Mortality Trends in Patients Undergoing Hemodialysis, 2003–2021: Data from National Health Insurance Service in Korea
Abstract
1. Introduction
2. Methods
2.1. Data Sources
2.2. Study Population
2.3. Outcome Measurement
2.4. Statistical Analyses
3. Results
3.1. Study Population
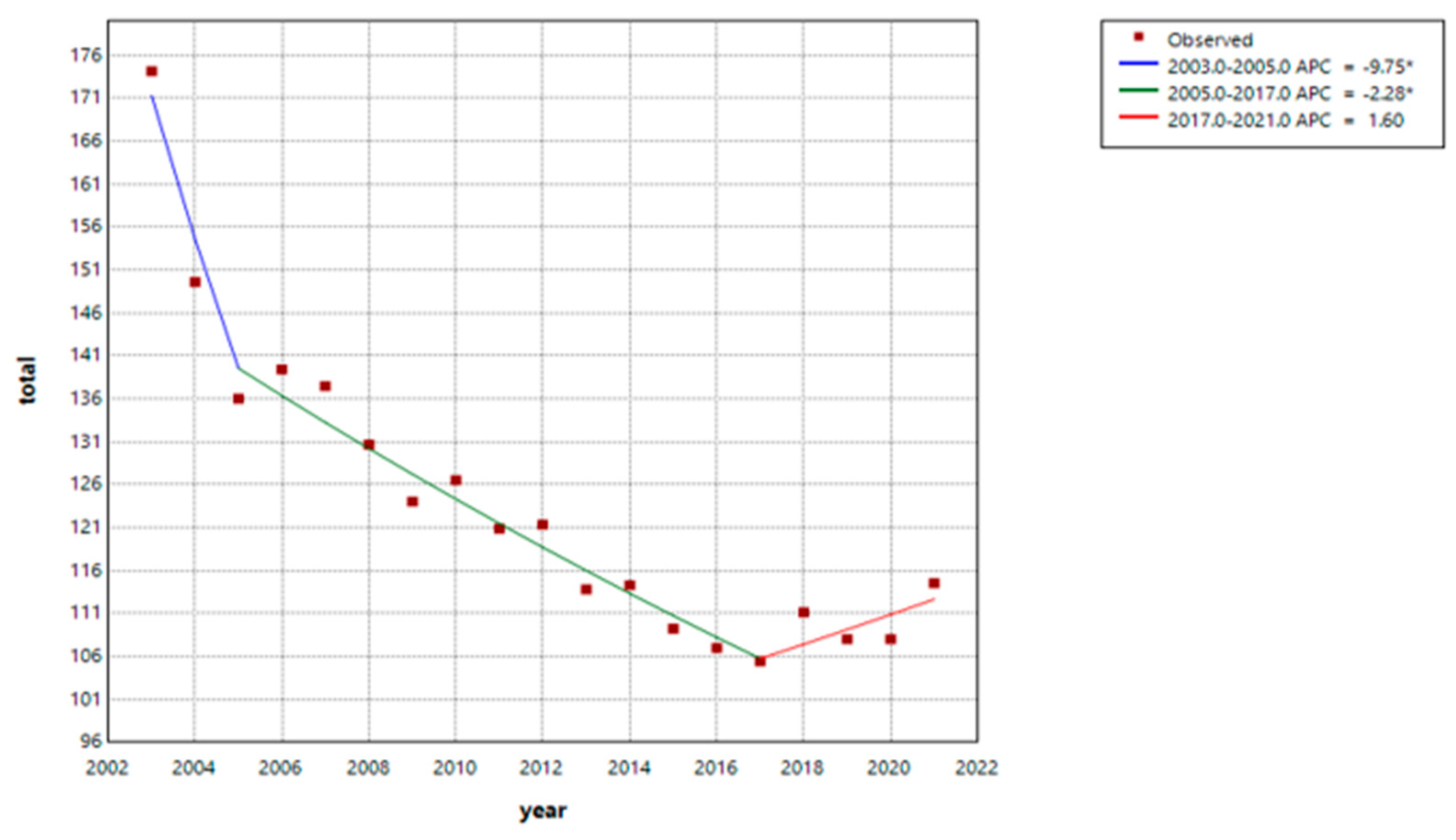
3.2. Mortality Trend
3.3. Trends in Mortality Rates by Cause
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Deziel, C.; Bouchard, J.; Zellweger, M.; Madore, F. Impact of hemocontrol on hypertension, nursing interventions, and quality of life: A randomized, controlled trial. Clin. J. Am. Soc. Nephrol. 2007, 2, 661–668. [Google Scholar] [CrossRef] [PubMed]
- Pruett, B.; Johnson, S.; O’Keefe, N. Improving IV iron and anemia management in the hemodialysis setting: A collaborative CQI approach. Nephrol. Nurs. J. 2007, 34, 206–213. [Google Scholar] [PubMed]
- van Walraven, C.; Manuel, D.G.; Knoll, G. Survival trends in ESRD patients compared with the general population in the United States. Am. J. Kidney Dis. 2014, 63, 491–499. [Google Scholar] [CrossRef]
- Wakasugi, M.; Kazama, J.J.; Narita, I. Mortality trends among Japanese dialysis patients, 1988–2013: A joinpoint regression analysis. Nephrol. Dial. Transplant. 2016, 31, 1501–1507. [Google Scholar] [CrossRef] [PubMed]
- Roberts, M.A.; Polkinghorne, K.R.; McDonald, S.P.; Ierino, F.L. Secular trends in cardiovascular mortality rates of patients receiving dialysis compared with the general population. Am. J. Kidney Dis. 2011, 58, 64–72. [Google Scholar] [CrossRef]
- Wakasugi, M.; Kazama, J.J.; Yamamoto, S.; Kawamura, K.; Narita, I. Cause-specific excess mortality among dialysis patients: Comparison with the general population in Japan. Ther. Apher. Dial. 2013, 17, 298–304. [Google Scholar] [CrossRef]
- Lindner, A.; Charra, B.; Sherrard, D.J.; Scribner, B.H. Accelerated atherosclerosis in prolonged maintenance hemodialysis. N. Engl. J. Med. 1974, 290, 697–701. [Google Scholar] [CrossRef]
- Foley, R.N.; Parfrey, P.S.; Sarnak, M.J. Clinical epidemiology of cardiovascular disease in chronic renal disease. Am. J. Kidney Dis. 1998, 32, S112–S119. [Google Scholar] [CrossRef]
- Foley, R.N.; Parfrey, P.S.; Sarnak, M.J. Epidemiology of cardiovascular disease in chronic renal disease. J. Am. Soc. Nephrol. 1998, 9, S16–S23. [Google Scholar]
- Cheung, A.K.; Sarnak, M.J.; Yan, G.; Berkoben, M.; Heyka, R.; Kaufman, A.; Lewis, J.; Rocco, M.; Toto, R.; Windus, D.; et al. Cardiac diseases in maintenance hemodialysis patients: Results of the HEMO Study. Kidney Int. 2004, 65, 2380–2389. [Google Scholar] [CrossRef]
- KNS. Mortality Rate in General Population. 2023. Available online: https://www.kostat.go.kr/board.es?mid=a10301010000&bid=218&act=view&list_no=433106 (accessed on 20 March 2025).
- Storey, B.C.; Staplin, N.; Harper, C.H.; Haynes, R.; Winearls, C.G.; Goldacre, R.; Emberson, J.R.; Goldacre, M.J.; Baigent, C.; Landray, M.J.; et al. Declining comorbidity-adjusted mortality rates in English patients receiving maintenance renal replacement therapy. Kidney Int. 2018, 93, 1165–1174. [Google Scholar] [CrossRef]
- USRDS 2022 Annual Data Reports. Available online: https://www.niddk.nih.gov/about-niddk/strategic-plans-reports/usrds/prior-data-reports (accessed on 20 March 2025).
- Pippias, M.; Jager, K.J.; Kramer, A.; Leivestad, T.; Sanchez, M.B.; Caskey, F.J.; Collart, F.; Couchoud, C.; Dekker, F.W.; Finne, P.; et al. The changing trends and outcomes in renal replacement therapy: Data from the ERA-EDTA Registry. Nephrol. Dial. Transplant. 2016, 31, 831–841. [Google Scholar] [CrossRef]
- Fliser, D.; Wiecek, A.; Suleymanlar, G.; Ortiz, A.; Massy, Z.; Lindholm, B.; Martinez-Castelao, A.; Agarwal, R.; Jager, K.J.; Dekker, F.W.; et al. The dysfunctional endothelium in CKD and in cardiovascular disease: Mapping the origin(s) of cardiovascular problems in CKD and of kidney disease in cardiovascular conditions for a research agenda. Kidney Int. Suppl. (2011) 2011, 1, 6–9. [Google Scholar] [CrossRef]
- Gansevoort, R.T.; Correa-Rotter, R.; Hemmelgarn, B.R.; Jafar, T.H.; Heerspink, H.J.; Mann, J.F.; Matsushita, K.; Wen, C.P. Chronic kidney disease and cardiovascular risk: Epidemiology, mechanisms, and prevention. Lancet 2013, 382, 339–352. [Google Scholar] [CrossRef]
- Nichols, M.; Townsend, N.; Scarborough, P.; Rayner, M. Cardiovascular disease in Europe 2014: Epidemiological update. Eur. Heart J. 2014, 35, 2929. [Google Scholar] [CrossRef]
- Szummer, K.; Lindhagen, L.; Evans, M.; Spaak, J.; Koul, S.; Akerblom, A.; Carrero, J.J.; Jernberg, T. Treatments and Mortality Trends in Cases With and Without Dialysis Who Have an Acute Myocardial Infarction: An 18-Year Nationwide Experience. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005879. [Google Scholar] [CrossRef]
- Lin, T.Y.; Hsieh, T.H.; Hung, S.C. Association of secondary prevention medication use after myocardial infarction with mortality in hemodialysis patients. Clin. Kidney J. 2022, 15, 2135–2143. [Google Scholar] [CrossRef]
- de Bie, M.K.; Ajmone Marsan, N.; Gaasbeek, A.; Bax, J.J.; Groeneveld, M.; Gabreels, B.A.; Delgado, V.; Rabelink, T.J.; Schalij, M.J.; Jukema, J.W. Left ventricular diastolic dysfunction in dialysis patients assessed by novel speckle tracking strain rate analysis: Prevalence and determinants. Int. J. Nephrol. 2012, 2012, 963504. [Google Scholar] [CrossRef]
- Antlanger, M.; Aschauer, S.; Kopecky, C.; Hecking, M.; Kovarik, J.J.; Werzowa, J.; Mascherbauer, J.; Genser, B.; Saemann, M.D.; Bonderman, D. Heart Failure with Preserved and Reduced Ejection Fraction in Hemodialysis Patients: Prevalence, Disease Prediction and Prognosis. Kidney Blood Press. Res. 2017, 42, 165–176. [Google Scholar] [CrossRef]
- Zhao, X.; Gan, L.; Niu, Q.; Hou, F.F.; Liang, X.; Chen, X.; Chen, Y.; Zhao, J.; McCullough, K.; Ni, Z.; et al. Clinical Outcomes in Patients on Hemodialysis with Congestive Heart Failure. Kidney Dis. 2023, 9, 306–316. [Google Scholar] [CrossRef]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Mathers, C.; Parkin, D.M.; Pineros, M.; Znaor, A.; Bray, F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 2019, 144, 1941–1953. [Google Scholar] [CrossRef] [PubMed]
- Rosner, M.H. Cancer Screening in Patients Undergoing Maintenance Dialysis: Who, What, and When. Am. J. Kidney Dis. 2020, 76, 558–566. [Google Scholar] [CrossRef] [PubMed]
- Rosales, B.M.; De La Mata, N.; Vajdic, C.M.; Kelly, P.J.; Wyburn, K.; Webster, A.C. Cancer Mortality in People Receiving Dialysis for Kidney Failure: An Australian and New Zealand Cohort Study, 1980–2013. Am J Kidney Dis 2022, 80, 449–461. [Google Scholar] [CrossRef] [PubMed]
- McCullough, K.P.; Morgenstern, H.; Rayner, H.C.; Port, F.K.; Jadoul, M.Y.; Akizawa, T.; Pisoni, R.L.; Herman, W.H.; Robinson, B.M.; Investigators, D.C. Explaining International Trends in Mortality on Hemodialysis Through Changes in Hemodialysis Practices in the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am. J. Kidney Dis. 2025, 85, 25–35.e21. [Google Scholar] [CrossRef]
- Hecking, M.; Bieber, B.A.; Ethier, J.; Kautzky-Willer, A.; Sunder-Plassmann, G.; Saemann, M.D.; Ramirez, S.P.; Gillespie, B.W.; Pisoni, R.L.; Robinson, B.M.; et al. Sex-specific differences in hemodialysis prevalence and practices and the male-to-female mortality rate: The Dialysis Outcomes and Practice Patterns Study (DOPPS). PLoS Med. 2014, 11, e1001750. [Google Scholar] [CrossRef]

| General Population | The Study Population | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | |
| 2003 | 59.6 | 108.4 | 263.8 | 567.7 | 1360.3 | 3688.8 | 11,593.4 | 3508.8 | 5231.9 | 7106.3 | 9742.5 | 17,661.6 | 24,975.9 | 41,678.5 |
| 2004 | 51.0 | 97.8 | 254.4 | 548.7 | 1315.5 | 3536.1 | 11,294.9 | 4038.3 | 4288.4 | 5886.8 | 9955.8 | 15,436.8 | 21,652.6 | 31,123.4 |
| 2005 | 54.3 | 96.1 | 239.1 | 511.6 | 1252.9 | 3383.7 | 11,053.2 | 4554.9 | 2215.9 | 4497.9 | 7945.7 | 13,688.4 | 20,749.8 | 31,111.1 |
| 2006 | 47.8 | 85.1 | 223.5 | 492.4 | 1176.5 | 3212.2 | 10,825.7 | 3692.3 | 3757.6 | 5600.4 | 9329.2 | 14,554.1 | 19,179.2 | 30,420.2 |
| 2007 | 55.1 | 87.1 | 218.4 | 461.5 | 1121.9 | 3086.6 | 10,501.5 | 4246.3 | 3993.9 | 6051.8 | 8983.7 | 14,285.7 | 18,986.4 | 29,926.3 |
| 2008 | 55.4 | 86.2 | 210.8 | 446.6 | 1052.3 | 2918.3 | 10,009.1 | 3104.9 | 3563.1 | 6288.5 | 8915.9 | 13,410.1 | 18,122.6 | 27,636.5 |
| 2009 | 56.8 | 92.1 | 206.5 | 433.0 | 1001.8 | 2766.0 | 9398.7 | 4100.2 | 3200.9 | 6225.9 | 8416.5 | 13,034.8 | 16,948.0 | 25,568.2 |
| 2010 | 54.3 | 87.4 | 201.7 | 420.8 | 971.7 | 2740.9 | 9423.9 | 3624.2 | 3686.9 | 6119.9 | 8124.6 | 14,184.2 | 17,044.5 | 26,034.1 |
| 2011 | 51.4 | 83.2 | 187.7 | 408.2 | 923.0 | 2623.6 | 9245.1 | 3428.6 | 3307.3 | 6593.1 | 8668.7 | 12,979.6 | 15,926.9 | 23,964.1 |
| 2012 | 45.0 | 79.5 | 180.5 | 389.9 | 873.5 | 2610.8 | 9466.6 | 4740.7 | 4565.9 | 5651.8 | 8299.1 | 13,469.2 | 16,400.8 | 23,451.1 |
| 2013 | 42.3 | 78.2 | 174.4 | 382.1 | 821.8 | 2475.5 | 8902.6 | 5223.9 | 4619.0 | 6889.5 | 7804.0 | 11,822.2 | 15,636.1 | 20,950.7 |
| 2014 | 39.2 | 75.7 | 165.8 | 372.4 | 781.7 | 2358.0 | 8597.5 | 5580.0 | 4442.1 | 6771.6 | 8730.8 | 11,713.2 | 15,342.1 | 20,223.4 |
| 2015 | 39.7 | 70.6 | 161.2 | 352.9 | 758.5 | 2333.6 | 8584.7 | 5516.3 | 5296.0 | 6853.5 | 8241.9 | 10,645.1 | 15,033.4 | 18,918.6 |
| 2016 | 37.4 | 68.8 | 153.6 | 346.9 | 740.8 | 2239.0 | 8393.2 | 4039.0 | 5112.8 | 6854.4 | 8508.1 | 10,434.8 | 13,978.3 | 19,111.2 |
| 2017 | 36.6 | 66.5 | 147.0 | 332.4 | 692.6 | 2138.0 | 8342.7 | 5483.4 | 6213.9 | 7081.9 | 7862.5 | 10,085.9 | 14,195.7 | 18,704.0 |
| 2018 | 37.3 | 69.8 | 148.2 | 330.7 | 684.9 | 2092.6 | 8407.7 | 6278.0 | 5889.2 | 7569.7 | 8958.1 | 10,417.9 | 14,877.1 | 19,029.2 |
| 2019 | 37.7 | 69.0 | 143.0 | 320.4 | 652.4 | 1948.1 | 7833.7 | 6240.7 | 6059.5 | 7868.7 | 9080.8 | 9536.9 | 14,263.8 | 18,619.7 |
| 2020 | 39.9 | 68.8 | 140.4 | 309.1 | 638.1 | 1895.5 | 7824.5 | 5555.6 | 7316.1 | 8923.0 | 8917.5 | 9393.2 | 14,035.6 | 18,049.7 |
| 2021 | 41.4 | 67.2 | 137.7 | 297.5 | 646.2 | 1873.6 | 7847.3 | 6679.0 | 8011.6 | 9375.8 | 9826.9 | 9864.7 | 14,690.7 | 18,825.1 |
| 2003–2007 | 2008–2012 | 2013–2017 | 2018–2021 | |
|---|---|---|---|---|
| Number of patients | 166,450 | 266,000 | 357,262 | 354,377 |
| Men, N (%) | 93,598 (56.23) | 151,615 (57.00) | 206,252 (57.73) | 209,265 (59.05) |
| Age group, N (%) | ||||
| 20–34 years | 10,000 (6.01) | 9875 (3.71) | 8392 (2.35) | 5911 (1.67) |
| 35–49 | 35,414 (21.28) | 47,945 (18.02) | 49,859 (13.96) | 37,879 (10.69) |
| 50–64 | 61,510 (36.95) | 97,839 (36.78) | 12,7021 (35.55) | 117,097 (33.04) |
| 65–79 | 52,385 (31.47) | 92,274 (34.69) | 131,220 (36.73) | 134,419 (37.93) |
| 80+ | 7141 (4.29) | 18,067 (6.79) | 40,770 (11.41) | 59,071 (16.67) |
| Year | Age-Standardized Mortality Rates (per 1000 Person-Years) | ||
|---|---|---|---|
| Total | Men | Women | |
| 2003 | 174.14 | 176.92 | 173.36 |
| 2004 | 149.61 | 155.14 | 144.06 |
| 2005 | 136.03 | 140.83 | 129.99 |
| 2006 | 139.44 | 143.62 | 134.45 |
| 2007 | 137.48 | 139.38 | 135.57 |
| 2008 | 130.63 | 133.16 | 127.84 |
| 2009 | 124.03 | 122.92 | 125.60 |
| 2010 | 126.54 | 127.02 | 126.25 |
| 2011 | 120.89 | 121.28 | 120.35 |
| 2012 | 121.34 | 125.82 | 115.34 |
| 2013 | 113.79 | 115.13 | 111.97 |
| 2014 | 114.32 | 116.58 | 111.06 |
| 2015 | 109.23 | 112.52 | 104.38 |
| 2016 | 106.99 | 109.74 | 102.92 |
| 2017 | 105.46 | 108.37 | 101.17 |
| 2018 | 111.13 | 113.13 | 107.73 |
| 2019 | 108.03 | 109.46 | 105.30 |
| 2020 | 108.00 | 110.71 | 103.43 |
| 2021 | 114.53 | 115.75 | 112.08 |
| 1st Period Trend | 2nd Period Trend | 3rd Period Trend | 4th Period Trend | |||||
|---|---|---|---|---|---|---|---|---|
| Year | APC (95% CI) | Year | APC (95% CI) | Year | APC (95% CI) | Year | APC (95% CI) | |
| All-cause | 2003−2005 | −9.8 (−12.3–−3.3) * | 2005−2017 | −2.3(−3.6–−1.1) * | 2017−2021 | 1.6 (−1.2–6.5) | ||
| Cardiovascular | 2003−2013 | −1.2 (−8.7–0.6) | 2013−2021 | 3.9 (1.3–14.0) * | ||||
| Noncardiovascular | 2003−2005 | −10.2 (−12.7–−4.0) | 2005−2017 | −2.7 (−3.9–−1.7) | 2017−2021 | 1.1 (−1.5–5.9) | ||
| Cause specific | ||||||||
| Ischemic heart disease | 2003−2021 | −0.5 (−1.4–0.4) | ||||||
| Heart failure | 2003−2009 | 30.1 (17.7–70.7) * | 2009−2012 | −15.3(−26.1–8.7) | 2012−2021 | 15.6 (7.3–50.5) * | ||
| Cerebrovascular disease | 2003−2012 | −5.1 (−13.6–−2.6) * | 2012−2021 | 2.3 (−0.4–12.2) | ||||
| Hyperkalemia/sudden death | 2003−2006 | −22.4 (−48.2–7.5) | 2006−2009 | 45.9 (15.4–75.1) * | 2009−2021 | 10.6 (−6.5–15.0) | ||
| Infection | 2003−2005 | 9.4 (1.9–15.5) * | 2005−2014 | −2.6 (−4.0–−1.8) * | 2014−2018 | 26.9 (23.3–30.8) * | 2018−2021 | 3.1 (−1.9–8.3) |
| Malignancy | 2003−2007 | −17.4 (−23.7–−13.3) * | 2007−2021 | −0.9 (−1.7–0.005) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, K.W.; Bae, Y.; Lee, J.Y.; Jo, Y.-I.; Cho, A. Mortality Trends in Patients Undergoing Hemodialysis, 2003–2021: Data from National Health Insurance Service in Korea. J. Clin. Med. 2025, 14, 2987. https://doi.org/10.3390/jcm14092987
Kim KW, Bae Y, Lee JY, Jo Y-I, Cho A. Mortality Trends in Patients Undergoing Hemodialysis, 2003–2021: Data from National Health Insurance Service in Korea. Journal of Clinical Medicine. 2025; 14(9):2987. https://doi.org/10.3390/jcm14092987
Chicago/Turabian StyleKim, Kyung Won, Yoonjong Bae, Jee Young Lee, Young-Il Jo, and AJin Cho. 2025. "Mortality Trends in Patients Undergoing Hemodialysis, 2003–2021: Data from National Health Insurance Service in Korea" Journal of Clinical Medicine 14, no. 9: 2987. https://doi.org/10.3390/jcm14092987
APA StyleKim, K. W., Bae, Y., Lee, J. Y., Jo, Y.-I., & Cho, A. (2025). Mortality Trends in Patients Undergoing Hemodialysis, 2003–2021: Data from National Health Insurance Service in Korea. Journal of Clinical Medicine, 14(9), 2987. https://doi.org/10.3390/jcm14092987






