Sacubitril/Valsartan Improves Hemodynamic Parameters of Pulmonary and Systemic Circulation in Patients Awaiting Heart Transplantation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population, Measured Parameters
2.2. Right Heart Catheterization
2.3. Statistics
3. Results
3.1. Patient Characteristics
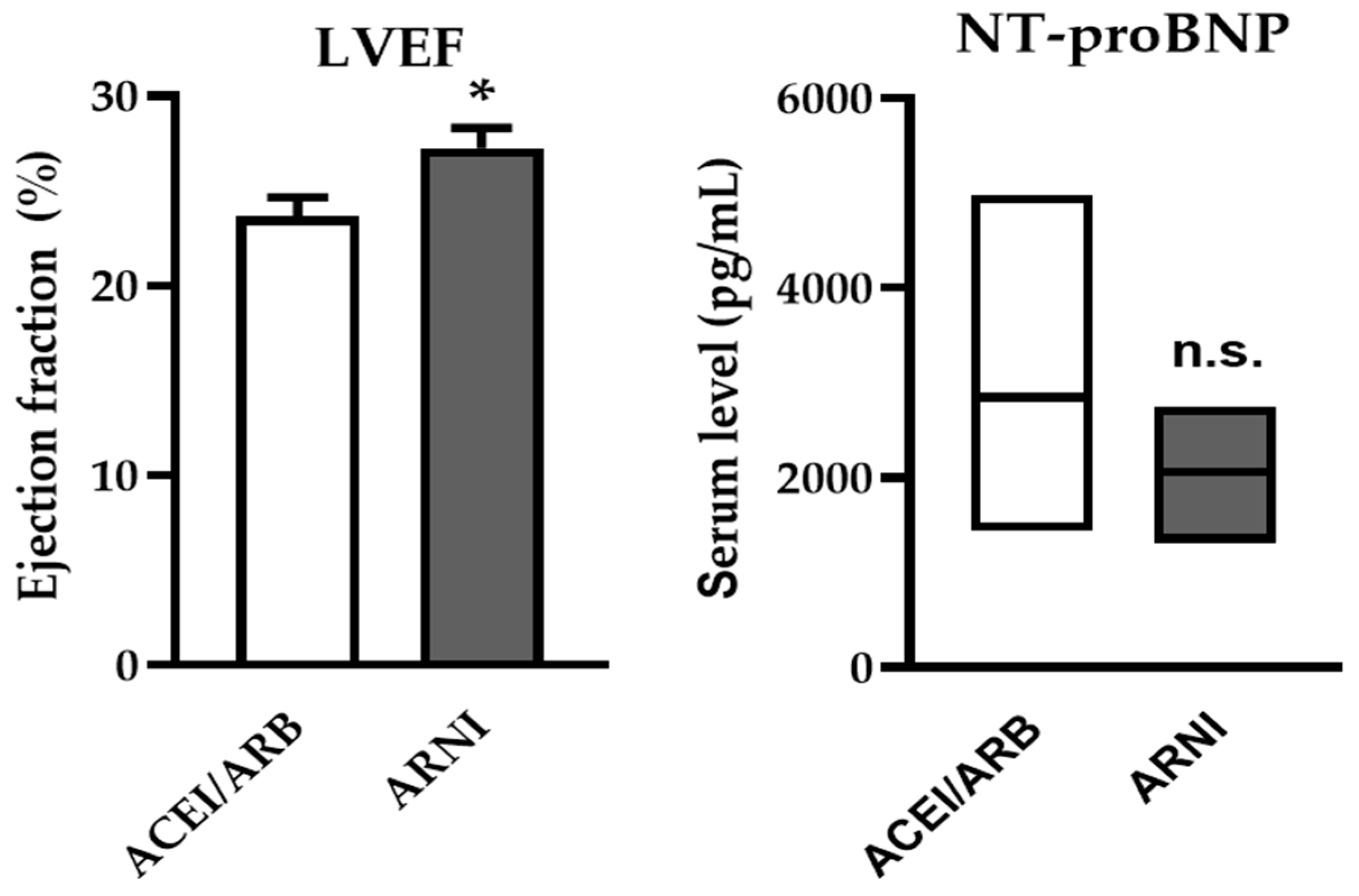
3.2. Effectiveness and Safety of ARNI—Changes in NYHA Class, LVEF and NT-proBNP
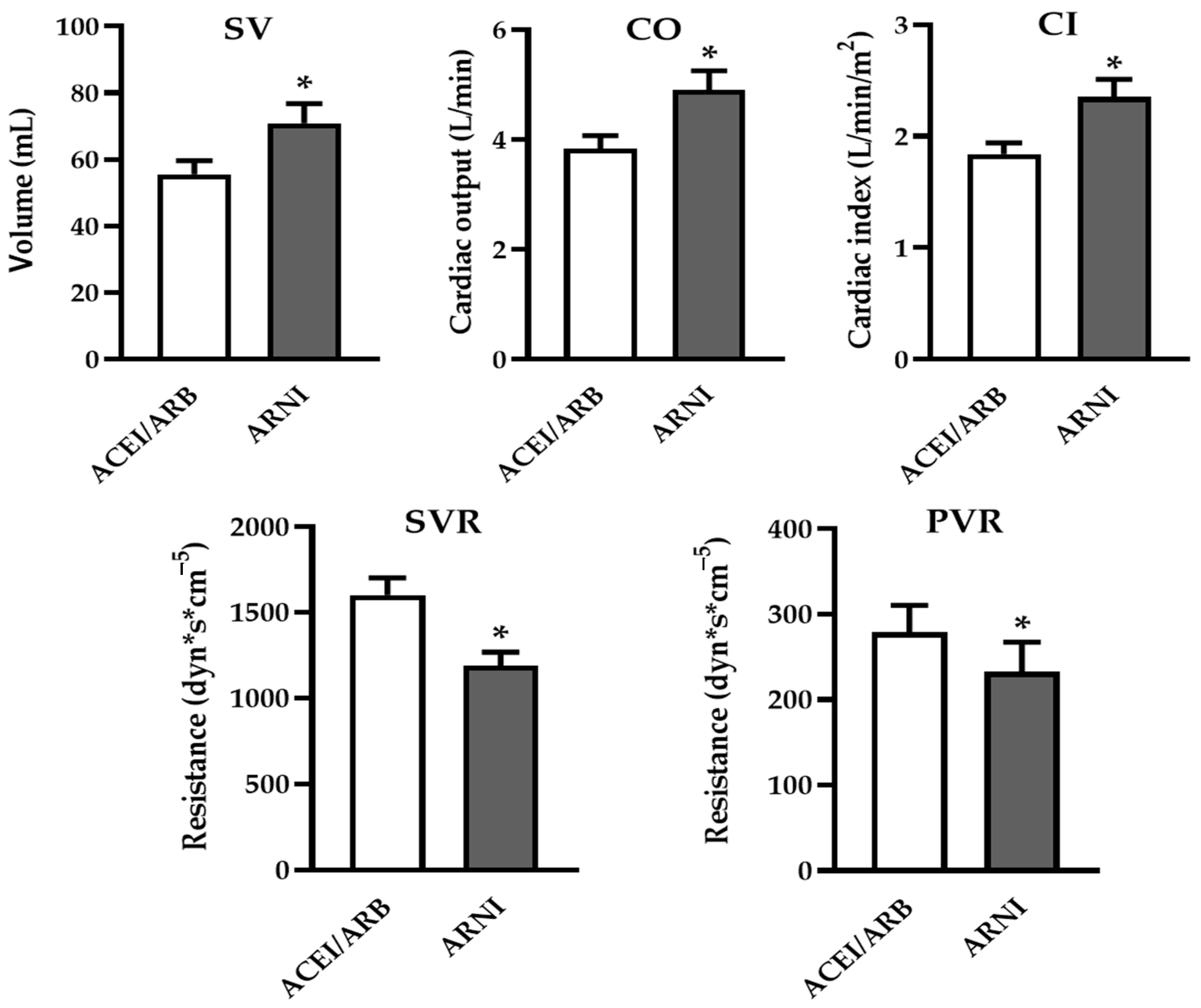
3.3. ARNI Significantly Improved Hemodynamic Parameters of Both Systemic and Pulmonary Circulation
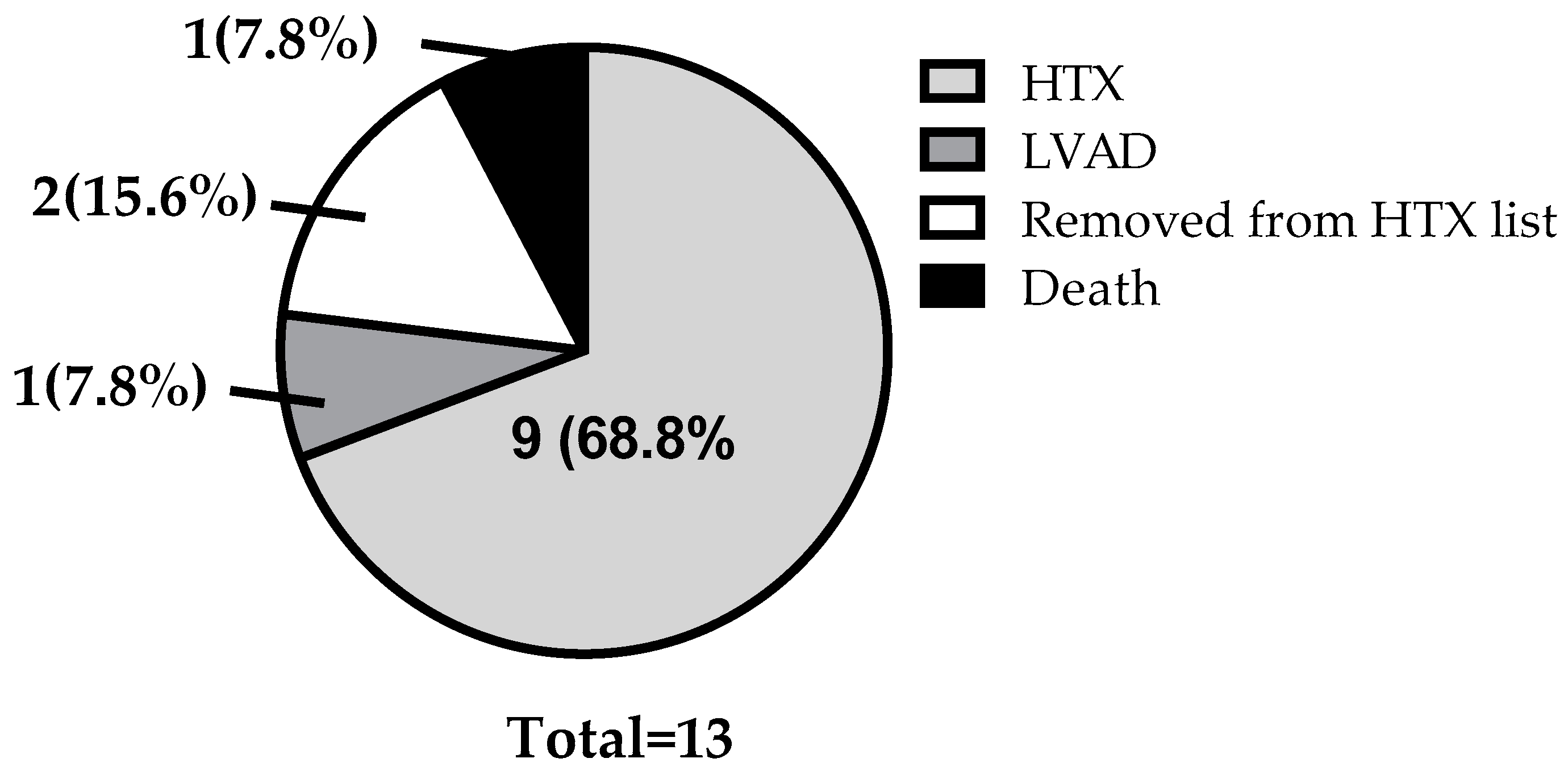
3.4. Clinical Outcomes
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Savarese, G.; Becher, P.M.; Lund, L.H.; Seferovic, P.; Rosano, G.M.C.; Coats, A.J.S. Global Burden of Heart Failure: A Comprehensive and Updated Review of Epidemiology. Cardiovasc. Res. 2023, 118, 3272–3287. [Google Scholar] [CrossRef]
- Berliner, D.; Bauersachs, J. New Drugs: Big Changes in Conservative Heart Failure Therapy? Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2019, 55, i3–i10. [Google Scholar] [CrossRef]
- Bauersachs, J. Heart Failure Drug Treatment: The Fantastic Four. Eur. Heart J. 2021, 42, 681–683. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- McMurray, J.J.V.; Packer, M.; Desai, A.S.; Gong, J.; Lefkowitz, M.P.; Rizkala, A.R.; Rouleau, J.L.; Shi, V.C.; Solomon, S.D.; Swedberg, K.; et al. Angiotensin-Neprilysin Inhibition versus Enalapril in Heart Failure. N. Engl. J. Med. 2014, 371, 993–1004. [Google Scholar] [CrossRef] [PubMed]
- Kuchulakanti, P.K. ARNI in Cardiovascular Disease: Current Evidence and Future Perspectives. Future Cardiol. 2020, 16, 505–515. [Google Scholar] [CrossRef] [PubMed]
- Bhat, T.S.; Hafeez, I.; Tak, S.F.; Mattoo, A.; Patigaroo, A.R.; Khan, A.; Lone, A.A.; Beig, J.R. Safety and Efficacy of ARNI (Valsartan/Sacubitril) vs ACEI (Enalapril) in Acute Heart Failure—A Prospective Observational Study. Indian Heart J. 2022, 74, 178–181. [Google Scholar] [CrossRef]
- Lewis, E.F.; Claggett, B.L.; McMurray, J.J.V.; Packer, M.; Lefkowitz, M.P.; Rouleau, J.L.; Liu, J.; Shi, V.C.; Zile, M.R.; Desai, A.S.; et al. Health-Related Quality of Life Outcomes in PARADIGM-HF. Circ. Heart Fail. 2017, 10, e003430. [Google Scholar] [CrossRef] [PubMed]
- Sapna, F.; Raveena, F.; Chandio, M.; Bai, K.; Sayyar, M.; Varrassi, G.; Khatri, M.; Kumar, S.; Mohamad, T. Advancements in Heart Failure Management: A Comprehensive Narrative Review of Emerging Therapies. Cureus 2023, 15, e46486. [Google Scholar] [CrossRef]
- Metra, M.; Dinatolo, E.; Dasseni, N. The New Heart Failure Association Definition of Advanced Heart Failure. Card. Fail. Rev. 2019, 5, 5–8. [Google Scholar] [CrossRef]
- Crespo-Leiro, M.G.; Metra, M.; Lund, L.H.; Milicic, D.; Costanzo, M.R.; Filippatos, G.; Gustafsson, F.; Tsui, S.; Barge-Caballero, E.; De Jonge, N.; et al. Advanced Heart Failure: A Position Statement of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2018, 20, 1505–1535. [Google Scholar] [CrossRef] [PubMed]
- Metra, M.; Tomasoni, D.; Adamo, M.; Bayes-Genis, A.; Filippatos, G.; Abdelhamid, M.; Adamopoulos, S.; Anker, S.D.; Antohi, L.; Böhm, M.; et al. Worsening of Chronic Heart Failure: Definition, Epidemiology, Management and Prevention. A Clinical Consensus Statement by the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2023, 25, 776–791. [Google Scholar] [CrossRef] [PubMed]
- Martyn, T.; Faulkenberg, K.D.; Albert, C.L.; Il’giovine, Z.J.; Randhawa, V.K.; Donnellan, E.; Menon, V.; Estep, J.D.; Nissen, S.E.; Wilson Tang, W.H.; et al. Acute Hemodynamic Effects of Sacubitril-Valsartan In Heart Failure Patients Receiving Intravenous Vasodilator and Inotropic Therapy. J. Card. Fail. 2021, 27, 368–372. [Google Scholar] [CrossRef]
- Khan, M.S.; Shahid, I.; Bennis, A.; Rakisheva, A.; Metra, M.; Butler, J. Global Epidemiology of Heart Failure. Nat. Rev. Cardiol. 2024, 21, 717–734. [Google Scholar] [CrossRef]
- Bozkurt, B.; Ahmad, T.; Alexander, K.; Baker, W.L.; Bosak, K.; Breathett, K.; Carter, S.; Drazner, M.H.; Dunlay, S.M.; Fonarow, G.C.; et al. HF STATS 2024: Heart Failure Epidemiology and Outcomes Statistics An Updated 2024 Report from the Heart Failure Society of America. J. Card. Fail. 2024, 31, 66–116. [Google Scholar] [CrossRef] [PubMed]
- Triposkiadis, F.; Xanthopoulos, A.; Parissis, J.; Butler, J.; Farmakis, D. Pathogenesis of Chronic Heart Failure: Cardiovascular Aging, Risk Factors, Comorbidities, and Disease Modifiers. Heart Fail. Rev. 2022, 27, 337–344. [Google Scholar] [CrossRef]
- Velazquez, E.J.; Morrow, D.A.; DeVore, A.D.; Duffy, C.I.; Ambrosy, A.P.; McCague, K.; Rocha, R.; Braunwald, E. Angiotensin–Neprilysin Inhibition in Acute Decompensated Heart Failure. N. Engl. J. Med. 2019, 380, 539–548. [Google Scholar] [CrossRef]
- Shah, M.R.; Hasselblad, V.; Stevenson, L.W.; Binanay, C.; O’Connor, C.M.; Sopko, G.; Califf, R.M. Impact of the Pulmonary Artery Catheter in Critically Ill Patients: Meta-Analysis of Randomized Clinical Trials. JAMA 2005, 294, 1664–1670. [Google Scholar] [CrossRef]
- Stevenson, L.W. Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization EffectivenessThe ESCAPE Trial. JAMA 2005, 294, 1625–1633. [Google Scholar] [CrossRef]
- Guglin, M.; Zucker, M.J.; Borlaug, B.A.; Breen, E.; Cleveland, J.; Johnson, M.R.; Panjrath, G.S.; Patel, J.K.; Starling, R.C.; Bozkurt, B. Evaluation for Heart Transplantation and LVAD Implantation: JACC Council Perspectives. J. Am. Coll. Cardiol. 2020, 75, 1471–1487. [Google Scholar] [CrossRef]
- Moon, M.-G.; Hwang, I.-C.; Choi, W.; Cho, G.-Y.; Yoon, Y.E.; Park, J.-B.; Lee, S.-P.; Kim, H.-K.; Kim, Y.-J. Reverse Remodelling by Sacubitril/Valsartan Predicts the Prognosis in Heart Failure with Reduced Ejection Fraction. ESC Heart Fail. 2021, 8, 2058–2069. [Google Scholar] [CrossRef] [PubMed]
- Abboud, A.; Januzzi, J.L. Reverse Cardiac Remodeling and ARNI Therapy. Curr. Heart Fail. Rep. 2021, 18, 71–83. [Google Scholar] [CrossRef]
- Wang, Y.; Zhou, R.; Lu, C.; Chen, Q.; Xu, T.; Li, D. Effects of the Angiotensin-Receptor Neprilysin Inhibitor on Cardiac Reverse Remodeling: Meta-Analysis. J. Am. Heart Assoc. 2019, 8, e012272. [Google Scholar] [CrossRef]
- Zern, E.K.; Cheng, S.; Wolfson, A.M.; Hamilton, M.A.; Zile, M.R.; Solomon, S.D.; Kittleson, M.M. Angiotensin Receptor-Neprilysin Inhibitor Therapy Reverses Pulmonary Hypertension in End-Stage Heart Failure Patients Awaiting Transplantation. Circ. Heart Fail. 2020, 13, e006696. [Google Scholar] [CrossRef] [PubMed]
- Chaumais, M.-C.; Djessas, M.R.A.; Thuillet, R.; Cumont, A.; Tu, L.; Hebert, G.; Gaignard, P.; Huertas, A.; Savale, L.; Humbert, M.; et al. Additive Protective Effects of Sacubitril/Valsartan and Bosentan on Vascular Remodelling in Experimental Pulmonary Hypertension. Cardiovasc. Res. 2021, 117, 1391–1401. [Google Scholar] [CrossRef] [PubMed]
- Mangini, S.; Alves, B.R.; Silvestre, O.M.; Pires, P.V.; Pires, L.J.T.; Curiati, M.N.C.; Bacal, F. Heart Transplantation: Review. Einstein 2015, 13, 310–318. [Google Scholar] [CrossRef]
- Quiram, B.J.; Killian, J.M.; Redfield, M.M.; Smith, J.; Hickson, L.J.; Schulte, P.J.; Ngufor, C.; Dunlay, S.M. Changes in Kidney Function After Diagnosis of Advanced Heart Failure. J. Card. Fail. 2023, 29, 1617–1625. [Google Scholar] [CrossRef]
- Morris, A.A.; Khazanie, P.; Drazner, M.H.; Albert, N.M.; Breathett, K.; Cooper, L.B.; Eisen, H.J.; O’Gara, P.; Russell, S.D.; on behalf of the American Heart Association Heart Failure and Transplantation Committee of the Council on Clinical Cardiology; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; and Council on Hypertension; et al. Guidance for Timely and Appropriate Referral of Patients with Advanced Heart Failure: A Scientific Statement from the American Heart Association. Circulation 2021, 144, e238–e250. [Google Scholar] [CrossRef]
- Pagnesi, M.; Ghiraldin, D.; Vizzardi, E.; Chiarito, M.; Stolfo, D.; Baldetti, L.; Adamo, M.; Lombardi, C.M.; Inciardi, R.M.; Tomasoni, D.; et al. Detailed Assessment of the “I Need Help” Criteria in Patients with Heart Failure: Insights from the HELP-HF Registry. Circ. Heart Fail. 2023, 16, e011003. [Google Scholar] [CrossRef]
| Parameter | Study Population (N = 13) |
|---|---|
| Age, n (%) | 56.4 ± 2.49 |
| Female, n (%) | 3 (23) |
| Male, n (%) | 10 (77) |
| BMI, (kg/m2) | 27.9 ± 2.82 |
| Time on ARNI therapy, (month, IQR) | 6.8 (4.9–16.1) |
| Etiology, n (%) | |
| Ischemic | 6 (46.2) |
| Non-ischemic | 7 (53.8) |
| NYHA class, n (%) | |
| III | 11 (84.5) |
| IV | 2 (15.5) |
| GDMT, n (%) | |
| ACEI/ARB | 13 (100) |
| BB | 13 (100) |
| MRA | 13 (100) |
| SGLT2 inhibitor | 4 (31) |
| ≥50% of target GDMT, n (%) | |
| ACEI/ARB | 13 (100) |
| BB | 12 (92.7) |
| MRA | 10 (76.9) |
| SGLT2 inhibitor | 4 (31) |
| Device therapy, n (%) | |
| ICD | 12 (92.3) |
| CRT-D | 1 (7.7) |
| Comorbidities, risk factors n (%) | |
| Hypertension | 7 (54) |
| Diabetes mellitus (type-2) | 4 (31) |
| Previous MI | 4 (31) |
| Atrial fibrillation | 6 (46) |
| CKD | 4 (31) |
| COPD | 3 (23) |
| Hyperlipidemia | 7 (54) |
| Previous smoker | 5 (39) |
| Previous alcohol consumption | 2 (15.5) |
| Parameter | ACEI/ARB Therapy (N = 13) | ARNI Therapy (N = 13) | p-Value |
|---|---|---|---|
| NYHA class, n (%) | |||
| I | 0 (0) | 1 (7.8) | |
| II | 0 (0) | 6 (46.1) | <0.001 |
| III | 11 (84.5) | 6 (46.1) | |
| IV | 2 (15.5) | 0 | |
| GDMT, n (%) | |||
| ACEI | 13 (100) | 0 (0) | |
| ARNI | 0 (0) | 13 (100) | n.a. |
| BB | 13 (100) | 13 (100) | |
| MRA | 13 (100) | 13 (100) | |
| SGLT2 inhibitor | 4 (31) | 4 (31) | |
| ≥50% of target GDMT, n (%) | |||
| ACEI | 13 (100) | 0 (0) | |
| ARNI | 0 (0) | 10 (76.9) | n.a. |
| BB | 12 (92.7) | 12 (92.7) | |
| MRA | 10 (76.9) | 12 (92.7) | |
| SGLT2 inhibitor | 4 (31) | 4 (31) | |
| Target dose of ARNI, n (%) | |||
| <50% | n.a. | 10 (76.9) | n.a. |
| ≥50% | n.a. | 3 (23.1) | n.a. |
| Laboratory parameters | |||
| NT-proBNP (pg/mL) | 2847 (1444–4977) | 2055 (1313–2754) | 0.092 |
| eGFR (mL/min/1.73 m2) | 70.8 ± 5.18 | 67.9 ± 5.69 | 0.433 |
| Serum creatinine (µmol/L) | 97.9 ± 7.32 | 103.1 ± 8.53 | 0.279 |
| BUN (mmol/L) | 8.6 ± 1.07 | 9.5 ± 1.12 | 0.223 |
| Potassium (mmol/L) | 4.39 ± 0.13 | 4.5 ± 0.11 | 0.533 |
| Echocardiography | |||
| LVEF (%) | 23.65 ± 1.02 | 27.27 ± 1.04 | 0.016 |
| EDD (mm) | 75 ± 3.04 | 77.1 ± 2.61 | n.s. |
| Hemodynamics | |||
| sSBP (mmHg) | 116 (98–124.5) | 106 (101–116) | 0.197 |
| dSBP (mmHg) | 67.9 ± 2.84 | 62.8 ± 1.85 | 0.193 |
| mSBP (mmHg) | 85 (75–86.5) | 79 (72.5–84) | 0.260 |
| sPAP (mmHg) | 46 ± 3.42 | 43.8 ± 3.52 | 0.421 |
| dPAP (mmHg) | 22 ± 1.4 | 19.6 ± 1.6 | 0.118 |
| mPAP (mmHg) | 32 (25.5–38.5) | 27.92 (17.5–35) | 0.168 |
| SVR (dyn·s·cm−5) | 1600 ± 100.5 | 1188 ± 79.8 | 0.004 |
| PVR (dyn·s·cm−5) | 278.9 ± 31.7 | 232.5 ± 34.8 | 0.04 |
| SV (mL) | 55.5 ± 4.12 | 70.9 ± 5.9 | 0.013 |
| CO (L/min) | 3.83 ± 0.24 | 4.9 ± 0.35 | 0.013 |
| CI (L/min/m2) | 1.84 ± 0.1 | 2.35 ± 0.16 | 0.009 |
| HR (1/min) | 70 ± 1.8 | 71 ± 2.71 | 0.593 |
| CVP (mmHg) | 8.31 ± 1.62 | 6.62 ± 1.16 | 0.321 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ráduly, A.P.; Saman Kothalawala, E.; Balogh, L.; Majoros, Z.; Pólik, Z.; Fülöp, L.; Győry, F.; Nagy, L.; Bódi, B.; Kovács, M.B.; et al. Sacubitril/Valsartan Improves Hemodynamic Parameters of Pulmonary and Systemic Circulation in Patients Awaiting Heart Transplantation. J. Clin. Med. 2025, 14, 2539. https://doi.org/10.3390/jcm14082539
Ráduly AP, Saman Kothalawala E, Balogh L, Majoros Z, Pólik Z, Fülöp L, Győry F, Nagy L, Bódi B, Kovács MB, et al. Sacubitril/Valsartan Improves Hemodynamic Parameters of Pulmonary and Systemic Circulation in Patients Awaiting Heart Transplantation. Journal of Clinical Medicine. 2025; 14(8):2539. https://doi.org/10.3390/jcm14082539
Chicago/Turabian StyleRáduly, Arnold Péter, Edward Saman Kothalawala, László Balogh, Zsuzsanna Majoros, Zsófia Pólik, László Fülöp, Ferenc Győry, László Nagy, Beáta Bódi, Máté Balázs Kovács, and et al. 2025. "Sacubitril/Valsartan Improves Hemodynamic Parameters of Pulmonary and Systemic Circulation in Patients Awaiting Heart Transplantation" Journal of Clinical Medicine 14, no. 8: 2539. https://doi.org/10.3390/jcm14082539
APA StyleRáduly, A. P., Saman Kothalawala, E., Balogh, L., Majoros, Z., Pólik, Z., Fülöp, L., Győry, F., Nagy, L., Bódi, B., Kovács, M. B., Csanádi, Z., Papp, Z., Muk, B., & Borbély, A. (2025). Sacubitril/Valsartan Improves Hemodynamic Parameters of Pulmonary and Systemic Circulation in Patients Awaiting Heart Transplantation. Journal of Clinical Medicine, 14(8), 2539. https://doi.org/10.3390/jcm14082539






