Association of Depression and Cervical Spondylosis: A Nationwide Retrospective Propensity Score-Matched Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Data Availability Statement
2.3. Ethics Statement
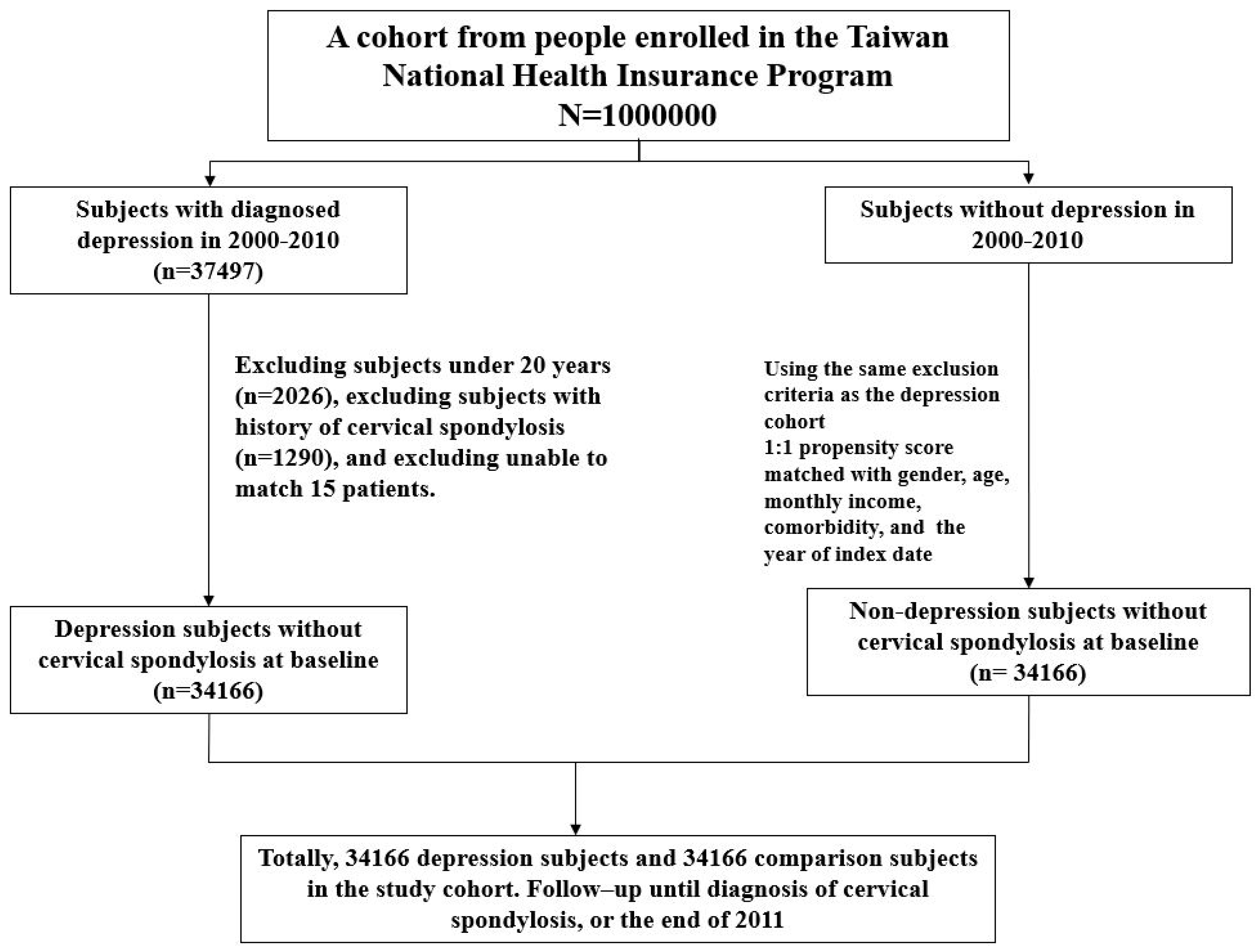
2.4. Study Population
2.5. Statistical Analyses
3. Results
4. Discussion
5. Limitations
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kalsi-Ryan, S.; Karadimas, S.K.; Fehlings, M.G. Cervical spondylotic myelopathy: The clinical phenomenon and the current pathobiology of an increasingly prevalent and devastating disorder. Neuroscientist 2013, 19, 409–421. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, D.M.; Brower, R.S. Cervical spondylotic myelopathy. Clinical syndrome and natural history. Orthop. Clin. N. Am. 1992, 23, 487–493. [Google Scholar]
- Brinjikji, W.; Luetmer, P.H.; Comstock, B.; Bresnahan, B.W.; Chen, L.E.; Deyo, R.A.; Halabi, S.; Turner, J.A.; Avins, A.L.; James, K.; et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. Am. J. Neuroradiol. 2015, 36, 811–816. [Google Scholar] [CrossRef] [PubMed]
- King, J.T.J.; McGinnis, K.A.; Roberts, M.S. Quality of life assessment with the medical outcomes study short form-36 among patients with cervical spondylotic myelopathy. Neurosurgery 2003, 52, 113–121. [Google Scholar] [PubMed]
- Wang, S.Y.; Liu, L.C.; Lu, M.C.; Koo, M. Comparisons of musculoskeletal disorders among ten different medical professions in Taiwan: A nationwide, population-based study. PLoS ONE 2015, 10, e0123750. [Google Scholar] [CrossRef] [PubMed]
- Baron, E.M.; Young, W.F. Cervical spondylotic myelopathy: A brief review of its pathophysiology, clinical course, and diagnosis. Neurosurgery 2007, 60, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.; Lopez, A.D. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet 1997, 349, 1498–1504. [Google Scholar] [CrossRef]
- Carson, A.J.; MacHale, S.; Allen, K.; Lawrie, S.M.; Dennis, M.; House, A.; Sharpe, M. Depression after stroke and lesion location: A systematic review. Lancet 2000, 356, 122–126. [Google Scholar] [CrossRef]
- Remy, P.; Doder, M.; Lees, A.; Turjanski, N.; Brooks, D. Depression in Parkinson’s disease: Loss of dopamine and noradrenaline innervation in the limbic system. Brain 2005, 128, 1314–1322. [Google Scholar] [CrossRef] [PubMed]
- Stoffman, M.R.; Roberts, M.S.; King, J.T.J. Cervical spondylotic myelopathy, depression, and anxiety: A cohort analysis of 89 patients. Neurosurgery 2005, 57, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Ford, D.E.; Mead, L.A.; Chang, P.P.; Cooper-Patrick, L.; Wang, N.Y.; Klag, M.J. Depression is a risk factor for coronary artery disease in men: The precursors study. Arch. Intern. Med. 1999, 158, 1422–1426. [Google Scholar] [CrossRef]
- Ownby, R.L.; Crocco, E.; Acevedo, A.; John, V.; Loewenstein, D. Depression and risk for Alzheimer disease: Systematic review, meta-analysis, and metaregression analysis. Arch. Gen. Psychiatry 2006, 63, 530–538. [Google Scholar] [CrossRef] [PubMed]
- Zonderman, A.B.; Costa, P.T.J.; McCrae, R.R. Depression as a risk for cancer morbidity and mortality in a nationally representative sample. JAMA 1989, 262, 1191–1195. [Google Scholar] [CrossRef] [PubMed]
- Barth, J.; Schumacher, M.; Herrmann-Lingen, C. Depression as a risk factor for mortality in patients with coronary heart disease: A meta-analysis. Psychosom. Med. 2004, 66, 802–813. [Google Scholar] [CrossRef] [PubMed]
- Moussavi, S.; Chatterji, S.; Verdes, E.; Tandon, A.; Patel, V.; Ustun, B. Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. Lancet 2007, 370, 851–858. [Google Scholar] [CrossRef]
- Keenan-Miller, D.; Hammen, C.L.; Brennan, P.A. Health outcomes related to early adolescent depression. J. Adolesc. Health 2007, 41, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Black, S.A.; Markides, K.S.; Ray, L.A. Depression predicts increased incidence of adverse health outcomes in older Mexican Americans with type 2 diabetes. Diabetes Care 2003, 26, 2822–2828. [Google Scholar] [CrossRef] [PubMed]
- Rosario, J.L.; Bezerra Diógenes, M.S.; Mattei, R.; Leite, J.R. Differences and similarities in postural alterations caused by sadness and depression. J. Bodyw. Mov. Ther. 2014, 14, 540–544. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.C.; Groarke, P.J.; Butler, J.S.; Poynton, A.R.; O’Byrne, J.M. The Natural History and Clinical Syndromes of Degenerative Cervical Spondylosis. Adv. Orthop. 2012, 2012, 393642. [Google Scholar] [CrossRef] [PubMed]
- Al-Tamimi, Y.Z.; Guilfoyle, M.; Seeley, H.; Laing, R.J. Measurement of long-term outcome in patients with cervical spondylotic myelopathy treated surgically. Eur. Spine J. 2013, 22, 2552–2557. [Google Scholar] [CrossRef] [PubMed]
- Hwang, C.Y.; Chen, Y.J.; Lin, M.W.; Chen, T.J.; Chu, S.Y.; Chen, C.C.; Lee, D.D.; Chang, Y.T.; Wang, W.J.; Liu, H.N. Prevalence of atopic dermatitis, allergic rhinitis and asthma in Taiwan: A national study 2000 to 2007. Acta. Derm. Venereol. 2010, 90, 589–594. [Google Scholar] [PubMed]
- Kao, C.H. Author’s Reply: National Health Insurance database in Taiwan. Eur. Int. Med. 2016, 31, e11–e12. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.L.; Wang, T.C.; Shen, T.C.; Huang, Y.J.; Lin, C.L.; Sung, F.C. Risk of depression in patients with chronic rhinosinusitis: A nationwide population-based retrospective cohort study. J. Affect. Disord. 2016, 206, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Parsons, L.S. Performing a 1: N Case-Control Match on Propensity Score. In Proceedings of the 29th Annual SAS Users Group International Conference, Seattle, Washington, USA, 2001; SAS Institute: Cary, NC, USA, 2004; pp. 165–229. [Google Scholar]
- Fan, C.Y.; Chao, H.L.; Lin, C.S.; Huang, W.Y.; Chen, C.M.; Lin, K.T.; Lin, C.L.; Kao, C.H. Risk of depressive disorder among patients with head and neck cancer: A nationwide population-based study. Head Neck 2018, 40, 312–323. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.M.; Liang, J.A.; Lin, C.L.; Sun, S.; Kao, C.H. Risk of mood disorders in patients with colorectal cancer. J. Affect. Disord. 2017, 218, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Chiu, C.H.; Wang, Y.C.; Lin, C.L.; Lee, F.Y.; Kao, C.H. Leptospirosis and Depression: A Nationwide Cohort Analysis. J. Clin. Psychiatry 2017, 78, e398–e403. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.F.; Tu, T.H.; Chen, Y.C.; Wu, J.C.; Chang, P.Y.; Liu, L.; Huang, W.C.; Lo, S.S.; Cheng, H. Risk of spinal cord injury in patients with cervical spondylotic myelopathy and ossification of posterior longitudinal ligament: A national cohort study. Neurosurg. Focus 2016, 40, E4. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.C.; Ko, C.C.; Yen, Y.S.; Huang, W.C.; Chen, Y.C.; Liu, L.; Tu, T.H.; Lo, S.S.; Cheng, H. Epidemiology of cervical spondylotic myelopathy and its risk of causing spinal cord injury: A national cohort study. Neurosurg. Focus 2013, 35, E10. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat. Med. 2009, 28, 3083–3107. [Google Scholar] [CrossRef] [PubMed]
- Fleming, T.H.; Harrington, D.P. Nonparametric estimation of the survival distribution in censored data. Commun. Stat. Theory Methods 1984, 13, 2469–2486. [Google Scholar] [CrossRef]
- Kalbfleisch, J.D.; Prentice, R.L. The Statistical Analysis of Failure Time Data, 1st ed.; John Wiley & Sons: New York, NY, USA, 1980. [Google Scholar]
- Link, C.L. Confidence intervals for the survival function using Cox’s proportional hazards model with covariates. Biometrics 1984, 40, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Wolkowitz, O.M.; Epel, E.S.; Reus, V.I.; Mellon, S.H. Depression gets old fast: Do stress and depression accelerate cell aging? Depress. Anxiety 2010, 27, 327–338. [Google Scholar] [CrossRef] [PubMed]
- Canales, J.Z.; Cordás, T.A.; Fiquer, J.T.; Cavalcante, A.F.; Moreno, R.A. Posture and body image in individuals with major depressive disorder: A controlled study. Rev. Bras. Psiquiatr. 2010, 32, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Kumaresan, S.; Yoganandan, N.; Pintar, F.A.; Maiman, D.J.; Goel, V.K. Contribution of disc degeneration to osteophyte formation in the cervical spine: A biomechanical investigation. J. Orthop. Res. 2001, 19, 977–984. [Google Scholar] [CrossRef]
- Katon, W.; Schulberg, H. Epidemiology of depression in primary care. Gen. Hosp. Psychiatry 1992, 14, 237–247. [Google Scholar] [CrossRef]
- An, H.S.; Silveri, C.P.; Simpson, J.M.; File, P.; Simmons, C.; Simeone, F.A.; Balderston, R.A. Comparison of smoking habits between patients with surgically confirmed herniated lumbar and cervical disc disease and controls. J. Spinal Disord. 1994, 7, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.C.; Liu, L.; Huang, W.C.; Chen, Y.C.; Ko, C.C.; Wu, C.L.; Chen, T.J.; Cheng, H.; Su, T.P. The incidence of adjacent segment disease requiring surgery after anterior cervical diskectomy and fusion: Estimation using an 11-year comprehensive nationwide database in Taiwan. Neurosurgery 2012, 70, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, H.S.; Gilles, E.; DeVita, M.V.; Panagopoulos, G.; Michelis, M.F. Hyponatremia associated with large-bone fracture in elderly patients. Intern. Urol. Nephrol. 2009, 41, 733–737. [Google Scholar] [CrossRef] [PubMed]
- Flament, M.F.; Bissada, H.; Spettigue, W. Evidence-based pharmacotherapy of eating disorders. Int. J. Neuropsychopharmacol. 2012, 15, 189–207. [Google Scholar] [CrossRef] [PubMed]
- Häuser, W.; Wolfe, F.; Tölle, T.; Uçeyler, N.; Sommer, C. The role of antidepressants in the management of fibromyalgia syndrome: A systematic review and meta-analysis. CNS Drugs 2012, 26, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Birmes, P.; Coppin, D.; Schmitt, L.; Lauque, D. Serotonin syndrome: A brief review. Can. Med. Assos. J. 2003, 168, 1439–1442. [Google Scholar]

| Depression | |||
|---|---|---|---|
| No N = 34,166 | Yes N = 34,166 | Standard Mean Difference | |
| n (%) | n (%) | ||
| Gender | |||
| Women | 21,193 (62.0) | 20,921 (61.2) | 0.02 |
| Men | 12,973 (38.0) | 13,245 (38.8) | 0.02 |
| Age stratified | |||
| <50 | 19,771 (57.9) | 20,193 (59.1) | 0.03 |
| 50–64 | 7248 (21.2) | 7509 (22.0) | 0.003 |
| 65+ | 7147 (20.9) | 6464 (18.9) | 0.04 |
| Mean ± SD | 47.2 (18.1) | 47.3 (17.3) | 0.004 |
| Monthly income (NTD) † | |||
| <15,000 | 9633 (28.2) | 9633 (28.2) | 0.000 |
| 15,000–19,999 | 16,039 (46.9) | 16,117 (47.2) | 0.005 |
| ≥20,000 | 8494 (24.9) | 8416 (24.6) | 0.005 |
| Comorbidity | |||
| Diabetes | 3058 (8.95) | 3011 (8.81) | 0.005 |
| Hypertension | 11,106 (32.5) | 10,922 (32.0) | 0.012 |
| Hyperlipidemia | 7358 (21.5) | 72,445 (21.2) | 0.008 |
| coronary artery disease (CAD) | 6411 (18.8) | 6455 (18.9) | 0.003 |
| chronic obstructive pulmonary disease (COPD) | 4052 (11.9) | 4077 (11.9) | 0.002 |
| Asthma | 2758 (8.07) | 2778 (8.13) | 0.002 |
| Stroke | 1838 (5.38) | 1917 (5.61) | 0.01 |
| chronic kidney disease (CKD) | 582 (1.70) | 578 (1.69) | 0.001 |
| Cirrhosis | 8483 (24.8) | 8427 (24.7) | 0.004 |
| Head injury | 1633 (4.78) | 1717 (5.03) | 0.01 |
| Depression | ||||||||
|---|---|---|---|---|---|---|---|---|
| No | Yes | |||||||
| Event | PY | Rate # | Event | PY | Rate # | Crude HR (95% CI) | Adjusted HR & (95% CI) | |
| Sex | ||||||||
| Women | 786 | 135,745 | 5.79 | 1334 | 132,257 | 10.1 | 1.74 (1.59–1.90) *** | 1.78 (1.63–1.94) *** |
| Men | 365 | 78,813 | 4.63 | 671 | 79,655 | 8.42 | 1.82 (1.60–2.07) *** | 1.80 (1.59–2.05) *** |
| All | 1151 | 214,558 | 5.36 | 2005 | 211,911 | 9.46 | 1.76 (1.64–1.90) *** | 1.79 (1.66–1.92) *** |
| Stratify age | ||||||||
| <50 | 392 | 131,139 | 2.99 | 919 | 131,501 | 6.99 | 2.34 (2.08–2.63) *** | 2.21 (1.96–2.49) *** |
| 50–64 | 412 | 45,221 | 9.11 | 635 | 45,641 | 13.9 | 1.52 (1.35–1.73) *** | 1.55 (1.37–1.75) *** |
| 65+ | 347 | 38,198 | 9.08 | 451 | 34,769 | 13.0 | 1.43 (1.24–1.65) *** | 1.46 (1.27–1.68) *** |
| Monthly income (NTD) † | ||||||||
| <15,000 | 265 | 57,034 | 4.65 | 468 | 56,878 | 9.56 | 1.77 (1.52–2.06) *** | 1.74 (1.50–2.03) *** |
| 15,000–19,999 | 561 | 101,791 | 5.51 | 966 | 10,163 | 9.56 | 1.73 (1.56–1.92) *** | 1.81 (1.63–2.01) *** |
| ≥20,000 | 325 | 55,733 | 8.23 | 571 | 53,970 | 10.6 | 1.81 (1.58–2.08) *** | 1.75 (1.53–2.01) *** |
| Comorbidity ‡ | ||||||||
| No | 248 | 106,644 | 2.33 | 530 | 94,149 | 5.63 | 2.42 (2.08–2.82) *** | 2.41 (2.08–2.81) *** |
| Yes | 903 | 107,914 | 8.37 | 1475 | 117,762 | 12.5 | 1.50 (1.38–1.63) *** | 1.55 (1.43–1.68) *** |
| Variable Comorbidity | Event | PY | Rate # | Crude HR (95% CI) | Adjusted HR & (95% CI) |
|---|---|---|---|---|---|
| Diabetes | |||||
| No | 2822 | 394,866 | 7.15 | 1.00 | 1.00 |
| Yes | 334 | 31,604 | 10.6 | 1.45 (1.30–1.63) *** | 1.03 (0.91–1.16) |
| Hypertension | |||||
| No | 1740 | 299,595 | 5.81 | 1.00 | 1.00 |
| Yes | 1416 | 126,875 | 11.2 | 1.90 (1.78–2.04) *** | 1.05 (0.95–1.15) |
| Hyperlipidemia | |||||
| No | 2047 | 342,060 | 5.98 | 1.00 | 1.00 |
| Yes | 1109 | 84,410 | 13.1 | 2.18 (2.02–2.34) *** | 1.40 (1.28–1.52) |
| CAD | |||||
| No | 2136 | 353,013 | 6.05 | 1.00 | 1.00 |
| Yes | 1020 | 73,456 | 13.9 | 2.27 (2.11–2.45) *** | 1.46 (1.33–1.60) |
| COPD | |||||
| No | 2564 | 382,726 | 6.70 | 1.00 | 1.00 |
| Yes | 592 | 43,743 | 13.5 | 1.99 (1.82–2.18) *** | 1.32 (1.19–1.46) |
| Asthma | |||||
| No | 2794 | 397,139 | 7.04 | 1.00 | 1.00 |
| Yes | 362 | 29,331 | 12.3 | 1.72 (1.54–1.92) *** | 1.15 (1.02–1.29) |
| Stroke | |||||
| No | 3000 | 408,669 | 7.34 | 1.00 | 1.00 |
| Yes | 156 | 17,801 | 8.76 | 1.16 (0.99–1.36) | |
| CKD | |||||
| No | 3098 | 421,405 | 7.35 | 1.00 | 1.00 |
| Yes | 58 | 5065 | 11.5 | 1.50 (1.16–1.95) ** | 0.96 (0.74–1.25) |
| Cirrhosis | |||||
| No | 1992 | 323,741 | 6.15 | 1.00 | 1.00 |
| Yes | 1164 | 102,729 | 11.3 | 1.84 (1.71–1.97) *** | 1.40 (1.30–1.51) |
| Head injury | |||||
| No | 2988 | 408,421 | 7.32 | 1.00 | 1.00 |
| Yes | 168 | 18,049 | 9.31 | 1.25 (1.07–1.46) ** | 1.22 (1.05–1.43) |
| Variables | N | Event | PY | Rate # | Adjusted HR † (98.75% CI) | Adjusted HR † (98.3% CI) | Adjusted SHR & (98.75% CI) | Adjusted SHR & (98.3% CI) |
|---|---|---|---|---|---|---|---|---|
| Without depression group | 34,166 | 1151 | 214,558 | 5.36 | 1 (Reference) | 1 (Reference) | ||
| Depression Group Without medication | 2268 | 95 | 14,529 | 6.54 | 1.20 (0.98–1.48) | 1 (Reference) | 1.20 (0.97–1.48) | 1 (Reference) |
| With medication | ||||||||
| Non-SSRI | 7557 | 528 | 46,044 | 11.5 | 1.97 (1.78–2.19) * | 1.67 (1.34–2.07) ** | 1.96 (1.77–2.18) * | 1.66 (1.33–2.07) ** |
| SSRI | 24,341 | 1382 | 151,338 | 9.13 | 1.78 (1.65–1.93) * | 1.49 (1.21–1.83) ** | 1.77 (1.64–1.92) * | 1.48 (1.20–1.82) ** |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, S.-Y.; Sung, F.-C.; Lin, C.-L.; Chou, L.-W.; Hsu, C.-Y.; Kao, C.-H. Association of Depression and Cervical Spondylosis: A Nationwide Retrospective Propensity Score-Matched Cohort Study. J. Clin. Med. 2018, 7, 387. https://doi.org/10.3390/jcm7110387
Lin S-Y, Sung F-C, Lin C-L, Chou L-W, Hsu C-Y, Kao C-H. Association of Depression and Cervical Spondylosis: A Nationwide Retrospective Propensity Score-Matched Cohort Study. Journal of Clinical Medicine. 2018; 7(11):387. https://doi.org/10.3390/jcm7110387
Chicago/Turabian StyleLin, Shih-Yi, Fung-Chang Sung, Cheng-Li Lin, Li-Wei Chou, Chung-Y. Hsu, and Chia-Hung Kao. 2018. "Association of Depression and Cervical Spondylosis: A Nationwide Retrospective Propensity Score-Matched Cohort Study" Journal of Clinical Medicine 7, no. 11: 387. https://doi.org/10.3390/jcm7110387
APA StyleLin, S.-Y., Sung, F.-C., Lin, C.-L., Chou, L.-W., Hsu, C.-Y., & Kao, C.-H. (2018). Association of Depression and Cervical Spondylosis: A Nationwide Retrospective Propensity Score-Matched Cohort Study. Journal of Clinical Medicine, 7(11), 387. https://doi.org/10.3390/jcm7110387






