Evaluation of Load and Stress Distribution for a Novel Design of Maxillary Protraction Facemask by Finite Element Analysis
Abstract
1. Introduction
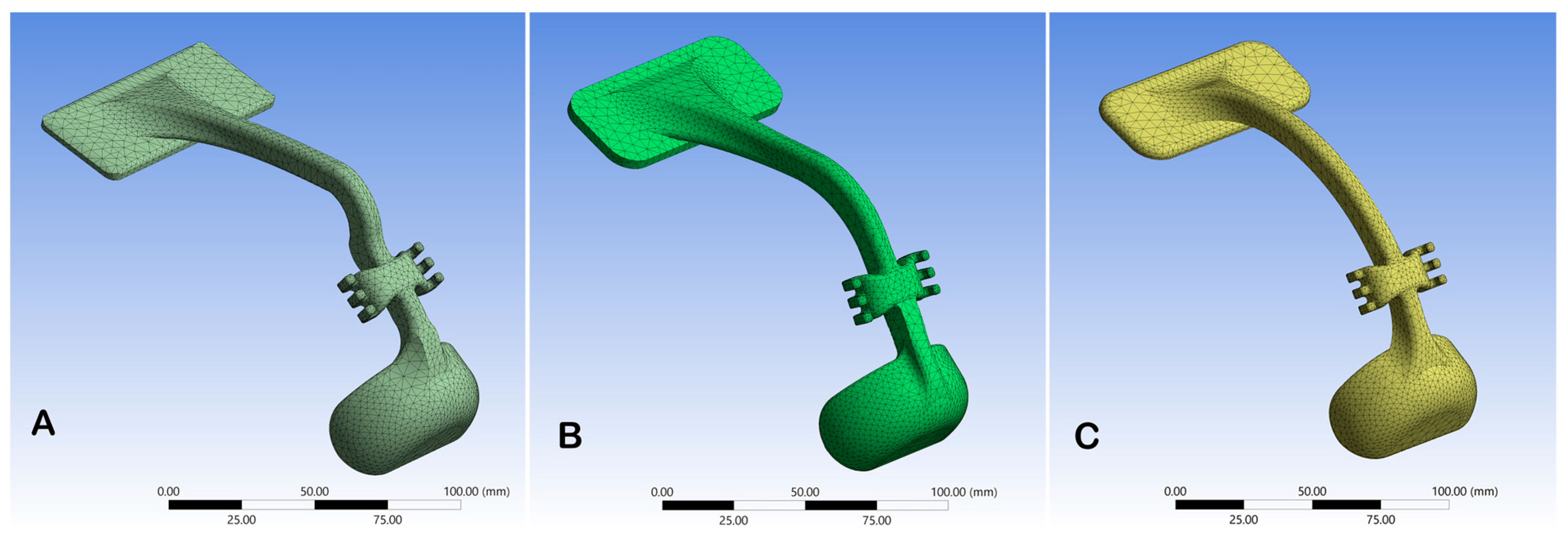
2. Material and Methods
- Geometrical features of the facemask, constructed by 3D modelling software (SOLIDWORKS (2023). Corp., Waltham, MA, USA);
- Material properties for all elements of the facemask, ABS;
- Meshing properties (sizes, shapes, and numbers of the elements used to discretize the facemask);
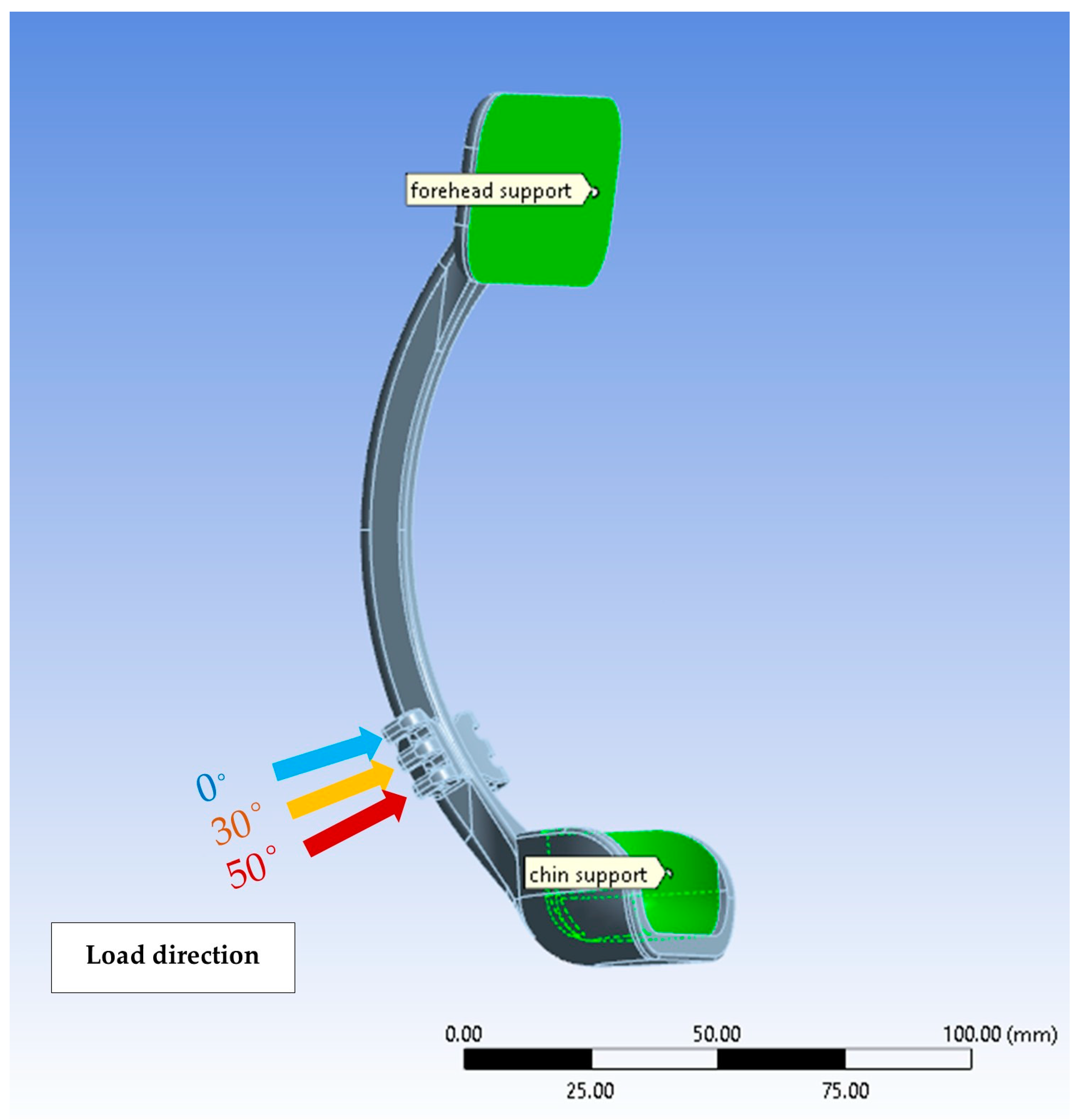
- Constraints and loads conditions applied on the system.
3. Ansys Simulations
4. Results
5. Discussion
6. Clinical Implications of the Study
7. Strength and Limitations
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nishitha, J.; Ahmad, M.H.; Walid, D.F. Skeletal Malocclusion: A Developmental Disorder with a Life-Long Morbidity. J. Clin. Med. Res. 2014, 6, 399–408. [Google Scholar] [CrossRef]
- Leck, R.; Paul, N.; Rolland, S.; Birnie, D. The consequences of living with a severe malocclusion: A review of the literature. J. Orthod. 2022, 49, 228–239. [Google Scholar] [CrossRef] [PubMed]
- Angelieri, F.; Franchi, L.; Cevidanes, L.; Hino, C.T.; Nguyen, T.; McNamara, J.A. Zygomaticomaxillary suture maturation: A predictor of maxillary protraction? Part I—A classification method. Orthod. Craniofac. Res. 2017, 20, 85–94. [Google Scholar] [CrossRef]
- Mandall, N.; Cousley, R.; DiBiase, A.; Dyer, F.; Littlewood, S.; Mattick, R.; Nute, S.J.; Doherty, B.; Stivaros, N.; McDowall, R.; et al. Early class III protraction facemask treatment reduces the need for orthognathic surgery: A multi-center, two-arm parallel randomized, controlled trial. J. Orthod. 2016, 43, 164–175. [Google Scholar] [CrossRef] [PubMed]
- Abid, M.; Al-Groosh, D.; Dziedzic, A.; Abed, H. Mothers’ knowledge and experience concerning presurgical orthopedic management for infants with cleft lip and palate. J. Orthod. Sci. 2021, 10, 8. [Google Scholar] [CrossRef]
- Woon, S.C.; Thiruvenkatachari, B. Early orthodontic treatment for Class III malocclusion: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 28–52. [Google Scholar] [CrossRef]
- Watkinson, S.; Harrison, J.E.; Furness, S.; Worthington, H.V. Orthodontic treatment for prominent lower front teeth (Class III malocclusion) in children. Cochrane Database Syst. 2013, 9. [Google Scholar] [CrossRef]
- Cordasco, G.; Matarese, G.; Rustico, L.; Fastuca, S.; Caprioglio, A.; Lindauer, S.J.; Nucera, R. Efficacy of orthopedic treatment with protraction facemask on skeletal Class III malocclusion: A systematic review and meta-analysis. Orthod. Craniofac. Res. 2014, 17, 133–143. [Google Scholar] [CrossRef]
- Abid, F.M.; Al-Attar, M.A.; Akram, A.F. Retention Protocols and Factors Affecting Retainer Choice among Iraqi Orthodontists. Int. J. Dent. 2020, 2020. [Google Scholar] [CrossRef]
- Toffol, L.D.; Pavoni, C.; Baccetti, T.; Franchi, L.; Cozza, P. Orthopedic treatment outcomes in Class III malocclusion. A systematic review. Angle Orthod. 2008, 78, 561–573. [Google Scholar] [CrossRef]
- Masucci, C.; Franchi, L.; Defraia, E.; Mucedero, M.; Cozza, P.; Baccetti, T. Stability of rapid maxillary expansion and facemask therapy: A long-term controlled study. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Mucedero, M.; Coviello, A.; Baccetti, T.; Franchi, L.; Cozza, P. Stability factors after double-jaw surgery in Class III malocclusion. A systematic review. Angle Orthod. 2008, 78, 1141–1152. [Google Scholar] [CrossRef] [PubMed]
- Pavoni, C.; Masucci, C.; Cerroni, S.; Franchi, L.; Cozza, P. Short-term effects produced by rapid maxillary expansion and facemask therapy in Class III patients with different vertical skeletal relationships. Angle Orthod. 2015, 85, 927–933. [Google Scholar] [CrossRef] [PubMed]
- Gazzani, F.; Pavoni, C.; Giancotti, A.; Cozza, P.; Lione, R. Facemask performance during maxillary protraction: A finite element analysis (FEA) evaluation of load and stress distribution on Delaire facemask. Prog. Orthod. 2018, 19, 21. [Google Scholar] [CrossRef]
- Abdulhussein, Z.A.; Aksoy, A. Compliance of patients with Class III malocclusion to orthodontic treatment. J. Bagh. Coll. Dent. 2022, 34, 12–24. [Google Scholar] [CrossRef]
- Billiet, T.; de Pauw, G.; Dermaut, L. Location of the center of resistance of the upper dentition and the nasomaxillary complex. An experimental study. Eur. J. Orthod. 2001, 23, 263–273. [Google Scholar] [CrossRef]
- Jain, S. Clinical Tip for Adjusting Reverse Pull Facemask/Headgear Assembly. J. Clin. Diagn. Res. 2016, 10, ZH01–ZH2. [Google Scholar] [CrossRef]
- Keles, A.; Tokmak, E.C.; Erverdi, N.; Nanda, R. Effect of varying the force direction on maxillary orthopedic protraction. Angle Orthod. 2002, 72, 387–396. [Google Scholar]
- Yepes, E.; Quintero, P.; Rueda, Z.V.; Pedroza, A. Optimal force for maxillary protraction facemask therapy in the early treatment of class III malocclusion. Eur. J. Orthod. 2014, 36, 586–594. [Google Scholar] [CrossRef]
- Zhao, Y.J.; Xiong, Y.X.; Wang, Y. Three-Dimensional Accuracy of Facial Scan for Facial Deformities in Clinics: A New Evaluation Method for Facial Scanner Accuracy. PLoS ONE 2017, 12, e0169402. [Google Scholar] [CrossRef]
- Kuhlman, D.C.; Almuzian, M.; Coppini, C.; Alzoubi, E.E. Accuracy (trueness and precision) of four tablet-based applications for three-dimensional facial scanning: An in-vitro study. J. Dent. 2023, 135, 104533. [Google Scholar] [CrossRef] [PubMed]
- AlSamarrai, F.F.; AlSheakli, I.I. Validity of Digital and Rapid Prototyped Orthodontic Study Models. J. Bagh. Coll. Dent. 2017, 29, 79–84. [Google Scholar] [CrossRef]
- Tsolakis, I.A.; Gizani, S.; Tsolakis, A.I.; Panayi, N. Three-Dimensional-Printed Customized Orthodontic and Pedodontic Appliances: A Critical Review of a New Era for Treatment. Children 2022, 9, 1107. [Google Scholar] [CrossRef] [PubMed]
- Laurence, W.M. Plastics Used in Medical Devices. In Handbook of Polymer Applications in Medicine and Medical Devices; Kayvon, M., Sina, E., Eds.; Elsevier: Oxford, UK, 2014; pp. 21–53. [Google Scholar] [CrossRef]
- Xiao, L.; Shimamura, N.; Kamio, T.; Ide, R.; Mochizuki, M.; Nakahara, T. Polycarbonate-Acrylonitrile Butadiene Styrene Three-Dimensional Printing Material Exhibits Biocompatibility and Enhances Osteogenesis and Gingival Tissue Formation with Human Cells. Cells 2025, 14, 167. [Google Scholar] [CrossRef]
- Tse, I.; Jay, A.; Na, I.; Murphy, S.; Niño-Martínez, N.; Martínez-Castañon, G.A.; Magrill, J.; Bach, H. Antimicrobial Activity of 3D-Printed Acrylonitrile Butadiene Styrene (ABS) Polymer-Coated with Silver Nanoparticles. Materials 2021, 14, 7681. [Google Scholar] [CrossRef]
- Ziąbka, M.; Dziadek, M.; Menaszek, E. Biocompatibility of Poly(acrylonitrile-butadiene-styrene) Nanocomposites Modified with Silver Nanoparticles. Polymers 2018, 10, 1257. [Google Scholar] [CrossRef]
- Odian, G. Principles of Polymerization, 4th ed.; Wiley: New York, NY, USA, 2004. [Google Scholar] [CrossRef]
- Rodriguez, J.; Thomas, J.; Renaud, J. Mechanical behavior of acrylonitrile butadiene styrene (ABS) fused deposition materials. Experimental investigation. Rapid Prototyp. J. 2001, 7, 148–158. [Google Scholar] [CrossRef]
- Matsuyama, Y.; Motoyoshi, M.; Tsurumachi, N.; Shimizu, N. Effects of palate depth, modified arm shape, and anchor screw on rapid maxillary expansion: A finite element analysis. Eur. J. Orthod. 2015, 37, 188–193. [Google Scholar] [CrossRef]
- Zhang, D.; Zheng, L.; Wang, Q.; Lu, L.; Ma, J. Displacements prediction from 3D finite element model of maxillary protraction with and without rapid maxillary expansion in a patient with unilateral cleft palate and alveolus. Biomed. Eng. Online 2015, 19, 80. [Google Scholar] [CrossRef]
- Gautam, P.; Valiathan, A.; Adhikari, R. Maxillary protraction with and without maxillary expansion: A finite element analysis of sutural stresses. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 361–366. [Google Scholar] [CrossRef]
- Yan, L.; Lim, J.L.; Lee, J.W.; Tia, C.S.H.; O’Neill, G.; Chong, D.Y.R. Finite element analysis of bone and implant stresses for customized 3D-printed orthopaedic implants in fracture fixation. Med. Biol. Eng. Comput. 2020, 58, 921–931. [Google Scholar] [CrossRef] [PubMed]
- ASTM D638-22; ASTM International. Standard Test Method for Tensile Properties of Plastics. ASTM International: West Conshohocken, PA, USA, 2022. Available online: https://www.astm.org/d0638-22.html (accessed on 7 April 2025).
- Letcher, T.; Rankouhi, B.; Javadpour, S. Experimental Study of Mechanical Properties of Additively Manufactured ABS Plastic as a Function of Layer Parameters. In Proceedings of the ASME 2015 International Mechanical Engineering Congress and Exposition, Houston, TX, USA, 13–19 November 2015; Volume 2A Advanced Manufacturing. [Google Scholar] [CrossRef]
- Cacciatore, G.; Poletti, L.; Ghislanzoni, L.T. A chairside customized chin cup. J. Clin. Orthod. 2013, 47, 352. [Google Scholar] [PubMed]
- Ierardo, G.; Luzzi, V.; Vozza, I.; Polimeni, A.; Bossù, M. Skin irritation from a facial mask in Class III malocclusion: Evaluation of individual silicone chin cups in a group of 100 children. Minerva Stomatol. 2018, 67, 45–48. [Google Scholar] [CrossRef]
- Turley, P.K. Orthopedic correction of Class III malocclusion with palatal expansion and custom protraction headgear. J. Clin. Orthod. 1988, 22, 314–325. [Google Scholar] [PubMed]
- Lee, N.K.; Yang, I.H.; Baek, S.H. The short-term treatment effects of face mask therapy in Class III patients based on the anchorage device: Miniplates vs rapid maxillary expansion. Angle Orthod. 2012, 82, 846–852. [Google Scholar] [CrossRef]
- Park, J.H.; Bayome, M.; Zahrowski, J.J.; Kook, Y.A. Displacement and stress distribution by different bone-borne palatal expanders with facemask: A 3-dimensional finite element analysis. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 105–117. [Google Scholar] [CrossRef]
- Vaughn, G.A.; Mason, B.; Moon, H.B.; Turley, P.K. The effects of maxillary protraction therapy with or without rapid palatal expansion: A prospective, randomized clinical trial. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 299–309. [Google Scholar] [CrossRef]

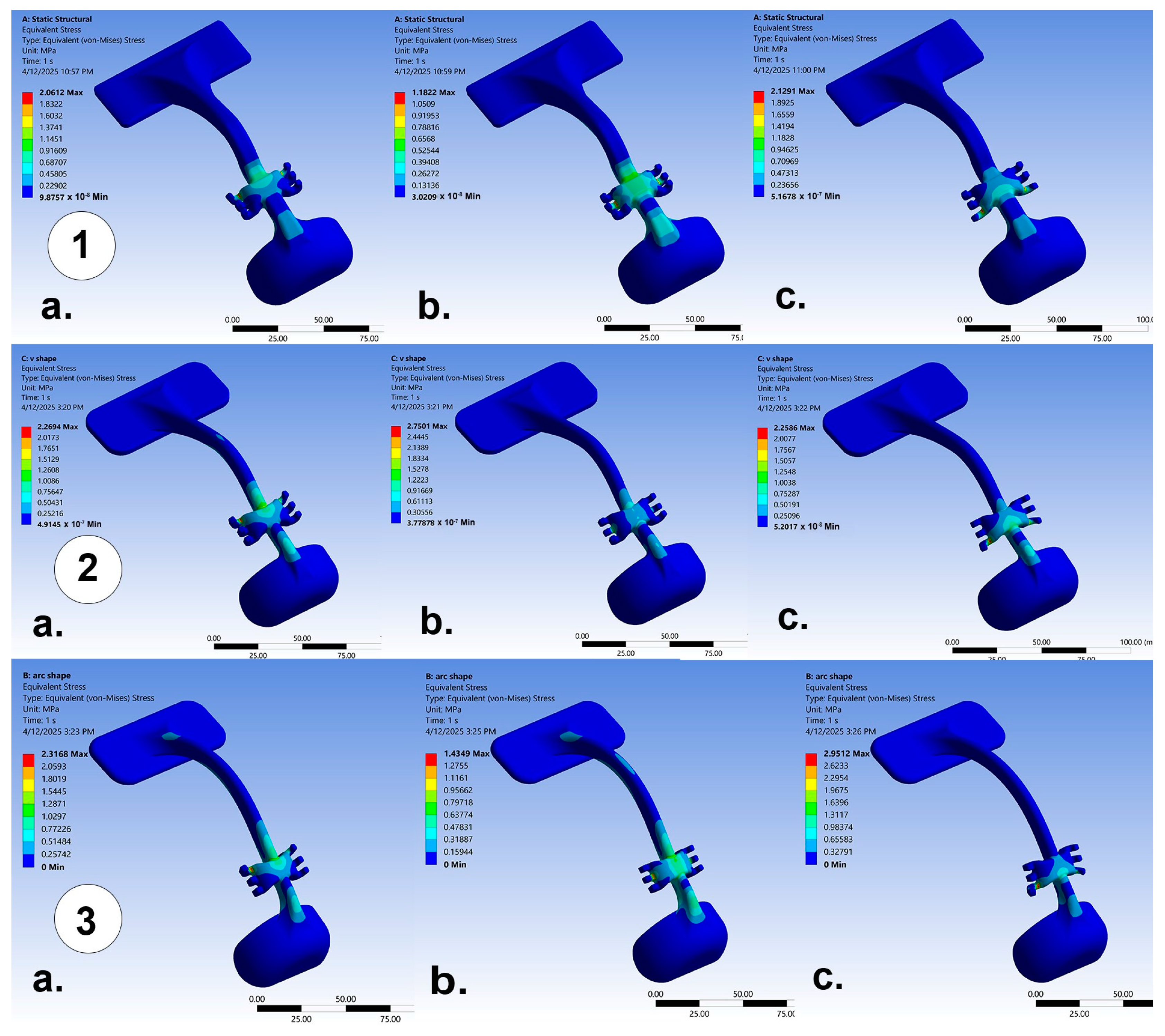
| Load Intensity (N) | 7.8 | 9.8 | ||||
|---|---|---|---|---|---|---|
| Angulations to Occlusal Plane | 0 | 30 | 50 | 0 | 30 | 50 |
| Anatomic | 1.27 | 0.97 | 1.29 | 1.6 | 1.22 | 1.63 |
| V-shape | 1.83 | 1.21 | 1.84 | 2.30 | 1.52 | 2.31 |
| Arc-shape | 1.87 | 1.11 | 2.48 | 2.35 | 1.38 | 3.11 |
| Load Intensity (N) | 7.8 | 9.8 | ||||
|---|---|---|---|---|---|---|
| Angulations to Occlusal Plane | 0 | 30 | 50 | 0 | 30 | 50 |
| Anatomic | 5.23 × 10−4 | 3.84 × 10−4 | 5.39 × 10−4 | 6.57 × 10−4 | 4.83 × 10−4 | 6.77 × 10−4 |
| V-shape | 7.47 × 10−4 | 6.12 × 10−4 | 7.45 × 10−4 | 9.39 × 10−4 | 7.69 × 10−4 | 9.36 × 10−4 |
| Arc-shape | 7.59 × 10−4 | 4.56 × 10−4 | 9.61 × 10−4 | 9.54 × 10−4 | 5.70 × 10−4 | 12.07 × 10−4 |
| Load Intensity (N) | 7.8 | 9.8 | ||||
|---|---|---|---|---|---|---|
| Angulations to Occlusal Plane | 0 | 30 | 50 | 0 | 30 | 50 |
| Anatomic | 2.15 × 10−2 | 1.53 × 10−2 | 1.37 × 10−2 | 2.70 × 10−2 | 1.93 × 10−2 | 1.73 × 10−2 |
| V-shape | 2.99 × 10−2 | 1.77 × 10−2 | 2.09 × 10−2 | 3.76 × 10−2 | 2.23 × 10−2 | 2.63 × 10−2 |
| Arc-shape | 3.16 × 10−2 | 1.95 × 10−2 | 2.35 × 10−2 | 3.97 × 10−2 | 2.38 × 10−2 | 2.96 × 10−2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdulkareem, G.B.; Cobourne, M.T.; Abid, M. Evaluation of Load and Stress Distribution for a Novel Design of Maxillary Protraction Facemask by Finite Element Analysis. J. Clin. Med. 2025, 14, 2676. https://doi.org/10.3390/jcm14082676
Abdulkareem GB, Cobourne MT, Abid M. Evaluation of Load and Stress Distribution for a Novel Design of Maxillary Protraction Facemask by Finite Element Analysis. Journal of Clinical Medicine. 2025; 14(8):2676. https://doi.org/10.3390/jcm14082676
Chicago/Turabian StyleAbdulkareem, Ghassan Bahir, Martyn T. Cobourne, and Mushriq Abid. 2025. "Evaluation of Load and Stress Distribution for a Novel Design of Maxillary Protraction Facemask by Finite Element Analysis" Journal of Clinical Medicine 14, no. 8: 2676. https://doi.org/10.3390/jcm14082676
APA StyleAbdulkareem, G. B., Cobourne, M. T., & Abid, M. (2025). Evaluation of Load and Stress Distribution for a Novel Design of Maxillary Protraction Facemask by Finite Element Analysis. Journal of Clinical Medicine, 14(8), 2676. https://doi.org/10.3390/jcm14082676






