Ventilatory Response to Exercise in HFrEF-COPD: Importance of Exercise Modality
Abstract
1. Introduction
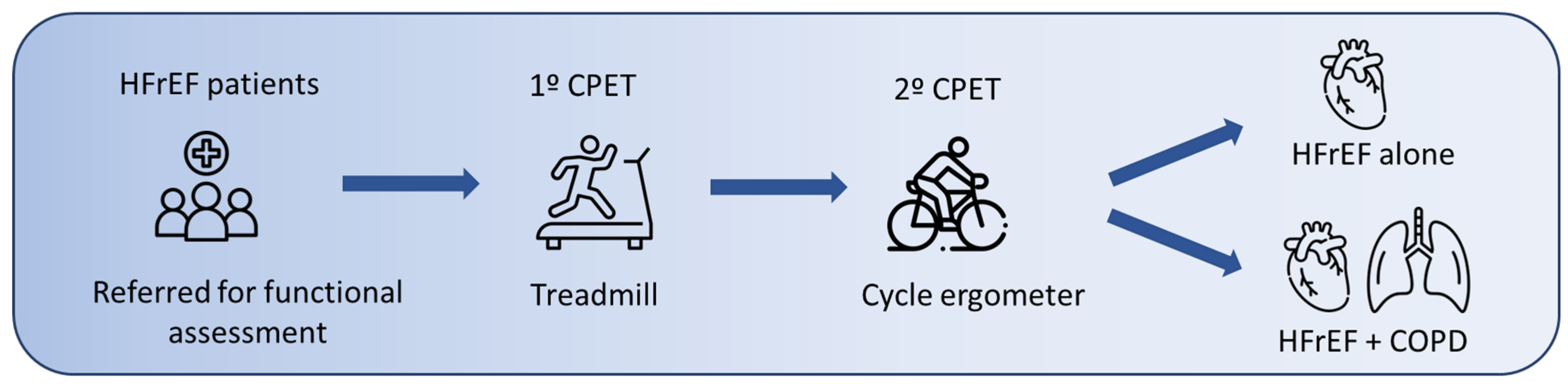
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Cardiopulmonary Exercise Test (CPET), Group HFrEF-COPD
3.2.1. Effort Level
3.2.2. Oxygen Consumption (V·O2)
3.2.3. Ventilatory Response and Gas Exchange
3.2.4. Cardiovascular Response
3.3. Comparison of Patients with HFrEF with and Without COPD
3.3.1. Symptoms and Preference
3.3.2. Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Natali, D.; Cloatre, G.; Hovette, P.; Cochrane, B. Screening for Comorbidities in COPD. Breathe 2020, 16, 190315. [Google Scholar] [CrossRef] [PubMed]
- Papaporfyriou, A.; Bartziokas, K.; Gompelmann, D.; Idzko, M.; Fouka, E.; Zaneli, S.; Bakakos, P.; Loukides, S.; Papaioannou, A.I. Cardiovascular Diseases in COPD: From Diagnosis and Prevalence to Therapy. Life 2023, 13, 1299. [Google Scholar] [CrossRef]
- Myers, L.C.; Quint, J.K.; Hawkins, N.M.; Putcha, N.; Hamilton, A.; Lindenauer, P.; Wells, J.M.; Witt, L.J.; Shah, S.P.; Lee, T.; et al. A Research Agenda to Improve Outcomes in Patients with Chronic Obstructive Pulmonary Disease and Cardiovascular Disease: An Official American Thoracic Society Research Statement. Am. J. Respir. Crit. Care Med. 2024, 210, 715–729. [Google Scholar] [CrossRef] [PubMed]
- Barron, A.; Francis, D.P.; Mayet, J.; Ewert, R.; Obst, A.; Mason, M.; Elkin, S.; Hughes, A.D.; Wensel, R. Oxygen Uptake Efficiency Slope and Breathing Reserve, Not Anaerobic Threshold, Discriminate Between Patients with Cardiovascular Disease Over Chronic Obstructive Pulmonary Disease. JACC Heart Fail. 2016, 4, 252–261. [Google Scholar] [CrossRef]
- Sietsema, K.E.; Sue, D.Y.; Stringer, W.W.; Ward, S.A. Wasserman & Whipp’s Principles of Exercise Testing and Interpretation, 6th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2021. [Google Scholar]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienè, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Eur. Heart J. 2021, 42, 3599–3726, Erratum in Eur. Heart J. 2021, 42, 4901. [Google Scholar] [CrossRef]
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for Prevention, Diagnosis and Management of COPD: 2025 Report; Global Initiative for Chronic Obstructive Lung Disease: Philadelphia, PA, USA, 2025. [Google Scholar]
- Hermansen, L.; Saltin, B. Oxygen Uptake during Maximal Treadmill and Bicycle Exercise. J. Appl. Physiol. 1969, 26, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Miyamara, M.; Honda, Y. Oxygen Intake and Cardiac Output during Maximal Treadmill and Bicycle Exercise. J. Appl. Physiol. 1972, 32, 185–188. [Google Scholar] [CrossRef]
- Lockwood, P.A.; Yoder, J.E.; Deuster, P.A. Comparison and Cross-Validation of Cycle Ergometry Estimates of VO2max. Med. Sci. Sports Exerc. 1997, 29, 1513–1520. [Google Scholar] [CrossRef]
- Herrero Huertas, J.; García Clemente, M.; Díaz Molina, B.; Lambert Rodríguez, J.L.; Íscar Urrutia, M. Heart Failure with Reduced Ejection Fraction and Prognostic Scales: The Impact of Exercise Modality in Cardiopulmonary Exercise Tests. J. Clin. Med. 2022, 11, 3122. [Google Scholar] [CrossRef]
- Guazzi, M.; Myers, J.; Vicenzi, M.; Bensimhon, D.; Chase, P.; Pinkstaff, S.; Arena, R. Cardiopulmonary Exercise Testing Characteristics in Heart Failure Patients with and without Concomitant Chronic Obstructive Pulmonary Disease. Am. Heart J. 2010, 160, 900–905. [Google Scholar] [CrossRef]
- Oliveira, M.F.; Arbex, F.F.; Alencar, M.C.; Souza, A.; Sperandio, P.A.; Medeiros, W.M.; Borghi-Silva, A.; Medina, L.A.; Santos, R.; Hirai, D.M.; et al. Heart Failure Impairs Muscle Blood Flow and Endurance Exercise Tolerance in COPD. COPD 2016, 13, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Arbex, F.F.; Alencar, M.C.; Souza, A.; Mazzuco, A.; Sperandio, P.A.; Rocha, A.; Berton, D.C.; Borghi-Silva, A.; Almeida, D.R.; O’Donnell, D.E.; et al. Exercise Ventilation in COPD: Influence of Systolic Heart Failure. COPD 2016, 13, 693–699. [Google Scholar] [CrossRef] [PubMed]
- Rocha, A.; Arbex, F.F.; Sperandio, P.A.; Souza, A.; Biazzim, L.; Mancuso, F.; Berton, D.C.; Hochhegger, B.; Alencar, M.C.N.; Nery, L.E.; et al. Excess Ventilation in Chronic Obstructive Pulmonary Disease-Heart Failure Overlap: Implications for Dyspnea and Exercise Intolerance. Am. J. Respir. Crit. Care Med. 2017, 196, 1264–1274. [Google Scholar] [CrossRef]
- Quanjer, P.H.; Stanojevic, S.; Cole, T.J.; Baur, X.; Hall, G.L.; Culver, B.H.; Enright, P.L.; Hankinson, J.L.; Ip, M.S.M.; Zheng, J.; et al. Multi-Ethnic Reference Values for Spirometry for the 3–95-Year Age Range: The Global Lung Function 2012 Equations. Eur. Respir. J. 2012, 40, 1324–1343. [Google Scholar] [CrossRef]
- Singh, D.; Agusti, A.; Anzueto, A.; Barnes, P.J.; Bourbeau, J.; Celli, B.R.; Criner, G.J.; Frith, P.; Halpin, D.M.G.; Han, M.; et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease: The GOLD Science Committee Report 2019. Eur. Respir. J. 2019, 53, 1900164. [Google Scholar] [CrossRef] [PubMed]
- Pereiro Alonso, M.E. Capacidad Aeróbica en una Población Adulta Sana y Calidad de Vida Relacionada con la Salud. 2003. Available online: http://hdl.handle.net/10651/16219 (accessed on 4 November 2024).
- Balady, G.J.; Arena, R.; Sietsema, K.; Myers, J.; Coke, L.; Fletcher, G.F.; Forman, D.; Franklin, B.; Guazzi, M.; Gulati, M.; et al. Clinician’s Guide to Cardiopulmonary Exercise Testing in Adults: A Scientific Statement from the American Heart Association. Circulation 2010, 122, 191–225. [Google Scholar] [CrossRef]
- American Thoracic Society; American College of Chest Physicians. ATS/ACCP Statement on Cardiopulmonary Exercise Testing. Am. J. Respir. Crit. Care Med. 2003, 167, 211–277. [Google Scholar] [CrossRef]
- Paolillo, S.; Agostoni, P. Prognostic Role of Cardiopulmonary Exercise Testing in Clinical Practice. Ann. Am. Thorac. Soc. 2017, 14 (Suppl. 1), S53–S58. [Google Scholar] [CrossRef]
- Ramalho, S.H.R.; de Albuquerque, A.L.P. Chronic Obstructive Pulmonary Disease in Heart Failure: Challenges in Diagnosis and Treatment for HFpEF and HFrEF. Curr. Heart Fail. Rep. 2024, 21, 163–173. [Google Scholar] [CrossRef]
- Hsia, D.; Casaburi, R.; Pradhan, A.; Torres, E.; Porszasz, J. Physiological Responses to Linear Treadmill and Cycle Ergometer Exercise in COPD. Eur. Respir. J. 2009, 34, 605–615. [Google Scholar] [CrossRef]
- Corrà, U.; Agostoni, P.G.; Anker, S.D.; Coats, A.J.; Crespo Leiro, M.G.; de Boer, R.A.; Harjola, V.P.; Hill, L.; Lainscak, M.; Lund, L.H.; et al. Role of Cardiopulmonary Exercise Testing in Clinical Stratification in Heart Failure. A Position Paper from the Committee on Exercise Physiology and Training of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2018, 20, 3–15, Erratum in Eur. J. Heart Fail. 2018, 20, 1501. [Google Scholar] [CrossRef] [PubMed]
- Beckers, P.J.; Possemiers, N.M.; Van Craenenbroeck, E.M.; Van Berendoncks, A.M.; Wuyts, K.; Vrints, C.J.; Conraads, V.M. Impact of Exercise Testing Mode on Exercise Parameters in Patients with Chronic Heart Failure. Eur. J. Prev. Cardiol. 2012, 19, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Neder, J.A.; Phillips, D.B.; Marillier, M.; Bernard, A.C.; Berton, D.C.; O’Donnell, D.E. Clinical Interpretation of Cardiopulmonary Exercise Testing: Current Pitfalls and Limitations. Front. Physiol. 2021, 12, 552000. [Google Scholar] [CrossRef]
- Haverkamp, H.C.; Balmain, B.N. Ventilatory Responses to Exercise by Age, Sex, and Health Status. Curr. Sports Med. Rep. 2024, 23, 79–85. [Google Scholar] [CrossRef]
- Kim, S.; Yamabe, H.; Yokoyama, M. Hemodynamic Characteristics during Treadmill and Bicycle Exercise in Chronic Heart Failure: Mechanism for Different Responses of Peak Oxygen Uptake. Jpn. Circ. J. 1999, 63, 965–970. [Google Scholar] [CrossRef] [PubMed]
- Boudestein, L.C.; Rutten, F.H.; Cramer, M.J.; Lammers, J.W.J.; Hoes, A.W. The Impact of Concurrent Heart Failure on Prognosis in Patients with Chronic Obstructive Pulmonary Disease. Eur. J. Heart Fail. 2009, 11, 1182–1188. [Google Scholar] [CrossRef]
| Variables | HFrEF (n = 47) | IHFrEF + COPD (n = 18) | p |
|---|---|---|---|
| General Characteristics | |||
| Age (years) | 56.4 ± 9.6 | 61.6 ± 7.6 | 0.04 |
| Male sex | 30 (70%) | 16 (89%) | 0.198 |
| BMI (kg/m2) | 30 ± 4.2 | 27.1 ± 4.4 | 0.01 |
| LVEF (%) | 29.9 ± 8.6 | 28.6 ± 8.6 | 0.599 |
| Lung function | |||
| FEV1 (%) | 88.5 ± 14.1 | 73.3 ± 14.8 | 0.001 |
| FVC (%) | 90.6 ± 14.4 | 89.7 ± 19.3 | 0.864 |
| FEV 1/ FVC (%) | 75.3 ± 3.8 | 62.4 ± 4.3 | 0.001 |
| Functional class | |||
| NYHA class I | 10 (21%) | 3 (17%) | 0.678 |
| NYHA class II | 29 (62%) | 12 (66%) | 0.711 |
| NYHA class III | 8 (17%) | 3 (17%) | 1000 |
| Cause of HFrEF | |||
| Ischemic | 18 (39%) | 10 (56%) | 0.209 |
| Idiopathic | 20 (44%) | 7 (39%) | 0.788 |
| Hereditary | 6 (13%) | 0 (0%) | 0.175 |
| Others | 2 (4%) | 1 (5%) | 0.823 |
| Chronic Treatment | HFrEF (n = 47) | HFrEF-COPD (n = 18) | p |
|---|---|---|---|
| Beta-blocker | 45 (95.8%) | 18 (100%) | 0.520 |
| Amiodarone | 1 (2.1%) | 2 (11.1%) | 0.183 |
| RAASi | 32 (68%) | 8 (44.4%) | 0.411 |
| MRA | 25 (53.2%) | 12 (66.7%) | 0.407 |
| Valsartan/Sacubitril | 13 (27.7%) | 9 (50%) | 0.142 |
| Ivabradine | 5 (10.6%) | 2 (11.1%) | 0.956 |
| Loop diuretics | 30 (63.8%) | 11 (61.1%) | 0.839 |
| Thiazides | 47 (100%) | 1 (5.6%) | 0.277 |
| Implantable cardioverter defibrillator | |||
| Single chamber | 7 (15%) | 4 (22%) | 0.693 |
| CRT | 12 (25.5%) | 10 (56%) | 0.03 |
| No device | 28 (59.6%) | 4 (22%) | 0.006 |
| Treadmill Median (IQR) | Cycle Ergometer Median (IQR) | p | |
|---|---|---|---|
| Test duration (min−1) | 11 (7.5–12) | 9 (8–10) | 0.216 |
| V·O2 baseline ( mL/min−1) | 420 (330–550) | 450 (370–545) | 0.580 |
| V·O2 peak ( mL/min−1) | 1550 (1180–1820) | 1225 (1040–1420) | <0.001 |
| V·O2 kg peak ( mL/kg/ min−1) | 20 (17–23) | 17 (15–19) | <0.001 |
| V·O2 at VT ( mL/min−1) | 1630 (1480–1710) | 1290 (1070–1410) | <0.001 |
| V·CO2 at VT ( mL/min−1) | 1610 (1465–1685) | 1275 (1040–1410) | <0.001 |
| RQ máx. | 0.9 (0.9–1) | 1 (0.9–1) | 0.880 |
| V·Emax (L/min−1) | 59 (48–62.5) | 45.9 (38.6–46.8) | <0.001 |
| RR max (bpm−1) | 30.9 (26.5–36.4) | 25.5 (21–28.5) | 0.017 |
| BR% | 12 (2–35) | 30 (22–48) | <0.001 |
| EQO2 at VT | 38 (34–39) | 36.5 (33–39) | 0.999 |
| EQCO2 at VT | 38 (35.5–39) | 37 (33.5–39.5) | 0.999 |
| VEslope | 32 (29–37) | 35 (31–38.6) | 0.042 |
| PETCO2 baseline | 32 (30–36) | 32.5 (31–34) | 0.412 |
| PETCO2 at VT (mmHg) | 35 (34–37) | 37.5 (34–39) | 0.249 |
| SatpO2 initial (%) | 96.5 (96–98) | 98 (96–98) | 0.007 |
| SatpO2 at the end (%) | 96 (95–98) | 98 (97–98) | 0.001 |
| HR baseline (lpm−1) | 71.5 (66.5–75) | 68.5 (66.5–73.5) | 0.348 |
| HR at the end (lpm−1) | 119 (102.5–132) | 108.5 (100–120.5) | 0.067 |
| HR recovery index (bpm−1) | 17 (12–25) | 16 (14–19) | 0.079 |
| V·O2 /FC (L/bpm/ min−1) | 14.1 (11.9–17.7) | 12.7 (10.3–15.5) | <0.001 |
| SBP initial (mmHg) | 120 (110–140) | 120 (115–140) | 0.702 |
| SBP at the end (mmHg) | 170 (150–185) | 162.5 (140–180) | 0.562 |
| DBP initial (mmHg) | 70 (60–80) | 80 (70–90) | 0.075 |
| DBP at the end (mmHg) | 80 (70–90) | 82.5 (80–90) | 0.037 |
| Borg dyspnea at the end | 5.5 (5–7) | 3.5 (2–4) | 0.001 |
| Borg lower limbs at the end | 4 (0–7) | 4 (3–5) | 0.545 |
| Parameters | HFrEF (n = 47) Median (IQR) | HFrEF+ COPD (n = 18) Median (IQR) | p |
|---|---|---|---|
| Test Duration (minutes) | |||
| Treadmill | 11 (9.1–12.5) | 11 (7.5–12) | 0.284 |
| Cycle Ergometer | 11 (9–12) | 9 (8–10) | 0.089 |
| Reaches VT (%) | |||
| Treadmill | 95.7% | 88.9% | 0.305 |
| Cycle Ergometer | 78.7% | 72.2% | 0.578 |
| HR max. (bpm) | |||
| Treadmill | 119 (108–131) | 119 (102.5–132) | 0.537 |
| Cycle Ergometer | 107 (99.5–120) | 108.5 (100–120.5) | 0.922 |
| HR recovery index (bpm) | |||
| Treadmill | 20.5 (14–31) | 17 (12–25) | 0.463 |
| Cycle Ergometer | 15 (10–25) | 16 (14–19) | 0.902 |
| SBP at the End of Exercise (mmHg) | |||
| Treadmill | 150 (137.5–170) | 170 (150–185) | 0.352 |
| Cycle Ergometer | 160 (140–180) | 162.5 (140–180) | 0.824 |
| DBP at the End of Exercise (mmHg) | |||
| Treadmill | 80 (70–90) | 80 (70–90) | 0.549 |
| Cycle Ergometer | 90 (80–100) | 82.5 (80–90) | 0.417 |
| Final O2 Saturation (%) | |||
| Treadmill | 97 (96–98) | 98 (97–98) | 0.380 |
| Cycle Ergometer | 97 (96–98) | 96 (95–98) | 0.294 |
| V·O2 peak (ml/min) | |||
| Treadmill | 1690 (1425–2140) | 1550 (1180–1820) | 0.101 |
| Cycle Ergometer | 1390 (1190–1680) | 1225 (1040–1420) | 0.125 |
| V·O2 /HR max. (ml/bpm/ min−1) | |||
| Treadmill | 14.1 (11.8–17.1) | 14.1 (11.9–17.7) | 0.675 |
| Cycle Ergometer | 12.1 (9.7–15.2) | 12.7 (10.3–15.5) | 0.806 |
| V·E Slope | |||
| Treadmill | 29 (27–34) | 32 (29–37) | 0.066 |
| Cycle Ergometer | 32 (27–35.8) | 35 (31–38.6) | 0.042 |
| V·E max. (L/ min−1) | |||
| Treadmill | 53.3 (46.5–65.5) | 59 (48–62.5) | 0.765 |
| Cycle Ergometer | 45.8 (37.9–51.8) | 45.9 (38.6–46.8) | 0.686 |
| RR max (rpm−1) | |||
| Treadmill | 30 (25.3–34.9) | 30.9 (26.5–36.4) | 0.804 |
| Cycle Ergometer | 27 (24.9–32.5) | 25.5 (21–28.5) | 0.076 |
| EqO2 at VT | |||
| Treadmill | 35 (32–38) | 38 (34–39) | 0.049 |
| Cycle Ergometer | 36.5 (33–41) | 36.5 (33–39) | 0.919 |
| EQCO2 at VT | |||
| Treadmill | 35.5 (32.5–38.5) | 38.8 (35.5–39) | 0.042 |
| Cycle Ergometer | 37 (33–41.5) | 37 (33.5–39.5) | 0.671 |
| PET CO2 at VT (mmHg) | |||
| Treadmill | 36.5 (33.5–39.5) | 35 (34–37) | 0.075 |
| Cycle Ergometer | 35.5 (32–39) | 37.5 (34–39) | 0.958 |
| ΔPETCO2 (mmHg) | |||
| Treadmill | 4.5 (1–6) | 3.5 (3–5.5) | 0.518 |
| Cycle Ergometer | 2 (0–5) | 3 (1.5–3.5) | 0.730 |
| BR at max. exercise (%) | |||
| Treadmill | 30 (25.3–34.9) | 12 (2–35) | 0.006 |
| Cycle Ergometer | 27 (24.9–32.5) | 30 (22–48) | 0.020 |
| EOV (%) | |||
| Treadmill | 41.3% | 0% | 0.001 |
| Cycle Ergometer | 45.6% | 11.8% | 0.010 |
| Final Borg Dyspnea (1–10) | |||
| Treadmill | 6 (3.5–7) | 5.5 (5–7) | 0.567 |
| Cycle Ergometer | 4 (2–5.5) | 3.5 (2–4) | 0.561 |
| Final Borg Lower Limbs (1–10) | |||
| Treadmill | 3 (0.5–7) | 4 (0–7) | 0.861 |
| Cycle Ergometer | 5 (4–7) | 4 (3–5) | 0.178 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Íscar Urrutia, M.; Huertas, J.H.; Castro, M.A.; Fernández Álvarez, R.; Molina, B.D.; Clemente, M.G. Ventilatory Response to Exercise in HFrEF-COPD: Importance of Exercise Modality. J. Clin. Med. 2025, 14, 2538. https://doi.org/10.3390/jcm14082538
Íscar Urrutia M, Huertas JH, Castro MA, Fernández Álvarez R, Molina BD, Clemente MG. Ventilatory Response to Exercise in HFrEF-COPD: Importance of Exercise Modality. Journal of Clinical Medicine. 2025; 14(8):2538. https://doi.org/10.3390/jcm14082538
Chicago/Turabian StyleÍscar Urrutia, Marta, Julia Herrero Huertas, Marina Acebo Castro, Ramón Fernández Álvarez, Beatriz Díaz Molina, and Marta García Clemente. 2025. "Ventilatory Response to Exercise in HFrEF-COPD: Importance of Exercise Modality" Journal of Clinical Medicine 14, no. 8: 2538. https://doi.org/10.3390/jcm14082538
APA StyleÍscar Urrutia, M., Huertas, J. H., Castro, M. A., Fernández Álvarez, R., Molina, B. D., & Clemente, M. G. (2025). Ventilatory Response to Exercise in HFrEF-COPD: Importance of Exercise Modality. Journal of Clinical Medicine, 14(8), 2538. https://doi.org/10.3390/jcm14082538






