Annual Trends in Total Ischemic Time and One-Year Fatalities: The Paradox of STEMI Network Performance Assessment
Abstract
:1. Introduction
2. Experimental Section
2.1. PL-ACS Registry
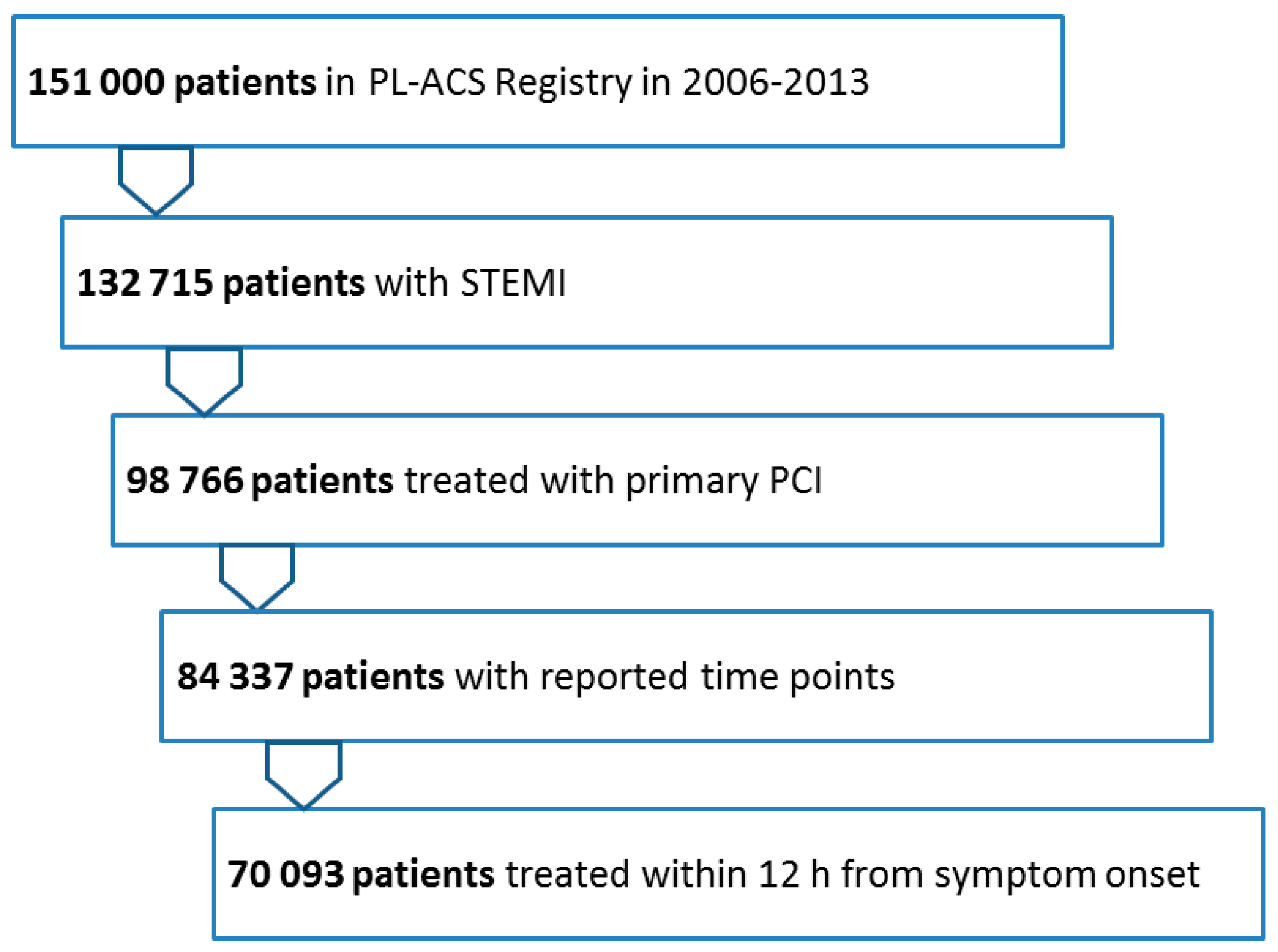
2.2. Current Analysis
2.3. Follow-Up
2.4. Statistics
2.5. Role of the Funding Source
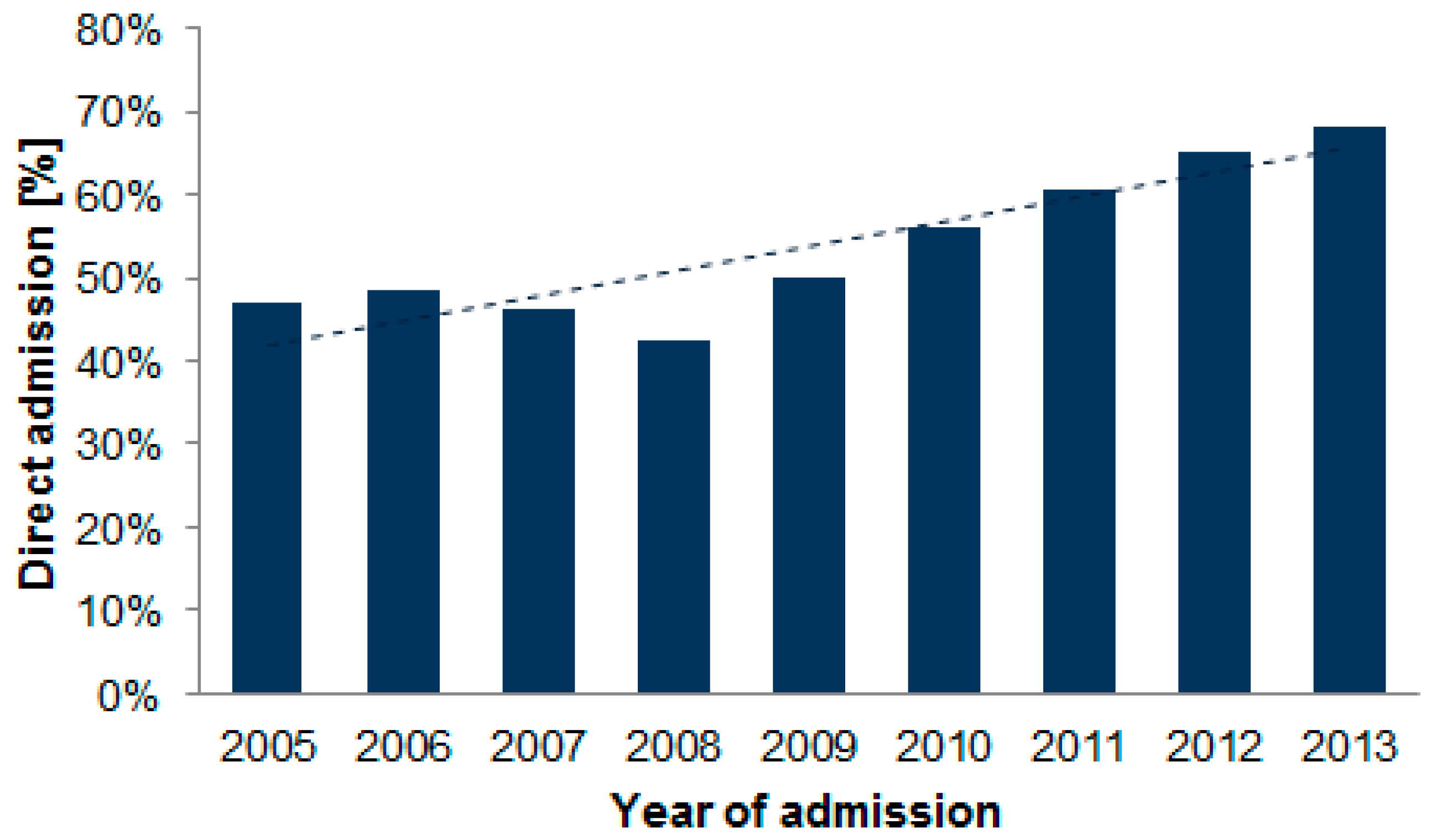
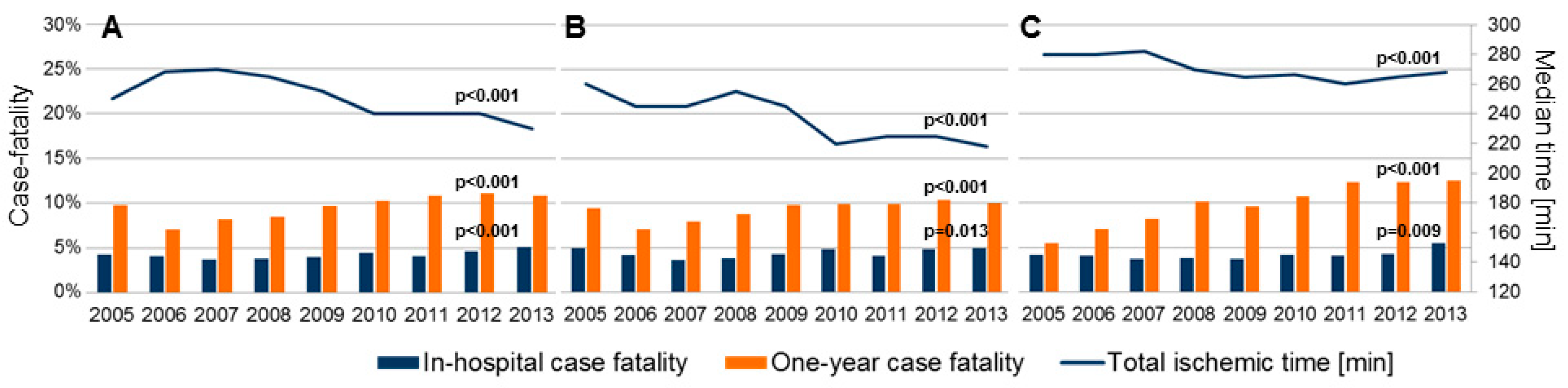
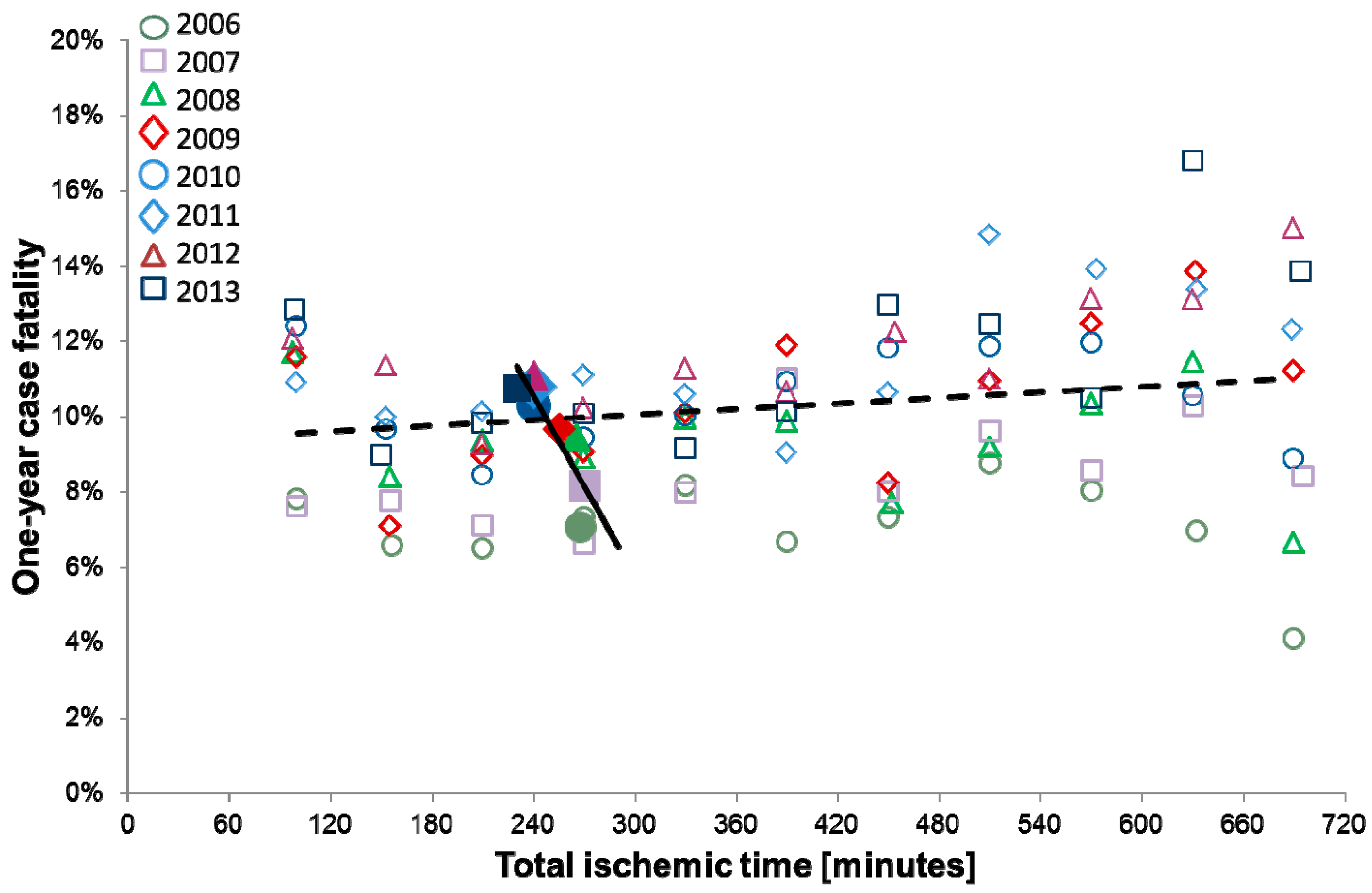
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gierlotka, M.; Zdrojewski, T.; Wojtyniak, B.; Polonski, L.; Stokwiszewski, J.; Gasior, M.; Kozierkiewicz, A.; Kalarus, Z.; Wierucki, L.; Chlebus, K.; et al. Incidence, treatment, in-hospital mortality and one-year outcomes of acute myocardial infarction in Poland in 2009–2012—Nationwide AMI-PL database. Kardiol. Pol. 2015, 73, 142–158. [Google Scholar] [CrossRef] [PubMed]
- Gierlotka, M.; Polonski, L.; Zdrojewski, T.; Gasior, M.; Wojtyniak, B.; Chlebus, K.; Kozierkiewicz, A.; Wierucki, L.; Stokwiszewski, J.; Rutkowski, D.; et al. Early and late outcomes and implementation of the ESC guidelines in NSTEMI and STEMI—A population approach to evaluate the system of care for AMI patients in Poland in 2009–2013. Eur. Heart J. 2017, 38, 2288. [Google Scholar] [CrossRef]
- Reimer, K.A.; Lowe, J.E.; Rasmussen, M.M.; Jennings, R.B. The wavefront phenomenon of ischemic cell death. 1. Myocardial infarct size vs duration of coronary occlusion in dogs. Circulation 1977, 56, 786–794. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2017, 39, 119–177. [Google Scholar]
- Barbagelata, A.; Perna, E.R.; Clemmensen, P.; Uretsky, B.F.; Canella, J.P.; Califf, R.M.; Granger, C.B.; Adams, G.L.; Merla, R.; Birnbaum, Y. Time to reperfusion in acute myocardial infarction. It is time to reduce it! J. Electrocardiol. 2007, 40, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Dudek, D.; Legutko, J.; Siudak, Z.; Maciejewski, P.; Ochala, A.; Karcz, M.; Wojakowski, W.; Peruga, Z.; Araszkiewicz, A.; Deptuch, T.; et al. Interventional cardiology in Poland in 2011. Report of the Board of the Association of Cardiovascular Interventions of the Polish Society of Cardiology. Postep. Kardiol. Interwencyjnej 2012, 8, 108–113. [Google Scholar]
- Polonski, L.; Gasior, M.; Gierlotka, M.; Kalarus, Z.; Cieslinski, A.; Dubiel, J.S.; Gil, R.J.; Ruzyllo, W.; Trusz-Gluza, M.; Zembala, M.; et al. Polish Registry of Acute Coronary Syndromes (PL-ACS). Characteristics, treatments and outcomes of patients with acute coronary syndromes in Poland. Kardiol. Pol. 2007, 65, 861–872, discussion 873–874. [Google Scholar]
- Flynn, M.R.; Barrett, C.; Cosio, F.G.; Gitt, A.K.; Wallentin, L.; Kearney, P.; Lonergan, M.; Shelley, E.; Simoons, M.L. The Cardiology Audit and Registration Data Standards (CARDS), European data standards for clinical cardiology practice. Eur. Heart J. 2005, 26, 308–313. [Google Scholar] [CrossRef]
- De Luca, G.; Suryapranata, H.; Ottervanger, J.P.; Antman, E.M. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: Every minute of delay counts. Circulation 2004, 109, 1223–1225. [Google Scholar] [CrossRef]
- Shanmugasundaram, M. Percutaneous coronary intervention in elderly patients: Is it beneficial? Tex. Heart Inst. J. 2011, 38, 398–403. [Google Scholar]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; de Ferranti, S.; Despres, J.P.; Fullerton, H.J.; et al. Heart Disease and Stroke Statistics-2016 Update: A Report from the American Heart Association. Circulation 2016, 133, e38–e360. [Google Scholar] [CrossRef] [PubMed]
- Shanmugam, V.B.; Harper, R.; Meredith, I.; Malaiapan, Y.; Psaltis, P.J. An overview of PCI in the very elderly. J. Geriatr. Cardiol. 2015, 12, 174–184. [Google Scholar] [PubMed]
- Nallamothu, B.K.; Normand, S.L.; Wang, Y.; Hofer, T.P.; Brush, J.E.; Messenger, J.C., Jr.; Bradley, E.H.; Rumsfeld, J.S.; Krumholz, H.M. Relation between door-to-balloon times and mortality after primary percutaneous coronary intervention over time: A retrospective study. Lancet 2015, 385, 1114–1122. [Google Scholar] [CrossRef]
- Sejersten, M.; Ripa, R.S.; Maynard, C.; Grande, P.; Andersen, H.R.; Wagner, G.S.; Clemmensen, P. DANAMI-2 Investigators. Timing of ischemic onset estimated from the electrocardiogram is better than historical timing for predicting outcome after reperfusion therapy for acute anterior myocardial infarction: A DANish trial in Acute Myocardial Infarction 2 (DANAMI-2) substudy. Am. Heart J. 2007, 154, 61.e1–61.e8. [Google Scholar] [PubMed]
- Kawecki, D.; Gierlotka, M.; Morawiec, B.; Hawranek, M.; Tajstra, M.; Skrzypek, M.; Wojakowski, W.; Polonski, L.; Nowalany-Kozielska, E.; Gasior, M. Direct Admission Versus Interhospital Transfer for Primary Percutaneous Coronary Intervention in ST-Segment Elevation Myocardial Infarction. JACC Cardiovasc. Interv. 2017, 10, 438–447. [Google Scholar] [CrossRef] [PubMed]
- Denktas, A.E.; Anderson, H.V.; McCarthy, J.; Smalling, R.W. Total ischemic time: The correct focus of attention for optimal ST-segment elevation myocardial infarction care. JACC Cardiovasc. Interv. 2011, 4, 599–604. [Google Scholar] [CrossRef] [PubMed]
- Sejersten, M.; Birnbaum, Y.; Ripa, R.S.; Maynard, C.; Wagner, G.S.; Clemmensen, P. DANAMI-2 Investigators. Influences of electrocardiographic ischaemia grades and symptom duration on outcomes in patients with acute myocardial infarction treated with thrombolysis versus primary percutaneous coronary intervention: Results from the DANAMI-2 trial. Heart 2006, 92, 1577–1582. [Google Scholar]
- Andersen, H.R.; Nielsen, T.T.; Rasmussen, K.; Thuesen, L.; Kelbaek, H.; Thayssen, P.; Abildgaard, U.; Pedersen, F.; Madsen, J.K.; Grande, P.; et al. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N. Engl. J. Med. 2003, 349, 733–742. [Google Scholar] [CrossRef]
- De Luca, G.; Cassetti, E.; Marino, P. Percutaneous coronary intervention-related time delay, patient’s risk profile, and survival benefits of primary angioplasty vs lytic therapy in ST-segment elevation myocardial infarction. Am. J. Emerg. Med. 2009, 27, 712–719. [Google Scholar] [CrossRef]
- Denktas, A.E.; Athar, H.; Henry, T.D.; Larson, D.M.; Simons, M.; Chan, R.S.; Niles, N.W.; Thiele, H.; Schuler, G.; Ahn, C.; et al. Reduced-dose fibrinolytic acceleration of ST-segment elevation myocardial infarction treatment. JACC Cardiovasc. Interv. 2008, 1, 504–510. [Google Scholar] [CrossRef]
- Prasad, A.; Gersh, B.J.; Mehran, R.; Brodie, B.R.; Brener, S.J.; Dizon, J.M.; Lansky, A.J.; Witzenbichler, B.; Kornowski, R.; Guagliumi, G.; et al. Effect of Ischemia Duration and Door-to-Balloon Time on Myocardial Perfusion in ST-Segment Elevation Myocardial Infarction: An Analysis From HORIZONS-AMI Trial (Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction). JACC Cardiovasc. Interv. 2015, 8, 1966–1974. [Google Scholar] [CrossRef] [PubMed]
- Hugelshofer, S.; Roffi, M.; Witassek, F.; Eberli, F.R.; Pilgrim, T.; Pedrazzini, G.; Rickli, H.; Radovanovic, D.; Erne, P.; Degrauwe, S.; et al. Impact of total ischemic time on manual thrombus aspiration benefit during primary percutaneous coronary intervention. Am. Heart J. 2018, 204, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Finney, J.W.; Humphreys, K.; Kivlahan, D.R.; Harris, A.H. Why health care process performance measures can have different relationships to outcomes for patients and hospitals: Understanding the ecological fallacy. Am. J. Public Health 2011, 101, 1635–1642. [Google Scholar] [CrossRef] [PubMed]
- Blaus, A.; Madabushi, R.; Pacanowski, M.; Rose, M.; Schuck, R.N.; Stockbridge, N.; Temple, R.; Unger, E.F. Personalized Cardiovascular Medicine Today: A Food and Drug Administration/Center for Drug Evaluation and Research Perspective. Circulation 2015, 132, 1425–1432. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total n = 70,093 | 2006 n = 7940 | 2007 n = 7428 | 2008 n = 6618 | 2009 n = 7932 | 2010 n = 10,463 | 2011 n = 9748 | 2012 n = 10,450 | 2013 n = 9514 | p Value for Trend |
|---|---|---|---|---|---|---|---|---|---|---|
| Age | 63 (55–73) | 61 (53–71) | 62 (54–72) | 62 (55–72) | 62 (55–72) | 62 (55–73) | 63 (55–74) | 63 (56–74) | 64 (56–74) | <0.001 |
| Age > 75 y | 14,746, 21% | 1318, 16.6% | 1352, 18.2% | 1323, 20% | 1539, 20.1% | 2268, 21.7% | 2248, 23.1% | 2407, 23% | 2237, 23% | <0.001 |
| Male sex | 48,248, 68.8% | 5569, 70.1% | 5226, 70.4% | 4532, 68.5% | 5540, 69.8% | 7333, 70.1% | 6630, 68.0% | 7167, 68.6% | 6251, 65.7% | <0.001 |
| Hyper-tension | 44,899, 64.1% | 4719, 59.4% | 4474, 60.2% | 4061, 61.4% | 5034, 63.5% | 6871, 65.7% | 6516, 66.8% | 6891, 65.9% | 6333, 66.6% | <0.001 |
| Diabetes Mellitus | 15,558, 22.2% | 1328, 16.7% | 1408, 19.0% | 1525, 23.0% | 1820, 22.9% | 2515, 24.0% | 2296, 23.6% | 2426, 23.2% | 2240, 23.5% | <0.001 |
| Smoking | 41,609, 59.4% | 3481, 43.8% | 3565, 48.0% | 3930, 59.4% | 4914, 62.0% | 6576, 62.9% | 6200, 63.6% | 6816, 65.2% | 6127, 64.4% | <0.001 |
| Obesity | 12,375, 17.7% | 1205, 15.2% | 1156, 15.6% | 1133, 17.1% | 1491, 18.8% | 1880, 18.0% | 1779, 18.2% | 1908, 18.3% | 1823, 19.2% | <0.001 |
| Prior AMI | 8166, 11.7% | 941, 11.9% | 846, 11.4% | 701, 10.6% | 886, 11.2% | 1250, 11.9% | 1138, 11.7% | 1282, 12.3% | 1122, 11.8% | 0.063 |
| Prior PCI | 4889, 7.0% | 102, 1.3% | 244, 3.3% | 396, 6.0% | 612, 7.7% | 866, 8.3% | 812, 8.3% | 979, 9.4% | 878, 9.2% | <0.001 |
| PriorCABG | 1429,2.0% | 377, 4.7% | 285, 3.8% | 121, 1.8% | 124, 1.6% | 136, 1.3% | 125, 1.3% | 125, 1.2% | 136, 1.4% | <0.001 |
| EF ≤ 35% | 15,200, 27.6% | 1519, 27.1% | 1376, 26.8% | 1314, 27.4% | 1678, 26.9% | 2308, 28.1% | 2161, 26.7% | 2477, 28.0% | 2376, 28.9% | 0.005 |
| Anterior AMI | 28,240, 40.3% | 3219, 40.5% | 2973, 40.0% | 2631, 39.8% | 3175. 40.0% | 4233, 40.5% | 3916, 40.2% | 4241, 40.6% | 3852, 40.5% | 0.45 |
| Killip class 3 | 1158, 1.7% | 118, 1.5% | 117, 1.6% | 92, 1.4% | 116, 1.5% | 195, 1.9% | 159, 1.6% | 197, 1.9% | 164, 1.7% | 0.013 |
| Killip class 4 | 3315, 4.7% | 356, 4.5% | 328, 4.4% | 274, 4.1% | 375, 4.7% | 514, 4.9% | 438, 4.5% | 530, 5.1% | 500, 5.3% | <0.001 |
| Pre-hospital cardiac arrest | 1677, 2.4% | 279, 3.5% | 262, 3.5% | 143, 2.2% | 154, 1.9% | 242, 2.3% | 217, 2.2% | 216, 2.1% | 164, 1.7% | <0.001 |
| Variable | Total n = 70,093 | 2006 n = 7940 | 2007 n = 7428 | 2008 n = 6618 | 2009 n = 7932 | 2010 n = 10,463 | 2011 n = 9748 | 2012 n = 10,450 | 2013 n = 9514 | P Value for Trend |
|---|---|---|---|---|---|---|---|---|---|---|
| Total ischemic time annual [minutes] | 250 | 268 | 270 | 265 | 255 | 240 | 240 | 240 | 230 | <0.001 |
| (165–400) | (180–415) | (180–430) | (175–417) | (170–400) | (160–395) | (158–385) | (160–395) | (153–390) | ||
| Symptom-to-door time [minutes] | 185 | 195 | 195 | 195 | 195 | 180 | 180 | 180 | 176 | <0.001 |
| (120–310) | (125–315) | (121–326) | (125–326) | (120–315) | (114–310) | (110–300) | (115–305) | (109–300) | ||
| Door-to-balloon time [minutes] | 42 | 46 | 45 | 45 | 41 | 43 | 43 | 44 | 42 | <0.001 |
| (30–64) | (30–75) | (30–75) | (30–73) | (30–65) | (30–65) | (30–65) | (30–67) | (30–64) | ||
| In-hospital case fatality | 3007, 4.3% | 324, 4.1% | 272, 3.7% | 252, 3.8% | 314, 4.0% | 475, 4.5% | 402, 4.1% | 481, 4.6% | 487, 5.1% | <0.001 |
| One-year case fatality | 6973, 9.8% | 561, 7.1% | 606, 8.2% | 627, 8.5% | 767, 9.7% | 1077, 10.3% | 1053, 0.8% | 1158,11.1% | 1024,10.8% | <0.001 |
| HR | 95% CI | p Value | HR | 95% CI | p Value | |
|---|---|---|---|---|---|---|
| Univariate | ||||||
| Symptom-to-PCI time patient specific * | 1.014 | 1.007–1.022 | <0.001 | - | - | - |
| Symptom-to-PCI time annual † | 0.911 | 0.989–0.993 | <0.001 | - | - | - |
| Multivariable | ||||||
| Symptom-to-PCI time patient specific * | 1.024 | 1.015–1.034 | <0.001 | 1.024 | 1.015–1.034 | <0.001 |
| Symptom-to-PCI time annual † | 0.992 | 0.989–0.994 | <0.001 | 1.006 | 0.998–1.013 | 0.139 |
| Age >75 years | 3.30 | 3.10–3.52 | <0.001 | 3.30 | 3.10–3.52 | <0.001 |
| Male sex | 0.93 | 0.87–0.99 | 0.019 | 0.93 | 0.87–0.99 | 0.022 |
| Hypertension | 0.87 | 0.81–0.93 | <0.001 | 0.87 | 0.81–0.93 | <0.001 |
| Diabetes mellitus | 1.30 | 1.21–1.39 | <0.001 | 1.29 | 1.21–1.38 | <0.001 |
| Prior AMI | 1.06 | 0.96–1.17 | 0.28 | 1.06 | 0.96–1.18 | 0.23 |
| Prior PCI | 0.59 | 0.51–0.69 | <0.001 | 0.59 | 0.50–0.68 | <0.001 |
| Anterior STEMI | 1.15 | 1.08–1.22 | <0.001 | 1.15 | 1.08–1.22 | <0.001 |
| Pre-hospital cardiac arrest | 1.82 | 1.58–2.09 | 0.001 | 1.84 | 1.59–2.11 | <0.001 |
| Cardiogenic shock | 4.38 | 4.01–4.80 | <0.001 | 4.39 | 4.01–4.80 | <0.001 |
| Inter-hospital transfer | 1.11 | 1.04–1.18 | 0.001 | 1.12 | 1.05–1.19 | 0.001 |
| LVEF (per 10% more) | 0.62 | 0.60–0.63 | <0.001 | 0.62 | 0.60–0.63 | <0.001 |
| Year of admission † | - | - | - | 1.09 | 1.05–1.14 | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawecki, D.; Morawiec, B.; Gąsior, M.; Wilczek, K.; Nowalany-Kozielska, E.; Gierlotka, M. Annual Trends in Total Ischemic Time and One-Year Fatalities: The Paradox of STEMI Network Performance Assessment. J. Clin. Med. 2019, 8, 78. https://doi.org/10.3390/jcm8010078
Kawecki D, Morawiec B, Gąsior M, Wilczek K, Nowalany-Kozielska E, Gierlotka M. Annual Trends in Total Ischemic Time and One-Year Fatalities: The Paradox of STEMI Network Performance Assessment. Journal of Clinical Medicine. 2019; 8(1):78. https://doi.org/10.3390/jcm8010078
Chicago/Turabian StyleKawecki, Damian, Beata Morawiec, Mariusz Gąsior, Krzysztof Wilczek, Ewa Nowalany-Kozielska, and Marek Gierlotka. 2019. "Annual Trends in Total Ischemic Time and One-Year Fatalities: The Paradox of STEMI Network Performance Assessment" Journal of Clinical Medicine 8, no. 1: 78. https://doi.org/10.3390/jcm8010078
APA StyleKawecki, D., Morawiec, B., Gąsior, M., Wilczek, K., Nowalany-Kozielska, E., & Gierlotka, M. (2019). Annual Trends in Total Ischemic Time and One-Year Fatalities: The Paradox of STEMI Network Performance Assessment. Journal of Clinical Medicine, 8(1), 78. https://doi.org/10.3390/jcm8010078





