Motor Capacities in Boys with High Functioning Autism: Which Evaluations to Choose?
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Motor Assessment
2.3. Statistical Analysis
3. Results
3.1. Principal Component Analysis
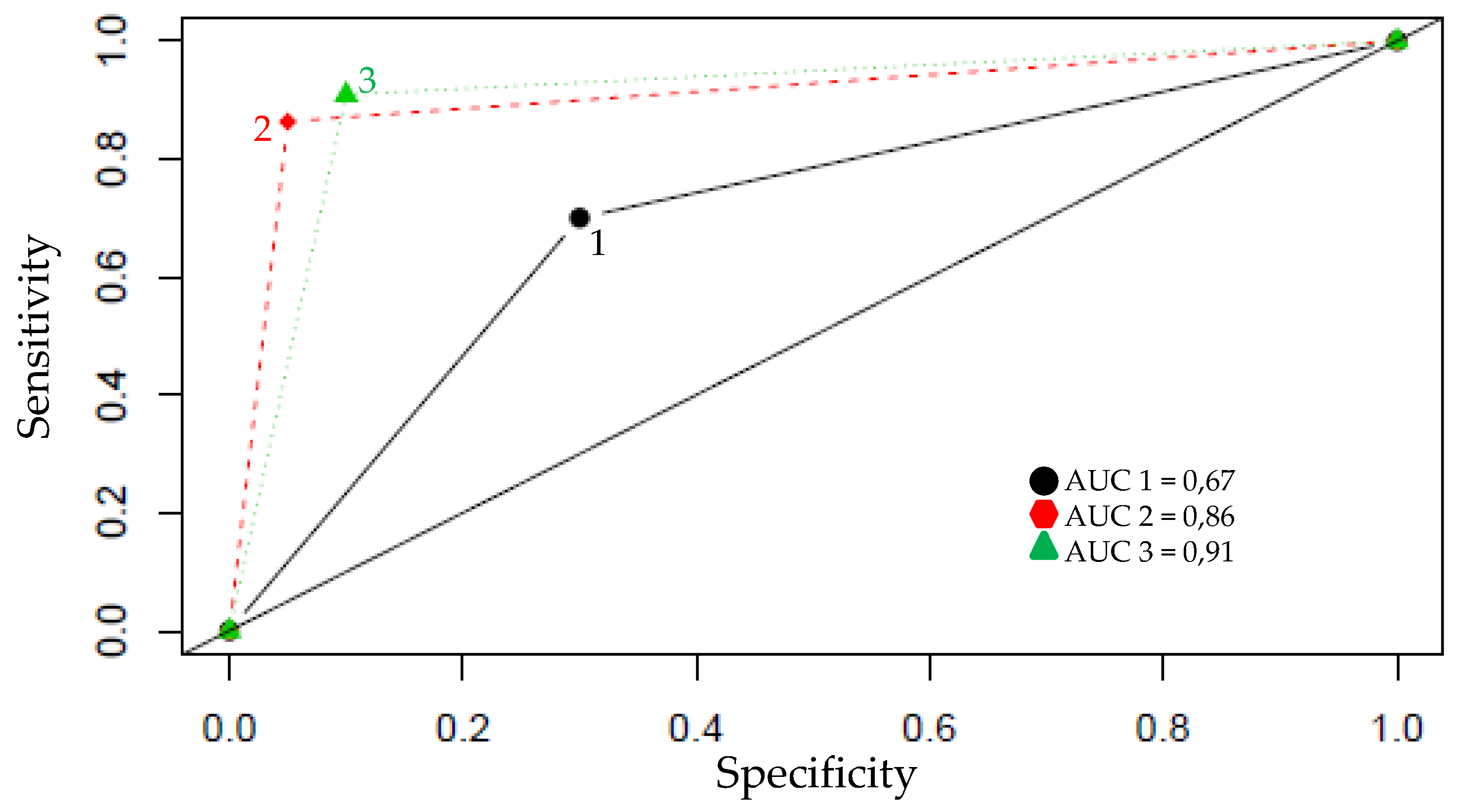
3.2. Agglomerative Hierarchical Cluster Analysis (AHCA)
- Cluster 1 (red) regrouped the controls and three children from the ASD group (subjects 23, 24 and 27). This cluster included children who had the best scores on muscular endurance and VO2 values, and low error scores on other motor items.
- Clusters 2 (green) and 4 (purple) only regrouped children with ASD. In these two clusters, these children have the lowest VO2 values and the highest error scores.
- Cluster 3 (blue) included two CONT and five ASD children. The two CONT children have the highest VO2 values (66.1 mLO2·kg−1·min−1 and 69.3 mLO2·kg−1·min−1, respectively) but they made many mistakes on the dexterity tests, balls skills and walk tests (seven and nine, respectively). The children with ASD in this cluster have the same profile: high VO2 values (mean = 53.2 mLO2·kg−1·min−1) but made many mistakes (mean = 10.8).
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Manual dexterity | Ball skills | Balance | |
|---|---|---|---|
| Band 2: 7–8 years | 1: Placing pegs 2: Threading lace 3: Drawing a line into a trail | 4: Bouncing and catching a ball with one hand 5: Throwing a bean bag into a box | 6: Stork balance 7: Jumping in squares 8: Heel-to-toe walking on a line |
| Band 3: 9–10 years | 1: Shifting pegs by rows 2: Threading nuts on a bolt 3: Drawing a line into a trail | 4: Throwing a ball at the wall and catching it 5: Throwing a bean bag into a box | 6: One-board balance 7: Hopping in squares 8: Walking while balancing a ball on a board |
| Band 4: 11–12 years | 1: Turning pegs 2: Cutting out an elephant 3: Drawing a line into a trail | 4: One-hand catch 5: Throwing at a wall target | 6: Two-board balance 7: Jumping and clapping 8: Walking backwards |
- Three tests to assess laterality: one for the preferential eye, one for the preferential hand (with 10 tasks) and one for the foot (with two tasks).
- Five tests to assess gait walking on a line: on heels, on toes, on the outsides of feet, forward, or backwards. The score is obtained by adding the number of errors.
- Six tests to assess stations: sustentation posture (one foot in front of the other) and sustentation steadiness (feet together) in order to maintain posture during 20 s finger to nose, stand on one foot; hop on one foot (50 hops max). The score is obtained by a code: 20 s = 0, 10–19 s = 1, <10 s = 2, and dysmetria (0-1-2).
- Flamingo Balance Test: this test assesses the ability to balance successfully on a single leg. While balancing on the preferred leg, the free leg is flexed at the knee. The number of falls in 30 s of balancing was used as the outcome.
- Plate Tapping Test: a reaction test using an alternating wall tapping action which measures upper body reaction time, hand–eye quickness and coordination. Two yellow discs are placed on a table with their centers 60 cm apart. The non-preferred hand is placed in the middle. The subject moves the preferred hand back and forth between the discs as quickly as possible for 25 full cycles (50 taps). The time is evaluated.
- Sit and Reach Flexibility Test: a common measure of flexibility of the lower back and hamstring muscles. The child—sitting on the floor with knees extended—is asked to bend the trunk and reach forward as far as possible. The line of the toes represented the zero point. Any measure beyond this line was positive and any measure below was negative. The score was expressed in centimeters and higher scores indicated better flexibility.
- Broad Jump Test: assesses explosive leg power. The child jumps as far as possible. The maximum horizontal distance reached was measured in centimeters.
- Hand Grip Strength Test: measures the maximum isometric strength of the hand and forearm muscles. The child holds the dynamometer (SMFD500TR1300N, Sensel, France) in the preferred hand. When ready, the child squeezes the dynamometer with maximum isometric effort. Hand grip measures the maximal amount of tension that could be applied in a single muscular contraction. The value was registered by a score on a digital sensor (PAXS0000, Sensel, France) in arbitrary units (a.u).
- EUROFIT Sit Up Test of Abdominal Strength and Muscular Endurance: the aim of this test is to perform as many sit ups as the subject can in 30 s. The child lays on a mat with knees bent at right angles, feet flat on the floor, and held down by a partner.
- Reactive Speed: the subject holds a stopwatch; it should start freely and then stop as fast as possible. The stopwatch shows a reaction time, evaluating action speed in milliseconds.
- Motor Educational Course: this is a test with successive motor tasks which must be consecutive in time and space (i.e., go under or go over obstacles, cones around which children turn, pick up a ball, throw it and then catch it again). The child has to run the course as fast as possible with no mistakes (omission or mistakes at obstacles). Pictograms are available for children with ASD for visual explanation. Children made a first attempt without running to discover and understand the exercises, and the second test was evaluated. The time is measured in seconds and the number of errors/omissions and knocking over of obstacles are recorded.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders-V, 5th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- Hilton, C.; Wente, L.; LaVesser, P.; Ito, M.; Reed, C.; Herzberg, G. Relationship between motor skill impairment and severity in children with Asperger syndrome. Res. Autism Spectr. Disord. 2007, 1, 339–349. [Google Scholar] [CrossRef]
- Fournier, K.A.; Hass, C.J.; Naik, S.K.; Lodha, N.; Cauraugh, J.H. Motor coordination in autism spectrum disorders: A synthesis and meta-Analysis. J. Autism. Dev. Disord. 2010, 40, 1227–1240. [Google Scholar] [CrossRef] [PubMed]
- Bhat, A.N.; Landa, R.J.; Galloway, J.C. Current Perspectives on Motor Functioning in Infants, Children, and Adults with Autism Spectrum Disorders. Phys. Ther. 2011, 91, 1116–1129. [Google Scholar] [CrossRef] [PubMed]
- Green, D.; Charman, T.; Pickles, A.; Chandler, S.; Loucas, T.; Simonoff, E.; Baird, G. Impairment in movement skills of children with autistic spectrum disorders. Dev. Med. Child Neurol. 2009, 51, 311–316. [Google Scholar] [CrossRef]
- Green, D.; Baird, G.; Barnett, A.L.; Henderson, L.; Huber, J.; Henderson, S.E. The severity and nature of motor impairment in Asperger’s syndrome: A comparison with specific developmental disorder of motor function. J. Child Psychol. Psychiatry 2002, 43, 655–668. [Google Scholar] [CrossRef] [PubMed]
- Ozonoff, S.; Young, G.S.; Goldring, S.; Greiss-Hess, L.; Herrera, A.M.; Steele, J.; Macari, S.; Hepburn, S.; Rogers, S.J. Gross motor development, movement abnormalities, and early identification of autism. J. Autism. Dev. Disord. 2008, 38, 644–656. [Google Scholar] [CrossRef] [PubMed]
- Dewey, D.; Cantell, M.; Crawford, S. Motor and gestural performance in children with autism spectrum disorders, developmental coordination disorder, and/or attention deficit hyperactivity disorder. J. Int. Neuropsychol. Soc. 2007, 13, 246–256. [Google Scholar] [CrossRef] [PubMed]
- Manjiviona, J.; Prior, M. Comparison of Asperger syndrome and high-Functioning autistic children on a test of motor impairment. J. Autism. Dev. Disord. 1995, 25, 23–39. [Google Scholar] [CrossRef] [PubMed]
- Provost, B. Levels of gross and fine motor development in young children with autism spectrum disorder. Phys. Occup. Ther. Pediatr. 2007, 27, 21–36. [Google Scholar] [CrossRef]
- Pace, M.; Bricout, V.-A. Assessment of motor skills for children with autism on the M-ABC. Sci. Sports 2016, 31, 336–341. [Google Scholar] [CrossRef]
- Vukićević, S.; Đorđević, M.; Glumbić, N.; Bogdanović, Z.; Đurić Jovičić, M.A. Demonstration Project for the Utility of Kinect-Based Educational Games to Benefit Motor Skills of Children with ASD. Percept. Mot. Skills 2019. [Google Scholar] [CrossRef]
- Chen, L.C.; Su, W.C.; Ho, T.L.; Lu, L.; Tsai, W.C.; Chiu, Y.N.; Jeng, S.F. Postural Control and Interceptive Skills in Children with Autism Spectrum Disorder. Phys. Ther. 2019, 99, 1231–1241. [Google Scholar] [CrossRef] [PubMed]
- Blair, S.N.; Cheng, Y.; Holder, J.S. Is physical activity or physical fitness more important in defining health benefits? Med. Sci. Sports Exerc. 2001, 33, 379–399. [Google Scholar] [CrossRef]
- Warburton, D.E.; Nicol, C.W.; Bredin, S.S. Health benefits of physical activity: The evidence. Can. Med. Assoc. J. 2006, 174, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Penedo, F.J.; Dahn, J.R. Exercise and well-Being: A review of mental and physical health benefits associated with physical activity. Curr. Opin. Psychiatry 2005, 18, 189–193. [Google Scholar] [CrossRef] [PubMed]
- Bricout, V.-A.; Pace, M.; Dumortier, L.; Baillieul, F.; Favre-Juvin, A.; Guinot, M. Reduced Cardiorespiratory Capacity in Children with Autism Spectrum Disorders. J. Clin. Med. 2018, 7, 361. [Google Scholar] [CrossRef]
- Gitimoghaddam, M.; McKellin, W.; Miller, A.R.; Weiss, J.A.; Majnemer, A.; Mâsse, L.C.; Brant, R.; Symington, V.; Wishart, R.L.; Collet, J.P. Gymnastic-Based Movement Therapy for Children with Neurodevelopmental Disabilities: Results from a Pilot Feasibility Study. Front. Pediatr. 2019, 7, 186. [Google Scholar] [CrossRef]
- Barak, S.; Oz, M.; Dagan, N.; Hutzler, Y. The Game of Life soccer program: Effect on skills, physical fitness and mobility in persons with intellectual disability and autism spectrum disorder. J. Appl. Res. Intellect. Disabil. 2019. [Google Scholar] [CrossRef]
- American College of Sports Medicine. Physical Fitness Assessment Manual, 4th ed.; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2014. [Google Scholar]
- Lord, C.; Risi, S.; Lambrecht, L.; Cook, E.H.; Leventhal, B.L.; DiLavore, P.C.; Pickles, A.; Rutter, M. The Autism Diagnostic Observation Schedule—Generic: A standard measure of social and communication deficits associated with the spectrum of autism. J. Autism Dev. Disord. 1999, 30, 205–223. [Google Scholar] [CrossRef]
- Wechsler, D. Wechsler Intelligence Scale for Children; American Psychological Association: New York, NY, USA, 2003. [Google Scholar]
- Sparrow, S.S.; Cicchetti, D.V. Diagnostic uses of the Vineland Adaptive Behavior Scales. J. Pediatr. Psychol. 1985, 10, 215–225. [Google Scholar] [CrossRef]
- Marshall, W.A.; Tanner, J.M. Variations in the pattern of pubertal changes in boys. Arch. Dis. Child. 1970, 45, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Willis, J.; Campbell, L. Exercise Psychology; Human Kinetics Publishers: Champaign, IL, USA, 1992. [Google Scholar]
- Henderson, S.E.; Sugden, D.A. Movement Assessment Battery for Children Manual; The Psychological Corporation Ltd.: London, UK, 1992. [Google Scholar]
- Denckla, M.B. Revised Neurological Examination for Subtle Signs. Psychopharmacol. Bull. 1985, 21, 773–800. [Google Scholar] [PubMed]
- Council of Europe. EUROFIT European Test of Physical Fitness; Central Direction for Sport’s Technical Activities Documentation and Information Division: Rome, Italy, 1988. [Google Scholar]
- Development Core Team R. R: A Language and Environment for Statistical Computing, Reference Index Version 2.15.1; R Foundation for Statistical Computing, Ed.; Development Core Team R: Vienna, Austria, 2012. [Google Scholar]
- Venables, W.N.; Ripley, B.D. Modern Applied Statistics with S; Springer Science & Business Media: Berlin, Germany, 2002. [Google Scholar]
- Zou, H.; Hastie, T. Regularization and variable selection via the elastic net. J. R. Stat. Soc. B 2005, 67, 301–320. [Google Scholar] [CrossRef]
- Ament, K.; Mejia, A.; Buhlman, R.; Erklin, S.; Caffo, B.; Mostofsky, S.; Wodka, E. Evidence for specificity of motor impairments in catching and balance in children with autism. J. Autism Dev. Disord. 2015, 45, 742–751. [Google Scholar] [CrossRef] [PubMed]
- Denckla, M.; Roeltgen, D. Disorders of Motor Function and Control; Elsevier: Amsterdam, The Netherlands, 1992. [Google Scholar]
- Dickinson, K.; Place, M. A Randomised Control Trial of the Impact of a Computer-Based Activity Programme upon the Fitness of Children with Autism. Autism Res. Treat. 2014, 2014, 419653. [Google Scholar] [CrossRef]
- Downey, R. Motor activity in children with autism: A review of current literature. Pediatr. Phys. Ther. 2012, 24, 2–20. [Google Scholar] [CrossRef]
- Dowell, L.R.; Mahone, E.M.; Mostofsky, S.H. Associations of postural knowledge and basic motor skill with dyspraxia in autism: Implication for abnormalities in distributed connectivity and motor learning. Neuropsychology 2009, 23, 563–570. [Google Scholar] [CrossRef]
- Jansiewicz, E.M.; Goldberg, M.C.; Newschaffer, C.J.; Denckla, M.B.; Landa, R.; Mostofsky, S.H. Motor signs distinguish children with high functioning autism and Asperger’s syndrome from controls. J. Autism Dev. Disord. 2006, 36, 613–621. [Google Scholar] [CrossRef]
- Kern, J.K.; Geier, D.A.; Adams, J.B.; Troutman, M.R.; Davis, G.A.; King, P.G.; Geier, M.R. Handgrip strength in autism spectrum disorder compared with controls. J. Strength Cond. Res. 2013, 27, 2277–2281. [Google Scholar]
- Pace, M.; Bricout, V.-A. Low heart rate response of children with autism spectrum disorders in comparison to controls during physical exercise. Physiol. Behav. 2015, 141, 63–68. [Google Scholar] [CrossRef]
- Pan, C.Y.; Tsai, C.L.; Chu, C.H. Fundamental movement skills in children diagnosed with autism spectrum disorders and attention deficit hyperactivity disorder. J. Autism Dev. Disord. 2009, 39, 1694–1705. [Google Scholar] [CrossRef] [PubMed]
- Piek, J.P.; Dyck, M.J.; Nieman, A.; Anderson, M.; Hay, D.; Smith, L.M.; McCoy, M.; Hallmayer, J. The relationship between motor coordination, executive functioning and attention in school aged children. Arch. Clin. Neuropsychol. 2004, 19, 1063–1076. [Google Scholar] [CrossRef] [PubMed]
- Schurink, J.; Hartman, E.; Scherder, E.J.A.; Houwen, S.; Visscher, C. Relationship between motor and executive functioning in school-Age children with pervasive developmental disorder not otherwise specified. Res. Autism Spectr. Disord. 2012, 6, 726–732. [Google Scholar] [CrossRef]
- Tyler, K.; MacDonald, M.; Menear, K. Physical activity and physical fitness of school-Aged children and youth with autism spectrum disorders. Autism Res. Treat. 2014, 2014, 312163. [Google Scholar] [CrossRef] [PubMed]
- Whyatt, C.P.; Craig, C.M. Motor skills in children aged 7–10 years, diagnosed with autism spectrum disorder. J. Autism Dev. Disord. 2012, 42, 1799–1809. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, I.; Yanarda, M.; Birkan, B.; Bumin, G. Effects of swimming training on physical fitness and water orientation in autism. Pediatr. Int. 2004, 46, 624–626. [Google Scholar] [CrossRef] [PubMed]
- Koziol, L.F.; Budding, D.; Andreasen, N.; D’Arrigo, S.; Bulgheroni, S.; Imamizu, H.; Ito, M.; Manto, M.; Marvel, C.; Parker, K.; et al. Consensus paper: The cerebellum’s role in movement and cognition. Cerebellum 2014, 13, 151–177. [Google Scholar] [CrossRef]
- Mostofsky, S.H.; Dubey, P.; Jerath, V.K.; Jansiewicz, E.M.; Goldberg, M.C.; Denckla, M.B. Developmental dyspraxia is not limited to imitation in children with autism spectrum disorders. J. Int. Neuropsychol. Soc. 2006, 12, 314–326. [Google Scholar] [CrossRef] [PubMed]
- Glazebrook, C.M.; Elliott, D.; Szatmari, P. How do individuals with autism plan their movements? J. Autism Dev. Disord. 2008, 38, 114–126. [Google Scholar] [CrossRef] [PubMed]

 = sum of errors on the 6 variables selected by the PCA (items B; C; D; E of M-ABC; tandem walking backward; walks on side of feet). Label 1: mainly characterized by CONT children (18 CONT and three ASD), with very good VO2 values (mean = 56.5 mLO2·kg−1·min−1) and with very few errors during motor evaluations. Two subgroups were observable depending on the muscular endurance: in label 1a, the mean value was lower than in label 1b (18.1 versus 29.6, respectively). Label 2: exclusively represented by children with ASD who had the same motor profile with average assessments. Label 3: mainly characterized by ASD children (five ASD + two CONT). In this group, children had satisfactory results, but the errors made on the tests were too numerous (>10) to be classified in another label. Label 4: exclusively represented by children with ASD who had the same motor profile, with low assessments.
= sum of errors on the 6 variables selected by the PCA (items B; C; D; E of M-ABC; tandem walking backward; walks on side of feet). Label 1: mainly characterized by CONT children (18 CONT and three ASD), with very good VO2 values (mean = 56.5 mLO2·kg−1·min−1) and with very few errors during motor evaluations. Two subgroups were observable depending on the muscular endurance: in label 1a, the mean value was lower than in label 1b (18.1 versus 29.6, respectively). Label 2: exclusively represented by children with ASD who had the same motor profile with average assessments. Label 3: mainly characterized by ASD children (five ASD + two CONT). In this group, children had satisfactory results, but the errors made on the tests were too numerous (>10) to be classified in another label. Label 4: exclusively represented by children with ASD who had the same motor profile, with low assessments.
 = sum of errors on the 6 variables selected by the PCA (items B; C; D; E of M-ABC; tandem walking backward; walks on side of feet). Label 1: mainly characterized by CONT children (18 CONT and three ASD), with very good VO2 values (mean = 56.5 mLO2·kg−1·min−1) and with very few errors during motor evaluations. Two subgroups were observable depending on the muscular endurance: in label 1a, the mean value was lower than in label 1b (18.1 versus 29.6, respectively). Label 2: exclusively represented by children with ASD who had the same motor profile with average assessments. Label 3: mainly characterized by ASD children (five ASD + two CONT). In this group, children had satisfactory results, but the errors made on the tests were too numerous (>10) to be classified in another label. Label 4: exclusively represented by children with ASD who had the same motor profile, with low assessments.
= sum of errors on the 6 variables selected by the PCA (items B; C; D; E of M-ABC; tandem walking backward; walks on side of feet). Label 1: mainly characterized by CONT children (18 CONT and three ASD), with very good VO2 values (mean = 56.5 mLO2·kg−1·min−1) and with very few errors during motor evaluations. Two subgroups were observable depending on the muscular endurance: in label 1a, the mean value was lower than in label 1b (18.1 versus 29.6, respectively). Label 2: exclusively represented by children with ASD who had the same motor profile with average assessments. Label 3: mainly characterized by ASD children (five ASD + two CONT). In this group, children had satisfactory results, but the errors made on the tests were too numerous (>10) to be classified in another label. Label 4: exclusively represented by children with ASD who had the same motor profile, with low assessments.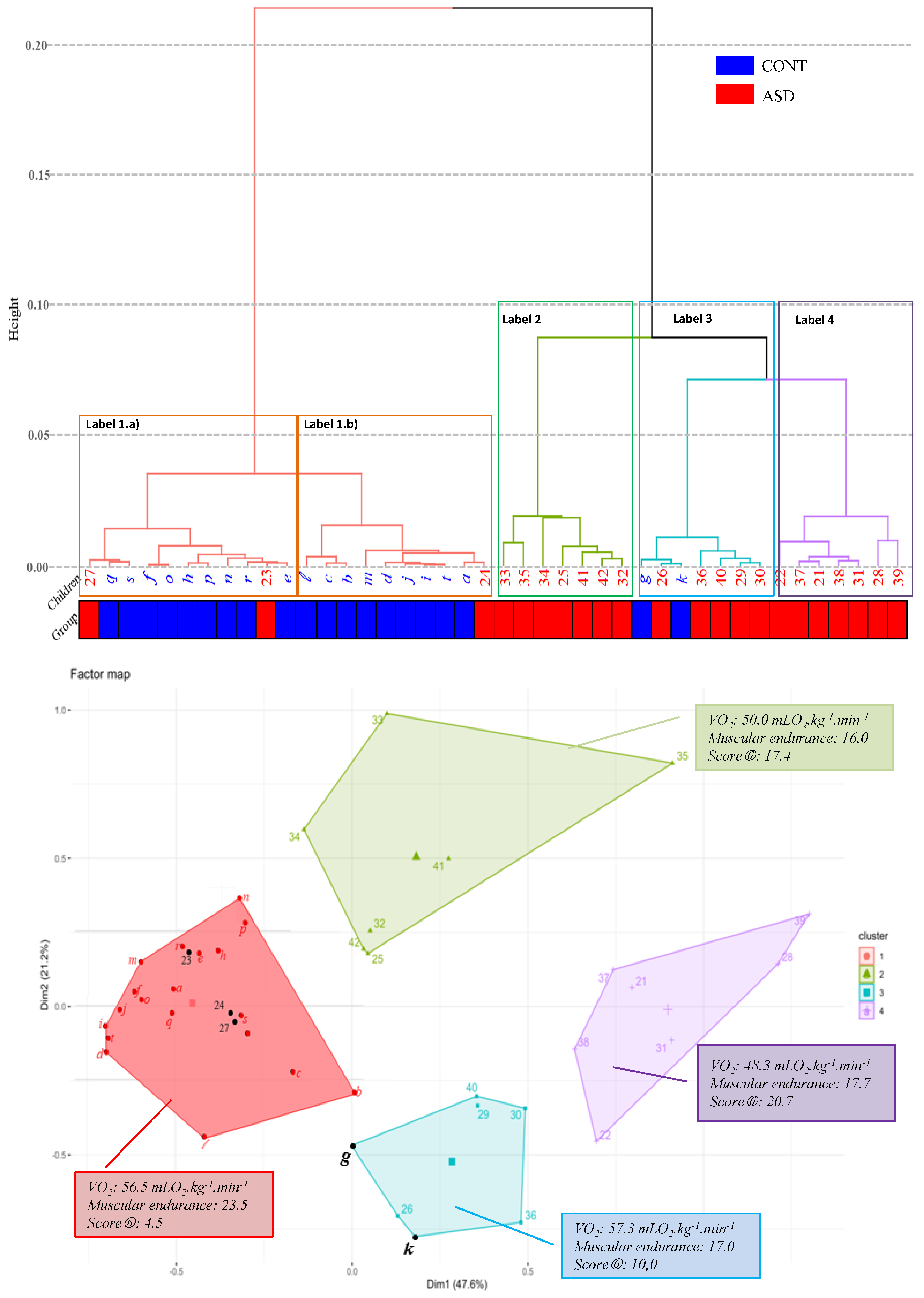
| CONT (n = 20) | ASD (n = 22) | |
|---|---|---|
| Age (years, min–max) | 10.0 ± 1.6 (8–12) | 10.7 ± 1.3 (8–12) |
| Weight (kg) | 33.3 ± 7.2 | 36.0 ± 13.3 |
| Height (cm) | 141.0 ± 10.5 | 144.7 ± 8.7 |
| BMI (kg/m2) | 16.0 ± 1.5 | 16.8 ± 3.8 |
| Ratio waist/hip | 0.88 ± 0.05 | 0.89 ± 0.05 |
| Tanner stage 1 (no. of subjects) | 16 | 16 |
| Tanner stage 2 (no. of subjects) | 4 | 6 |
| Vineland Assessment | ||
| Communication | 121 ± 5 | 105 ± 12 *** |
| Daily living skills | 132 ± 12 | 114 ± 13 *** |
| Socialization | 106 ± 9 | 88 ± 11 *** |
| Aerobic Capacity | CONT | ASD |
|---|---|---|
| VO2peak (mLO2·kg−1·min−1) | 58.1 ± 8.8 | 50.6 ± 8.9 ** |
| EUROFIT and Additional Tests | ||
| Flamingo Balance Test (s) | 29.4 ± 2.7 | 26.4 ± 6.6 |
| Plate Tapping Test (s) | 41.9 ± 9.7 | 43.4 ± 9.4 |
| Sit and Reach Flexibility (cm) | −16.4 ± 8.3 | −22.0 ± 7.1 * |
| Broad Jump (cm) | 132.0 ± 22.6 | 113.8 ± 23.6 ** |
| Vertical Jump (cm) | 24.2 ± 5.9 | 21.4 ± 7.1 |
| Hand Grip Strength Test (a.u) | 162 ± 51 | 127 ± 39 ** |
| EUROFIT Sit Up Test (n) | 23.2 ± 6.3 | 17.5 ± 5.2 * |
| Reactive Speed (ds) | 22.7 ± 3.3 | 21.0 ± 4.1 |
| Motor Educational Course (s) | 14.5 ± 2.3 | 18.9 ± 5.4 ** |
| M-ABC | ||
| Dexterity (score total of items A, B and C) | 2.08 ± 3.02 | 7.22 ± 4.28 *** |
| Ball skills (score total of items D and E) | 0.76 ± 1.22 | 3.41 ± 3.03 *** |
| Balance (score total of items F, G and H) | 1.84 ± 2.00 | 3.39 ± 3.58 |
| Total score of M-ABC | 4.68 ± 3.95 | 14.02 ± 8.29 *** |
| PANESS | CONT | ASD |
|---|---|---|
| Lateral preference pattern (1) | 1.75 ± 1.01 (12 Right/2 Left/5 mixed/1 eye alone) | 1.90 ± 1.26 (14 Right/4 mixed/4 eye alone) |
| Walks on heels (2) | 2.9 ± 1.6 (0 to 7) | 3.5 ± 3.3 (1 to 15) |
| Walks on tiptoe (2) | 0.2 ± 0.4 (0 to 1) | 0.6 ± 0.8 (0 to 3) * |
| Walks on side of feet (2) | 1.3 ± 1.3 (0 to 5) | 3.1 ± 2.3 (0 to 8) ** |
| Tandem walk forward (2) | 0.3 ± 0.6 (0 to 2) | 2.2 ± 3.6 (0 to 15) * |
| Tandem walk backward (2) | 1.1 ± 1.1(0 to 4) | 3.4 ± 3.5 (0 to 15) ** |
| Sustentation posture (3) | 18.5 ± 4.0 | 15.9 ± 6.5 |
| Sustentation steadiness (3) | 19.6 ± 1.6 | 19.9 ± 0.2 |
| Finger to nose (L+R) (2) | 0.1 ± 0.44 (0–2) | 0.32 ± 0.72 (0–2) |
| Tongue protrusion (3) | 20.0 ± 0.0 | 18.6 ± 3.7 NS |
| Stand on one foot (mean L+R) (3) | 28.6 ± 3.4 | 24.3 ± 7.7 * |
| Hop on one foot (mean L+R) (4) | 49.8 ± 0.9 | 41.9 ± 15.2 * |
| Foot tap (mean L+R) (3) | 7.0 ± 1.8 | 7.0 ± 2.1 |
| Foot heel toe tap (mean L+R) (3) | 9.3 ± 2.5 | 11.0 ± 4.2 |
| Hand pat (mean L+R) (3) | 6.1 ± 2.1 | 6.0 ± 1.7 |
| Hand pronation/supination (mean L+R) (3) | 7.9 ± 2.0 | 8.1 ± 2.0 |
| Finger tap (mean L+R) (3) | 6.8 ± 1.1 | 6.3 ± 1.4 |
| Finger succession (mean L+R) (3) | 10.6 ± 2.8 | 11.0 ± 3.5 |
| Tongue wiggles side to side (3) | 9.0 ± 2.3 | 8.5 ± 2.6 |
| Global score of PANESS | ||
| Gait and balance total score | 6.60 ± 3.64 | 17.50 ± 12.68 *** |
| Dysrhythmias | 1.3 ± 1.2 | 3.0 ± 1.3 *** |
| Impersistence | 0.60 ± 1.32 | 2.09 ± 3.68 |
| Involuntary movement score | 1.40 ± 1.14 | 1.40 ± 1.50 |
| Repetitive speed of movement score | 12.80 ± 3.06 | 15.22 ± 9.2 |
| Overflow, grand total | 5.75 ± 4.43 | 10.0 ± 7.26 * |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
BRICOUT, V.-A.; PACE, M.; DUMORTIER, L.; MIGANEH, S.; MAHISTRE, Y.; GUINOT, M. Motor Capacities in Boys with High Functioning Autism: Which Evaluations to Choose? J. Clin. Med. 2019, 8, 1521. https://doi.org/10.3390/jcm8101521
BRICOUT V-A, PACE M, DUMORTIER L, MIGANEH S, MAHISTRE Y, GUINOT M. Motor Capacities in Boys with High Functioning Autism: Which Evaluations to Choose? Journal of Clinical Medicine. 2019; 8(10):1521. https://doi.org/10.3390/jcm8101521
Chicago/Turabian StyleBRICOUT, Véronique-Aurélie, Marion PACE, Léa DUMORTIER, Sahal MIGANEH, Yohan MAHISTRE, and Michel GUINOT. 2019. "Motor Capacities in Boys with High Functioning Autism: Which Evaluations to Choose?" Journal of Clinical Medicine 8, no. 10: 1521. https://doi.org/10.3390/jcm8101521
APA StyleBRICOUT, V.-A., PACE, M., DUMORTIER, L., MIGANEH, S., MAHISTRE, Y., & GUINOT, M. (2019). Motor Capacities in Boys with High Functioning Autism: Which Evaluations to Choose? Journal of Clinical Medicine, 8(10), 1521. https://doi.org/10.3390/jcm8101521





