Comparison of Visual Performance Between Two Diffractive Trifocal Intraocular Lenses
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Surgical Procedure and Intraocular Lenses
2.3. Preoperative and Postoperative Measurements
2.4. Statistical Analysis
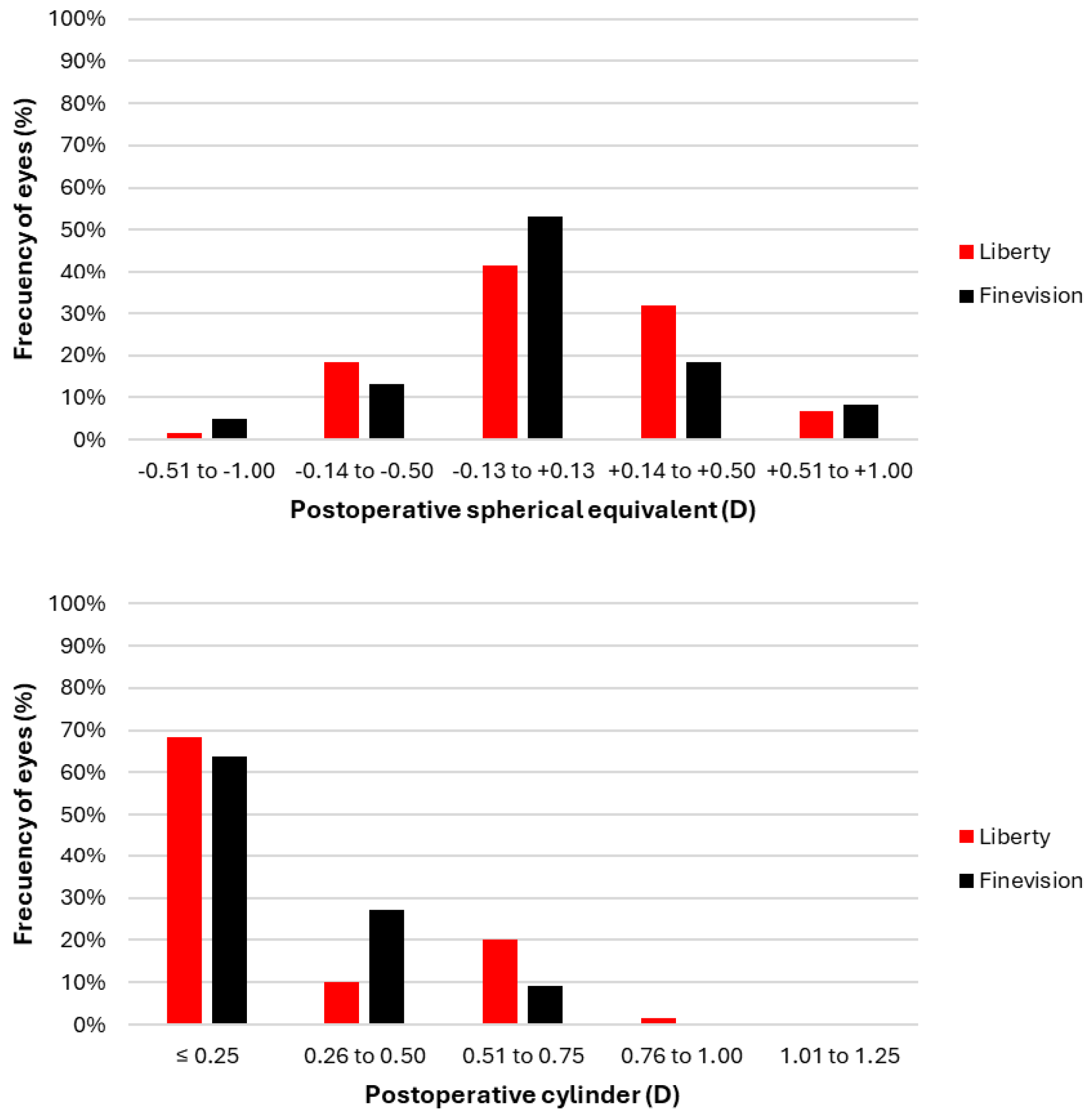
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schnider, C.; Yuen, L.; Rampat, R.; Zhu, D.; Dhallu, S.; Trinh, T.; Gurnani, B.; Abdelmaksoud, A.; Bhogal-Bhamra, G.; Wolffsohn, J.S.; et al. BCLA CLEAR presbyopia: Management with intraocular lenses. Cont. Lens Anterior Eye 2024, 47, 102253. [Google Scholar] [CrossRef] [PubMed]
- de Silva, S.R.; Evans, J.R.; Kirthi, V.; Ziaei, M.; Leyland, M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst. Rev. 2016, 12, Cd003169. [Google Scholar] [CrossRef] [PubMed]
- Mencucci, R.; Morelli, A.; Cennamo, M.; Roszkowska, A.M.; Favuzza, E. Enhanced Monofocal Intraocular Lenses: A Retrospective, Comparative Study between Three Different Models. J. Clin. Med. 2023, 12, 3588. [Google Scholar] [CrossRef] [PubMed]
- Davison, J.A.; Simpson, M.J. History and development of the apodized diffractive intraocular lens. J. Cataract. Refract. Surg. 2006, 32, 849–858. [Google Scholar] [CrossRef] [PubMed]
- Alio, J.L.; Plaza-Puche, A.B.; Férnandez-Buenaga, R.; Pikkel, J.; Maldonado, M. Multifocal intraocular lenses: An overview. Surv. Ophthalmol. 2017, 62, 611–634. [Google Scholar] [CrossRef] [PubMed]
- EuroTimes. ESCRS Clinical Trends Survey 2023 Results; EuroTimes: London, UK, 2024. [Google Scholar]
- Rampat, R.; Gatinel, D. Multifocal and Extended Depth-of-Focus Intraocular Lenses in 2020. Ophthalmology 2021, 128, e164–e185. [Google Scholar] [CrossRef] [PubMed]
- Karam, M.; Alkhowaiter, N.; Alkhabbaz, A.; Aldubaikhi, A.; Alsaif, A.; Shareef, E.; Alazaz, R.; Alotaibi, A.; Koaik, M.; Jabbour, S. Extended Depth of Focus Versus Trifocal for Intraocular Lens Implantation: An Updated Systematic Review and Meta-Analysis. Am. J. Ophthalmol. 2023, 251, 52–70. [Google Scholar] [CrossRef] [PubMed]
- Law, E.M.; Aggarwal, R.K.; Kasaby, H. Clinical outcomes with a new trifocal intraocular lens. Eur. J. Ophthalmol. 2014, 24, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Mojzis, P.; Peña-García, P.; Liehneova, I.; Ziak, P.; Alió, J.L. Outcomes of a new diffractive trifocal intraocular lens. J. Cataract. Refract. Surg. 2014, 40, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Fernández, J.; Rodríguez-Vallejo, M.; Martínez, J.; Tauste, A.; Piñero, D.P. Standard Clinical Outcomes With a New Low Addition Trifocal Intraocular Lens. J. Refract. Surg. 2019, 35, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Zamora-de La Cruz, D.; Bartlett, J.; Gutierrez, M.; Ng, S.M. Trifocal intraocular lenses versus bifocal intraocular lenses after cataract extraction among participants with presbyopia. Cochrane Database Syst. Rev. 2023, 1, Cd012648. [Google Scholar] [CrossRef] [PubMed]
- García-Bella, J.; Ventura-Abreu, N.; Morales-Fernández, L.; Talavero-González, P.; Carballo-Álvarez, J.; Sanz-Fernández, J.C.; Vázquez-Moliní, J.M.; Martínez-de-la-Casa, J.M. Visual outcomes after progressive apodized diffractive intraocular lens implantation. Eur. J. Ophthalmol. 2018, 28, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Cochener, B.; Vryghem, J.; Rozot, P.; Lesieur, G.; Chevalier, J.P.; Henry, J.M.; David, T.; Lesueur, L.; Gatinel, D.; Ganem, C.; et al. Clinical outcomes with a trifocal intraocular lens: A multicenter study. J. Refract. Surg. 2014, 30, 762–768. [Google Scholar] [CrossRef] [PubMed]
- Carballo-Alvarez, J.; Vazquez-Molini, J.M.; Sanz-Fernandez, J.C.; Garcia-Bella, J.; Polo, V.; García-Feijoo, J.; Martinez-de-la-Casa, J.M. Visual outcomes after bilateral trifocal diffractive intraocular lens implantation. BMC Ophthalmol. 2015, 15, 26. [Google Scholar] [CrossRef] [PubMed]
- Ang, R.E.T. Long Term Clinical Outcomes of Hydrophilic and Hydrophobic Versions of a Trifocal IOL with the Same Optical Design. Clin. Ophthalmol. 2023, 17, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Kniestedt, C.; Stamper, R.L. Visual acuity and its measurement. Ophthalmol. Clin. N. Am. 2003, 16, 155–170. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Vallejo, M.; Burguera, N.; Rocha-de-Lossada, C.; Aramberri, J.; Fernández, J. Refraction and defocus curves in eyes with monofocal and multifocal intraocular lenses. J. Optom. 2023, 16, 236–243. [Google Scholar] [CrossRef] [PubMed]
- Carpena-Torres, C.; Batres, L.; Serramito, M.; Carracedo, G. Repeatability of Subjective Refraction in Different Age Groups. Photonics 2024, 11, 634. [Google Scholar] [CrossRef]
- Baker, D.H.; Lygo, F.A.; Meese, T.S.; Georgeson, M.A. Binocular summation revisited: Beyond √2. Psychol. Bull. 2018, 144, 1186–1199. [Google Scholar] [CrossRef] [PubMed]
- Fernández, J.; Ribeiro, F.; Rocha-de-Lossada, C.; Rodríguez-Vallejo, M. Functional Classification of Intraocular Lenses Based on Defocus Curves: A Scoping Review and Cluster Analysis. J. Refract. Surg. 2024, 40, e108–e116. [Google Scholar] [CrossRef] [PubMed]

| Parameter | Liberty | Finevision |
|---|---|---|
| Technical name | Bi-Flex Liberty 677MY | FineVision POD F |
| Manufacturer | Medicontur (Zsámbék, Hungary) | BVI Medical (Waltham, MA, USA) |
| Material | 25% Hydrophilic | 26% Hydrophilic |
| Overall diameter (mm) | 13.00 | 11.40 |
| Optic diameter (mm) | 6.00 | 6.00 |
| Diffractive diameter (mm) | 3.00 | Unspecified |
| Optic design | Biconvex aspheric trifocal | Biconvex aspheric trifocal |
| Haptic design | Posterior vaulting fenestrated C-loop (0° angulation) | 4-closed C-loops and posterior angulated haptic |
| Refractive index | 1.46 | 1.46 |
| Abbe number | 58 | 58 |
| A constant (SRK/T) | 118.9 | 118.8 |
| Addition (IOL plane) | +1.75 D, +3.50 D | +1.75 D, +3.50 D |
| Filtration | UV, blue light | UV, blue light |
| Variable | Liberty | Finevision | p-Value |
|---|---|---|---|
| Participants (n) | 31 | 31 | - |
| Eyes analyzed (n) | 62 | 62 | - |
| Gender (male, %) | 29.0% | 32.3% | 0.68 |
| Age (years) | 61.1 ± 6.4 | 61.9 ± 6.8 | 0.47 |
| Sphere (D) | 0.65 ± 1.93 | 0.81 ± 2.13 | 0.41 |
| Cylinder (D) | −0.81 ± 1.01 | −0.60 ± 0.59 | 0.66 |
| Variable | Lens | Baseline | 1 Month | 3 Months |
|---|---|---|---|---|
| UDVA (logMAR) | Liberty | 0.56 ± 0.06 | 0.08 ± 0.07 | 0.09 ± 0.08 |
| Finevision | 0.53 ± 0.09 | 0.08 ± 0.09 | 0.10 ± 0.10 | |
| p-Value | 0.60 | 0.49 | 0.98 | |
| CDVA (logMAR) | Liberty | 0.05 ± 0.08 | 0.01 ± 0.03 | 0.02 ± 0.04 |
| Finevision | 0.07 ± 0.11 | 0.03 ± 0.07 | 0.02 ± 0.06 | |
| p-Value | 0.22 | 0.43 | 0.94 | |
| UNVA (logMAR) | Liberty | - | 0.03 ± 0.05 | 0.01 ± 0.02 |
| Finevision | - | 0.01 ± 0.05 | 0.02 ± 0.06 | |
| p-Value | - | < 0.01 * | 0.21 | |
| CNVA (logMAR) | Liberty | - | 0.00 ± 0.02 | 0.00 ± 0.02 |
| Finevision | - | 0.01 ± 0.05 | 0.02 ± 0.06 | |
| p-Value | - | 0.73 | 0.08 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Segura-Duch, G.; Oliver-Gutierrez, D.; Arans, M.; Duch-Tuesta, S.; Carpena-Torres, C.; Carracedo, G.; Andreu-Andreu, D. Comparison of Visual Performance Between Two Diffractive Trifocal Intraocular Lenses. J. Clin. Med. 2025, 14, 3128. https://doi.org/10.3390/jcm14093128
Segura-Duch G, Oliver-Gutierrez D, Arans M, Duch-Tuesta S, Carpena-Torres C, Carracedo G, Andreu-Andreu D. Comparison of Visual Performance Between Two Diffractive Trifocal Intraocular Lenses. Journal of Clinical Medicine. 2025; 14(9):3128. https://doi.org/10.3390/jcm14093128
Chicago/Turabian StyleSegura-Duch, Gloria, David Oliver-Gutierrez, Mar Arans, Susana Duch-Tuesta, Carlos Carpena-Torres, Gonzalo Carracedo, and David Andreu-Andreu. 2025. "Comparison of Visual Performance Between Two Diffractive Trifocal Intraocular Lenses" Journal of Clinical Medicine 14, no. 9: 3128. https://doi.org/10.3390/jcm14093128
APA StyleSegura-Duch, G., Oliver-Gutierrez, D., Arans, M., Duch-Tuesta, S., Carpena-Torres, C., Carracedo, G., & Andreu-Andreu, D. (2025). Comparison of Visual Performance Between Two Diffractive Trifocal Intraocular Lenses. Journal of Clinical Medicine, 14(9), 3128. https://doi.org/10.3390/jcm14093128






