Effectiveness between Dry Needling and Ischemic Compression in the Triceps Surae Latent Myofascial Trigger Points of Triathletes on Pressure Pain Threshold and Thermography: A Single Blinded Randomized Clinical Trial
Abstract
1. Introduction
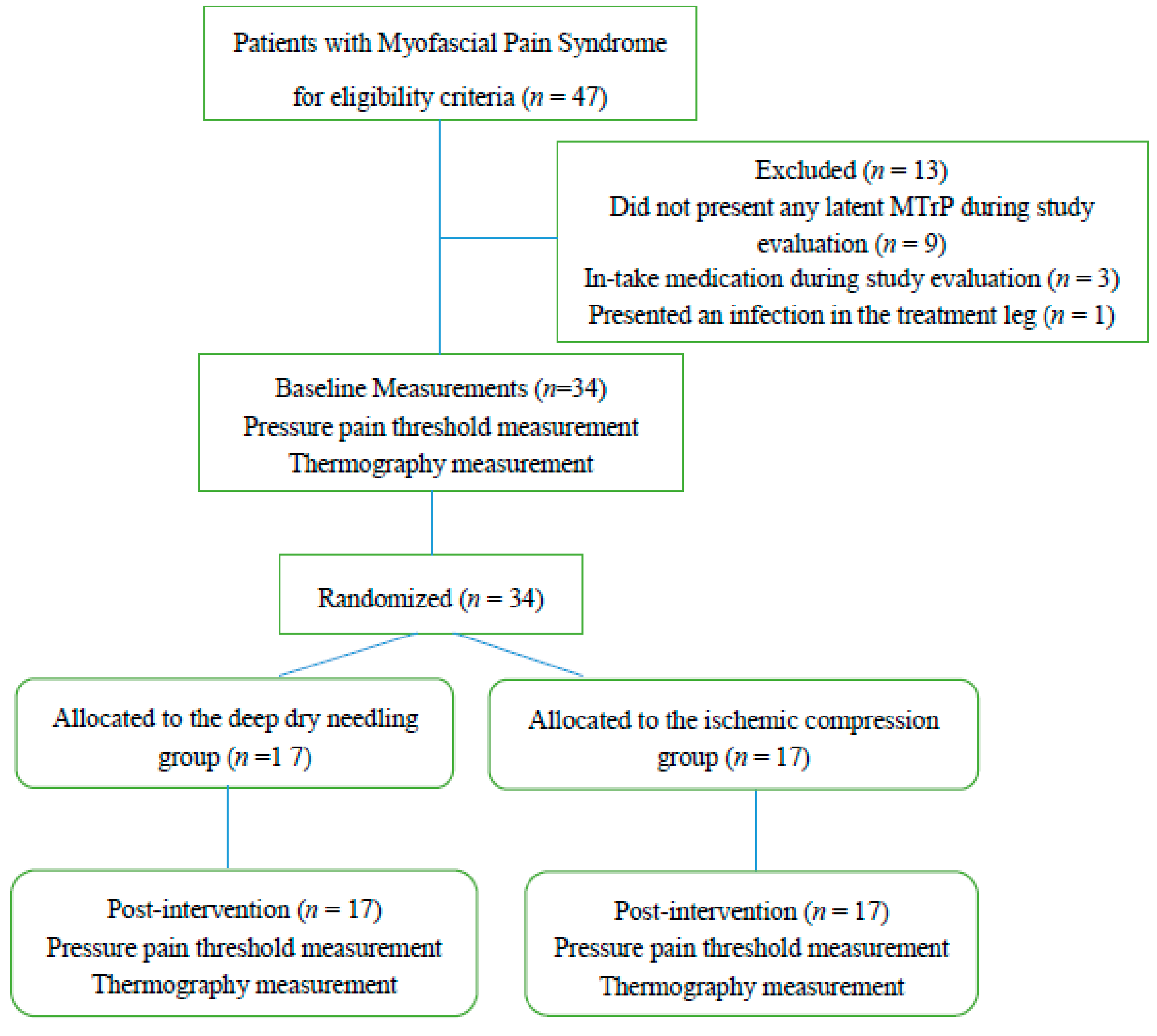
2. Methods
2.1. Design
2.2. Participants
2.3. Simple Size Calculation
2.4. Latent MTrPs Identification
2.5. Primary Outcome: Pressure Pain Threshold
2.6. Second Outcome: Thermographic Measurement.
2.7. Treatment Allocation
2.8. Invasive Procedure: DDN Group
2.9. Conservative Treatment: ICT Group
2.10. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics Attending to the Division by Treatment Groups
3.2. Pressure Pain Threshold
3.3. Thermography
3.4. Reliability Analysis
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Conflicts of Interest
References
- Bron, C.; Dommerholt, J.D. Etiology of myofascial trigger points. Curr. Pain Headache Rep. 2012, 16, 439–444. [Google Scholar] [CrossRef]
- Travell, J.G.; Simons, D. Myofascial pain and dysfunction. In Apropos of a Muscles; Travell, J.G., Simons, D., Eds.; Williams & Wilkins: Baltimore, MD, USA, 2002; Volume 1. [Google Scholar]
- Skootsky, S.A.; Jaeger, B.; Oye, R.K. Prevalence of myofascial pain in general internal medicine practice. West. J. Med. 1989, 151, 157–160. [Google Scholar] [PubMed]
- Gerwin, R.D.; Shannon, S.; Hong, C.Z.; Hubbard, D.; Gevirtz, R. Interrater reliability in myofascial trigger point examination. Pain 1997, 69, 65–73. [Google Scholar] [CrossRef]
- Cummings, M.; Baldry, P. Regional myofascial pain: Diagnosis and management. Best Pract. Res. Clin. Rheumatol. 2007, 21, 367–387. [Google Scholar] [CrossRef]
- Borg-Stein, J.; Simons, D.G. Focused review: Myofascial pain. Arch. Phys. Med. Rehabil. 2002, 83, S40–S47. [Google Scholar] [CrossRef]
- Fernández-de-Las-Peñas, C.; Simons, D.; Cuadrado, M.L.; Pareja, J. The role of myofascial trigger points in musculoskeletal pain syndromes of the head and neck. Curr. Pain Headache Rep. 2007, 11, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Ballyns, J.J.; Shah, J.P.; Hammond, J.; Gebreab, T.; Gerber, L.H.; Sikdar, S. Objective sonographic measures for characterizing myofascial trigger points associated with cervical pain. J. Ultrasound Med. 2011, 30, 1331–1340. [Google Scholar] [CrossRef] [PubMed]
- Ibarra, J.M.; Ge, H.-Y.; Wang, C.; Martínez Vizcaíno, V.; Graven-Nielsen, T.; Arendt-Nielsen, L. Latent myofascial trigger points are associated with an increased antagonistic muscle activity during agonist muscle contraction. J. Pain 2011, 12, 1282–1288. [Google Scholar] [CrossRef]
- Bennett, R. Myofascial pain syndromes and their evaluation. Best Pract. Res. Clin. Rheumatol. 2007, 21, 427–445. [Google Scholar] [CrossRef]
- Ge, H.-Y.; Zhang, Y.; Boudreau, S.; Yue, S.-W.; Arendt-Nielsen, L. Induction of muscle cramps by nociceptive stimulation of latent myofascial trigger points. Exp. Brain Res. 2008, 187, 623–629. [Google Scholar] [CrossRef]
- Gerwin, R.D. A review of myofascial pain and fibromyalgia—Factors that promote their persistence. Acupunct. Med. 2005, 23, 121–134. [Google Scholar] [CrossRef] [PubMed]
- Kimura, Y.; Ge, H.Y.; Zhang, Y.; Kimura, M.; Sumikura, H.; Arendt-Nielsen, L. Evaluation of sympathetic vasoconstrictor response following nociceptive stimulation of latent myofascial trigger points in humans. Acta Physiol. 2009, 196, 411–417. [Google Scholar] [CrossRef]
- Getzin, A.R.; Milner, C.; Harkins, M. Fueling the Triathlete: Evidence-Based Practical Advice for Athletes of All Levels. Curr. Sports Med. Rep. 2017, 16, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Caine, D.; Caine, C.; Maffulli, N. Incidence and Distribution of Pediatric Sport-Related Injuries. Clin. J. Sport Med. 2006, 16, 500–513. [Google Scholar] [CrossRef] [PubMed]
- Tirabassi, J.; Brou, L.; Khodaee, M.; Lefort, R.; Fields, S.K.; Comstock, R.D. Epidemiology of High School Sports-Related Injuries Resulting in Medical Disqualification. Am. J. Sports Med. 2016, 44, 2925–2932. [Google Scholar] [CrossRef]
- Ekstrand, J.; Hagglund, M.; Walden, M. Injury incidence and injury patterns in professional football: The UEFA injury study. Br. J. Sports Med. 2011, 45, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Bertola, I.P.; Sartori, R.P.; Corrêa, D.G.; Zotz, T.G.G.; Gomes, A.R.S. Profile of injures prevalence in athletes who participated in SESC Triathlon Caiobá-2011. Acta Ortop. Bras. 2014, 22, 191–196. [Google Scholar] [CrossRef]
- Andersen, C.A.; Clarsen, B.; Johansen, T.V.; Engebretsen, L. High prevalence of overuse injury among iron-distance triathletes. Br. J. Sports Med. 2013, 47, 857–861. [Google Scholar] [CrossRef]
- Kennedy, J.G.; Knowles, B.; Dolan, M.; Bohne, W. Foot and ankle injuries in the adolescent runner. Curr. Opin. Pediatr. 2005, 17, 34–42. [Google Scholar] [CrossRef]
- Edwards, J.; Knowles, N. Superficial dry needling and active stretching in the treatment of myofascial pain--a randomised controlled trial. Acupunct. Med. 2003, 21, 80–86. [Google Scholar] [CrossRef]
- Dommerholt, J. Dry needling—Peripheral and central considerations. J. Man. Manip. Ther. 2011, 19, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Zwingenberger, S.; Valladares, R.D.; Walther, A.; Beck, H.; Stiehler, M.; Kirschner, S.; Engelhardt, M.; Kasten, P. An epidemiological investigation of training and injury patterns in triathletes. J. Sports Sci. 2014, 32, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Grieve, R.; Barnett, S.; Coghill, N.; Cramp, F. The prevalence of latent myofascial trigger points and diagnostic criteria of the triceps surae and upper trapezius: A cross sectional study. Physiotherapy 2013, 99, 278–284. [Google Scholar] [CrossRef] [PubMed]
- Hong, C.-Z. Treatment of myofascial pain syndrome. Curr. Pain Headache Rep. 2006, 10, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Cagnie, B.; Dewitte, V.; Coppieters, I.; Van Oosterwijck, J.; Cools, A.; Danneels, L. Effect of Ischemic Compression on Trigger Points in the Neck and Shoulder Muscles in Office Workers: A Cohort Study. J. Manip. Physiol. Ther. 2013, 36, 482–489. [Google Scholar] [CrossRef] [PubMed]
- Kalichman, L.; Vulfsons, S. Dry Needling in the Management of Musculoskeletal Pain. J. Am. Board Fam. Med. 2010, 23, 640–646. [Google Scholar] [CrossRef]
- Morikawa, Y.; Takamoto, K.; Nishimaru, H.; Taguchi, T.; Urakawa, S.; Sakai, S.; Ono, T.; Nishijo, H. Compression at Myofascial Trigger Point on Chronic Neck Pain Provides Pain Relief through the Prefrontal Cortex and Autonomic Nervous System: A Pilot Study. Front. Neurosci. 2017, 11, 186. [Google Scholar] [CrossRef]
- Vernon, H.; Schneider, M. Chiropractic management of myofascial trigger points and myofascial pain syndrome: A systematic review of the literature. J. Manipulative Physiol. Ther. 2009, 32, 14–24. [Google Scholar] [CrossRef]
- Baldry, P. Acupuncture, Trigger Points and Musculoskeletal Pain, 3rd ed.; Brookline, M., Ed.; Churchill Livingstone: London, UK, 1993. [Google Scholar]
- Moraska, A.F.; Hickner, R.C.; Kohrt, W.M.; Brewer, A. Changes in blood flow and cellular metabolism at a myofascial trigger point with trigger point release (ischemic compression): A proof-of-principle pilot study. Arch. Phys. Med. Rehabil. 2013, 94, 196–200. [Google Scholar] [CrossRef]
- Holowatz, L.A.; Kenney, W.L. Peripheral mechanisms of thermoregulatory control of skin blood flow in aged humans. J. Appl. Physiol. 2010, 109, 1538–1544. [Google Scholar] [CrossRef]
- Rodriguez, D.; Becerro-de-Bengoa-Vallejo, R.; Iglesias, M.E.L.; Jimenez, E.V.A.M.M.; Muñoz-García, D.; Boal, E.P.; Lobo, C.C.; López-López, D. Effects of Compressive Stockings and Standard Stockings in Skin Temperature and Pressure Pain Threshold in Runners with Functional Ankle Equinus Condition. J. Clin. Med. 2018, 7, 454. [Google Scholar] [CrossRef] [PubMed]
- Sanz, D.R.; Iglesias, M.E.L.; de Bengoa-Vallejo, R.B.; Lopez, P.P.; Alacreu, H.B.; Lobo, C.C.; Flores, E.N.; Lopez, D.L. Skin temperature in youth soccer players with functional equinus and non-equinus condition after running. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 2020–2024. [Google Scholar] [CrossRef] [PubMed]
- Dibai-Filho, A.V.; Guirro, R.R.d.J. Evaluation of Myofascial Trigger Points Using Infrared Thermography: A Critical Review of the Literature. J. Manip. Physiol. Ther. 2015, 38, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Cojocaru, M.C.; Cojocaru, I.M.; Voiculescu, V.M.; Cojan-Carlea, N.A.; Dumitru, V.L.; Berteanu, M. Trigger points—Ultrasound and thermal findings. J. Med. Life 2015, 8, 315–318. [Google Scholar] [PubMed]
- Paulson, K.L.; Shay, B.L. Sympathetic nervous system responses to acupuncture and non-penetrating sham acupuncture in experimental forearm pain: A single-blind randomised descriptive study. Acupunct. Med. 2013, 31, 178–184. [Google Scholar] [CrossRef]
- Ohkubo, M.; Hamaoka, T.; Niwayama, M.; Murase, N.; Osada, T.; Kime, R.; Kurosawa, Y.; Sakamoto, A.; Katsumura, T. Local increase in trapezius muscle oxygenation during and after acupuncture. Dyn. Med. 2009, 8, 2. [Google Scholar] [CrossRef]
- Tekin, L.; Akarsu, S.; Durmuş, O.; Cakar, E.; Dinçer, U.; Kıralp, M.Z. The effect of dry needling in the treatment of myofascial pain syndrome: A randomized double-blinded placebo-controlled trial. Clin. Rheumatol. 2013, 32, 309–315. [Google Scholar] [CrossRef]
- Aguilera, F.J.M.; Martín, D.P.; Masanet, R.A.; Botella, A.C.; Soler, L.B.; Morell, F.B. Immediate effect of ultrasound and ischemic compression techniques for the treatment of trapezius latent myofascial trigger points in healthy subjects: A randomized controlled study. J. Manipulative Physiol. Ther. 2009, 32, 515–520. [Google Scholar] [CrossRef]
- Tesch, R.D.S.; Macedo, L.C.D.S.P.; Fernandes, F.S.; Goffredo Filho, G.D.S.; Goes, C.P.D.Q.F. Effectiveness of dry needling on the local pressure pain threshold in patients with masticatory myofascial pain. Systematic review and preliminary clinical trial. CRANIO® 2019, 1–9. [Google Scholar] [CrossRef]
- Cagnie, B.; Castelein, B.; Pollie, F.; Steelant, L.; Verhoeyen, H.; Cools, A. Evidence for the Use of Ischemic Compression and Dry Needling in the Management of Trigger Points of the Upper Trapezius in Patients with Neck Pain. Am. J. Phys. Med. Rehabil. 2015, 94, 573–583. [Google Scholar] [CrossRef]
- Ganesh, G.S.; Singh, H.; Mushtaq, S.; Mohanty, P.; Pattnaik, M. Effect of cervical mobilization and ischemic compression therapy on contralateral cervical side flexion and pressure pain threshold in latent upper trapezius trigger points. J. Bodyw. Mov. Ther. 2016, 20, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Ziaeifar, M.; Arab, A.M.; Nourbakhsh, M.R. Clinical Effectiveness of Dry Needling Immediately After Application on Myofascial Trigger Point in Upper Trapezius Muscle. J. Chiropr. Med. 2016, 15, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Benito-de-Pedro, M.; Becerro-de-Bengoa-Vallejo, R.; Elena Losa-Iglesias, M.; Rodríguez-Sanz, D.; López-López, D.; Palomo-López, P.; Mazoteras-Pardo, V.; Calvo-Lobo, A.C. Effectiveness of Deep Dry Needling vs Ischemic Compression in the Latent Myofascial Trigger Points of the Shortened Triceps Surae from Triathletes on Ankle Dorsiflexion, Dynamic, and Static Plantar Pressure Distribution: A Clinical Trial. Pain Med. 2019, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Llamas-Ramos, R.; Pecos-Martín, D.; Gallego-Izquierdo, T.; Llamas-Ramos, I.; Plaza-Manzano, G.; Ortega-Santiago, R.; Cleland, J.; Fernández-de-las-Peñas, C. Comparison of the Short-Term Outcomes Between Trigger Point Dry Needling and Trigger Point Manual Therapy for the Management of Chronic Mechanical Neck Pain: A Randomized Clinical Trial. J. Orthop. Sport. Phys. Ther. 2014, 44, 852–861. [Google Scholar] [CrossRef] [PubMed]
- Martínez de la Iglesia, J.; Dueñas Herrero, R.; Onís Vilches, M.C.; Aguado Taberné, C.; Albert Colomer, C.; Luque Luque, R. Spanish language adaptation and validation of the Pfeiffer’s questionnaire (SPMSQ) to detect cognitive deterioration in people over 65 years of age. Med. Clin. (Barc) 2001, 117, 129–134. [Google Scholar] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Lobo, C.; Pacheco-Da-Costa, S.; Hita-Herranz, E. Efficacy of deep dry needling on latent myofascial trigger points in older adults with nonspecific shoulder pain: A randomized, controlled clinical trial pilot study. J. Geriatr. Phys. Ther. 2017, 40. [Google Scholar] [CrossRef]
- Calvo-Lobo, C.; Pacheco-da-Costa, S.; Martínez-Martínez, J.; Rodríuez-Sanz, D.; Cuesta-Álvaro, P.; López-López, D. Dry Needling on the Infraspinatus Latent and Active Myofascial Trigger Points in Older Adults with Nonspecific Shoulder Pain. J. Geriatr. Phys. Ther. 2018, 41, 1–13. [Google Scholar] [CrossRef]
- Vanderweeën, L.; Oostendorp, R.A.B.; Vaes, P.; Duquet, W. Pressure algometry in manual therapy. Man. Ther. 1996, 1, 258–265. [Google Scholar] [CrossRef]
- Park, G.; Kim, C.W.; Park, S.B.; Kim, M.J.; Jang, S.H.; Kwon, S. Reliability and Usefulness of the Pressure Pain Threshold Measurement in Patients with Myofascial Pain. Ann. Rehabil. Med. 2011, 35, 412. [Google Scholar] [CrossRef]
- Chesterton, L.S.; Sim, J.; Wright, C.C.; Foster, N.E. Interrater reliability of algometry in measuring pressure pain thresholds in healthy humans, using multiple raters. Clin. J. Pain 2007, 23, 760–766. [Google Scholar] [CrossRef] [PubMed]
- Walton, D.M.; Macdermid, J.C.; Nielson, W.; Teasell, R.W.; Chiasson, M.; Brown, L. Reliability, standard error, and minimum detectable change of clinical pressure pain threshold testing in people with and without acute neck pain. J. Orthop. Sports Phys. Ther. 2011, 41, 644–650. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Sanz, D.; Losa-Iglesias, M.E.; López-López, D.; Calvo-Lobo, C.; Palomo-López, P.; Becerro-de-Bengoa-Vallejo, R. Infrared thermography applied to lower limb muscles in elite soccer players with functional ankle equinus and non-equinus condition. PeerJ 2017, 5. [Google Scholar] [CrossRef] [PubMed]
- Cagnie, B.; Barbe, T.; De Ridder, E.; Van Oosterwijck, J.; Cools, A.; Danneels, L. The influence of dry needling of the trapezius muscle on muscle blood flow and oxygenation. J. Manip. Physiol. Ther. 2012, 35, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Moral, O.M.D. Dry needling treatments for myofascial trigger points. J. Musculoskelet. Pain 2010, 18, 411–416. [Google Scholar] [CrossRef]
- Hong, C.Z. Lidocaine injection versus dry needling to myofascial trigger point. The importance of the local twitch response. Am. J. Phys. Med. Rehabil. 1994, 73, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Baldry, P. Superficial versus deep dry needling. Acupunct. Med. 2002, 20, 78–81. [Google Scholar] [CrossRef]
- Hallgren, K.A. Computing Inter-Rater Reliability for Observational Data: An Overview and Tutorial. Tutor. Quant. Methods Psychol. 2012, 8, 23–34. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Int. J. Nurs. Stud. 2010, 47, 931–936. [Google Scholar] [CrossRef]
- Cummings, T.M.; White, A.R. Needling therapies in the management of myofascial trigger point pain: A systematic review. Arch. Phys. Med. Rehabil. 2001, 82, 986–992. [Google Scholar] [CrossRef]
- Tough, E.A.; White, A.R.; Cummings, T.M.; Richards, S.H.; Campbell, J.L. Acupuncture and dry needling in the management of myofascial trigger point pain: A systematic review and meta-analysis of randomised controlled trials. Eur. J. Pain 2009, 13, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Srbely, J.Z. New Trends in the Treatment and Management of Myofascial Pain Syndrome. Curr. Pain Headache Rep. 2010, 14, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Cagnie, B.; Dewitte, V.; Barbe, T.; Timmermans, F.; Delrue, N.; Meeus, M. Physiologic effects of dry needling. Curr. Pain Headache Rep. 2013, 17, 348. [Google Scholar] [CrossRef] [PubMed]
- Kubo, K.; Yajima, H.; Takayama, M.; Ikebukuro, T.; Mizoguchi, H.; Takakura, N. Effects of acupuncture and heating on blood volume and oxygen saturation of human Achilles tendon in vivo. Eur. J. Appl. Physiol. 2010, 109, 545–550. [Google Scholar] [CrossRef] [PubMed]
- Skorupska, E.; Rychlik, M.; Samborski, W. Validation and Test-Retest Reliability of New Thermographic Technique Called Thermovision Technique of Dry Needling for Gluteus Minimus Trigger Points in Sciatica Subjects and TrPs-Negative Healthy Volunteers. Biomed. Res. Int. 2015, 2015, 546497. [Google Scholar] [CrossRef] [PubMed]
- Skorupska, E.; Rychlik, M.; Samborski, W. Intensive vasodilatation in the sciatic pain area after dry needling. BMC Complement. Altern. Med. 2015, 15, 72. [Google Scholar] [CrossRef] [PubMed]
- Skorupska, E.; Rychlik, M.; Pawelec, W.; Samborski, W. Dry Needling Related Short-Term Vasodilation in Chronic Sciatica under Infrared Thermovision. Evid. Based Complement. Altern. Med. 2015, 2015, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Skorupska, E.; Rychlik, M.; Pawelec, W.; Bednarek, A.; Samborski, W. Trigger Point-Related Sympathetic Nerve Activity in Chronic Sciatic Leg Pain: A Case Study. Acupunct. Med. 2014, 32, 418–422. [Google Scholar] [CrossRef]
- De Jesus Guirro, R.R.; Oliveira Lima Leite Vaz, M.M.; das Neves, L.M.S.; Dibai-Filho, A.V.; Carrara, H.H.A.; de Oliveira Guirro, E.C. Accuracy and Reliability of Infrared Thermography in Assessment of the Breasts of Women Affected by Cancer. J. Med. Syst. 2017, 41, 87. [Google Scholar] [CrossRef]
- Martín-Pintado-Zugasti, A.; Pecos-Martin, D.; Rodríguez-Fernández, Á.L.; Alguacil-Diego, I.M.; Portillo-Aceituno, A.; Gallego-Izquierdo, T.; Fernandez-Carnero, J. Ischemic Compression After Dry Needling of a Latent Myofascial Trigger Point Reduces Postneedling Soreness Intensity and Duration. PMR 2015, 7, 1026–1034. [Google Scholar] [CrossRef]
- Martín-Pintado-Zugasti, A.; Rodríguez-Fernández, Á.L.; Fernandez-Carnero, J. Postneedling soreness after deep dry needling of a latent myofascial trigger point in the upper trapezius muscle: Characteristics, sex differences and associated factors. J. Back Musculoskelet. Rehabil. 2016, 29, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Simons, D.G.; Travell, J.G.; Simons, L.S. Travell and Simons’ Myofascial Pain and Dysfunction: The Trigger Point Manual. Upper Half of Body, 2nd ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 1999. [Google Scholar]
- Graven-Nielsen, T.; Arendt-Nielsen, L. Induction and assessment of muscle pain, referred pain, and muscular hyperalgesia. Curr. Pain Headache Rep. 2003, 7, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Grieve, R.; Cranston, A.; Henderson, A.; John, R.; Malone, G.; Mayall, C. The immediate effect of triceps surae myofascial trigger point therapy on restricted active ankle joint dorsiflexion in recreational runners: A crossover randomised controlled trial. J. Bodyw. Mov. Ther. 2013, 17, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Gemmell, H.; Miller, P.; Nordstrom, H. Immediate effect of ischaemic compression and trigger point pressure release on neck pain and upper trapezius trigger points: A randomised controlled trial. Clin. Chiropr. 2008, 11, 30–36. [Google Scholar] [CrossRef]
- Hou, C.-R.; Tsai, L.-C.; Cheng, K.-F.; Chung, K.-C.; Hong, C.-Z. Immediate effects of various physical therapeutic modalities on cervical myofascial pain and trigger-point sensitivity. Arch. Phys. Med. Rehabil. 2002, 83, 1406–1414. [Google Scholar] [CrossRef] [PubMed]
- Mutlu, E.K.; Ozdincler, A.R. Reliability and responsiveness of algometry for measuring pressure pain threshold in patients with knee osteoarthritis. J. Phys. Ther. Sci. 2015, 27, 1961–1965. [Google Scholar] [CrossRef] [PubMed]
- Steentjes, K.; de Vries, L.M.A.; Ridwan, B.U.; Wijgman, A.J.J. Infection of a hip prosthesis after dry needling. Ned. Tijdschr. Geneeskd. 2016, 160, A9364. [Google Scholar]
- Lee, J.-H.; Lee, H.; Jo, D.-J. An Acute Cervical Epidural Hematoma as a Complication of Dry Needling. Spine (Phila. Pa. 1976) 2011, 36, E891–E893. [Google Scholar] [CrossRef]
- Giamberardino, M.A.; Dragani, L.; Valente, R.; Di Lisa, F.; Saggini, R.; Vecchiet, L. Effects of prolonged L-carnitine administration on delayed muscle pain and CK release after eccentric effort. Int. J. Sports Med. 1996, 17, 320–324. [Google Scholar] [CrossRef]
- Fischer, A.A. Pressure algometry over normal muscles. Standard values, validity and reproducibility of pressure threshold. Pain 1987, 30, 115–126. [Google Scholar] [CrossRef]
| DDN Group (n = 17) | ICT Group (n = 17) | p-Value | |
|---|---|---|---|
| Age (years) | 35.29 ± 5.39 (32.73–37.85) | 33.76 ± 5.76 (31.02–36.50) | 0.215 |
| Weight (kg) | 65.17 ± 10.71 (60.08–70.27) | 69.17 ± 10.66 (64.10–74.24) | 0.141 |
| Height (cm) | 170.35 ± 12.94 (164.19–176.50) | 174.94 ± 6.96 (171.62–178.25) | 0.103 |
| BMI (kg/m2) | 22.37±1.92 (21.46–23.29) | 22.48 ± 2.35 (21.36–23.6) | 0.443 |
| Size of footwear (cm) | 41.55±3.26 (40.00–43.11) | 41.35 ± 2.73 (40.05–42.65) | 0.421 |
| Before Treatment | After Treatment | |||||
|---|---|---|---|---|---|---|
| Variable | DDN group (n = 17) | ICT group (n= 17) | p-value * | DDN group (n = 17) | ICT group (n = 17) | p-value * |
| Pressure pain threshold | 2.63±0.65 (2.32–2.94) | 2.62 ± 0.66 (2.30–2.94) | 0.485 | 1.94 ± 0.58 (1.66–2.22) | 2.38 ± 0.73 (2.02–2.73) | 0.032 |
| Before Treatment | After Treatment | |||||
|---|---|---|---|---|---|---|
| Variable | DDN group (n = 17) | ICT group (n = 17) | p-value ** | DDN group (n = 17) | ICT group (n = 17) | p-value ** |
| Temperature in superficial area of MTrP | 31.73 ± 1.99 (30.78–3.67) | 31.85 ± 1.71 (31.04–32.66) | 0.422 | 31.71 ± 1.98 (30.77–32.65) | 32.25 ± 1.47 (31.55–32.95) | 0.186 |
| Temperature in the contralateral limb | 31.81±1.78 (30.96–32.66) | 31.98±1.39 (31.31–32.65) | 0.380 | 31.81 ± 1.75 (30.98–32.64) | 32.22 ± 1.35 (31.57–32.86) | 0.227 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benito-de-Pedro, M.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Rodríguez-Sanz, D.; López-López, D.; Cosín-Matamoros, J.; Martínez-Jiménez, E.M.; Calvo-Lobo, C. Effectiveness between Dry Needling and Ischemic Compression in the Triceps Surae Latent Myofascial Trigger Points of Triathletes on Pressure Pain Threshold and Thermography: A Single Blinded Randomized Clinical Trial. J. Clin. Med. 2019, 8, 1632. https://doi.org/10.3390/jcm8101632
Benito-de-Pedro M, Becerro-de-Bengoa-Vallejo R, Losa-Iglesias ME, Rodríguez-Sanz D, López-López D, Cosín-Matamoros J, Martínez-Jiménez EM, Calvo-Lobo C. Effectiveness between Dry Needling and Ischemic Compression in the Triceps Surae Latent Myofascial Trigger Points of Triathletes on Pressure Pain Threshold and Thermography: A Single Blinded Randomized Clinical Trial. Journal of Clinical Medicine. 2019; 8(10):1632. https://doi.org/10.3390/jcm8101632
Chicago/Turabian StyleBenito-de-Pedro, María, Ricardo Becerro-de-Bengoa-Vallejo, Marta Elena Losa-Iglesias, David Rodríguez-Sanz, Daniel López-López, Julia Cosín-Matamoros, Eva María Martínez-Jiménez, and César Calvo-Lobo. 2019. "Effectiveness between Dry Needling and Ischemic Compression in the Triceps Surae Latent Myofascial Trigger Points of Triathletes on Pressure Pain Threshold and Thermography: A Single Blinded Randomized Clinical Trial" Journal of Clinical Medicine 8, no. 10: 1632. https://doi.org/10.3390/jcm8101632
APA StyleBenito-de-Pedro, M., Becerro-de-Bengoa-Vallejo, R., Losa-Iglesias, M. E., Rodríguez-Sanz, D., López-López, D., Cosín-Matamoros, J., Martínez-Jiménez, E. M., & Calvo-Lobo, C. (2019). Effectiveness between Dry Needling and Ischemic Compression in the Triceps Surae Latent Myofascial Trigger Points of Triathletes on Pressure Pain Threshold and Thermography: A Single Blinded Randomized Clinical Trial. Journal of Clinical Medicine, 8(10), 1632. https://doi.org/10.3390/jcm8101632







