Arthroscopic Excision of Scapular Exostoses: A Technical Note
Abstract
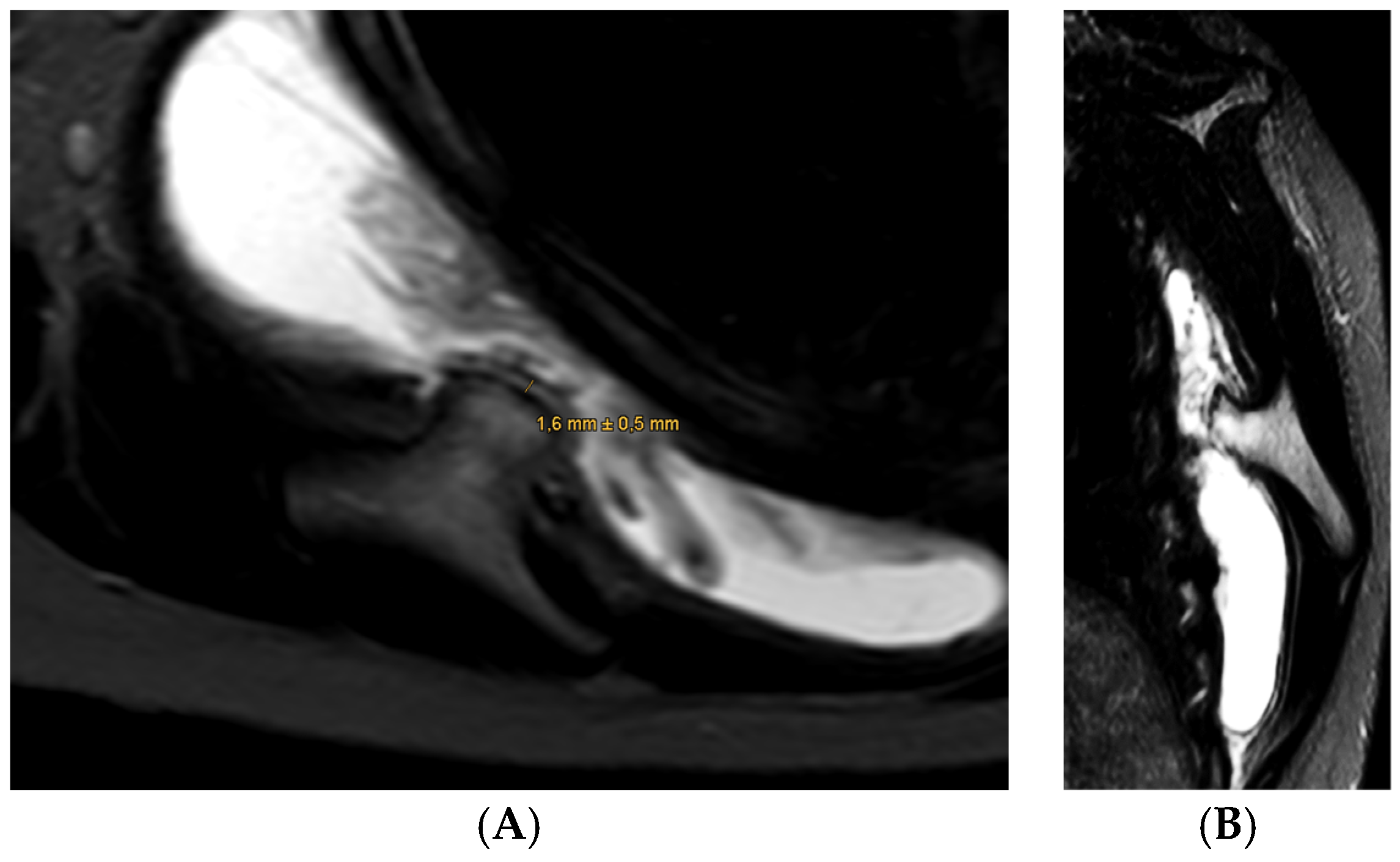
1. Case Presentation
2. Introduction
3. Surgical Technique
- Posterior portal (visualization): Located 2 cm medial and inferior to the posterolateral acromial border.
- Lateral portal: Placed over the lateral scapular border for instrumentation or triangulation.
- Anterior portal: Established under direct visualization when additional access is needed for retraction or instrument guidance.
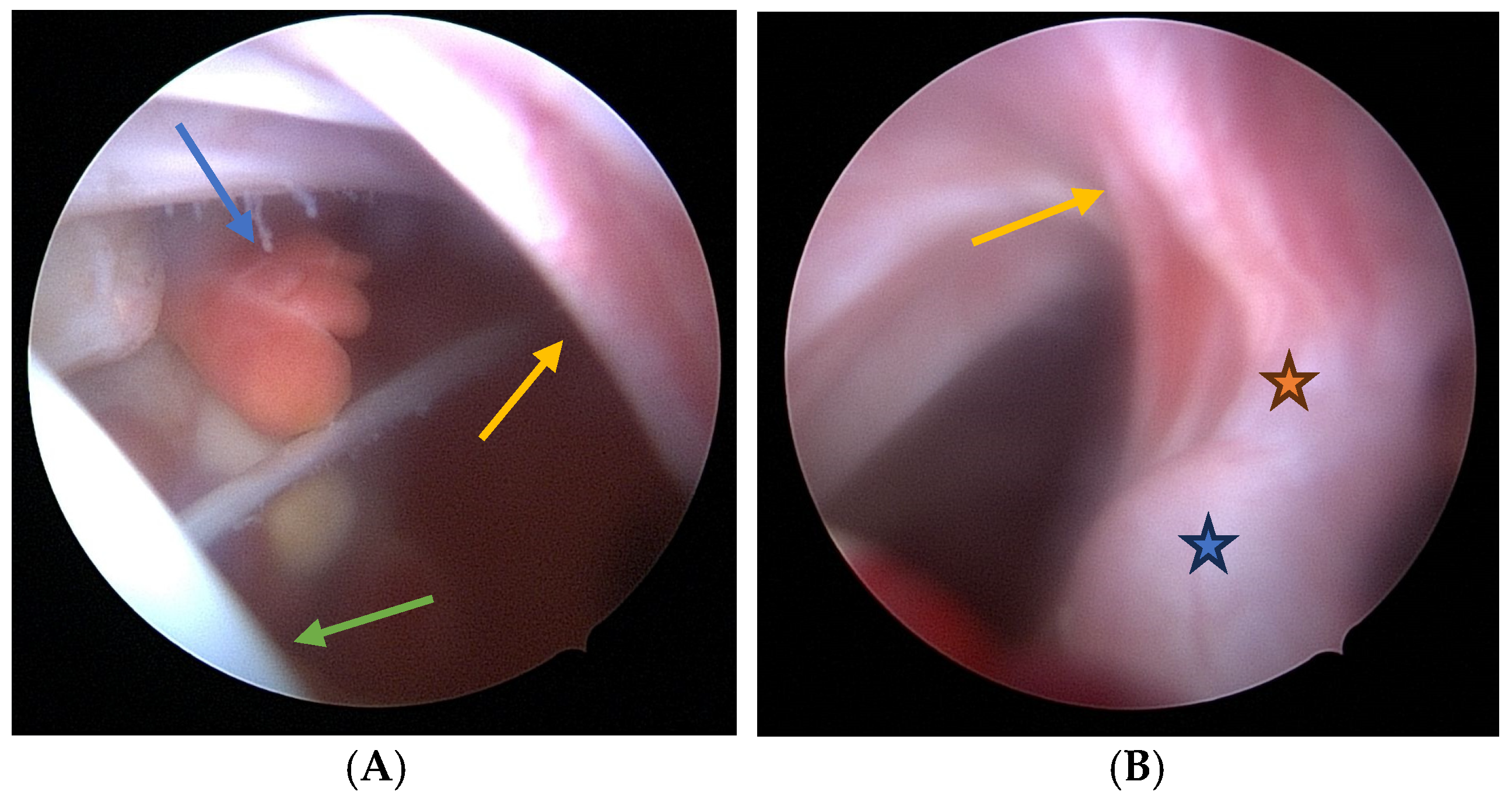
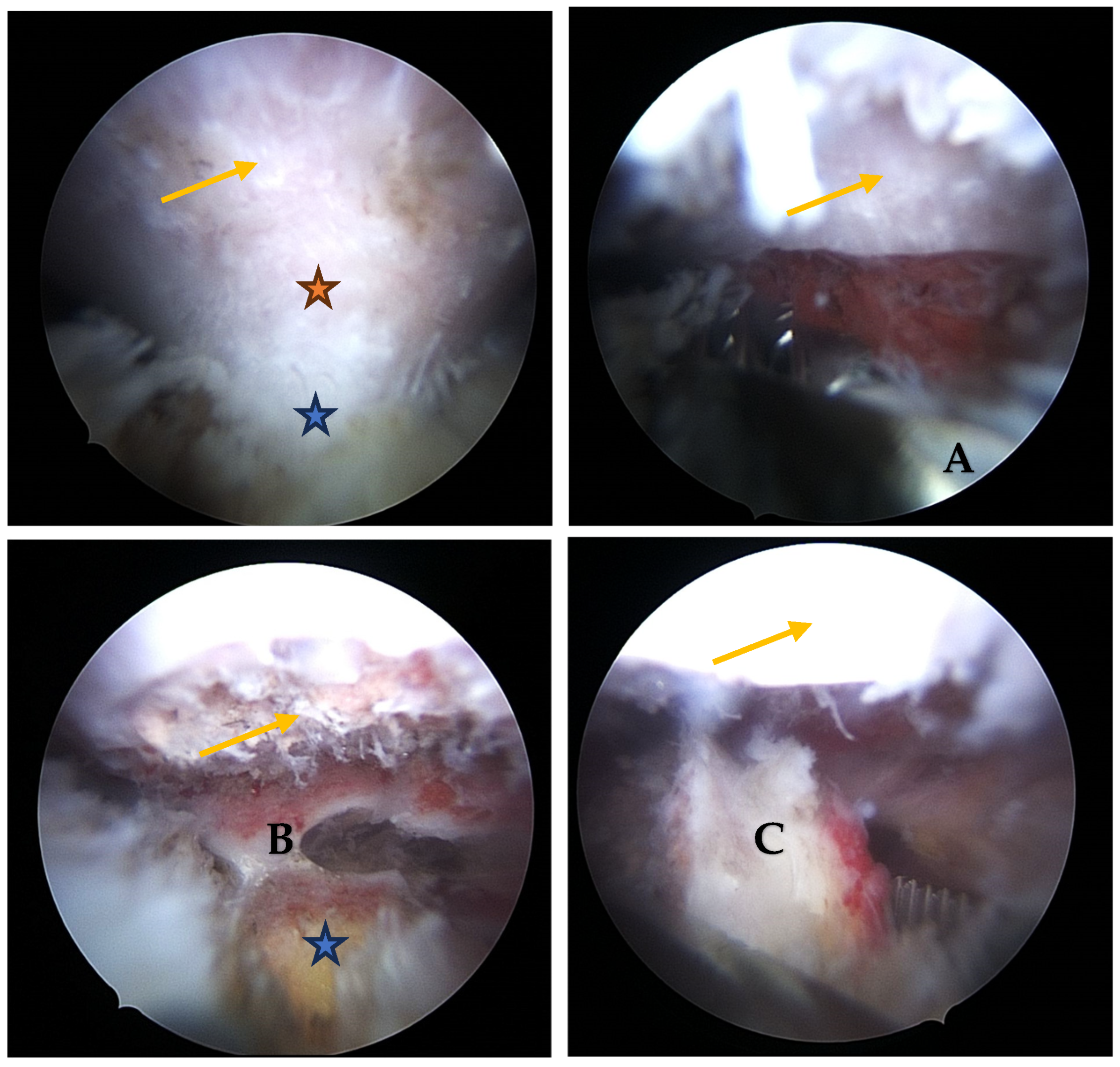
- Visualization: The arthroscope is introduced through the posterior portal. Initial visualization targets the inflamed scapulothoracic bursa to gain orientation (Figure 3A,B). In the present case, the exostosis was partially protruding through the subscapularis muscle and thus visible upon entry. A blunt dissection plane is established between the scapula and the subscapularis muscle to expose the exostosis base.
- Instrumentation: A second posterior portal is established for working access. Through this portal, arthroscopic burrs, graspers, and the electrosurgical device are inserted. In certain cases, lateral or anterior accessory portals may enhance triangulation or access to deeper portions of the scapula.
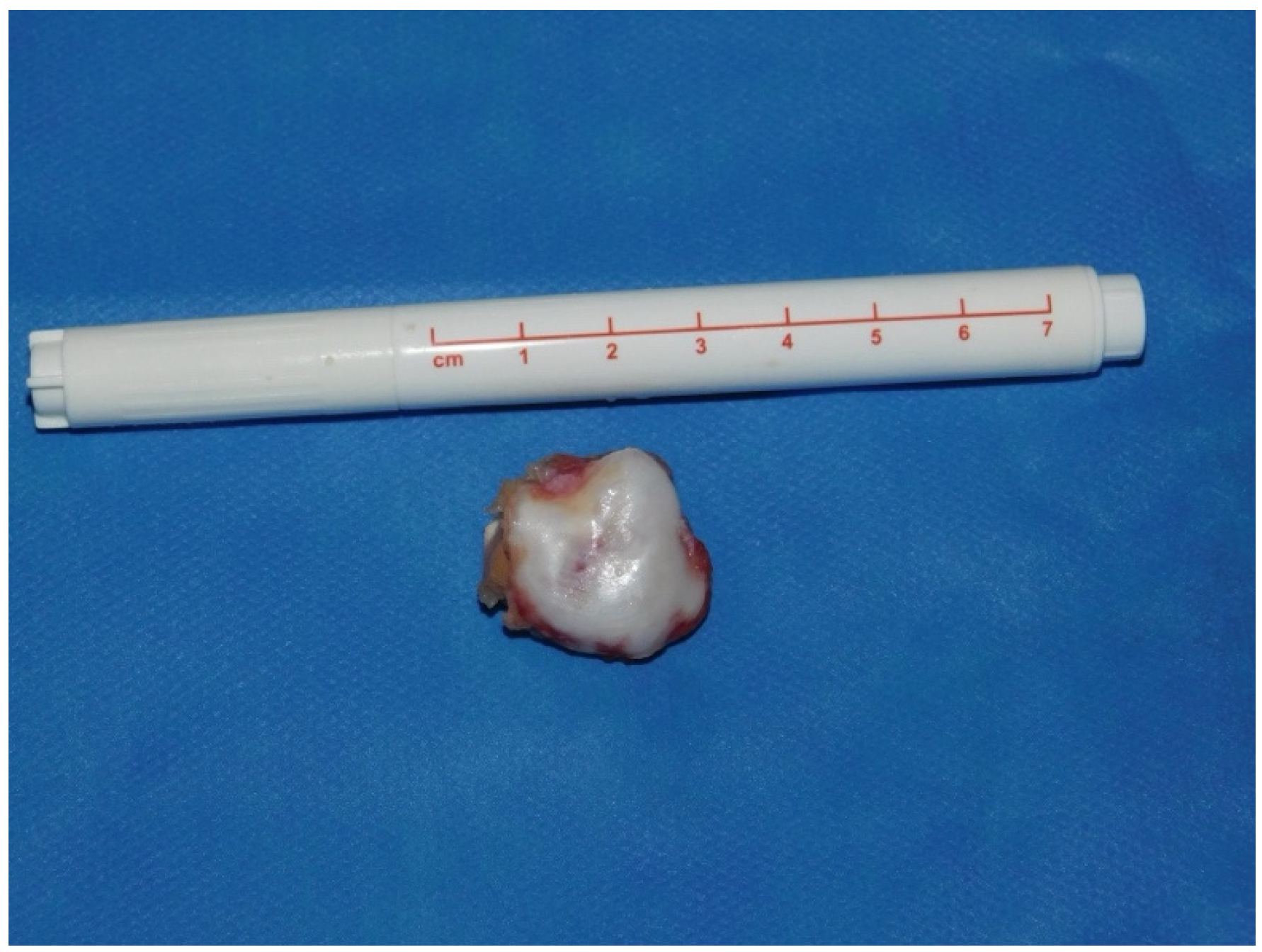
- Resection: Using a high-speed burr under continuous irrigation, the lesion is carefully resected flush to the scapular surface. To ensure oncologic safety, the exostosis is excised at its base as a single piece and removed using an arthroscopic grasper for histopathological examination (Figure 4). Constant visualization is maintained to avoid iatrogenic injury to adjacent structures.
- Histopathological Confirmation: The excised specimen (Figure 5) is sent for formal pathological analysis. In our case, the diagnosis of benign osteochondroma was confirmed without atypical or malignant features.
- Hemostasis and Debridement: Electrocautery (vapor electrode) is used to control minor bleeding. Loose bone fragments and inflamed bursal tissue are debrided thoroughly using a 4 mm shaver and suction.
- Closure: All portals are closed with absorbable sutures. Sterile dressings are applied, and the patient is placed in a sling for comfort.
4. Postoperative Rehabilitation and Outcomes
5. Risks and Technical Challenges
6. Discussion
7. Limitations
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Fageir, M.M.; Edwards, M.R.; Addison, A.K. The surgical management of osteochondroma on the ventral surface of the scapula. J. Pediatr. Orthop. B 2009, 18, 304–307. [Google Scholar] [CrossRef] [PubMed]
- Alshayhan, F.A.; Alahaidib, A.; Alsowaigh, M.; Alahaideb, A. Bilateral scapular osteochondroma in Multiple Hereditary Exostosis patient presented with bilateral shoulder pain treated with arthroscopic and open excision: Case report. Ann. Med. Surg. 2021, 67, 102481. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, K.; Inokuchi, W. Solitary Osteochondroma of the Ventral Scapula Associated with Large Bursa Formation and Pseudowinging of the Scapula: A Case Report and Literature Review. Case Rep. Orthop. 2018, 2018, 5145642. [Google Scholar] [CrossRef]
- Spannagel, T.; Haug, L.; Achenbach, L.; List, K. Kartilaginäre Exostose als seltene Ursache für ein externes Impingement der Schulter. Arthroskopie 2023, 36, 58–61. [Google Scholar] [CrossRef]
- Schmidt, A. Multiple kartilaginäre Exostosen. Osteologie 2018, 27, 229–234. [Google Scholar] [CrossRef]
- Wülker, N.; Kluba, T.; Roetman, B.; Rudert, M. Taschenlehrbuch Orthopädie und Unfallchirurgie; Thieme: Stuttgart, Gremany, 2022. [Google Scholar]
- Schmitt, S.; Esslinger, T.; Obernhuber, E. Solitäre kartilaginäre Exostose der lateralen Klavikula. Arthroskopie 2011, 24, 232. [Google Scholar] [CrossRef]
- Stieber, J.R.; Dormans, J.P. Manifestations of hereditary multiple exostoses. J. Am. Acad. Orthop. Surg. 2005, 13, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Bovee, J.V. Multiple osteochondromas. Orphanet J. Rare Dis. 2008, 3, 3. [Google Scholar] [CrossRef] [PubMed]
- Krakowski, P.; Rejniak, A.; Sobczyk, J.; Karpiński, R. Cartilage Integrity: A Review of Mechanical and Frictional Properties and Repair Approaches in Osteoarthritis. Healthcare 2024, 12, 1648. [Google Scholar] [CrossRef] [PubMed]
- Villar Quintana, R.; Maggini, E.; Scheibel, M. Dynamic Scapular Winging Caused by Long Thoracic Nerve Compression due to Scapular Osteochondroma: A Case Report. JBJS Case Connect. 2024, 14, e24.00003. [Google Scholar] [CrossRef] [PubMed]
- WHO Classification of Tumours Editorial Board. WHO Classification of Tumours Soft Tissue and Bone Tumours, 5th ed.; IARC Press: Lyon, France, 2020. [Google Scholar]
- Aalderink, K.; Wolf, B. Scapular osteochondroma treated with arthroscopic excision using prone positioning. Am. J. Orthop. 2010, 39, E11–E14. [Google Scholar] [PubMed]
- Fukunaga, S.; Futani, H.; Yoshiya, S. Endoscopically assisted resection of a scapular osteochondroma causing snapping scapula syndrome. World J. Surg. Oncol. 2007, 5, 37. [Google Scholar] [CrossRef] [PubMed]
- Peterson, H.A. Multiple hereditary osteochondromata. Clin. Orthop. Relat. Res. 1989, 239, 222–230. [Google Scholar]
- van Riet, R.P.; Van Glabbeek, F. Arthroscopic resection of a symptomatic snapping subscapular osteochondroma. Acta Orthop. Belg. 2007, 73, 252–254. [Google Scholar] [PubMed]
- Blacksin, M.F.; Benevenia, J. Neoplasms of the scapula. AJR Am. J. Roentgenol. 2000, 174, 1729–1735. [Google Scholar] [CrossRef] [PubMed]
- Ruland, L.J., 3rd; Ruland, C.M.; Matthews, L.S. Scapulothoracic anatomy for the arthroscopist. Arthroscopy 1995, 11, 52–56. [Google Scholar] [CrossRef] [PubMed]

| Parameter | Open Technique | Arthroscopic Technique |
|---|---|---|
| Operative Time | Typically longer due to extensive exposure and muscle detachment [1] | Generally shorter with targeted access and minimal dissection [2] |
| Tissue Disruption | Significant; involves detachment of major muscles, leading to potential weakness and longer recovery [1] | Minimal; preserves muscle integrity, reducing the risk of postoperative dysfunction [2] |
| Complication Rate | Higher risk of infection, nerve injury, and scapular dyskinesis [1] | Lower complication rates with reduced risk of neurovascular damage and soft tissue trauma [3] |
| Recovery Time | Extended rehabilitation required; delayed return to daily activities [1] | Accelerated rehabilitation; earlier return to function reported in small series and case reports [2,3] |
| Postoperative Pain | Increased due to larger incisions and muscle dissection [1] | Reduced postoperative pain attributed to minimal invasiveness and smaller incisions [2] |
| Tissue Containment | Follows principles of tumor surgery with en bloc resection and controlled tissue handling | Potential dissemination of tumor tissue into the subscapular bursa due to fragmenting or shaving techniques |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hochberger, F.; List, K. Arthroscopic Excision of Scapular Exostoses: A Technical Note. J. Clin. Med. 2025, 14, 2464. https://doi.org/10.3390/jcm14072464
Hochberger F, List K. Arthroscopic Excision of Scapular Exostoses: A Technical Note. Journal of Clinical Medicine. 2025; 14(7):2464. https://doi.org/10.3390/jcm14072464
Chicago/Turabian StyleHochberger, Felix, and Kilian List. 2025. "Arthroscopic Excision of Scapular Exostoses: A Technical Note" Journal of Clinical Medicine 14, no. 7: 2464. https://doi.org/10.3390/jcm14072464
APA StyleHochberger, F., & List, K. (2025). Arthroscopic Excision of Scapular Exostoses: A Technical Note. Journal of Clinical Medicine, 14(7), 2464. https://doi.org/10.3390/jcm14072464






