Maxillary Incisor Fragment Reattachment Protocols: Influence on Tooth Fracture Resistance and Strength of Bonding to Orthodontic Brackets
Abstract
1. Introduction
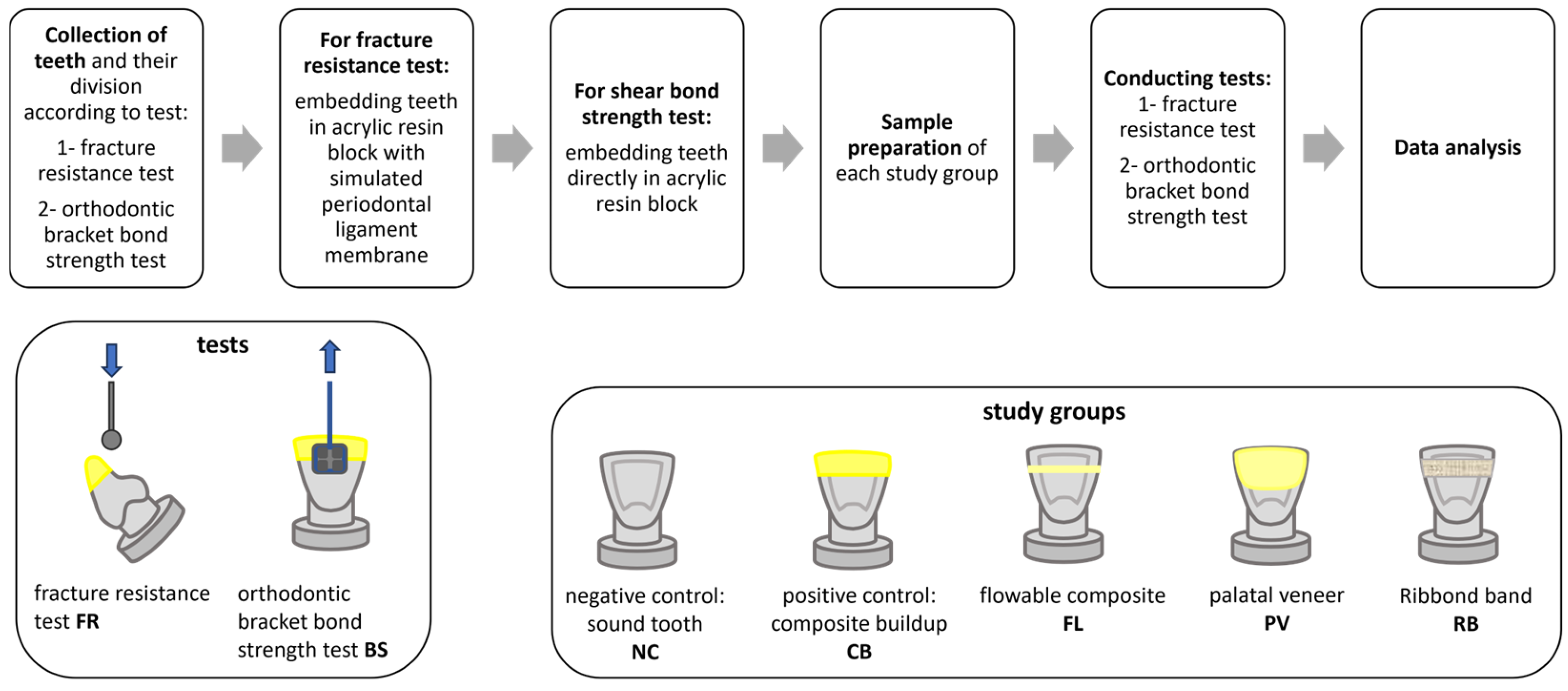
2. Materials and Methods
2.1. Collection of Teeth
2.2. Sample Size Calculation
2.3. Teeth Mounting
2.4. Study Groups
2.5. Induced Incisal Fracture
2.6. Reattachment and Restoration Protocols
2.6.1. Positive Control with Composite Buildup (CB)
2.6.2. Incisal Fragment Reattachment Using Flowable Composite (FL)
2.6.3. Incisal Fragment Reattachment Using a Palatal Composite Veneer (PV)
2.6.4. Incisal Fragment Reattachment Using a Ribbond Band (RB)
2.7. Fracture Resistance (FR) Test
2.8. Orthodontic Bracket Bond Strength (BS) Test
2.9. Failure Mode Analysis
2.10. Statistical Analysis
3. Results
3.1. Fracture Resistance and Orthodontic Bracket Bond Strength
3.2. Fracture Resistance Failure Mode
3.3. Bond Strength Failure Mode
4. Discussion
5. Conclusions
- 1-
- Among the incisal fragment reattachment protocols investigated, using Ribbond polyethylene fiber bands seems to provide the best performance in reattached tooth reinforcement and the best orthodontic bracket bond strength.
- 2-
- Using resin composite buildup to restore a fractured incisor appears to provide the best bonding quality for orthodontic brackets.
- 3-
- Tooth fracture resistance and orthodontic bracket bond strength seem to be inversely proportional to each other.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lise, D.P.; Vieira, L.C.; Araújo, É.; Lopes, G.C. Tooth fragment reattachment: The natural restoration. Oper. Dent. 2012, 37, 584–590. [Google Scholar] [CrossRef] [PubMed]
- Belcheva, A. Reattachment of fractured permanent incisors in schoolchildren (review). J. IMAB—Annu. Proceeding Sci. Pap. 2009, 14, 93–96. [Google Scholar] [CrossRef]
- Maitin, N.; Maitin, S.N.; Rastogi, K.; Bhushan, R. Fracture tooth fragment reattachment. BMJ Case Rep. 2013, 2013, bcr2013009183. [Google Scholar] [CrossRef] [PubMed]
- Vaz, V.T.; Presoto, C.D.; Jordão, K.C.; Paleari, A.G.; Dantas, A.A.; Segalla, J.C.; de Oliveira Junior, O.B. Fragment reattachment after atypical crown fracture in maxillary central incisor. Case Rep. Dent. 2014, 2014, 231603. [Google Scholar] [CrossRef]
- Olsburgh, S.; Jacoby, T.; Krejci, I. Crown fractures in the permanent dentition: Pulpal and restorative considerations. Dent. Traumatol. 2002, 18, 103–115. [Google Scholar] [CrossRef]
- Hecova, H.; Tzigkounakis, V.; Merglova, V.; Netolicky, J. A retrospective study of 889 injured permanent teeth. Dent. Traumatol. 2010, 26, 466–475. [Google Scholar] [CrossRef]
- Atabek, D.; Alaçam, A.; Aydintuğ, I.; Konakoğlu, G. A retrospective study of traumatic dental injuries. Dent. Traumatol. 2014, 30, 154–161. [Google Scholar] [CrossRef]
- Tonini, R. An Innovative Method for Fragment Reattachment after Complicated Crown Fracture. J. Esthet. Restor. Dent. 2017, 29, 172–177. [Google Scholar] [CrossRef]
- Macedo, G.V.; Diaz, P.I.; De, O.F.C.A.; Ritter, A.V. Reattachment of anterior teeth fragments: A conservative approach. J. Esthet. Restor. Dent. 2008, 20, 5–18, Discussion 19–20. [Google Scholar] [CrossRef]
- Dean, J.A.; Avery, D.R.; Swartz, M.L. Attachment of anterior tooth fragments. Pediatr. Dent. 1986, 8, 139–143. [Google Scholar]
- Jagannath-Torvi, S.; Kala, M. Restore the natural—A review and case series report on reattachment. J. Clin. Exp. Dent. 2014, 6, e595–e598. [Google Scholar] [CrossRef]
- Garcia, F.C.P.; Poubel, D.L.N.; Almeida, J.C.F.; Toledo, I.P.; Poi, W.R.; Guerra, E.N.S.; Rezende, L.V.M.L. Tooth fragment reattachment techniques-A systematic review. Dent. Traumatol. 2018, 34, 135–143. [Google Scholar] [CrossRef]
- Bruschi-Alonso, R.C.; Alonso, R.C.; Correr, G.M.; Alves, M.C.; Lewgoy, H.R.; Sinhoreti, M.A.; Puppin-Rontani, R.M.; Correr-Sobrinho, L. Reattachment of anterior fractured teeth: Effect of materials and techniques on impact strength. Dent. Traumatol. 2010, 26, 315–322. [Google Scholar] [CrossRef]
- Shirani, F.; Malekipour, M.R.; Sakhaei Manesh, V.; Aghaei, F. Hydration and dehydration periods of crown fragments prior to reattachment. Oper. Dent. 2012, 37, 501–508. [Google Scholar] [CrossRef]
- Sharmin, D.D.; Thomas, E. Evaluation of the effect of storage medium on fragment reattachment. Dent. Traumatol. 2013, 29, 99–102. [Google Scholar] [CrossRef]
- Ramesh, P.; Mathew, S.; Murthy, S.B.; George, J.V.; Hegde, S.; Premkumar, R. Efficacy of Ribbond and a fibre post on the fracture resistance of reattached maxillary central incisors with two fracture patterns: A comparative in vitro study. Dent. Traumatol. 2016, 32, 110–115. [Google Scholar] [CrossRef]
- Patel, K.; Mack, G.; Djemal, S. Management of acute traumatic dental injuries in the orthodontic patient. Br. Dent. J. 2022, 232, 695–700. [Google Scholar] [CrossRef]
- Thayer, M.L.T.; Ali, R. The dental demolition derby: Bruxism and its impact—Part 3: Repair and reconstruction. Br. Dent. J. 2022, 232, 775–782. [Google Scholar] [CrossRef]
- Hasanzade, M.; Ghodsi, S.; Yaghoobi, N. Rehabilitation of a deep bite patient with worn dentition using minimally invasive approach: A 3-year follow-up. Clin. Case Rep. 2021, 9, e05121. [Google Scholar] [CrossRef]
- Sandler, C.; Al-Musfir, T.; Barry, S.; Duggal, M.S.; Kindelan, S.; Kindelan, J.; Littlewood, S.; Nazzal, H. Guidelines for the orthodontic management of the traumatised tooth. J. Orthod. 2021, 48, 74–81. [Google Scholar] [CrossRef]
- Salama, F.; Abdelmegid, F.; Alhussain, M.; Muaddi, H.; AlMaflehi, N.; Alhowaish, L. Comparison of Fracture Resistance of Primary Incisors Restored with Different Intracanal-Reinforcement Materials. Clin. Cosmet. Investig. Dent. 2021, 13, 507–512. [Google Scholar] [CrossRef]
- Serdar, C.C.; Cihan, M.; Yücel, D.; Serdar, M.A. Sample size, power and effect size revisited: Simplified and practical approaches in pre-clinical, clinical and laboratory studies. Biochem. Med. 2021, 31, 010502. [Google Scholar] [CrossRef]
- Naik, S.; Murry, J.N.; Sharma, S.; Vashisth, P.; Abbey, P.; Singh, V. Comparative Evaluation of the Effect of Various Storage Media on the Fracture Resistance of the Reattached Tooth Fragment: An Observational Study. Int. J. Clin. Pediatr. Dent. 2024, 17, 665–672. [Google Scholar] [CrossRef]
- Abo El-Ela, O.A.; Atta, O.A.; El-Mowafy, O. Fracture resistance of anterior teeth restored with a novel nonmetallic post. J. Can. Dent. Assoc. 2008, 74, 441. [Google Scholar]
- Hegde, R.J.; Kale, S.J. Comparison of the Effect of Various Storage Media on the Fracture Resistance of the Reattached Incisor Tooth Fragments: An In Vitro Study. Indian J. Dent. Sci. 2017, 9, 233–236. [Google Scholar]
- Soares, C.J.; Pizi, E.C.; Fonseca, R.B.; Martins, L.R. Influence of root embedment material and periodontal ligament simulation on fracture resistance tests. Braz. Oral Res. 2005, 19, 11–16. [Google Scholar] [CrossRef]
- de Sousa, A.P.B.R.; França, K.; de Lucas Rezende, L.V.M.; do Nascimento Poubel, D.L.; Almeida, J.C.F.; de Toledo, I.P.; Garcia, F.C.P. In vitro tooth reattachment techniques: A systematic review. Dent. Traumatol. 2018, 34, 297–310. [Google Scholar] [CrossRef]
- Madhubala, A.; Tewari, N.; Mathur, V.P.; Bansal, K. Comparative evaluation of fracture resistance using two rehydration protocols for fragment reattachment in uncomplicated crown fractures. Dent. Traumatol. 2019, 35, 199–203. [Google Scholar] [CrossRef]
- 3M-ESPE Adper Single Bond 2 Adhesive Technical Profile. Available online: https://www.eudent.sk/obchod_homedir/data/3129/prilohy/bro-sb-2-tp.pdf (accessed on 27 April 2025).
- Barkmeier, W.W.; Erickson, R.L.; Kimmes, N.S.; Latta, M.A.; Wilwerding, T.M. Effect of enamel etching time on roughness and bond strength. Oper. Dent. 2009, 34, 217–222. [Google Scholar] [CrossRef]
- Bortoluzzi, E.A.; Souza, E.M.; Reis, J.M.; Esberard, R.M.; Tanomaru-Filho, M. Fracture strength of bovine incisors after intra-radicular treatment with MTA in an experimental immature tooth model. Int. Endod. J. 2007, 40, 684–691. [Google Scholar] [CrossRef]
- Qing, H.; Zhu, Z.; Chao, Y.; Zhang, W. In vitro evaluation of the fracture resistance of anterior endodontically treated teeth restored with glass fiber and zircon posts. J. Prosthet. Dent. 2007, 97, 93–98. [Google Scholar] [CrossRef]
- Abu Haimed, T.; Osama Filfilan, R.; Nazih Hassoubah, M.; Abou Neel, E.A.; Bamashmous, M. Cyclic shear fatigue of orthodontic brackets bonded to enamel using self-adhering flowable composites. Saudi Dent. J. 2023, 35, 834–840. [Google Scholar] [CrossRef]
- Shamohammadi Heidari, M.; Moradinejad, M.; Tabatabaei, H.; Rakhshan, V. Effects of Three Novel Bracket Luting Agents Containing Zirconia Primer on Shear Bond Strength of Metal Orthodontic Brackets Attached to Monolithic Zirconia Crowns: A Preliminary In Vitro Study. Int. J. Dent. 2022, 2022, 7107526. [Google Scholar] [CrossRef]
- Liddelow, G.; Carmichael, G. The restoration of traumatized teeth. Aust. Dent. J. 2016, 61 (Suppl. S1), 107–119. [Google Scholar] [CrossRef]
- Ghoreishizadeh, A.; Mohammadi, F.; Rezayi, Y.; Ghavimi, M.; Pourlak, T. Comparison of shear bond strengths with different bevel preparations for the reattachment of fractured fragments of maxillary central incisors. Dent. Traumatol. 2020, 36, 648–653. [Google Scholar] [CrossRef]
- Machado, V.; Alves, R.; Lopes, L.; Botelho, J.; Mendes, J.J. Tooth Reattachment and Palatal Veneer on a Multidisciplinary Approach of Crown Fractures in Upper Central Incisors. Case Rep. Dent. 2017, 2017, 4702635. [Google Scholar] [CrossRef]
- Fennis, W.M.; Kreulen, C.M.; Wolke, J.G.; Fokkinga, W.A.; Machado, C.; Creugers, N.H. Fracture resistance of reattached incisor fragments with mini fibre-reinforced composite anchors. J. Dent. 2009, 37, 462–467. [Google Scholar] [CrossRef]
- Li, Y.; Jacox, L.A.; Little, S.H.; Ko, C.C. Orthodontic tooth movement: The biology and clinical implications. Kaohsiung J. Med. Sci. 2018, 34, 207–214. [Google Scholar] [CrossRef]
- Henkin, F.S.; Macêdo, É.; Santos, K.D.; Schwarzbach, M.; Samuel, S.M.; Mundstock, K.S. In vitro analysis of shear bond strength and adhesive remnant index of different metal brackets. Dent. Press. J. Orthod. 2016, 21, 67–73. [Google Scholar] [CrossRef]
- Pereira, R.V.; Tabata, L.F.; Rosemberg, E.T.; Ribeiro, A.P.D.; Poubel, D.L.D.N.; Garcia, F.C.P. Fragment reattachment or direct restoration? An in vitro study. Dent. Traumatol. 2023, 39, 257–263. [Google Scholar] [CrossRef]
- Nagi, S.M.; Khadr, S.M. Influence of different tooth preparation and bonding techniques on the fracture resistance of tooth fragment reattachment. Biomater. Investig. Dent. 2021, 8, 112–118. [Google Scholar] [CrossRef]
- Metwaly, A.A.; Elzoghby, A.F.; Abd ElAziz, R.H. Clinical performance of polyethylenefiber reinforced resin composite restorations in endodontically treated teeth: A randomized controlled clinical trial. BMC Oral Health 2024, 24, 1285. [Google Scholar] [CrossRef]
- Agrawal, V.S.; Shah, A.; Kapoor, S. Effect of fiber orientation and placement on fracture resistance of large class II mesio-occluso-distal cavities in maxillary premolars: An in vitro study. J. Conserv. Dent. Endod. 2022, 25, 122–127. [Google Scholar] [CrossRef]
- Mangoush, E.; Säilynoja, E.; Prinssi, R.; Lassila, L.; Vallittu, P.K.; Garoushi, S. Comparative evaluation between glass and polyethylene fiber reinforced composites: A review of the current literature. J. Clin. Exp. Dent. 2017, 9, e1408–e1417. [Google Scholar] [CrossRef]
- Albar, N.H.M.; Khayat, W.F. Evaluation of Fracture Strength of Fiber-Reinforced Direct Composite Resin Restorations: An In Vitro Study. Polymers 2022, 14, 4339. [Google Scholar] [CrossRef]
- Hiremath, H.; Kulkarni, S.; Saikalyan, S.; Chordhiya, R. Use of ribbond and panavia F cement in reattaching fractured tooth fragments of vital maxillary anterior teeth. Contemp. Clin. Dent. 2012, 3, 478–480. [Google Scholar] [CrossRef]
- Albar, N.H.M. Evaluation of Fracture Resistance of Reattached Tooth Fragments Restored Using Fiber-reinforced Composites: A Systematic Review. J. Contemp. Dent. Pr. 2024, 25, 605–615. [Google Scholar] [CrossRef]
- Sreen, D.; Abraham, D.; Gupta, A.; Singh, A.; Aggarwal, V.; Chauhan, N.; Jala, S.; Mehta, N. Comparative evaluation of the force required to fracture coronal segments reattached using different methods. Dent. Traumatol. 2022, 38, 143–148. [Google Scholar] [CrossRef]
- Saeed, U.; Al-Turaif, H.; Siddiqui, M.E. Stress relaxation performance of glass fiber-reinforced high-density polyethylene composite. Polym. Polym. Compos. 2021, 29, 705–713. [Google Scholar] [CrossRef]
- Goh, K.; Aspden, R.M.; Hukins, D.W.L. finite element analysis of stress transfer in short-fibre composite materials. Compos. Sci. Technol. 2004, 64, 1091–1100. [Google Scholar] [CrossRef]
- Jadhav, G.R.; Mittal, P.; Shinde, S.; Al-Qarni, M.A.; Al-Obaid, M.; Abullais, S.S.; Cicciù, M.; Minervini, G. Biomimetic approach to strengthen the incisal fracture composite build-up: An in vitro study. BMC Oral Health 2024, 24, 42. [Google Scholar] [CrossRef]
- Zhang, L.; Ye, N.; Aregawi, W.A.; Fok, A. Effect of chamfer design on load capacity of reattached incisors. Dent. Mater. 2021, 37, 1168–1175. [Google Scholar] [CrossRef]
- Zhou, X.; Huang, X.; Li, M.; Peng, X.; Wang, S.; Zhou, X.; Cheng, L. Development and status of resin composite as dental restorative materials. J. Appl. Polym. Sci. 2019, 136, 48180. [Google Scholar] [CrossRef]
- Kaur, G.; Shetty, C.; Saji, S.A.; Bajpe, S.; Prabha, C.; Shroff, R. Tooth fragment reattachment using cyanoacrylate tissue adhesive and flowable composite: An in vitro study. Endodontology 2024, 36, 339–345. [Google Scholar] [CrossRef]
- Yikilgan, İ.; Guven, N.; Kedıcı Alp, C.; Tokar, E.; Topuz, O.; Kamak, H. Efficacy of Palatal Applications on Fracture Resistance of Reattached Maxillary Central Incisors: An In Vitro Study. Appl. Bionics Biomech. 2017, 2017, 9124545. [Google Scholar] [CrossRef]
- Ribeiro, A.A.; de Morais, A.V.; Brunetto, D.P.; Ruellas, A.C.; de Araujo, M.T. Comparison of shear bond strength of orthodontics brackets on composite resin restorations with different surface treatments. Dent. Press. J. Orthod. 2013, 18, 98–103. [Google Scholar] [CrossRef]
- Bayram, M.; Yesilyurt, C.; Kusgöz, A.; Ulker, M.; Nur, M. Shear bond strength of orthodontic brackets to aged resin composite surfaces: Effect of surface conditioning. Eur. J. Orthod. 2011, 33, 174–179. [Google Scholar] [CrossRef]
- Smyth, R.S.; Hunt, N.P.; Sharif, M.O. An Overview of Orthodontic Bonding. Orthod. Update 2020, 13, 130–133. [Google Scholar] [CrossRef]
- Jiang, W.; Bo, H.; Yongchun, G.; LongXing, N. Stress distribution in molars restored with inlays or onlays with or without endodontic treatment: A three-dimensional finite element analysis. J. Prosthet. Dent. 2010, 103, 6–12. [Google Scholar] [CrossRef]
- Kaur, A.; Gupta, S.; Tewari, N.; Chanda, A. A computational model to assess the effectiveness of adhesive materials in restoration of crown-root fractures. Biomed. Technol. 2024, 6, 1–8. [Google Scholar] [CrossRef]
- Elsaka, S.E.; Hammad, S.M.; Ibrahim, N.F. Evaluation of stresses developed in different bracket-cement-enamel systems using finite element analysis with in vitro bond strength tests. Prog. Orthod. 2014, 15, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hearn, E.J. Experimental stress analysis. In Mechanics of Materials, 3rd ed.; Butterworth-Heinemann, Elsevier Ltd.: Oxford, UK, 1997; pp. 430–456. [Google Scholar]
- Biau, D.J.; Kernéis, S.; Porcher, R. Statistics in brief: The importance of sample size in the planning and interpretation of medical research. Clin. Orthop. Relat. Res. 2008, 466, 2282–2288. [Google Scholar] [CrossRef] [PubMed]
- Selvaraj, M.; Mohaideen, K.; Sennimalai, K.; Gothankar, G.S.; Arora, G. Effect of oral environment on contemporary orthodontic materials and its clinical implications. J. Orthod. Sci. 2023, 12, 1. [Google Scholar] [CrossRef] [PubMed]
- Abou Neel, E.A.; Knowles, J.C.; Bozec, L. Effect of sodium hypochlorite on adhesive charactersitics of dentin: A systematic review of laboratory-based testing. Int. J. Adhes. Adhes. 2019, 95, 102419. [Google Scholar] [CrossRef]
| Material | Composition | Manufacturer | Lot No. |
|---|---|---|---|
| 3M Scotchbond universal etchant, etching gel | 35% orthophosphoric acid | 3M, Deutschland GmbH, Neuss, Germany | 9513767 |
| 3M Adper Single Bond 2 Adhesive, single-bond adhesive | BisGMA, HEMA, dimethacrylates, ethanol, water, a novel photoinitiator system, and a methacrylate functional copolymer of polyacrylic and polyitaconic acids | 3M ESPE, St. Paul, MN, USA | NF18673 |
| Filtek Z250 Universal Restorative, nanohybrid composite resin | Bis-GMA (Bisphenol A diglycidyl ether dimethacrylate) and a blend of UDMA (urethane dimethacrylate) and Bis-EMA(Bisphenol A polyethylene glycol diether dimethacrylate) | 3M ESPE, St. Paul, MN, USA | NF15836 |
| Filtek Supreme flowable composite, flowable composite | Procrylat, BisGMA, and TEGDMA resins. The fillers were a combination of a non-agglomerated/non-aggregated surface-modified 20 nm silica filler, a non-agglomerated/non-aggregated surface-modified 75 nm silica filler, an aggregated surface-modified zirconia/silica cluster filler (comprising 20 nm silica and 4 to 11 nm zirconia particles), and an ytterbium trifluoride filler with particle sizes ranging from 0.1 to 5.0 μm. The aggregate had an average cluster particle size of 0.6 to 10 μm. The total inorganic filler loading was approximately 65% by weight (46% by volume). | 3M ESPE, St. Paul, MN, USA | NF20803 10/2024 |
| Ribbond THM, reinforcement ribbon | Ultra-High-Molecular-Weight Polyethylene-Polyethylene, Homopolymer H-(CH2-CH2)n-H | Ribbond, Inc., Seattle, WA, USA | 00236334430 |
| PINNACLE™, stainless steel orthodontic brackets | Stainless steel | Ortho Technology Inc, West Columbia, SC, USA | 1026793 |
| Orthodontic bracket adhesive and primer system: I-Transbond™ PLUS Colour Change Adhesive II-Transbond™ XT Light Cure Adhesive Primer | I-Bisphenol A Diglycidyl Ether Dimethacrylate (BisGMA), Triethylene Glycol, Dimethacrylate (TEGDMA), Silane-treated quartz, photoinitiators for light curing, and color-changing agents to assist in positioning and excess clean-up | 3M Unitek, Monrovia, CA, USA | NF20792 |
| II-Bisphenol A Diglycidyl Ether Dimethacrylate (BisGMA): 45–55%; Triethylene Glycol Dimethacrylate (TEGDMA): 45–55%; -4-(Dimethylamino)-Benzeneethanol: <0.5% | 9178214 |
| Group | Fracture Resistance Mean (N) ± SD | Significant Differences * | Shear Bond Strength Mean (MPa) ± SD | Significant Differences * |
|---|---|---|---|---|
| Negative control (sound tooth) (NC) | 514.4 ± 19.4 | A | 17.6 ± 0.6 | A |
| Composite buildup (CB) | 224.9 ± 23.8 | C | 16.6 ± 0.5 | B |
| Flowable composite (FL) | 203.7 ± 7.8 | D | 13.4 ± 0.8 | D |
| Palatal veneer (PV) | 234.6 ± 6.6 | C | 6.5 ± 0.9 | E |
| Ribbond band (RB) | 324.6 ± 20.9 | B | 15.2 ± 0.7 | C |
| Group | Cohesive Failure (%) | Adhesive Failure (%) | Mixed Failure (%) | Substrate (%) |
|---|---|---|---|---|
| CB | 25 | 12.5 | 37.5 | 25 |
| FL | 25 | 25 | 50 | 0 |
| PV | 12.5 | 62.5 | 12.5 | 12.5 |
| RB | 0 | 25 | 37.5 | 37.5 |
| Group | Cohesive Failure (%) | Adhesive Failure (%) | Mixed Failure (%) |
|---|---|---|---|
| NC | 0 | 25 | 75 |
| CB | 0 | 25 | 75 |
| FL | 0 | 62.5 | 37.5 |
| PV | 0 | 62.5 | 37.5 |
| RB | 0 | 50 | 50 |
| Groups | Bracket Debonding with Incisal Fragment | Bracket Debonding Without Incisal Fragment |
|---|---|---|
| Composite buildup (CB) | 0 | 8 |
| Flowable composite (FL) | 6 | 2 |
| Palatal veneer (PV) | 4 | 4 |
| Ribbond band (RB) | 1 | 7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elgezawi, M.; Haridy, R.; Almulhim, K.S.; Abdalla, M.A.; Alsulaiman, A.A.; Al Dehailan, L.; Alsheikh, R.; Alotaibi, S.; Alghamdi, D.; Almutairi, O.; et al. Maxillary Incisor Fragment Reattachment Protocols: Influence on Tooth Fracture Resistance and Strength of Bonding to Orthodontic Brackets. J. Clin. Med. 2025, 14, 3220. https://doi.org/10.3390/jcm14093220
Elgezawi M, Haridy R, Almulhim KS, Abdalla MA, Alsulaiman AA, Al Dehailan L, Alsheikh R, Alotaibi S, Alghamdi D, Almutairi O, et al. Maxillary Incisor Fragment Reattachment Protocols: Influence on Tooth Fracture Resistance and Strength of Bonding to Orthodontic Brackets. Journal of Clinical Medicine. 2025; 14(9):3220. https://doi.org/10.3390/jcm14093220
Chicago/Turabian StyleElgezawi, Moataz, Rasha Haridy, Khalid S. Almulhim, Moamen A. Abdalla, Ahmed A. Alsulaiman, Laila Al Dehailan, Rasha Alsheikh, Shahad Alotaibi, Deena Alghamdi, Ohud Almutairi, and et al. 2025. "Maxillary Incisor Fragment Reattachment Protocols: Influence on Tooth Fracture Resistance and Strength of Bonding to Orthodontic Brackets" Journal of Clinical Medicine 14, no. 9: 3220. https://doi.org/10.3390/jcm14093220
APA StyleElgezawi, M., Haridy, R., Almulhim, K. S., Abdalla, M. A., Alsulaiman, A. A., Al Dehailan, L., Alsheikh, R., Alotaibi, S., Alghamdi, D., Almutairi, O., Alwehaibi, S. F., Kamal, A., & Kaisarly, D. (2025). Maxillary Incisor Fragment Reattachment Protocols: Influence on Tooth Fracture Resistance and Strength of Bonding to Orthodontic Brackets. Journal of Clinical Medicine, 14(9), 3220. https://doi.org/10.3390/jcm14093220









