Virtual Reality Distraction during Endoscopic Urologic Surgery under Spinal Anesthesia: A Randomized Controlled Trial
Abstract
1. Introduction
2. Methods
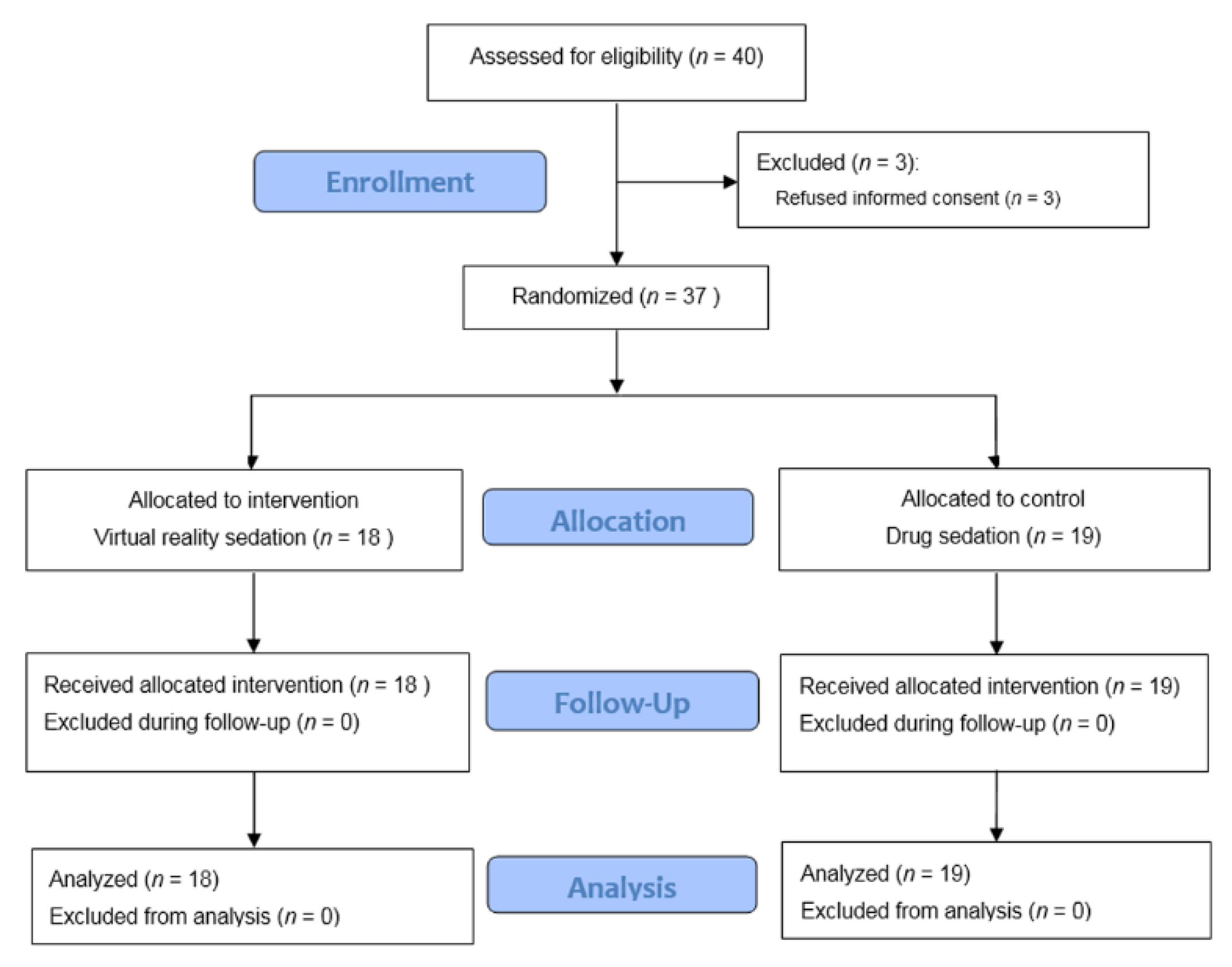
2.1. Study Design
2.2. Patients
2.3. Anesthesia Protocol
2.4. VR Group
2.5. Study Outcomes
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Li, A.; Montano, Z.; Chen, V.J.; Gold, J.I. Virtual reality and pain management: Current trends and future directions. Pain Manag. 2011, 1, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Zeng, N.; Pope, Z.; Lee, J.E.; Gao, Z. Virtual reality exercise for anxiety and depression: A preliminary review of current research in an emerging field. J. Clin. Med. 2018, 7, 42. [Google Scholar] [CrossRef] [PubMed]
- Jensen, J.K.; Dyre, L.; Jorgensen, M.E.; Andreasen, L.A.; Tolsgaard, M.G. Simulation-based point-of-care ultrasound training: A matter of competency rather than volume. Acta Anaesthesiol. Scand. 2018, 62, 811–819. [Google Scholar] [CrossRef] [PubMed]
- Zaveri, P.P.; Davis, A.B.; O’Connell, K.J.; Willner, E.; Aronson Schinasi, D.A.; Ottolini, M. Virtual reality for pediatric sedation: A randomized controlled trial using simulation. Cureus 2016, 8, e486. [Google Scholar] [CrossRef]
- Jensen, K.; Ringsted, C.; Hansen, H.J.; Petersen, R.H.; Konge, L. Simulation-based training for thoracoscopic lobectomy: A randomized controlled trial: Virtual-reality versus black-box simulation. Surg. Endosc. 2014, 28, 1821–1829. [Google Scholar] [CrossRef] [PubMed]
- Kulcsar, Z.; O’Mahony, E.; Lovquist, E.; Aboulafia, A.; Sabova, D.; Ghori, K.; Iohom, G.; Shorten, G. Preliminary evaluation of a virtual reality-based simulator for learning spinal anesthesia. J. Clin. Anesth. 2013, 25, 98–105. [Google Scholar] [CrossRef]
- Latif, R.K.; Bautista, A.; Duan, X.; Neamtu, A.; Wu, D.; Wadhwa, A.; Akça, O. Teaching basic fiberoptic intubation skills in a simulator: Initial learning and skills decay. J. Anesth. 2016, 30, 12–19. [Google Scholar] [CrossRef]
- Gold, J.I.; Kim, S.H.; Kant, A.J.; Joseph, M.H.; Rizzo, A.S. Effectiveness of virtual reality for pediatric pain distraction during IV placement. Cyberpsychol. Behav. 2006, 9, 207–212. [Google Scholar] [CrossRef]
- Furman, E.; Jasinevicius, T.R.; Bissada, N.F.; Victoroff, K.Z.; Skillicorn, R.; Buchner, M. Virtual reality distraction for pain control during periodontal scaling and root planing procedures. J. Am. Dent. Assoc. 2009, 140, 1508–1516. [Google Scholar] [CrossRef]
- Morris, L.D.; Louw, Q.A.; Grimmer-Somers, K. The effectiveness of virtual reality on reducing pain and anxiety in burn injury patients: A systematic review. Clin. J. Pain 2009, 25, 815–826. [Google Scholar] [CrossRef]
- Ryu, J.H.; Park, J.W.; Nahm, F.S.; Jeon, Y.T.; Oh, A.Y.; Lee, H.J.; Kim, J.H.; Han, S.H. The effect of gamification through a virtual reality on preoperative anxiety in pediatric patients undergoing general anesthesia: A prospective, randomized, and controlled trial. J. Clin. Med. 2018, 7, 284. [Google Scholar] [CrossRef] [PubMed]
- Chan, P.Y.; Scharf, S. Virtual reality as an adjunctive nonpharmacological sedative during orthopedic surgery under regional anesthesia: A pilot and feasibility study. Anesth. Analg. 2017, 125, 1200–1202. [Google Scholar] [CrossRef] [PubMed]
- Angelini, G.; Ketzler, J.T.; Coursin, D.B. Use of propofol and other nonbenzodiazepine sedatives in the intensive care unit. Crit. Care Clin. 2001, 17, 863–880. [Google Scholar] [CrossRef]
- Shafer, A. Complications of sedation with midazolam in the intensive care unit and a comparison with other sedative regimens. Crit. Care Med. 1998, 26, 947–956. [Google Scholar] [CrossRef]
- Ramsay, M.A.; Savege, T.M.; Simpson, B.R.; Goodwin, R. Controlled sedation with alphaxalone-alphadolone. Br. Med. J. 1974, 2, 656–659. [Google Scholar] [CrossRef]
- Aldrete, J.A. Modifications to the postanesthesia score for use in ambulatory surgery. J. PeriAnesth. Nurs. 1998, 13, 148–155. [Google Scholar] [CrossRef]
- Nagendran, M.; Gurusamy, K.S.; Aggarwal, R.; Loizidou, M.; Davidson, B.R. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst. Rev. 2013, 8, Cd006575. [Google Scholar] [CrossRef]
- Piromchai, P.; Avery, A.; Laopaiboon, M.; Kennedy, G.; O’Leary, S. Virtual reality training for improving the skills needed for performing surgery of the ear, nose or throat. Cochrane Database Syst. Rev. 2015, 9, Cd010198. [Google Scholar] [CrossRef]
- Teeley, A.M.; Soltani, M.; Wiechman, S.A.; Jensen, M.P.; Sharar, S.R.; Patterson, D.R. Virtual reality hypnosis pain control in the treatment of multiple fractures: A case series. Am. J. Clin. Hypn. 2012, 54, 184–194. [Google Scholar] [CrossRef]
- Patterson, D.R.; Jensen, M.P.; Wiechman, S.A.; Sharar, S.R. Virtual reality hypnosis for pain associated with recovery from physical trauma. Int. J. Clin. Exp. Hypn. 2010, 58, 288–300. [Google Scholar] [CrossRef]
- Enea, V.; Dafinoiu, I.; Opris, D.; David, D. Effects of hypnotic analgesia and virtual reality on the reduction of experimental pain among high and low hypnotizables. Int. J. Clin. Exp. Hypn. 2014, 62, 360–377. [Google Scholar] [CrossRef] [PubMed]
- Dockx, K.; Bekkers, E.M.; Van den Bergh, V.; Ginis, P.; Rochester, L.; Hausdorff, J.M.; Mirelman, A.; Nieuwboer, A. Virtual reality for rehabilitation in Parkinson’s disease. Cochrane Database Syst. Rev. 2016, 12, Cd010760. [Google Scholar] [CrossRef] [PubMed]
- Laver, K.E.; Lange, B.; George, S.; Deutsch, J.E.; Saposnik, G.; Crotty, M. Virtual reality for stroke rehabilitation. Cochrane Database Syst. Rev. 2017, 11, Cd008349. [Google Scholar] [CrossRef] [PubMed]
- Pandya, P.G.; Kim, T.E.; Howard, S.K.; Stary, E.; Leng, J.C.; Hunter, O.O.; Mariano, E.R. Virtual reality distraction decreases routine intravenous sedation and procedure-related pain during preoperative adductor canal catheter insertion: A retrospective study. Korean J. Anesthesiol. 2017, 70, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.S.; Song, E.S.; Lee, K.H.; Park, Y.H.; Shin, W.C.; Ku, J.H. Sleep-related nocturnal erections and erections during midazolam-induced sedation in healthy young men. Int. J. Impot. Res. 2006, 18, 522–526. [Google Scholar] [CrossRef] [PubMed]
- Sriganesh, K.; Reddy, M.; Jena, S.; Mittal, M.; Rao, G.S.U. A comparative study of dexmedetomidine and propofol as sole sedative agents for patients with aneurysmal subarachnoid hemorrhage undergoing diagnostic cerebral angiography. J. Anesth. 2015, 29, 409–415. [Google Scholar] [CrossRef]
- Ryu, J.H.; Park, S.J.; Park, J.W.; Kim, J.W.; Yoo, H.J.; Kim, T.W.; Hong, J.S.; Han, S.H. Randomized clinical trial of immersive virtual reality tour of the operating theatre in children before anaesthesia. Br. J. Surg. 2017, 104, 1628–1633. [Google Scholar] [CrossRef] [PubMed]
- Muller, S.; Borowics, S.M.; Fortis, E.A.; Stefani, L.C.; Soares, G.; Maguilnik, I.; Breyer, H.P.; Hidalgo, M.P.; Caumo, W. Clinical efficacy of dexmedetomidine alone is less than propofol for conscious sedation during ERCP. Gastrointest. Endosc. 2008, 67, 651–659. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H. Safe sedation and hypnosis using dexmedetomidine for minimally invasive spine surgery in a prone position. Korean J. Pain 2014, 27, 313–320. [Google Scholar] [CrossRef]
- Arain, S.R.; Ebert, T.J. The efficacy, side effects, and recovery characteristics of dexmedetomidine versus propofol when used for intraoperative sedation. Anesth. Analg. 2002, 95, 461–466. [Google Scholar]
- Ter Bruggen, F.; Eralp, I.; Jansen, C.K.; Stronks, D.L.; Huygen, F. Efficacy of dexmedetomidine as a sole sedative agent in small diagnostic and therapeutic procedures: A systematic review. Pain Pract. 2017, 17, 829–840. [Google Scholar] [CrossRef] [PubMed]
| Rater | Score | Description |
|---|---|---|
| Surgeon | 1 (extremely dissatisfied) | Any of the following: 1. Patients involuntarily moved or repeatedly spoke, which made the surgical procedure stop more than twice. 2. Persistent penile erection (3 or more episode lasting >10 s) that significantly interfered with the surgical procedure and required phenylephrine injection. |
| 2 (dissatisfied) | Any of the following: 1. Patients involuntarily moved or repeatedly spoke, which made the surgical procedure stop once. 2. Persistent penile erection (2 or more episodes >10 s) that interfered with the surgical procedure, but not used phenylephrine. | |
| 3 (undecided) | Any of the following: 1. Patients involuntarily moved or spoke a little, but no interference with the surgical procedure. 2. Transient penile erection (<10 s) that did not interfere with surgical procedure significantly. | |
| 4 (satisfied) | All of the following: 1. No patient’s voluntary movement or speaking. No interference with the surgical procedure. 2. Transient penile erection (<10 s) which did not interfere with the surgical procedure at all. | |
| 5 (extremely satisfied) | All of the following: 1. No patient’s voluntary movement or speaking. No interference with the surgical procedure. 2. No penile erection at all. | |
| Patient | 1 (extremely dissatisfied) | Any of the following: 1. Patients recalled all steps of the surgical procedure. 2. Patients felt severe pain during surgery (NRS ≥ 7). 3. Patients repeatedly moved due to discomfort. |
| 2 (dissatisfied) | Any of the following: 1. Patients recalled about two-thirds of the surgical procedure time (including recall of inserting and withdrawing the fiberoptic scope into the urethra). 2. Patients felt moderate pain (NRS of 4 to 6). 3. Patients moved several times due to discomfort. | |
| 3 (undecided) | Any of the following: 1. Patients recalled less than one-third of the surgical procedure time. 2. Patients felt mild pain (NRS of 2 to 3). | |
| 4 (satisfied) | All of the following: 1. No patient’s recall of surgery. 2. No pain at all. 3. Patients felt comfortable during surgery. | |
| 5 (extremely satisfied) | All of the following: 1. No patient’s recall of surgery. 2. No pain at all. 3. Patients felt extreme comfort and were not concerned about the lithotomy position and surgery at all. | |
| Anesthesiologist | 1 (extremely dissatisfied) | Any of the following: 1. Patients involuntarily moved 3 or more times and repeatedly spoke which interfered the surgical procedure. 2. More than three events of apnea. 3. Desaturation (SpO2 < 90% more than 5 s) more than twice. 4. Assisted ventilation required due to desaturation and apnea. |
| 2 (dissatisfied) | Any of the following: 1. Patients involuntarily moved or spoke 1 to 2 times, which interfered the surgical procedure. 2. Apnea developed twice. 3. Desaturation (SpO2 < 90% more than 5 s) once. 4. Oral or nasal airway insertion due to desaturation or apnea. | |
| 3 (undecided) | All of the following: 1. Patients involuntarily moved or spoke 1 to 2 times, but did not interfere with the surgery. 2. Apnea developed once but did not require oral or nasal airway insertion or assisted ventilation. | |
| 4 (satisfied) | All of the following: 1. No patient’s voluntary movement or speaking. 2. Apnea developed once but did not require oral or nasal airway insertion or assisted ventilation. | |
| 5 (extremely satisfied) | All of the following: 1. No patient’s voluntary movement or speaking. 2. No Apnea. |
| Variables | VR Group | Sedation Group |
|---|---|---|
| Case number, n | 18 | 19 |
| Age, years | 69 (65–70) | 69 (63–72) |
| Weight, kg | 69 (64–73) | 64 (62–69) |
| Height, cm | 167 (163–170) | 167 (162–170) |
| Body-mass index, kg m−2 | 24.8 (23.3–26.9) | 23.9 (21.3–25.1) |
| ASA PS, 1/2/3 | 7/7/4 | 9/7/3 |
| Underlying disease (n) | ||
| Hypertension | 8 (44.4) | 8 (42.1) |
| Diabetes Mellitus | 3 (16.7) | 3 (15.8) |
| Angina pectoris | 3 (15.8) | 3 (16.7) |
| Stroke | 2 (11.1) | - |
| Chronic obstructive pulmonary disease | - | 1 (5.3) |
| Chronic kidney disease | 2 (11.1) | - |
| Prostate weight (g) | 65 (38–98) | 75 (39–110) |
| Duration of anesthesia (min) | 65 (55–100) | 65 (60–85) |
| Duration of surgery (min) | 40 (35–75) | 45 (30–60) |
| Fluid administration (mL) | 200 (60–200) | 100 (70–150) |
| Colloid administration (mL) | - | - |
| Variables | VR Group | Sedation Group | p-Value |
|---|---|---|---|
| Case number, n | 18 | 19 | |
| Intraoperative variables | |||
| Patients who do not move involuntarily during surgery, n | 16 (88.9) | 13 (68.4) | 0.001 |
| Patients who requested to stop watching VR, n | 0 | - | |
| Midazolam administration, mg | 4 (4–6) | - | |
| Administration of rescue sedative, n | 0 | 0 | |
| Desaturation (SpO2 < 90%, more than 5 s), n | 0 | 1 (5.3) | 0.999 |
| Apnea (flat ETco2, more than 5 s) | |||
| Develop, n | 1 (5.6) | 7 (36.8) | 0.042 |
| Frequency in the patients with apnea, range | 1–2 | 1–5 | |
| Assisted mask ventilation, n | 0 | 1 | 0.999 |
| Conversion to general anesthesia, n | 0 | 0 | |
| Ephedrine administration | |||
| Incidence, n | 2 (11.1) | 6 (31.6) | 0.232 |
| Dose, median (IQR) (range), mg | 0 [0,0] (5–10) | 0 (0–5) (5–10) | 0.313 |
| Atropine administration | |||
| Incidence, n | 1 (5.6) | 4 (21.1) | 0.340 |
| Dose, median (IQR) (range), mg | 0 [0,0] (0–0.5) | 0 (0–0) (0–0.5) | 0.425 |
| Nausea (≥3 of numerical rating scale), n | 0 | 2 | 0.486 |
| Vomiting. n | 0 | 0 | |
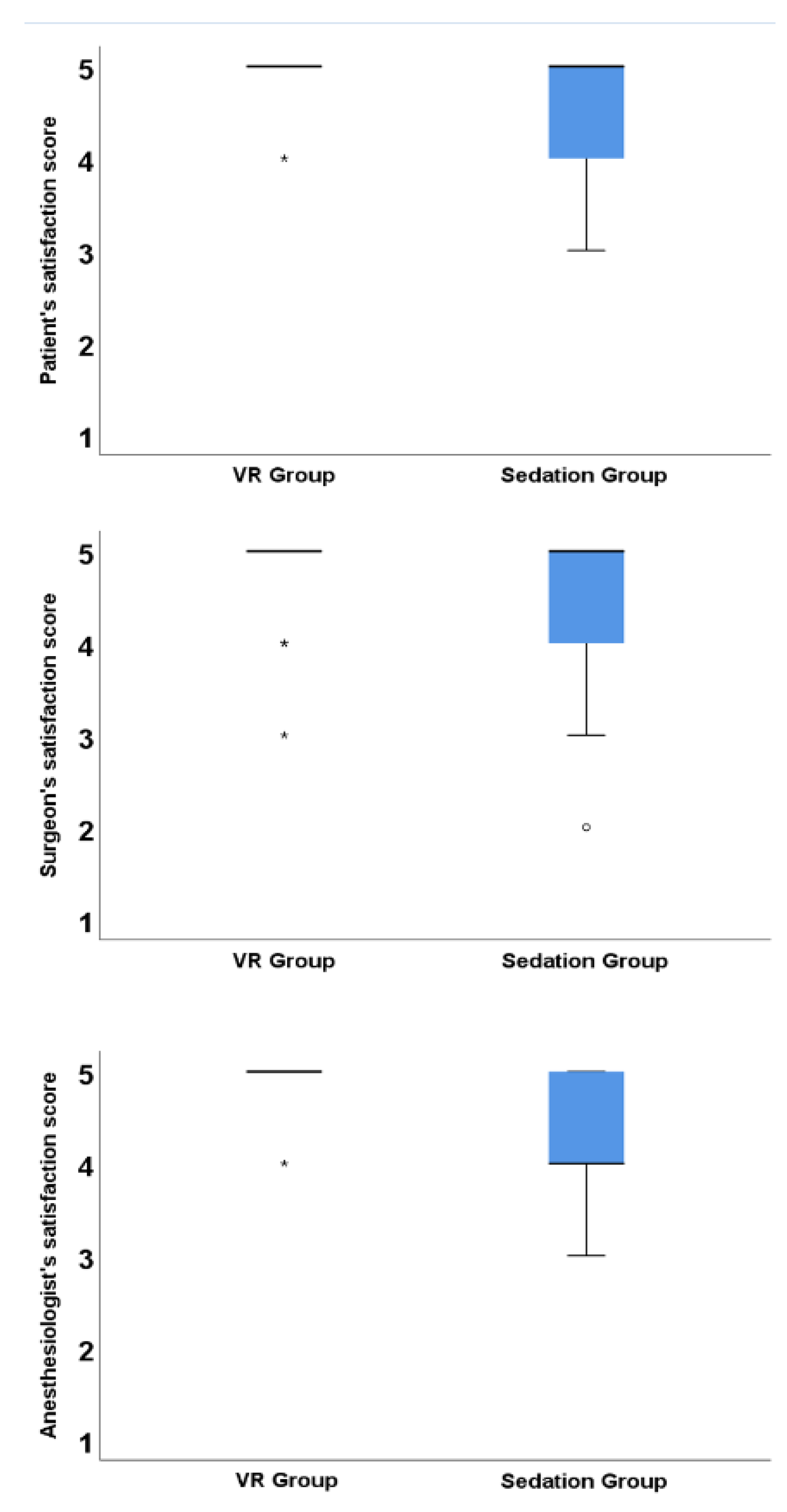
| Satisfaction score as a continuous variable | |||
| Patient | 5 (5–5) | 5 (4–5) | 0.105 |
| Surgeon | 5 (5–5) | 5 (4–5) | 0.558 |
| Anesthesiologist | 5 (5–5) | 4 (4–5) | 0.005 |
| Incidence of extreme satisfaction | |||
| Patient | 17 (94.4) | 12 (63.2) | 0.042 |
| Surgeon | 14 (77.8) | 13 (68.4) | 0.714 |
| Anesthesiologist | 17 (94.4) | 8 (42.1) | 0.001 |
| Recovery room parameters | |||
| Remember the operative procedure, n | 0 | 3 (15.8) | 0.230 |
| Felt procedural pain during surgery, n | 0 | 0 | |
| Duration of recovery room stay, min | 27 (21–44) | 29 (22–53) | 0.620 |
| Nausea (≥3 of numerical rating scale), n | 1 | 2 | 0.999 |
| Vomiting, n | 0 | 0 | |
| Optimal patient, anesthesia, and surgical condition, n | 17 (94.4) | 12 (63.2) | 0.042 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moon, J.Y.; Shin, J.; Chung, J.; Ji, S.-H.; Ro, S.; Kim, W.H. Virtual Reality Distraction during Endoscopic Urologic Surgery under Spinal Anesthesia: A Randomized Controlled Trial. J. Clin. Med. 2019, 8, 2. https://doi.org/10.3390/jcm8010002
Moon JY, Shin J, Chung J, Ji S-H, Ro S, Kim WH. Virtual Reality Distraction during Endoscopic Urologic Surgery under Spinal Anesthesia: A Randomized Controlled Trial. Journal of Clinical Medicine. 2019; 8(1):2. https://doi.org/10.3390/jcm8010002
Chicago/Turabian StyleMoon, Jee Youn, Jungho Shin, Jaeyeon Chung, Sang-Hwan Ji, Soohan Ro, and Won Ho Kim. 2019. "Virtual Reality Distraction during Endoscopic Urologic Surgery under Spinal Anesthesia: A Randomized Controlled Trial" Journal of Clinical Medicine 8, no. 1: 2. https://doi.org/10.3390/jcm8010002
APA StyleMoon, J. Y., Shin, J., Chung, J., Ji, S.-H., Ro, S., & Kim, W. H. (2019). Virtual Reality Distraction during Endoscopic Urologic Surgery under Spinal Anesthesia: A Randomized Controlled Trial. Journal of Clinical Medicine, 8(1), 2. https://doi.org/10.3390/jcm8010002





