Fleshman, J.M.; Matrisian, L.M. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the united states. Cancer Res. 2014, 74, 2913–2921. [Google Scholar] [CrossRef] [PubMed]
- Quante, A.S.; Ming, C.; Rottmann, M.; Engel, J.; Boeck, S.; Heinemann, V.; Westphalen, C.B.; Strauch, K. Projections of cancer incidence and cancer-related deaths in germany by 2020 and 2030. Cancer Med. 2016, 5, 2649–2656. [Google Scholar] [CrossRef] [PubMed]
- Stathis, A.; Moore, M.J. Advanced pancreatic carcinoma: Current treatment and future challenges. Nat. Rev. Clin. Oncol. 2010, 7, 163–172. [Google Scholar] [CrossRef]
- Banafea, O.; Mghanga, F.P.; Zhao, J.; Zhao, R.; Zhu, L. Endoscopic ultrasonography with fine-needle aspiration for histological diagnosis of solid pancreatic masses: A meta-analysis of diagnostic accuracy studies. BMC Gastroenterol. 2016, 16, 108. [Google Scholar] [CrossRef] [PubMed]
- Ho, C.S.; Tao, L.C.; McLoughlin, M.J. Percutaneous fine-needle aspiration biopsy of intra-abdominal masses. Can. Med. Assoc. J. 1978, 119, 1311–1314. [Google Scholar] [PubMed]
- Armellini, E.; Manfrin, E.; Trisolini, E.; Andorno, S.; Ballare, M.; Bernardoni, L.; Boldorini, R.L.; Gabbrielli, A.; Frulloni, L.; Larghi, A.; et al. Histologic retrieval rate of a newly designed side-bevelled 20g needle for eus-guided tissue acquisition of solid pancreatic lesions. United Eur. Gastroenterol. J. 2019, 7, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Volmar, K.E.; Vollmer, R.T.; Jowell, P.S.; Nelson, R.C.; Xie, H.B. Pancreatic fna in 1000 cases: A comparison of imaging modalities. Gastrointest Endosc. 2005, 61, 854–861. [Google Scholar] [CrossRef]
- Micames, C.; Jowell, P.S.; White, R.; Paulson, E.; Nelson, R.; Morse, M.; Hurwitz, H.; Pappas, T.; Tyler, D.; McGrath, K. Lower frequency of peritoneal carcinomatosis in patients with pancreatic cancer diagnosed by eus-guided fna vs. Percutaneous fna. Gastrointest Endosc. 2003, 58, 690–695. [Google Scholar] [CrossRef]
- Iglesias-Garcia, J.; Dominguez-Munoz, J.E.; Abdulkader, I.; Larino-Noia, J.; Eugenyeva, E.; Lozano-Leon, A.; Forteza-Vila, J. Influence of on-site cytopathology evaluation on the diagnostic accuracy of endoscopic ultrasound-guided fine needle aspiration (eus-fna) of solid pancreatic masses. Am. J. Gastroenterol. 2011, 106, 1705–1710. [Google Scholar] [CrossRef]
- Varadarajulu, S.; Bang, J.Y.; Holt, B.A.; Hasan, M.K.; Logue, A.; Hawes, R.H.; Hebert-Magee, S. The 25-gauge eus-fna needle: Good for on-site but poor for off-site evaluation? Results of a randomized trial. Gastrointest Endosc. 2014, 80, 1056–1063. [Google Scholar] [CrossRef] [PubMed]
- Wani, S.; Mullady, D.; Early, D.S.; Rastogi, A.; Collins, B.; Wang, J.F.; Marshall, C.; Sams, S.B.; Yen, R.; Rizeq, M.; et al. The clinical impact of immediate on-site cytopathology evaluation during endoscopic ultrasound-guided fine needle aspiration of pancreatic masses: A prospective multicenter randomized controlled trial. Am. J. Gastroenterol. 2015, 110, 1429–1439. [Google Scholar] [CrossRef] [PubMed]
- Van Riet, P.A.; Larghi, A.; Attili, F.; Rindi, G.; Nguyen, N.Q.; Ruszkiewicz, A.; Kitano, M.; Chikugo, T.; Aslanian, H.; Farrell, J.; et al. A multicenter randomized trial comparing a 25-gauge eus fine-needle aspiration device with a 20-gauge eus fine-needle biopsy device. Gastrointest Endosc. 2019, 89, 329–339. [Google Scholar] [CrossRef] [PubMed]
- Larson, B.K.; Tuli, R.; Jamil, L.H.; Lo, S.K.; Deng, N.; Hendifar, A.E. Utility of endoscopic ultrasound-guided biopsy for next-generation sequencing of pancreatic exocrine malignancies. Pancreas 2018, 47, 990–995. [Google Scholar] [CrossRef] [PubMed]
- Tyng, C.J.; Bitencourt, A.G.V.; Almeida, M.F.A.; Barbosa, P.N.V.; Martins, E.B.L.; Junior, J.P.K.M.; Chojniak, R.; Coimbra, F.J.F. Computed tomography-guided percutaneous biopsy of pancreatic masses using pneumodissection. Radiologia Brasileira 2013, 46, 139–142. [Google Scholar] [CrossRef][Green Version]
- Asvadi, N.H.; Arellano, R.S. Hydrodissection-assisted image-guided percutaneous biopsy of abdominal and pelvic lesions: Experience with seven patients. AJR Am. J. Roentgenol. 2015, 204, 865–867. [Google Scholar] [CrossRef] [PubMed]
- Hsu, M.Y.; Pan, K.T.; Chen, C.M.; Lui, K.W.; Chu, S.Y.; Hung, C.F.; Huang, Y.T.; Tseng, J.H. Trans-organ versus trans-mesenteric computed tomography-guided percutaneous fine-needle aspiration biopsy of pancreatic masses: Feasibility and safety. Clin. Radiol. 2014, 69, 1050–1055. [Google Scholar] [CrossRef]
- Beazley, R.M. Percutaneous needle biopsy for diagnosis of pancreatic cancer. Semin Oncol. 1979, 6, 344–346. [Google Scholar]
- Lin, C.Y.; Ou, M.C.; Liu, Y.S.; Chuang, M.T.; Shan, Y.S.; Tsai, H.M.; Wang, C.K.; Tsai, Y.S. A ct-guided fat transversing coaxial biopsy technique for pancreatic lesion biopsy that avoids major organs and vessels. Saudi J. Gastroenterol. 2017, 23, 341–347. [Google Scholar]
- Ducreux, M.; Cuhna, A.S.; Caramella, C.; Hollebecque, A.; Burtin, P.; Goere, D.; Seufferlein, T.; Haustermans, K.; Van Laethem, J.L.; Conroy, T.; et al. Cancer of the pancreas: Esmo clinical practice guidelines for diagnosis, treatment and follow-up. Ann. Oncol 2015, 26, 56–68. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network. Pancreatic Adenocarcinoma (version 2.2019). Available online: https://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf (accessed on 1 July 2019).
- Sugiura, R.; Kuwatani, M.; Hirata, K.; Sano, I.; Kato, S.; Kawakubo, K.; Sakamoto, N. Effect of pancreatic mass size on clinical outcomes of endoscopic ultrasound-guided fine-needle aspiration. Dig. Dis. Sci. 2019, 64, 2006–2013. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Ahrar, K.; Morello, F.A., Jr.; Wallace, M.J.; Hicks, M.E. Masses in or around the pancreatic head: CT-guided coaxial fine-needle aspiration biopsy with a posterior transcaval approach. Radiology 2002, 222, 63–69. [Google Scholar] [CrossRef]
- Paulsen, S.D.; Nghiem, H.V.; Negussie, E.; Higgins, E.J.; Caoili, E.M.; Francis, I.R. Evaluation of imaging-guided core biopsy of pancreatic masses. AJR Am. J. Roentgenol. 2006, 187, 769–772. [Google Scholar] [CrossRef] [PubMed]
- Meier-Meitinger, M.; Anders, K.; Alibek, S.; Uder, M.; Baum, U. Ct-guided biopsies of pancreatic lesions: Impact of contrast application prior to versus following needle placement. Acad Radiol. 2009, 16, 1386–1392. [Google Scholar] [CrossRef] [PubMed]
- Yang, R.Y.; Ng, D.; Jaskolka, J.D.; Rogalla, P.; Sreeharsha, B. Evaluation of percutaneous ultrasound-guided biopsies of solid mass lesions of the pancreas: A center’s 10-year experience. Clin. Imaging 2015, 39, 62–65. [Google Scholar] [CrossRef] [PubMed]
- Tyng, C.J.; Almeida, M.F.; Barbosa, P.N.; Bitencourt, A.G.; Berg, J.A.; Maciel, M.S.; Coimbra, F.J.; Schiavon, L.H.; Begnami, M.D.; Guimaraes, M.D.; et al. Computed tomography-guided percutaneous core needle biopsy in pancreatic tumor diagnosis. World J. Gastroenterol. 2015, 21, 3579–3586. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Wang, L.; He, X.; Xu, Y.; Lu, D.; Li, P.; Lv, R.; Feng, Y.; Liu, M.; Li, C. 1.0t MR-guided percutaneous coaxial cutting needle biopsy in pancreatic lesion diagnosis. J. Magn. Reson Imaging 2018, 48, 382–388. [Google Scholar] [CrossRef] [PubMed]
- Stella, S.F.; Van Borsel, M.; Markose, G.; Nair, S.B. Image-guided percutaneous biopsy for pancreatic lesions: 10-year experience in a tertiary cancer center. Can. Assoc. Radiol. J. 2019, 70, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Ikezawa, K.; Uehara, H.; Sakai, A.; Fukutake, N.; Imanaka, K.; Ohkawa, K.; Tanakura, R.; Ioka, T.; Tanaka, S.; Ishikawa, O.; et al. Risk of peritoneal carcinomatosis by endoscopic ultrasound-guided fine needle aspiration for pancreatic cancer. J. Gastroenterol. 2013, 48, 966–972. [Google Scholar] [CrossRef]
- Thomassen, I.; Lemmens, V.E.; Nienhuijs, S.W.; Luyer, M.D.; Klaver, Y.L.; De Hingh, I.H. Incidence, prognosis, and possible treatment strategies of peritoneal carcinomatosis of pancreatic origin: A population-based study. Pancreas 2013, 42, 72–75. [Google Scholar] [CrossRef]
- Kim, S.H.; Woo, Y.S.; Lee, K.H.; Lee, J.K.; Lee, K.T.; Park, J.K.; Kang, S.H.; Kim, J.W.; Park, J.K.; Park, S.W. Preoperative eus-guided fna: Effects on peritoneal recurrence and survival in patients with pancreatic cancer. Gastrointest Endosc. 2018, 88, 926–934. [Google Scholar] [CrossRef] [PubMed]
- Okasha, H.H.; Naga, M.I.; Esmat, S.; Naguib, M.; Hassanein, M.; Hassani, M.; El-Kassas, M.; Mahdy, R.E.; El-Gemeie, E.; Farag, A.H.; et al. Endoscopic ultrasound-guided fine needle aspiration versus percutaneous ultrasound-guided fine needle aspiration in diagnosis of focal pancreatic masses. Endosc. Ultrasound 2013, 2, 190–193. [Google Scholar] [CrossRef] [PubMed]
- Leach, S.D.; Rose, J.A.; Lowy, A.M.; Lee, J.E.; Charnsangavej, C.; Abbruzzese, J.L.; Katz, R.L.; Evans, D.B. Significance of peritoneal cytology in patients with potentially resectable adenocarcinoma of the pancreatic head. Surgery 1995, 118, 472–478. [Google Scholar] [CrossRef]
- Matsuyama, M.; Ishii, H.; Kuraoka, K.; Yukisawa, S.; Kasuga, A.; Ozaka, M.; Suzuki, S.; Takano, K.; Sugiyama, Y.; Itoi, T. Ultrasound-guided vs endoscopic ultrasound-guided fine-needle aspiration for pancreatic cancer diagnosis. World J. Gastroenterol. 2013, 19, 2368–2373. [Google Scholar] [CrossRef] [PubMed]
- Uesaka, K.; Boku, N.; Fukutomi, A.; Okamura, Y.; Konishi, M.; Matsumoto, I.; Kaneoka, Y.; Shimizu, Y.; Nakamori, S.; Sakamoto, H.; et al. Adjuvant chemotherapy of s-1 versus gemcitabine for resected pancreatic cancer: A phase 3, open-label, randomised, non-inferiority trial (jaspac 01). Lancet 2016, 388, 248–257. [Google Scholar] [CrossRef]
- Maturen, K.E.; Nghiem, H.V.; Marrero, J.A.; Hussain, H.K.; Higgins, E.G.; Fox, G.A.; Francis, I.R. Lack of tumor seeding of hepatocellular carcinoma after percutaneous needle biopsy using coaxial cutting needle technique. AJR Am. J. Roentgenol. 2006, 187, 1184–1187. [Google Scholar] [CrossRef] [PubMed]

| Tumor Size | 10–20 mm n = 47 | 21–30 mm n = 103 | 31–40 mm n = 99 | >41 mm n = 171 | Overall n = 420 |
|---|---|---|---|---|---|
| Age, mean ± SD, year | 64.2 ± 12.0 | 63.9 ± 11.5 | 63.0 ± 12.7 | 60.7 ± 11.4 | 62.4 ± 11.9 |
| Gender (male/female) | 26/21 | 57/46 | 60/39 | 105/66 | 248/172 |
| Location | |||||
| Head | 37 | 71 | 46 | 59 | 213 (50.7%) |
| Body | 6 | 27 | 38 | 59 | 130 (31.0%) |
| Tail | 4 | 5 | 15 | 53 | 77 (18.3%) |
| Access | |||||
| Detour route 1 | 26 | 49 | 43 | 51 | 169 (40.2%) |
| Detour route 2 | 16 | 32 | 39 | 82 | 169 (40.2%) |
| Detour route 3 | 2 | 4 | 3 | 17 | 26 (6.2%) |
| Detour route 4 | 0 | 2 | 6 | 11 | 19 (4.5%) |
| Detour route 5 | 3 | 10 | 6 | 7 | 26 (6.2%) |
| Detour route 6 | 0 | 6 | 2 | 3 | 11 (2.6%) |
| Procedure time, median (range), minutes | 34 (14–54) | 31 (18–53) | 30 (22–46) | 23 (12–42) | 28 (12–54) |
| Number of tissue strips, median (range) | 2 (1–3) | 2 (1–3) | 2 (1–3) | 2 (1–5) | 2 (1–5) |
| Performed year | |||||
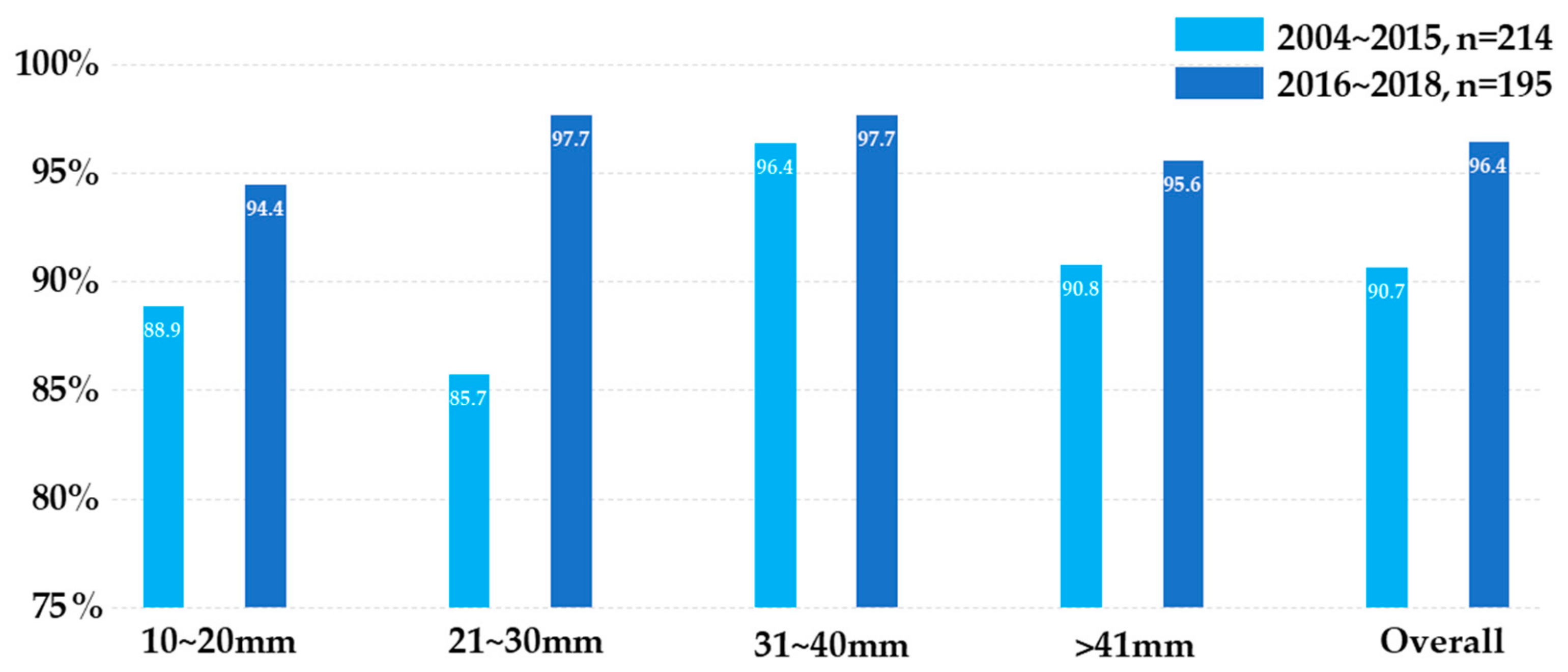
| 2004–2015 | 28 | 58 | 55 | 77 | 218 (57.9%) |
| 2016–2018 | 19 | 45 | 44 | 94 | 202 (42.1%) |
| Technique performance | |||||
| Success tissue acquisition | 47 | 103 | 99 | 168 | 417 (99.3%) |
| Inadequate specimen | 0 | 0 | 0 | 3 | 3 (0.7%) |
| Final diagnosis | |||||
| Neoplasms | 41 | 97 | 95 | 162 | 395 (94.1%) |
| Benign lesions | 4 | 2 | 3 | 5 | 14 (3.3%) |
| Inconclusive cases * | 2 | 4 | 1 | 4 | 11 (2.6%) |
| Positive Diagnosis by CT-CNB/All Cases, n (%) | Size, Median (Range), cm | Stage | ||||
|---|---|---|---|---|---|---|
| I n = 6 | II n = 21 | III n = 93 | IV n = 275 | |||
| Histology type | ||||||
| Adenocarcinoma | 302/323 (93.5%) | 3.5 (1.1–15.5) | 3 | 19 | 84 | 217 |
| Poorly differentiated carcinoma | 13/13 (100%) | 4.7 (2.5–9.7) | 0 | 0 | 3 | 10 |
| Metastatic tumor | 15/17 (88.2%) | 3.6 (1.6–6.7) | 0 | 0 | 0 | 17 |
| Neuroendocrine tumor | 17/17 (100%) | 4.0 (2.0–17.0) | 1 | 1 | 3 | 12 |
| Mucinous neoplasms | 5/5 (100%) | 4.2 (1.7–7.0) | 1 | 1 | 1 | 2 |
| Lymphoma | 9/10 (90.0%) | 5.2 (2.9–9.1) | 1 | 0 | 0 | 9 |
| Adenosquamous carcinoma | 5/6 (83.3%) | 4.2 (3.4–8.0) | 0 | 0 | 1 | 5 |
| Others * | 2/4 (50.0%) | 4.8 (1.7–8.5) | 0 | 0 | 1 | 3 |
| Location | ||||||
| Head | 179/194 (92.3%) | 3.0 (1.1–9.0) | 5 | 17 | 56 | 116 |
| Body | 120/127 (94.5%) | 3.9 (1.6–17.0) | 1 | 3 | 33 | 90 |
| Tail | 69/74 (93.2%) | 4.8 (1.8–15.5) | 0 | 1 | 4 | 69 |
| Tumor Size | 10~20 mm n = 45 * | 21~30 mm n = 99 * | 31~40 mm n = 98 * | >41 mm n = 167 * | Overall n = 409 * |
|---|---|---|---|---|---|
| True positive | 37 | 82 | 92 | 151 | 368 |
| True negative | 4 | 2 | 3 | 5 | 14 |
| False positive | 0 | 0 | 0 | 0 | 0 |
| False negative | 4 | 9 | 3 | 11 | 27 |
| Sensitivity | 90.2% | 90.7% | 96.8% | 93.2% | 93.2% |
| Specificity | 100% | 100% | 100% | 100% | 100% |
| Accuracy | 91.1% | 90.9% | 96.9% | 93.4% | 93.4% |
| Subsequent diagnostic procedures in first CT-CNB false negative cases | |||||
| Re-biopsy † | 0 | 3 | 0 | 3 | 6 |
| Biopsy via EUS | 0 | 0 | 0 | 1 | 1 |
| Biopsy of metastatic lesion | 3 | 2 | 0 | 6 | 11 |
| Surgical specimen | 1 | 2 | 2 | 0 | 5 |
| Clinically significant metastases | 0 | 0 | 1 | 1 | 2 |
| BMI < 18.5 n = 35 | BMI 18.5–22.9 n = 175 | BMI 23–24.9 n = 91 | BMI ≥ 25 n = 119 | Overall n = 420 | |
|---|---|---|---|---|---|
| No complications | 35 (100%) | 161 (92.0%) | 85 (93.4%) | 103 (86.6%) | 384 (91.4%) |
| Major complications | 0 | 0 | 0 | 0 | 0 |
| Minor complications | |||||
| Local hematoma | 0 | 7 | 5 | 4 | 16 |
| Intra-procedural tract bleeding | 0 | 6 | 0 | 10 | 16 |
| Pancreatitis | 0 | 0 | 0 | 1 | 1 |
| Transient hypotension | 0 | 1 | 0 | 1 | 2 |
| Bacteria peritonitis | 0 | 0 | 1 | 0 | 1 |
| Trans-organ | |||||
| Trans-gastric | 0 | 1 | 3 | 2 | 6 |
| Trans-renal | 0 | 1 | 0 | 0 | 1 |
| Stage I n = 6 | Stage II n = 21 | Stage III n = 93 | Stage IV n = 275 | |
|---|---|---|---|---|
| PC before CT-CNB | 0 | 0 | 0 | 21/48 * |
| No PC before CT-CNB | 6 | 21 | 93 | 206 |
| Loss of F/U after CT-CNB, n | 0 | 1 | 9 | 57 |
| F/U image available, n | 6 | 20 | 84 | 149 † |
| Median (range) F/U duration, months | 13.4 (7.0–16.3) | 10.2 (0.5–41.9) | 8.8 (0.1–90.3) | 6.1 (0.2–99.0) |
| PC detected during follow-up, n (%) PC alone PC and other sites of metastasis | 1 (16.7%) 0 1 | 4 (20%) 1 3 | 30 (35.7%) 15 15 | 32 (21.5%) 18 14 |
| Median (range) time to PC, months | 11.7 | 6.1 (4.3–10.6) | 10.0 (2.1–28.9) | 7.8 (1.5–24.4) |
| Reference | Guidance Image Modality | Case Number Coaxial System/All cases | Accuracy | Complications | Biopsy Tract Seeding |
|---|---|---|---|---|---|
| [23] | CT | 29/29 | 82.2% | 13.8% | Not mentioned |
| [24] | CT/US | 110/110 | 94.4% | 2.7% | Not mentioned |
| [25] | CT/MRI | 30/30 | 93% | 16.7% | Not mentioned |
| [26] | US | 75/88 | 93.2% | 3.3% | Not mentioned |
| [27] | CT | 103/103 | 98.1% | 8.7% | 0 |
| [28] | MRI | 31/31 | 93.5% | 6.5% | Not mentioned |
| [29] | CT/US | 67/82 | 82.9% | 11.0% | Not mentioned |
| Current study | CT | 420/420 | 93.4% | 8.6% | 0 |
| Reference | EUS-FNA | Percutaneous-FNA | p-Value * | |
|---|---|---|---|---|
| Micames C, et al. [9] | N | 46 | 43 | |
| Tumor seeding, n (%) | 1 (2.2%) | 7 (16.3%) | 0.03 | |
| Okashi HH, et al. [31] | N | 72 | 125 | |
| Tumor seeding, n (%) | 0% | 3 (2.4%) | 0.3 | |
| Matsuyama, M, et al. [35] | N | 75 | 46 | |
| Tumor seeding, n (%) | 0% | 0% | 1.0 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, Y.-Y.; Liu, Y.-S.; Chao, Y.-J.; Chiang, N.-J.; Yen, C.-J.; Tsai, H.-M. Percutaneous Computed Tomography-Guided Coaxial Core Biopsy for the Diagnosis of Pancreatic Tumors. J. Clin. Med. 2019, 8, 1633. https://doi.org/10.3390/jcm8101633
Su Y-Y, Liu Y-S, Chao Y-J, Chiang N-J, Yen C-J, Tsai H-M. Percutaneous Computed Tomography-Guided Coaxial Core Biopsy for the Diagnosis of Pancreatic Tumors. Journal of Clinical Medicine. 2019; 8(10):1633. https://doi.org/10.3390/jcm8101633
Chicago/Turabian StyleSu, Yung-Yeh, Yi-Sheng Liu, Ying-Jui Chao, Nai-Jung Chiang, Chia-Jui Yen, and Hong-Ming Tsai. 2019. "Percutaneous Computed Tomography-Guided Coaxial Core Biopsy for the Diagnosis of Pancreatic Tumors" Journal of Clinical Medicine 8, no. 10: 1633. https://doi.org/10.3390/jcm8101633
APA StyleSu, Y.-Y., Liu, Y.-S., Chao, Y.-J., Chiang, N.-J., Yen, C.-J., & Tsai, H.-M. (2019). Percutaneous Computed Tomography-Guided Coaxial Core Biopsy for the Diagnosis of Pancreatic Tumors. Journal of Clinical Medicine, 8(10), 1633. https://doi.org/10.3390/jcm8101633






