Impact of the Recanalization Level and the First-Pass Effect on Functional Outcomes in Patients After M2 MCA Occlusion Thrombectomy
Abstract
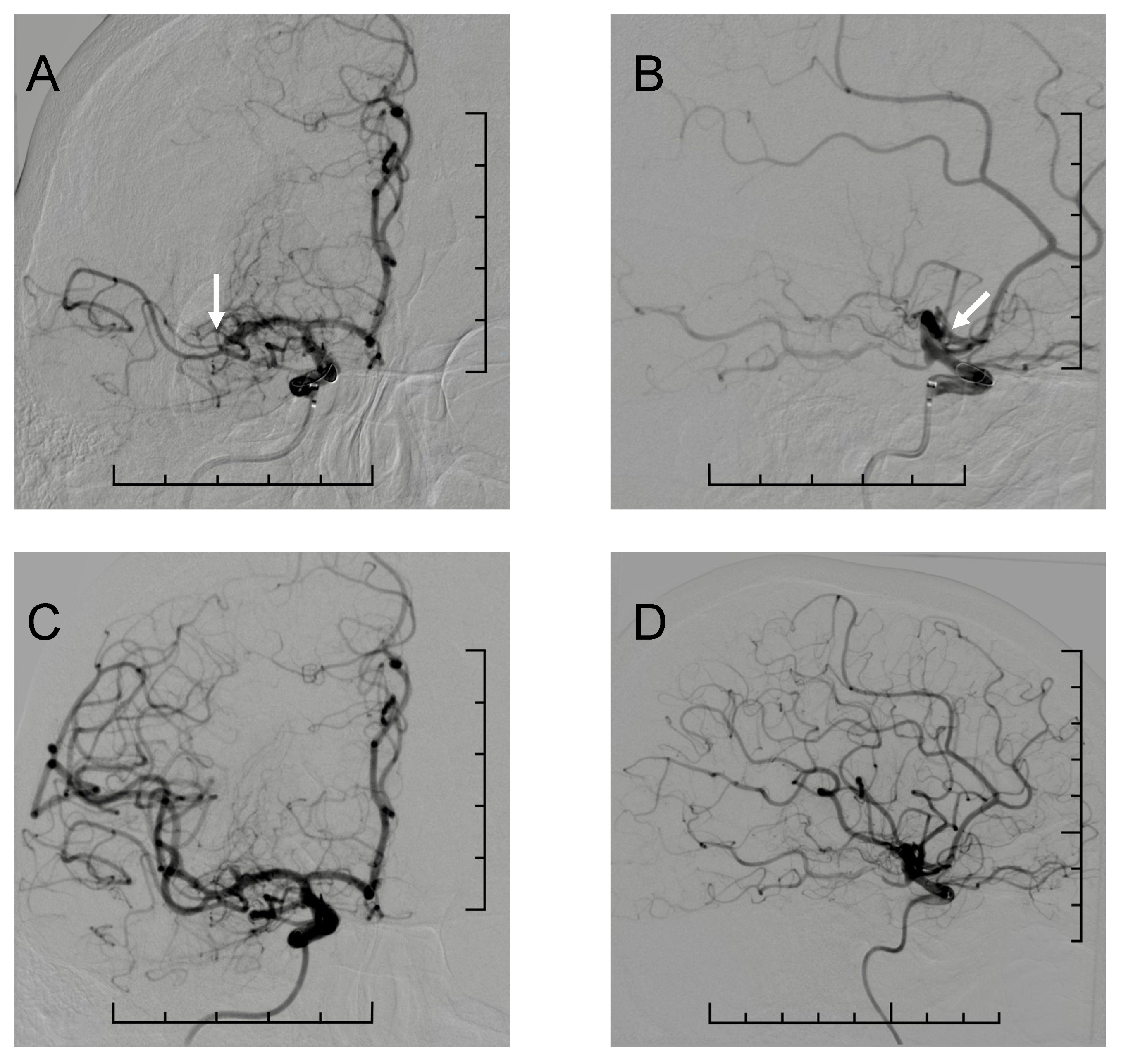
1. Introduction
Distal and Medium Vessel Occlusion
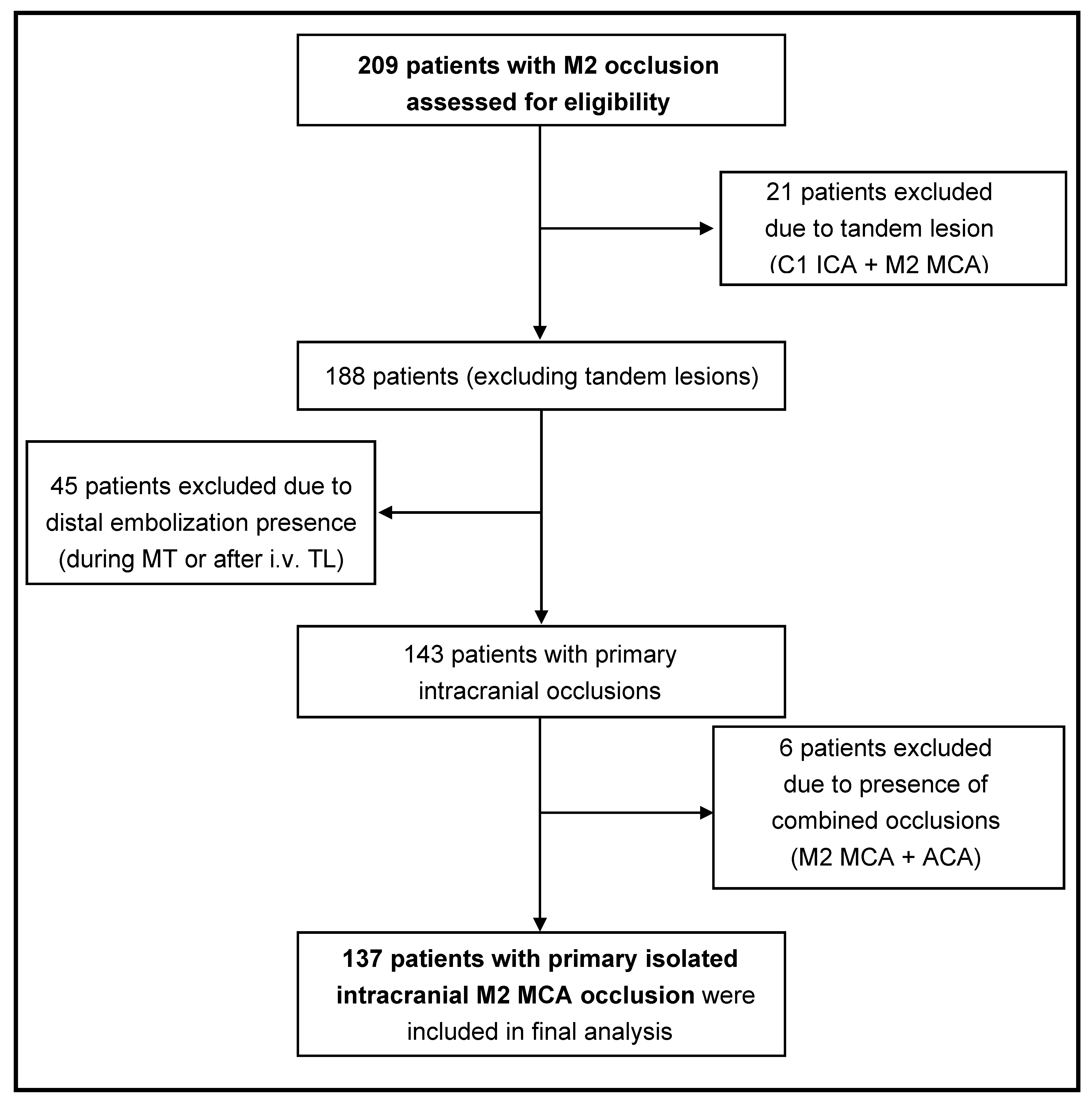
2. Methods
2.1. Study Design and Oversight
2.2. Participants
2.3. Interventional Procedures
- Local anesthesia.
- Monitored anesthetic care (conscious sedation administered by an anesthesiology team), which can be beneficial for the patient, especially because of more stable blood pressure levels, the possibility of continuously monitoring neurological status and a shorter time to recanalization. On the other hand, sedative agents may potentially compromise the patient’s airway. As these are emergency cases, there is a risk of aspiration. Also, the involuntary movement of the patient may prolong the procedure.
- General anesthesia [17].
2.4. Measures
2.5. Outcomes
2.6. Statistical Analysis
3. Results
3.1. Basic Epidemiological Parameters
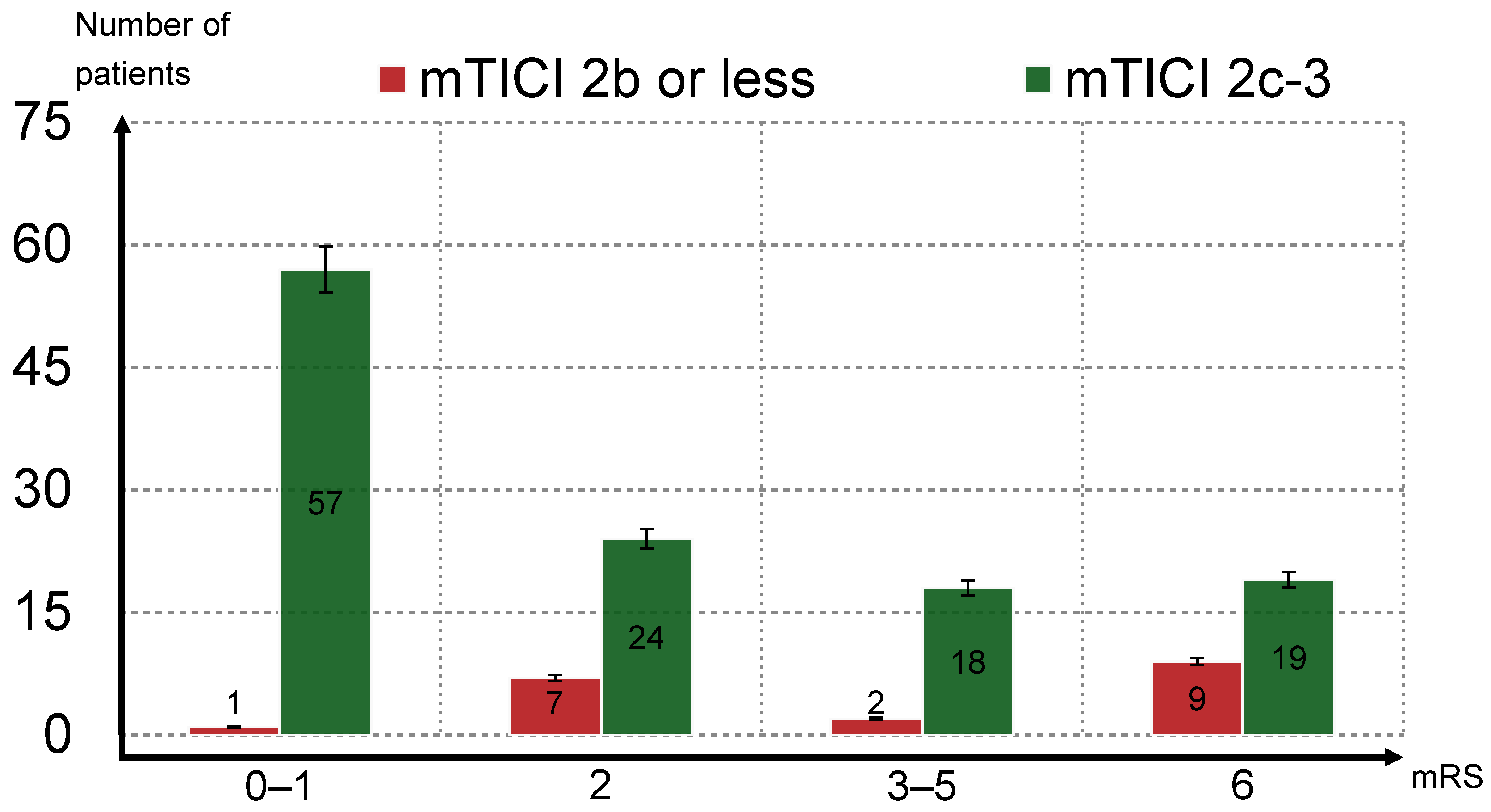
3.2. Primary and Secondary Outcomes
3.3. Safety Outcomes
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American heart association/American stroke association. Stroke 2019, 50, e344–e418. [Google Scholar] [CrossRef] [PubMed]
- Goyal, N.; Tsivgoulis, G.; Frei, D.; Turk, A.; Baxter, B.; Froehler, M.T.; Mocco, J.; Ishfaq, M.F.; Malhotra, K.; Chang, J.J.; et al. Comparative safety and efficacy of modified TICI 2b and TICI 3 reperfusion in acute ischemic strokes treated with mechanical thrombectomy. Neurosurgery 2018, 83, 593. [Google Scholar] [CrossRef] [PubMed]
- Chamorro, Á.; Blasco, J.; López, A.; Amaro, S.; Román, L.S.; Llull, L.; Renú, A.; Rudilosso, S.; Laredo, C.; Obach, V.; et al. Complete reperfusion is required for maximal benefits of mechanical thrombectomy in stroke patients. Sci. Rep. 2017, 7, 11636. [Google Scholar] [CrossRef]
- Dargazanli, C.; Fahed, R.; Blanc, R.; Gory, B.; Labreuche, J.; Duhamel, A.; Marnat, G.; Costalat, V.; Bracard, S.; Desal, H.; et al. Modified thrombolysis in cerebral infarction 2c/thrombolysis in cerebral infarction 3 reperfusion should be the aim of mechanical thrombectomy: Insights from the ASTER Trial (contact aspiration versus stent retriever for successful revascularization). Stroke 2018, 49, 1189–1196. [Google Scholar] [CrossRef]
- Zaidat, O.O.; Castonguay, A.C.; Linfante, I.; Gupta, R.; Martin, C.O.; Holloway, W.E.; Mueller-Kronast, N.; English, J.D.; Dabus, G.; Malisch, T.W.; et al. First pass effect: A new measure for stroke thrombectomy devices. Stroke 2018, 49, 660–666. [Google Scholar] [CrossRef]
- Nikoubashman, O.; Dekeyzer, S.; Riabikin, A.; Keulers, A.; Reich, A.; Mpotsaris, A.; Wiesmann, M. True first-pass effect. Stroke 2019, 50, 2140–2146. [Google Scholar] [CrossRef]
- Zaidat, O.O.; Ribo, M.; Mattle, H.P.; Saver, J.L.; Bozorgchami, H.; Yoo, A.J.; Ehm, A.; Kottenmeier, E.; Cameron, H.L.; Qadeer, R.A.; et al. Health economic impact of first-pass success among patients with acute ischemic stroke treated with mechanical thrombectomy: A United States and European perspective. J. NeuroInterv. Surg. 2020, 21, 016930. [Google Scholar] [CrossRef]
- Savel, J.L.; Chapot, R.; Acid, R.; Hassan, A.; Jadhav, A.P.; Liebeskind, D.S.; Lobotesis, K.; Meila, D.; Meyer, L.; Raphaeli, G.; et al. Distal Thrombectomy Summit Group. Thrombectomy for distal medium vessel occlusions: A consensus treatment on present knowledge and promising directions. Stroke 2020, 51, 2872–2884. [Google Scholar] [CrossRef]
- Nakano, T.; Shigeta, K.; Ota, T.; Amano, T.; Ueda, M.; Matsumara, Y.; Shiokawa, Y.; Hirano, T. Efficacy and Safety of mechanical thrombevctomy for occlusion of the second segment of the middle cerebral artery: Retrospective analysis of the Tama-REgistry of Acute endovascular Thrombectomy (TREAT). Clin. Neuroradiol. 2020, 30, 481–487. [Google Scholar] [CrossRef]
- Munich, S.A.; Vakharia, K.; Levy, E.I. Overview of Mechanical Thrombectomy Techniques. Neurosurgery 2019, 85 (Suppl. S1), S60–S67. [Google Scholar] [CrossRef]
- Menon, B.K.; Hill, M.D.; Davalos, A.; Roos, Y.B.W.E.M.; Campbell, B.C.V.; Dippel, D.W.J.; Guillemin, F.; Saver, J.L.; van der Lugt, A.; Demchuk, A.M.; et al. Efficacy of endovascular thrombectomy in patients with 2 segment middle cerebral artery occlusions: Meta-analysis of data from the HERMES collaboration. J Neurointerv. Surg. 2019, 11, 1065–1069. [Google Scholar] [CrossRef] [PubMed]
- Almekhlafi, M.; Ospel, J.M.; Saposnik, G.; Kasha, N.; Demchuk, A.; Hill, M.D.; Goyal, M.; Menon, B.K. Endovascular Treatment Decisions in Patients with M2 Segment MCA Occlusions AJNR. Am. J. Neuroradiol. 2020, 41, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Kneip, H.; Meyer, L.; Broocks, G.; Fazit, T.D.; Bechstein, M.; Brekenfeld, C.; Flottmann, F.; van Horn, N.; Geest, V.; Winkelmeier, L.; et al. German Stroke Registry-Endovascular Treatment (GSR-ET), Thrombectomy in M2 occlusion compared to M1 occlusion: Treatment effects of Thrombolysis In Cerebral Infarction (TICI) 2b and TICI 3 recanalization on functional outcome. Neurointerv. Surg. 2023, 15, e438–e445. [Google Scholar] [CrossRef] [PubMed]
- Aoki, J.; Suzuki, K.; Kanamru, T.; Katano, T.; Kutsuna, A.; Sakamoto, Y.; Suda, S.; Nishiyama, Y.; Morita, N.; Harada, M.; et al. Impact of complete recanalisation on clinical recovery in cardioembolic stroke stroke patients with M2 occlusion. J. Neurol. Sci. 2020, 415, 116873. [Google Scholar] [CrossRef]
- Joseph, P.B.; Opeolu, A.; Jordan, E. The Evolution of the Modified Rankin Scale and Its Use in Future Stroke Trials. Stroke 2017, 48, 2007–2012. [Google Scholar] [CrossRef]
- Almekhlafi, M.A.; Mishra, S.; Dean, J.A.; Nambiar, V.; Nolan, O.; Goes, A.; Eesa, M.; Demchuk, A.M.; Menon, B.K.; Goyal, M. Not all “successful” angiographic reperfusion patients are an equal validation of a modified TICI scoring system. Interv. Neuroradiol. 2014, 20, 21–27. [Google Scholar] [CrossRef]
- Wijayatilake, D.S.; Ratnayake, G.; Ragavan, D. Anaesthesia for neuroradiology: Thrombectomy: ‘One small step for man, one giant leap for anaesthesia’. Curr. Opin. Anaesthesiol. 2016, 29, 568–575. [Google Scholar] [CrossRef]
- Kniep, H.; Meyer, L.; Broocks, G.; Bechstein, M.; Heitkamp, C.; Winkelmeier, L.; Faizy, T.; Brekenfeld, C.; Flottmann, F.; Deb-Chatterji, M.; et al. German Stroke Registry-Endovascular Treatment (GSR-ET), Thrombectomy for M2 Occlusions: Predictors of Successful and Futile Recanalization. Stroke 2023, 54, 2002–2012. [Google Scholar] [CrossRef]
- Barber, P.A.; Demchuk, A.M.; Zhang, J.; Buchan, A.M. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. Lancet 2000, 355, 1670–1674. [Google Scholar] [CrossRef]
- Tan, I.Y.L.; Demchuk, A.M.; Hopyan, J.; Zhang, L.; Gladstone, D.; Wong, K.; Martin, M.; Symons, S.P.; Fox, A.J.; Aviv, R.I. CT angiography clot burden score and collateral score: Correlation with clinical and radiologic outcomes in acute middle cerebral artery infarct. JNR Am. J. Neuroradiol. 2009, 30, 525–531. [Google Scholar] [CrossRef]
- Mazya, M.D.; Egido, J.A.; Ford, G.A.; Lees, K.R.; Mikulik, R.; Toni, D.; Wahlgren, N.; Ahmed, N. Predicting the Risk of Symptomatic Intracerebral Hemorrhage in Ischemic Stroke Treated With Intravenous Alteplase: Safe Implementation of Treatments in Stroke (SITS) Symptomatic Intracerebral Hemorrhage Risk Score Michael. Stroke 2012, 43, 6. [Google Scholar] [CrossRef]
- Saber, H.; Narayanan, S.; Palla, M.; Saver, J.L.; Nogueira, R.G.; Yoo, A.J.; Sheth, S.A. Mechanical thrombectomy for acute ischemic stroke with occlusion of the M2 segment of the middle cerebral artery: A meta-analysis. J. Neurointerv. Surg. 2018, 10, 620–624. [Google Scholar] [CrossRef] [PubMed]
- Sarraj, A.; Parsons, M.; Bivar, A.; Do, A.E.H.; Abraham, M.G.; Wu, T.; Kleinig, T.; Lin, L.; Chen, C.; Levi, C.; et al. Endovascular Thrombectomy Versus Medical Management in Isolated M2 Occlusions: Pooled Patient-Level Analysis from the EXTEND-IA Trials, INSPIRE, and SELECT Studies. Ann. Neurol. 2022, 91, 629–639. [Google Scholar] [CrossRef] [PubMed]
- Sheth, S.A.; Yoo, B.; Saver, J.L.; Starkman, S.; Ali, L.K.; Kim, D.; Gonzalez, N.R.; Jahan, R.; Tateshima, S.; Duckwiler, G.; et al. M2 occlusions as targets for endovascular therapy: Comprehensive analysis of diffusion/perfusion MRI, angiography, and clinical outcomes. J. Neurointerv. Surg. 2015, 7, 478–483. [Google Scholar] [CrossRef] [PubMed]
- Dargazanli, C.; Consoli, A.; Barral, M.; Labreuche, J.; Redjem, H.; Ciccio, G.; Smajda, S.; Desilles, J.; Taylor, G.; Preda, C.; et al. Impact of modified TICI 3 versus modified TICI 2b reperfusion score to predict good outcome following endovascular therapy. AJNR Am. J. Neuroradiol. 2017, 38, 90–96. [Google Scholar]
- Kleine, J.F.; Wunderlich, S.; Zimmer, C.; Kaesmacher, J. Time to redefine success? TICI 3 versus TICI 2b recanalization in middle cerebral artery occlusion treated with thrombectomy. J. Neurointerv. Surg. 2017, 9, 117–121. [Google Scholar] [CrossRef]
- Kaesmacher, J.; Dobrocky, T.; Heldner, M.R.; Bellwald, S.; Mosimann, P.J.; Mordasini, P.; Bigi, S.; Arnold, M.; Gralla, J.; Fischer, U. Systematic review and meta-analysis on outcome differences among patients with TICI2b versus TICI3 reperfusions: Success revisited. J. Neurol. Neurosurg. Psychiatry 2018, 89, 910–917. [Google Scholar]
- Maier, I.L.; Almallouhi, E.; Psychogios, M.N.; Liman, J.; Al Kasab, S.; Alawieh, A.; Chalhoub, R.; Wolfe, S.; Arthur, A.; Shaban, A.; et al. Importance of First Pass Reperfusion in Endovascular Stroke Care—Insights From Thrombectomy and Aneurysm Registry (STAR). Stroke Vasc. Interv. Neurol. 2022, 2, 6. [Google Scholar] [CrossRef]
- Muszynski, P.; Anadani, M.; Richard, S.; Marnat, G.; Bourcier, R.; Sibon, I.; Dargazanli, C.; Arquizan, C.; Maïer, B.; Blanc, R.; et al. Endovascular reperfusion of M2 occlusions in acute ischemic stroke reduced disability and mortality: ETIS Registry results. J. Neurointerv. Surg. 2022, 14, 017380. [Google Scholar] [CrossRef]
- Goyal, M.; Demchuk, A.M.; Menon, B.K.; Eesa, M.; Rempel, J.L.; Thornton, J.; Roy, D.; Jovin, T.G.; Willinsky, R.A.; Sapkota, B.L.; et al. Randomized Assessment of Rapid Endovascular Treatment of Ischemic Stroke. N. Engl. J. Med. 2015, 372, 1019–1030. [Google Scholar] [CrossRef]
- Albers, G.W.; Marks, M.P.; Kemp, S.; Christensen, S.; Tsai, J.P.; Ortega-Gutierrez, S.; McTaggart, R.A.; Torbey, M.T.; Kim-Tenser, M.; Leslie-Mazwi, T.; et al. Thrombectomy for Stroke at 6 to 16 Hours with Selection by Perfusion Imaging. N. Engl. J. Med. 2018, 378, 708–718. [Google Scholar] [CrossRef] [PubMed]
- Dasic, D.; Morgan, L.; Panezai, A.; Syrmos, N.; Ligarotti, G.K.I.; Zaed, I.; Chibbaro, S.; Khan, T.; Prisco, L.; Ganau, M. A scoping review on the challenges, improvement programs, and relevant output metrics for neurotrauma services in major trauma centers. Surg. Neurol. Int. 2022, 13, 171. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Treurniet, K.M.; Jansen, I.G.H.; Emmer, B.J.; van den Berg, R.; Marquering, H.A.; Uyttenboogaart, M.; Jenniskens, S.F.M.; Roos, Y.B.W.E.M.; van Doormaal, P.J.; et al. Majoie CBLM for the MR CLEAN Registry Investigators, Operator Versus Core Lab Adjudication of Reperfusion After Endovascular Treatment of Acute Ischemic Stroke. Stroke 2018, 49, 10. [Google Scholar] [CrossRef]
| Parameter | First-Pass mTICI 2c–3 (n = 63) | Non-First-Pass mTICI 2c–3 (n = 74) | p Value |
|---|---|---|---|
| % | 46 | 54 | |
| Males (%) | 29 (46) | 30 (40.5) | 0.764 |
| Females (%) | 34 (54) | 34 (59.1) | |
| Age (mean ± SD) | 70.6 ± 12.5 | 72.6 ± 11.1 | 0.467 |
| Admission NIHSS (median) | 11.5 | 10.0 | |
| Arterial hypertension (%) | 51 (81) | 65 (87.8) | 0.269 |
| Atrial fibrillation (%)—including primo-manifestation | 32 (50.8) | 38 (51.4) | 0.567 |
| Diabetes mellitus (%) | 13 (20.6) | 18 (24.3) | 0.772 |
| Wake-up stroke (%) | 8 (12.7) | 13 (17.6) | 0.430 |
| i.v. Thrombolysis (%) | 28 (44.4) | 24 (32.4) | 0.149 |
| ASPECTS score (mean ± SD/median) | 9.4 ± 1.0/10 | 9.4 ± 1.0/10 | |
| Collateral score (mean ± SD/median) | 2.2 ± 0.5/2 | 2.2 ± 0.6/2 | |
| M2 dominant branch (%) | 26 (41.3) | 37 (50) | 0.307 |
| Parameter | mTICI 2b or Less (n = 19) | mTICI 2c–3 (n = 118) | p Value |
|---|---|---|---|
| mRS 0–2 (%) | 8 (42.1) | 81 (68.6) | 0.024 |
| mRS 0–1 (%) | 1 (5.3) | 57 (48.3) | <0.001 |
| Mortality = mRS 6 (%) | 9 (47.4) | 19 (16.1) | 0.002 |
| Any ICH (%) | 6 (31.6) | 36 (30.5) | 0.925 |
| Symptomatic ICH (%) | 1 (5.3) | 4 (3.4) | 0.686 |
| Parameter | First-Pass mTICI 2c–3 (n = 63) | Non-First-Pass mTICI 2c–3 (n = 74) | p Value |
|---|---|---|---|
| mRS 0–2 (%) | 39 (61.9) | 50 (67.6) | 0.489 |
| mRS 0–1 (%) | 31 (49.2) | 27 (36.5) | 0.133 |
| Mortality = mRS 6 (%) | 12 (19.1) | 16 (21.6) | 0.710 |
| Any ICH (%) | 17 (27) | 25 (33.8) | 0.390 |
| Symptomatic ICH (%) | 3 (4.8) | 2 (2.7) | 0.522 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pataky, S.; Fedorko, J.; Pedowski, P.; Skorvanek, M.; Gdovinova, Z. Impact of the Recanalization Level and the First-Pass Effect on Functional Outcomes in Patients After M2 MCA Occlusion Thrombectomy. J. Clin. Med. 2025, 14, 2563. https://doi.org/10.3390/jcm14082563
Pataky S, Fedorko J, Pedowski P, Skorvanek M, Gdovinova Z. Impact of the Recanalization Level and the First-Pass Effect on Functional Outcomes in Patients After M2 MCA Occlusion Thrombectomy. Journal of Clinical Medicine. 2025; 14(8):2563. https://doi.org/10.3390/jcm14082563
Chicago/Turabian StylePataky, Stefan, Jakub Fedorko, Piotr Pedowski, Matej Skorvanek, and Zuzana Gdovinova. 2025. "Impact of the Recanalization Level and the First-Pass Effect on Functional Outcomes in Patients After M2 MCA Occlusion Thrombectomy" Journal of Clinical Medicine 14, no. 8: 2563. https://doi.org/10.3390/jcm14082563
APA StylePataky, S., Fedorko, J., Pedowski, P., Skorvanek, M., & Gdovinova, Z. (2025). Impact of the Recanalization Level and the First-Pass Effect on Functional Outcomes in Patients After M2 MCA Occlusion Thrombectomy. Journal of Clinical Medicine, 14(8), 2563. https://doi.org/10.3390/jcm14082563






