Impact of Single-Lumen Versus Double-Lumen Endotracheal Tube on Postoperative Swallowing Function in Lung Transplantation Patients: A Single-Center, Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Outcomes
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BOS | Bronchiolitis obliterans syndrome |
| CPB | Cardiopulmonary bypass |
| DLT | Double-lumen endotracheal tube |
| ECMO | Extracorporeal membrane oxygenation |
| EMR | Electronic medical record |
| FOIS | Functional oral intake score |
| ICU | Intensive care unit |
| IDDSI | International dysphagia diet standardization initiative |
| IRB | International review board |
| LOS | Length of stay |
| LTx | Lung transplant |
| MBSS | Modified barium swallow study |
| OPD | Oropharyngeal dysphagia |
| SLT | Single-lumen endotracheal tube |
References
- Atkins, B.Z.; Petersen, R.P.; Daneshmand, M.A.; Turek, J.W.; Lin, S.S.; Davis, R.D. Impact of Oropharyngeal Dysphagia on Long-Term Outcomes of Lung Transplantation. Ann. Thorac. Surg. 2010, 90, 1622–1628. [Google Scholar] [CrossRef] [PubMed]
- Atkins, B.Z.; Trachtenberg, M.S.; Prince-Petersen, R.; Vess, G.; Bush, E.L.; Balsara, K.R.; Lin, S.S.; Davis, R.D. Assessing Oropharyngeal Dysphagia After Lung Transplantation: Altered Swallowing Mechanisms and Increased Morbidity. J. Heart Lung Transplant. 2007, 26, 1144–1148. [Google Scholar] [CrossRef] [PubMed]
- Baumann, B.; Byers, S.; Wasserman-Wincko, T.; Smith, L.; Hathaway, B.; Bhama, J.; Shigemura, N.; Hayanga, J.A.; D’Cunha, J.; Johnson, J.T. Postoperative Swallowing Assessment After Lung Transplantation. Ann. Thorac. Surg. 2017, 104, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Arjuna, A.; Olson, M.T.; Walia, R.; Bremner, R.M.; Smith, M.A.; Mohanakumar, T. An update on current treatment strategies for managing bronchiolitis obliterans syndrome after lung transplantation. Expert Rev. Respir. Med. 2021, 15, 339–350. [Google Scholar] [CrossRef] [PubMed]
- Malik, Z.; Shenoy, K. Esophageal Evaluation for Patients Undergoing Lung Transplant Evaluation. Gastroenterol. Clin. North Am. 2020, 49, 451–466. [Google Scholar] [CrossRef] [PubMed]
- D’ovidio, F.; Mura, M.; Tsang, M.; Waddell, T.K.; Hutcheon, M.A.; Singer, L.G.; Hadjiliadis, D.; Chaparro, C.; Gutierrez, C.; Pierre, A.; et al. Bile acid aspiration and the development of bronchiolitis obliterans after lung transplantation. J. Thorac. Cardiovasc. Surg. 2005, 129, 1144–1152. [Google Scholar] [CrossRef] [PubMed]
- Murthy, R.; Williams, D.; Kinnebrew, S.; Waters, J.; Torres, F.; Kaza, V.; Ring, W.; Wait, M.; Peltz, M. Oropharyngeal Dysphagia and Aspiration After Lung Transplantation in the Current Era. J. Heart Lung Transplant. 2015, 34, S252. [Google Scholar] [CrossRef]
- Plowman, E.; DiBiase, L.; Anderson, A.; Colsky, J.; Eckart, J.; Scheuble, V.; Chandrashekaran, S.; Emtiazjoo, A.; Shahmohammadi, A.; Alnuaimat, H.; et al. Incidence of Dysphagia and Associated Morbidity in Lung Transplanted Adults. J. Heart Lung Transplant. 2020, 39, S385. [Google Scholar] [CrossRef]
- Graham, K.; Kaiho, T.; Thomae, B.L.; Yagi, Y.; Cerier, E.; Martin-Harris, B.; Bharat, A.; Kurihara, C. Risk factors and impact of swallowing impairment and aspiration after lung transplantation. J. Thorac. Dis. 2024, 16, 5755–5764. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Crary, M.A.; Mann, G.D.C.; Groher, M.E. Initial Psychometric Assessment of a Functional Oral Intake Scale for Dysphagia in Stroke Patients. Arch. Phys. Med. Rehabil. 2005, 86, 1516–1520. [Google Scholar] [CrossRef] [PubMed]
- Zielske, J.; Bohne, S.; Brunkhorst, F.M.; Axer, H.; Guntinas-Lichius, O. Acute and long-term dysphagia in critically ill patients with severe sepsis: Results of a prospective controlled observational study. Eur. Arch. Oto-Rhino-Laryngol. 2014, 271, 3085–3093. [Google Scholar] [CrossRef]
- Steele, C.M.; Namasivayam-MacDonald, A.M.; Guida, B.T.; Cichero, J.A.; Duivestein, J.; Hanson, B.; Lam, P.; Riquelme, L.F. Creation and Initial Validation of the International Dysphagia Diet Standardisation Initiative Functional Diet Scale. Arch. Phys. Med. Rehabil. 2018, 99, 934–944. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ito, I.; Hamada, K.; Sato, H.; Shindo, N. Long-Lasting Dysphagia Developing After Thoracotomy for Pulmonary Resection: A Case Series. Indian J. Surg. 2017, 79, 486–491. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Krisciunas, G.P.M.; Langmore, S.E.; Gomez-Taborda, S.B.; Fink, D.; Levitt, J.E.; McKeehan, J.M.; McNally, E.; Scheel, R.; Rubio, A.C.B.; Siner, J.M.; et al. The Association Between Endotracheal Tube Size and Aspiration (During Flexible Endoscopic Evaluation of Swallowing) in Acute Respiratory Failure Survivors. Crit. Care Med. 2020, 48, 1604–1611. [Google Scholar] [CrossRef] [PubMed]
- Iyer, M.H.; Kumar, N.; Hussain, N.; Essandoh, M.; Kumar, J.; Gorelik, L.; Flores, A.S.; Bhandary, S.P.; Bhatt, A. Airway Management During Anesthesia for Lung Transplantation: Double-Lumen Tube or Endobronchial Blocker? J. Cardiothorac. Vasc. Anesth. 2021, 35, 1286–1291. [Google Scholar] [CrossRef] [PubMed]
- Marczin, N.; de Waal, E.E.; Hopkins, P.M.; Mulligan, M.S.; Simon, A.; Shaw, A.D.; Van Raemdonck, D.; Neyrinck, A.; Gries, C.J.; Algotsson, L.; et al. International consensus recommendations for anesthetic and intensive care management of lung transplantation. An EACTAIC, SCA, ISHLT, ESOT, ESTS, and AST approved document. J. Heart Lung Transplant. 2021, 40, 1327–1348. [Google Scholar] [CrossRef] [PubMed]
- Duthie, D.J.; O’Leary, R. Double lumen endobronchial tube (DLT) sizes in routine practice. Eur. J. Anaesthesiol. 2012, 29, 231. [Google Scholar] [CrossRef]
- Shah, S.B.; Hariharan, U.; Chawla, R. Choosing the Correct-Sized Adult Double-Lumen Tube: Quest for the Holy Grail. Ann. Card. Anaesth. 2023, 26, 124–132. [Google Scholar] [CrossRef] [PubMed]


| Characteristic | Single (n = 21) | Double (n = 49) | p |
|---|---|---|---|
| Age, years * | 63.6 (8.10) | 54.9 (12.9) | 0.006 |
| Sex, Male | 14 (66.7) | 28 (57.1) | 0.456 |
| BMI, kg/m2 * | 26.8 (3.39) | 25.3 (3.88) | 0.119 |
| Lung transplant type | 0.212 | ||
| Left lung | 2 (9.52) | 1 (2.04) | |
| Both | 19 (90.5) | 48 (98.0) | |
| Any ECMO, Yes | 2 (9.52) | 14 (28.6) | 0.121 |
| Intraoperative ECMO, Yes | 1 (4.76) | 10 (20.4) | 0.154 |
| Postoperative ECMO, Yes | 1 (4.76) | 4 (8.16) | 1.000 |
| Cardiopulmonary bypass, Yes | 20 (95.2) | 36 (73.5) | 0.050 |
| Intraoperative cardiopulmonary mechanical support time, min † | 163 (45; 87, 456) | 124 (81; 0, 294) | 0.002 |
| Tracheostomy, Yes | 3 (14.3) | 3 (6.12) | 0.355 |
| Operative time, min † | 378 (89; 237, 499) | 377 (93; 104, 626) | 0.380 |
| Ventilation time, min † | 1800 (2306; 592, 49,928) | 1195 (1086; 400, 85,420) | 0.183 |
| Univariate | Multivariable | |||
|---|---|---|---|---|
| Predictor | cOR (95% CI) | p | cOR (95% CI) | p |
| Type of Lumen Tube, Double vs. Single | 2.90 (1.08, 7.82) | 0.035 | 5.17 (1.68, 15.9) | 0.004 |
| Operative time, 1 h increase | 0.74 (0.50, 1.11) | 0.144 | 0.69 (0.45, 1.05) | 0.086 |
| Intraop ECMO, Yes vs. No | 0.31 (0.09, 1.04) | 0.057 | 0.18 (0.05, 0.70) | 0.013 |
| Intraop CPB, Yes vs. No | 2.38 (0.78, 7.24) | 0.126 | ||
| CPB time, 10 min increase | 0.94 (0.88, 1.01) | 0.100 | ||
| Age, 1 year increase | 1.01 (0.97, 1.05) | 0.718 | ||
| Sex, Male vs. Female | 0.87 (0.34, 2.25) | 0.780 | ||
| BMI, 1 kg/m2 increase | 0.98 (0.87, 1.11) | 0.779 | ||
| Time on Ventilator, 1 h increase | 0.999 (0.997, 1.001) | 0.328 | ||
| Outcome | Single (n = 21) | Double (n = 49) | p |
|---|---|---|---|
| Discharge Destination, n (%) | 1.000 | ||
| Home | 14 (66.7) | 32 (65.3) | |
| Rehabilitation Center | 2 (9.52) | 4 (8.16) | |
| Other | 5 (23.8) | 13 (26.5) | |
| 30-Day ventilator-free days, median (IQR; range) | 28.4 (1.1; 0, 29.5) | 28.6 (0.29; 0, 39.3) | 0.049 |
| ICU length of stay, days, median (IQR; range) | 6 (5; 3, 140) | 6 (3; 3, 48) | 0.643 |
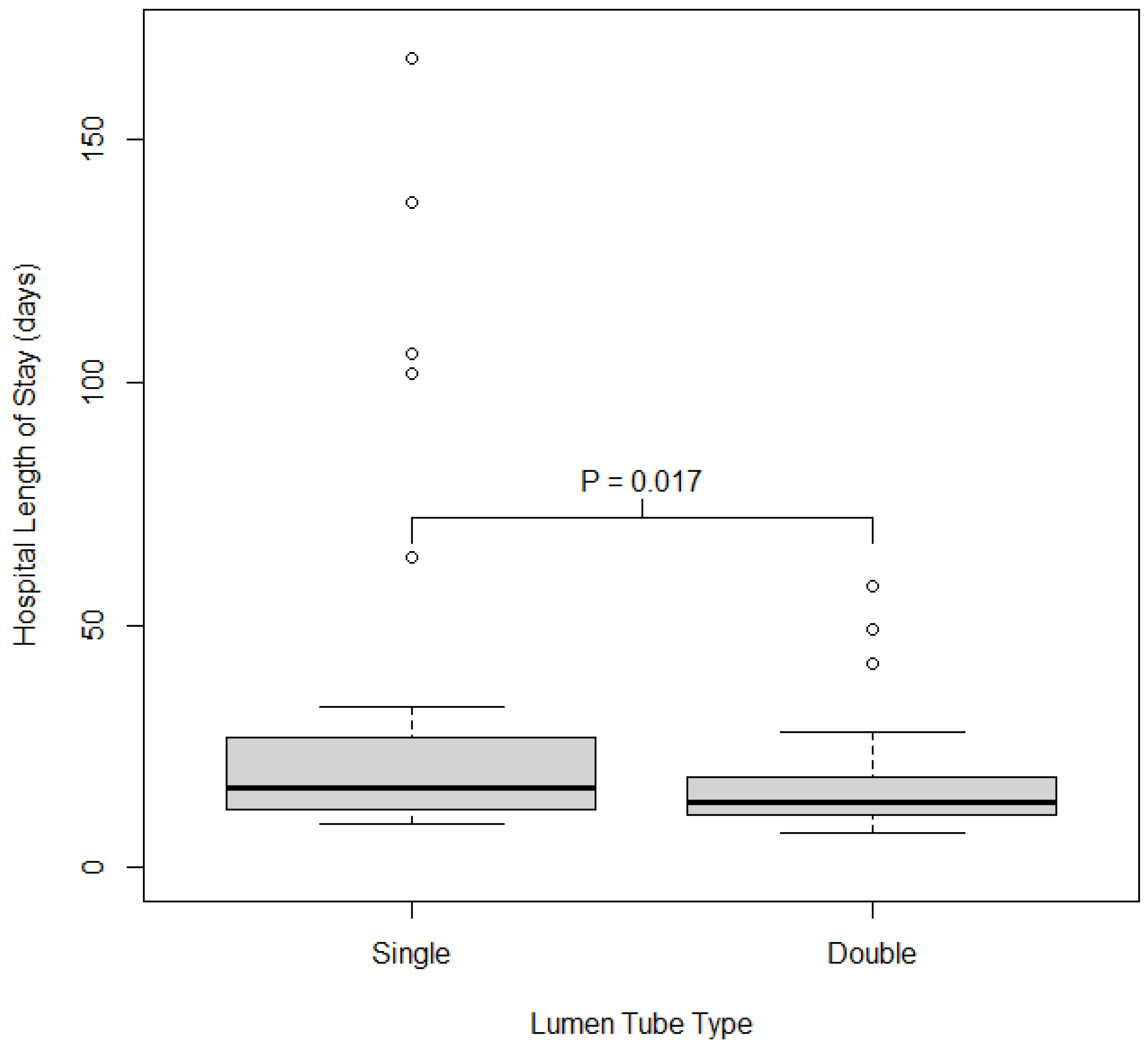
| Hospital length of stay, days, median (IQR; range) | 18 (13; 10, 167) | 14 (7; 7, 102) | 0.017 |
| FiO2 72 h Postop | 40 (10; 20, 60) | 25 (11; 21, 100) | 0.005 |
| PO2 arterial 72 h Postop | 84 (57; 36, 227) | 86 (27; 38, 376) | 0.796 |
| PO2/FiO2 ratio | 255 (187.6; 71.7, 905) | 314.3 (87.5; 140, 850) | 0.038 |
| Any Enteral Nutrition via Feeding Tube, Yes | 16 (76.2) | 25 (51.0) | 0.050 |
| If Yes, duration in days | 8.5 (10; 1, 146) | 5 (8; 1, 82) | 0.532 |
| If Yes, # enteral feedings | 7.5 (8; 1, 31) | 5 (9; 1, 28) | 0.873 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patel, R.A.; Nitchie, H.; Wolf, B.J.; Taylor, C.; Francis, L. Impact of Single-Lumen Versus Double-Lumen Endotracheal Tube on Postoperative Swallowing Function in Lung Transplantation Patients: A Single-Center, Retrospective Cohort Study. J. Clin. Med. 2025, 14, 3075. https://doi.org/10.3390/jcm14093075
Patel RA, Nitchie H, Wolf BJ, Taylor C, Francis L. Impact of Single-Lumen Versus Double-Lumen Endotracheal Tube on Postoperative Swallowing Function in Lung Transplantation Patients: A Single-Center, Retrospective Cohort Study. Journal of Clinical Medicine. 2025; 14(9):3075. https://doi.org/10.3390/jcm14093075
Chicago/Turabian StylePatel, Rishi Ashok, Haley Nitchie, Bethany J. Wolf, Cecilia Taylor, and Loren Francis. 2025. "Impact of Single-Lumen Versus Double-Lumen Endotracheal Tube on Postoperative Swallowing Function in Lung Transplantation Patients: A Single-Center, Retrospective Cohort Study" Journal of Clinical Medicine 14, no. 9: 3075. https://doi.org/10.3390/jcm14093075
APA StylePatel, R. A., Nitchie, H., Wolf, B. J., Taylor, C., & Francis, L. (2025). Impact of Single-Lumen Versus Double-Lumen Endotracheal Tube on Postoperative Swallowing Function in Lung Transplantation Patients: A Single-Center, Retrospective Cohort Study. Journal of Clinical Medicine, 14(9), 3075. https://doi.org/10.3390/jcm14093075






