Comparison of Outcomes Among Neurovascular Patients Managed in Dedicated Neurological Intensive Care Units vs. General Intensive Care Units
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Title and Abstract Screening
2.4. Full Text Review
2.5. Data Extraction
2.6. Qualitative Assessment
2.7. Ethical Considerations
3. Results
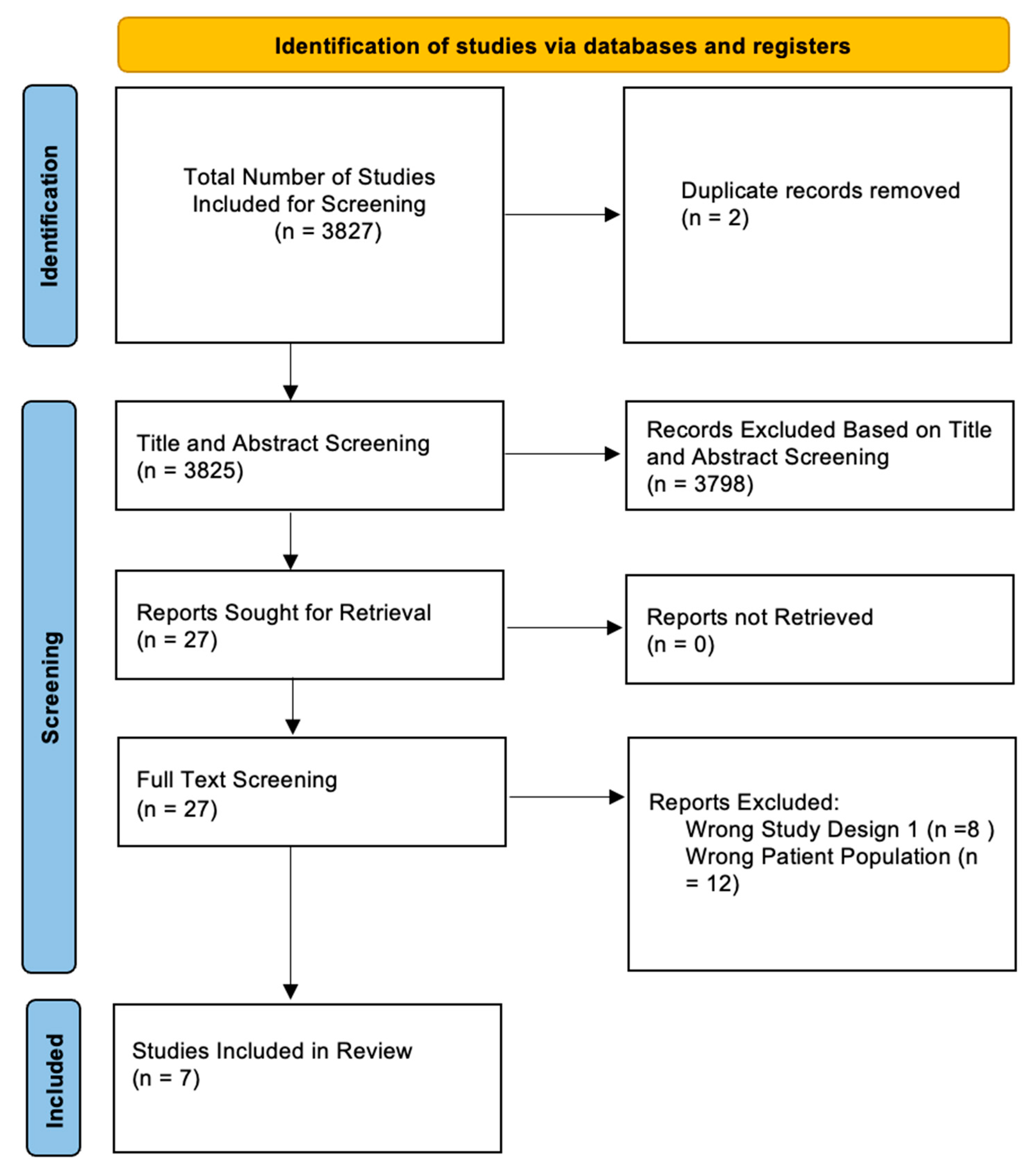
3.1. Article Search Results
3.2. Intracerebral Hemorrhage
3.3. Acute Ischemic Stroke
3.4. Subarachnoid Hemorrhage
3.5. Intracerebral Hemorrhage and Acute Ischemic Stroke
3.6. Risk of Bias Assessment
4. Discussion
4.1. Key Results
4.2. Research Background
4.3. Review of the Literature
4.4. Future Research Directions
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AIS | acute ischemic stroke |
| ICH | intracerebral hemorrhage |
| ICU | intensive care unit |
References
- Hilkens, N.A.; Casolla, B.; Leung, T.W.; de Leeuw, F.-E. Stroke. Lancet 2024, 403, 2820–2836. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.F.; Wu, J.S.; Mao, Y.; Chen, X.C.; Zhou, L.F.; Zhang, Y. The optimal time-window for surgical treatment of spontaneous intracerebral hemorrhage: Result of prospective randomized controlled trial of 500 cases. Acta Neurochir. Suppl. 2008, 105, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Hostettler, I.C.; Lange, N.; Schwendinger, N.; Frangoulis, S.; Hirle, T.; Trost, D.; Gempt, J.; Kreiser, K.; Wostrack, M.; Meyer, B. Duration between aneurysm rupture and treatment and its association with outcome in aneurysmal subarachnoid haemorrhage. Sci. Rep. 2023, 13, 1527. [Google Scholar] [CrossRef]
- Bershad, E.M.; Feen, E.S.; Hernandez, O.H.; Suri, M.F.K.; Suarez, J.I. Impact of a specialized neurointensive care team on outcomes of critically ill acute ischemic stroke patients. Neurocrit. Care 2008, 9, 287–292. [Google Scholar] [CrossRef]
- Shen, Y.; Chao, B.-H.; Cao, L.; Tu, W.-J.; Wang, L.-D. Stroke Center Care and Outcome: Results from the CSPPC Stroke Program. Transl. Stroke Res. 2020, 11, 377–386. [Google Scholar] [CrossRef] [PubMed]
- Feigin, V.L.; Nichols, E.; Alam, T.; Bannick, M.S.; Beghi, E.; Blake, N.; Culpepper, W.J.; Dorsey, E.R.; Elbaz, A.; Ellenbogen, R.G.; et al. Global, regional, and national burden of neurological disorders, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 459–480. [Google Scholar] [CrossRef]
- Kalkonde, Y.V.; Alladi, S.; Kaul, S.; Hachinski, V. Stroke Prevention Strategies in the Developing World. Stroke 2018, 49, 3092–3097. [Google Scholar] [CrossRef] [PubMed]
- Pu, L.; Wang, L.; Zhang, R.; Zhao, T.; Jiang, Y.; Han, L. Projected Global Trends in Ischemic Stroke Incidence, Deaths and Disability-Adjusted Life Years From 2020 to 2030. Stroke 2023, 54, 1330–1339. [Google Scholar] [CrossRef]
- Wang, S.; Zou, X.-L.; Wu, L.-X.; Zhou, H.-F.; Xiao, L.; Yao, T.; Zhang, Y.; Ma, J.; Zeng, Y.; Zhang, L. Epidemiology of intracerebral hemorrhage: A systematic review and meta-analysis. Front. Neurol. 2022, 13, 915813. [Google Scholar] [CrossRef]
- Hostettler, I.C.; Seiffge, D.J.; Werring, D.J. Intracerebral hemorrhage: An update on diagnosis and treatment. Expert Rev. Neurother. 2019, 19, 679–694. [Google Scholar] [CrossRef]
- van Gijn, J.; Rinkel, G.J. Subarachnoid haemorrhage: Diagnosis, causes and management. Brain 2001, 124, 249–278. [Google Scholar] [CrossRef]
- Isaksen, J.; Egge, A.; Waterloo, K.; Romner, B.; Ingebrigtsen, T. Risk factors for aneurysmal subarachnoid haemorrhage: The Tromsø study. J. Neurol. Neurosurg. Psychiatry 2002, 73, 185–187. [Google Scholar] [CrossRef] [PubMed]
- Nahed, B.V.; DiLuna, M.L.; Morgan, T.; Ocal, E.; Hawkins, A.A.; Ozduman, K.; Kahle, K.T.; Chamberlain, A.; Amar, A.P.; Gunel, M. Hypertension, age, and location predict rupture of small intracranial aneurysms. Neurosurgery 2005, 57, 676–683, discussion 676–683. [Google Scholar] [CrossRef] [PubMed]
- Tjoumakaris, S.I.; Hanel, R.; Mocco, J.; Ali-Aziz Sultan, M.; Froehler, M.; Lieber, B.B.; Coon, A.; Tateshima, S.; Altschul, D.J.; Narayanan, S.; et al. ARISE I Consensus Review on the Management of Intracranial Aneurysms. Stroke 2024, 55, 1428–1437. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, S.M.; Ziai, W.C.; Cordonnier, C.; Dowlatshahi, D.; Francis, B.; Goldstein, J.N.; Hemphill, J.C.; Johnson, R.; Keigher, K.M.; Mack, W.J.; et al. 2022 Guideline for the Management of Patients with Spontaneous Intracerebral Hemorrhage: A Guideline From the American Heart Association/American Stroke Association. Stroke 2022, 53, e282–e361. [Google Scholar] [CrossRef]
- Kurtz, P.; Fitts, V.; Sumer, Z.; Jalon, H.; Cooke, J.; Kvetan, V.; Mayer, S.A. How does care differ for neurological patients admitted to a neurocritical care unit versus a general ICU? Neurocrit. Care 2011, 15, 477–480. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’Connell, D.; Robertson, J.; Peterson, J.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analysis. Available online: https://www.google.com.hk/url?sa=t&source=web&rct=j&opi=89978449&url=http://www.evidencebasedpublichealth.de/download/Newcastle_Ottowa_Scale_Pope_Bruce.pdf&ved=2ahUKEwiin9PIrfWMAxU48DQHHY97GaIQFnoECBcQAQ&usg=AOvVaw1uMVAPUhnxn_VNxMRTmSFm (accessed on 5 March 2025).
- Drobot, R.B.; Stawarz, G.; Lipa, M.; Antoniewicz, A.A. Robot-Assisted Urachal Excision and Partial Cystectomy for Urachal Pathologies: Systematic Review with Insights from Single-Center Experience. J. Clin. Med. 2025, 14, 1273. [Google Scholar] [CrossRef]
- Tran, Q.K.; Dave, S.; Haase, D.J.; Tiffany, L.; Gaasch, S.; Chang, W.-T.W.; Jones, K.; Kole, M.J.; Wessell, A.; Schwartzbauer, G.; et al. Transfer of Patients with Spontaneous Intracranial Hemorrhage who Need External Ventricular Drain: Does Admission Location Matter? West. J. Emerg. Med. 2021, 22, 379–388. [Google Scholar] [CrossRef]
- Mirski, M.A.; Chang, C.W.; Cowan, R. Impact of a neuroscience intensive care unit on neurosurgical patient outcomes and cost of care: Evidence-based support for an intensivist-directed specialty ICU model of care. J. Neurosurg. Anesthesiol. 2001, 13, 83–92. [Google Scholar] [CrossRef]
- Diringer, M.N.; Edwards, D.F. Admission to a neurologic/neurosurgical intensive care unit is associated with reduced mortality rate after intracerebral hemorrhage. Crit. Care Med. 2001, 29, 635–640. [Google Scholar] [CrossRef]
- Lott, J.P.; Iwashyna, T.J.; Christie, J.D.; Asch, D.A.; Kramer, A.A.; Kahn, J.M. Critical illness outcomes in specialty versus general intensive care units. Am. J. Respir. Crit. Care Med. 2009, 179, 676–683. [Google Scholar] [CrossRef] [PubMed]
- Tran, Q.K.; Yarbrough, K.L.; Capobianco, P.; Chang, W.-T.W.; Jindal, G.; Medic, A.; Menaker, J.; Rehan, M.A.; Swafford, I.; Traynor, T.; et al. Comparison of Outcomes After Treatment of Large Vessel Occlusion in a Critical Care Resuscitation Unit or a Neurocritical Care Unit. Neurocrit. Care 2020, 32, 725–733. [Google Scholar] [CrossRef] [PubMed]
- Mielke, D.; Malinova, V.; Moerer, O.; Suntheim, P.; Voit, M.; Rohde, V. Does the subspecialty of an intensive care unit (ICU) has an impact on outcome in patients suffering from aneurysmal subarachnoid hemorrhage? Neurosurg. Rev. 2019, 42, 147–153. [Google Scholar] [CrossRef]
- Egawa, S.; Hifumi, T.; Kawakita, K.; Okauchi, M.; Shindo, A.; Kawanishi, M.; Tamiya, T.; Kuroda, Y. Impact of neurointensivist-managed intensive care unit implementation on patient outcomes after aneurysmal subarachnoid hemorrhage. J. Crit. Care 2016, 32, 52–55. [Google Scholar] [CrossRef] [PubMed]
- Moheet, A.M.; Livesay, S.L.; Abdelhak, T.; Bleck, T.P.; Human, T.; Karanjia, N.; Lamer-Rosen, A.; Medow, J.; Nyquist, P.A.; Rosengart, A.; et al. Standards for Neurologic Critical Care Units: A Statement for Healthcare Professionals from The Neurocritical Care Society. Neurocrit. Care 2018, 29, 145–160. [Google Scholar] [CrossRef] [PubMed]
- Varelas, P.N.; Eastwood, D.; Yun, H.J.; Spanaki, M.V.; Hacein Bey, L.; Kessaris, C.; Gennarelli, T.A. Impact of a neurointensivist on outcomes in patients with head trauma treated in a neurosciences intensive care unit. J. Neurosurg. 2006, 104, 713–719. [Google Scholar] [CrossRef]
- An, S.J.; Kim, T.J.; Yoon, B.-W. Epidemiology, Risk Factors, and Clinical Features of Intracerebral Hemorrhage: An Update. J. Stroke 2017, 19, 3–10. [Google Scholar] [CrossRef]
- Feigin, V.L.; Lawes, C.M.M.; Bennett, D.A.; Barker-Collo, S.L.; Parag, V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: A systematic review. Lancet Neurol. 2009, 8, 355–369. [Google Scholar] [CrossRef]
- Patel, N.M.; Tran, Q.K.; Capobianco, P.; Traynor, T.; Armahizer, M.J.; Motta, M.; Parikh, G.Y.; Badjatia, N.; Chang, W.-T.; Morris, N.A. Triage of Patients with Intracerebral Hemorrhage to Comprehensive Versus Primary Stroke Centers. J. Stroke Cerebrovasc. Dis. 2021, 30, 105672. [Google Scholar] [CrossRef]
- Burns, J.D.; Green, D.M.; Lau, H.; Winter, M.; Koyfman, F.; DeFusco, C.M.; Holsapple, J.W.; Kase, C.S. The Effect of a Neurocritical Care Service without a Dedicated Neuro-ICU on Quality of Care in Intracerebral Hemorrhage. Neurocrit. Care 2013, 18, 305–312. [Google Scholar] [CrossRef]
- Thilak, S.; Brown, P.; Whitehouse, T.; Gautam, N.; Lawrence, E.; Ahmed, Z.; Veenith, T. Diagnosis and management of subarachnoid haemorrhage. Nat. Commun. 2024, 15, 1850. [Google Scholar] [CrossRef]
- Weir, R.U.; Marcellus, M.L.; Do, H.M.; Steinberg, G.K.; Marks, M.P. Aneurysmal subarachnoid hemorrhage in patients with Hunt and Hess grade 4 or 5: Treatment using the Guglielmi detachable coil system. AJNR Am. J. Neuroradiol. 2003, 24, 585–590. [Google Scholar] [PubMed]
- Bracard, S.; Lebedinsky, A.; Anxionnat, R.; Neto, J.M.; Audibert, G.; Long, Y.; Picard, L. Endovascular treatment of Hunt and Hess grade IV and V aneuryms. AJNR Am. J. Neuroradiol. 2002, 23, 953–957. [Google Scholar] [PubMed]
- Samuels, O.; Webb, A.; Culler, S.; Martin, K.; Barrow, D. Impact of a dedicated neurocritical care team in treating patients with aneurysmal subarachnoid hemorrhage. Neurocrit. Care 2011, 14, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Josephson, S.A.; Douglas, V.C.; Lawton, M.T.; English, J.D.; Smith, W.S.; Ko, N.U. Improvement in intensive care unit outcomes in patients with subarachnoid hemorrhage after initiation of neurointensivist co-management. J. Neurosurg. 2010, 112, 626–630. [Google Scholar] [CrossRef]
- Herpich, F.; Rincon, F. Management of Acute Ischemic Stroke. Crit. Care Med. 2020, 48, 1654–1663. [Google Scholar] [CrossRef]
- Adcock, A.K.; Schwamm, L.H.; Smith, E.E.; Fonarow, G.C.; Reeves, M.J.; Xu, H.; Matsouaka, R.A.; Xian, Y.; Saver, J.L. Trends in Use, Outcomes, and Disparities in Endovascular Thrombectomy in US Patients with Stroke Aged 80 Years and Older Compared with Younger Patients. JAMA Netw. Open 2022, 5, e2215869. [Google Scholar] [CrossRef]
- Asif, K.S.; Otite, F.O.; Desai, S.M.; Herial, N.; Inoa, V.; Al-Mufti, F.; Jadhav, A.P.; Dmytriw, A.A.; Castonguay, A.; Khandelwal, P.; et al. Mechanical Thrombectomy Global Access for Stroke (MT-GLASS): A Mission Thrombectomy (MT-2020 Plus) Study. Circulation 2023, 147, 1208–1220. [Google Scholar] [CrossRef]
- Etminan, N.; Macdonald, R.L. Management of aneurysmal subarachnoid hemorrhage. Handb. Clin. Neurol. 2017, 140, 195–228. [Google Scholar] [CrossRef]
- Prust, M.L.; Mbonde, A.; Rubinos, C.; Shrestha, G.S.; Komolafe, M.; Saylor, D.; Mangat, H.S. Providing Neurocritical Care in Resource-Limited Settings: Challenges and Opportunities. Neurocrit. Care 2022, 37, 583–592. [Google Scholar] [CrossRef]
- Raees, M.; Cheserem, B.; Mutiso, B.; Laeke, T.; Brotherton, B.J. The Next Frontier in Neurocritical Care in Resource-Constrained Settings. Crit. Care Clin. 2022, 38, 721–745. [Google Scholar] [CrossRef] [PubMed]
- Mehrpour, M.; Taghipour, S.; Abdollahi, S.; Oliaee, F.; Goran, A.; Motamed, M.; Ashayeri, R. Positive impact of stroke unit establishment on patient recovery in Firoozgar hospital. Med. J. Islam. Repub. Iran. 2016, 30, 446. [Google Scholar] [PubMed]
- Santana, D.; Mosteiro, A.; Llull, L.; Massons, M.; Zattera, L.; Pujol-Fontrodona, G.; Werner, M.; Torné, R.; Amaro, S.; Chamorro, A. Stroke Unit as an alternative to Intensive Care Unit for initial hospital admission of low-grade non-aneurysmal subarachnoid haemorrhage: A safety and cost-minimisation analysis. Eur. Stroke J. 2024, 9, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Sadaka, F.; Cytron, M.A.; Fowler, K.; Javaux, V.M.; O’Brien, J. A Model for Identifying Patients Who May Not Need Neurologic Intensive Care Unit Admission: Resource Utilization Study. J. Intensive Care Med. 2016, 31, 193–197. [Google Scholar] [CrossRef]
| Author | Year | Country | Pathology | Comparison |
|---|---|---|---|---|
| Tran et al. [19] | 2021 | USA | ICH | NCCU vs. CCRU vs. other ICUs |
| Mirski et al. [20] | 2001 | USA | ICH | Neurological ICU vs. general ICU (surgical or medical ICUs) |
| Diringer et al. [21] | 2001 | Germany | ICH | Neurosurgical ICU vs. general ICU |
| Lott et al. [22] | 2009 | USA | AIS and ICH | General ICU vs. neurological ICU vs. non-ideal specialty ICU |
| Tran et al. [23] | 2020 | USA | AIS | NCCU vs. CCRU vs. other ICU |
| Mielke et al. [24] | 2019 | Germany | aSAH | Neurosurgical ICU vs. general ICU |
| Egawa et al. [25] | 2016 | Japan | aSAH | Intensivist-managed ICU vs. neurointensivist-managed ICU |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roy, J.M.; Musmar, B.; Tziviskos, N.; Patel, S.; DeLeon, R.; Thommana, A.; Mina, S.; Tjoumakaris, S.I.; Gooch, M.R.; Rosenwasser, R.H.; et al. Comparison of Outcomes Among Neurovascular Patients Managed in Dedicated Neurological Intensive Care Units vs. General Intensive Care Units. J. Clin. Med. 2025, 14, 3090. https://doi.org/10.3390/jcm14093090
Roy JM, Musmar B, Tziviskos N, Patel S, DeLeon R, Thommana A, Mina S, Tjoumakaris SI, Gooch MR, Rosenwasser RH, et al. Comparison of Outcomes Among Neurovascular Patients Managed in Dedicated Neurological Intensive Care Units vs. General Intensive Care Units. Journal of Clinical Medicine. 2025; 14(9):3090. https://doi.org/10.3390/jcm14093090
Chicago/Turabian StyleRoy, Joanna M., Basel Musmar, Nassos Tziviskos, Saarang Patel, Roberto DeLeon, Ashley Thommana, Shady Mina, Stavropoula I. Tjoumakaris, Michael. Reid Gooch, Robert H. Rosenwasser, and et al. 2025. "Comparison of Outcomes Among Neurovascular Patients Managed in Dedicated Neurological Intensive Care Units vs. General Intensive Care Units" Journal of Clinical Medicine 14, no. 9: 3090. https://doi.org/10.3390/jcm14093090
APA StyleRoy, J. M., Musmar, B., Tziviskos, N., Patel, S., DeLeon, R., Thommana, A., Mina, S., Tjoumakaris, S. I., Gooch, M. R., Rosenwasser, R. H., & Jabbour, P. M. (2025). Comparison of Outcomes Among Neurovascular Patients Managed in Dedicated Neurological Intensive Care Units vs. General Intensive Care Units. Journal of Clinical Medicine, 14(9), 3090. https://doi.org/10.3390/jcm14093090






