No Short-Term Effects of Acromioclavicular Joint Augmentation in Acute Acromioclavicular Joint Stabilization Surgery: A Randomized Controlled Clinical Trial on 70 Patients
Abstract
1. Introduction
2. Materials and Methods
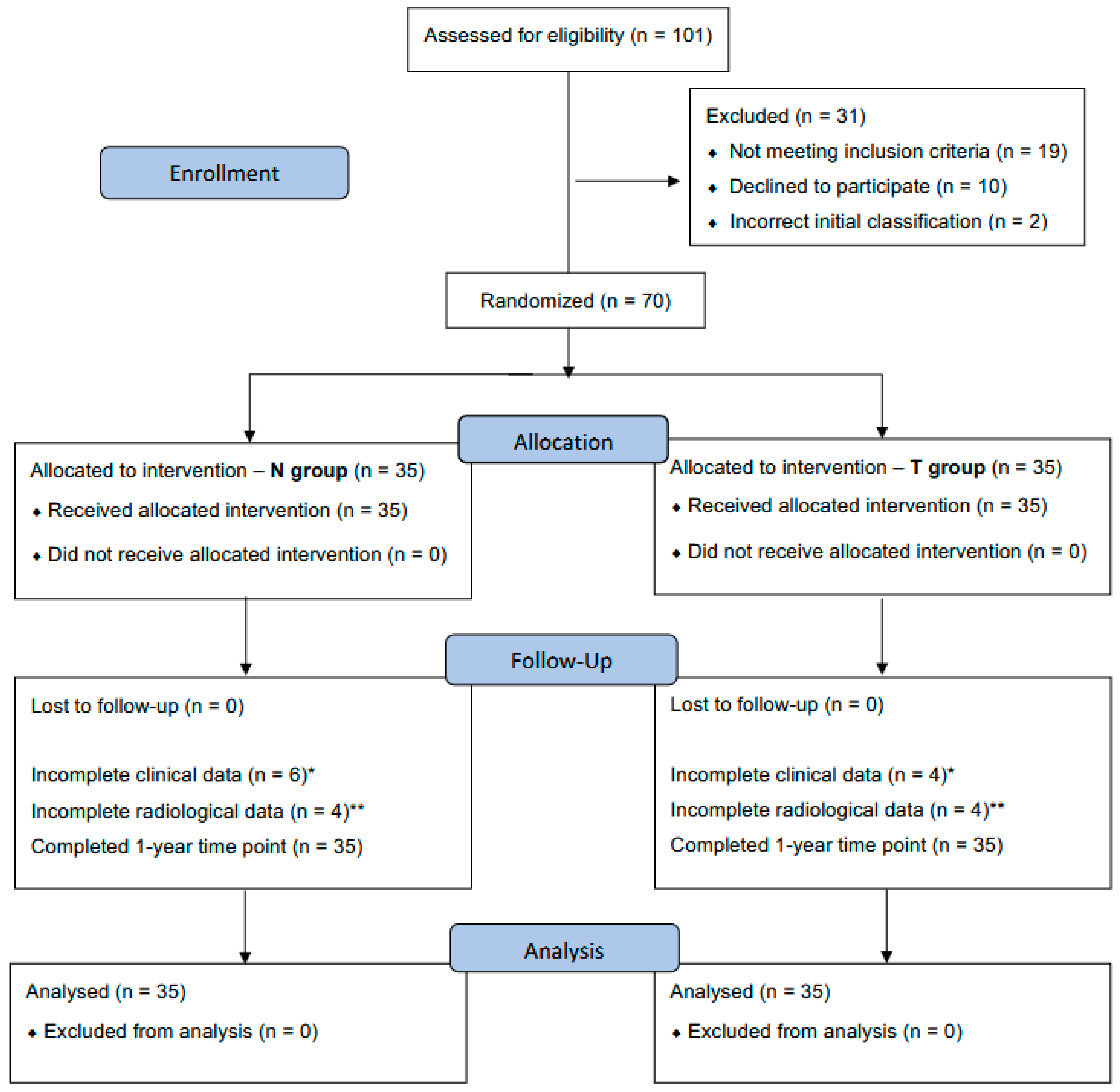
2.1. Patient Allocation, Study Design, and Eligibility Criteria
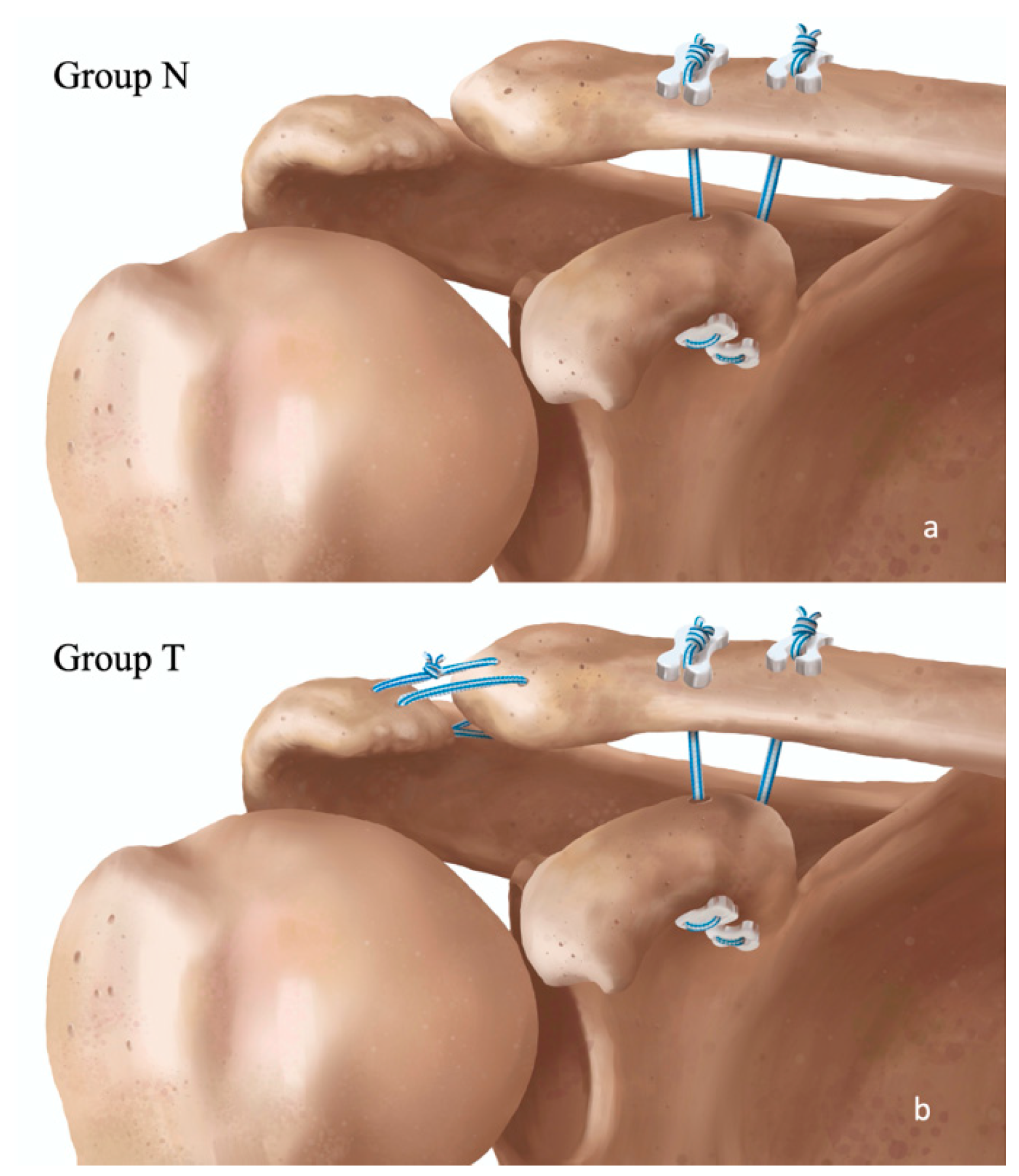
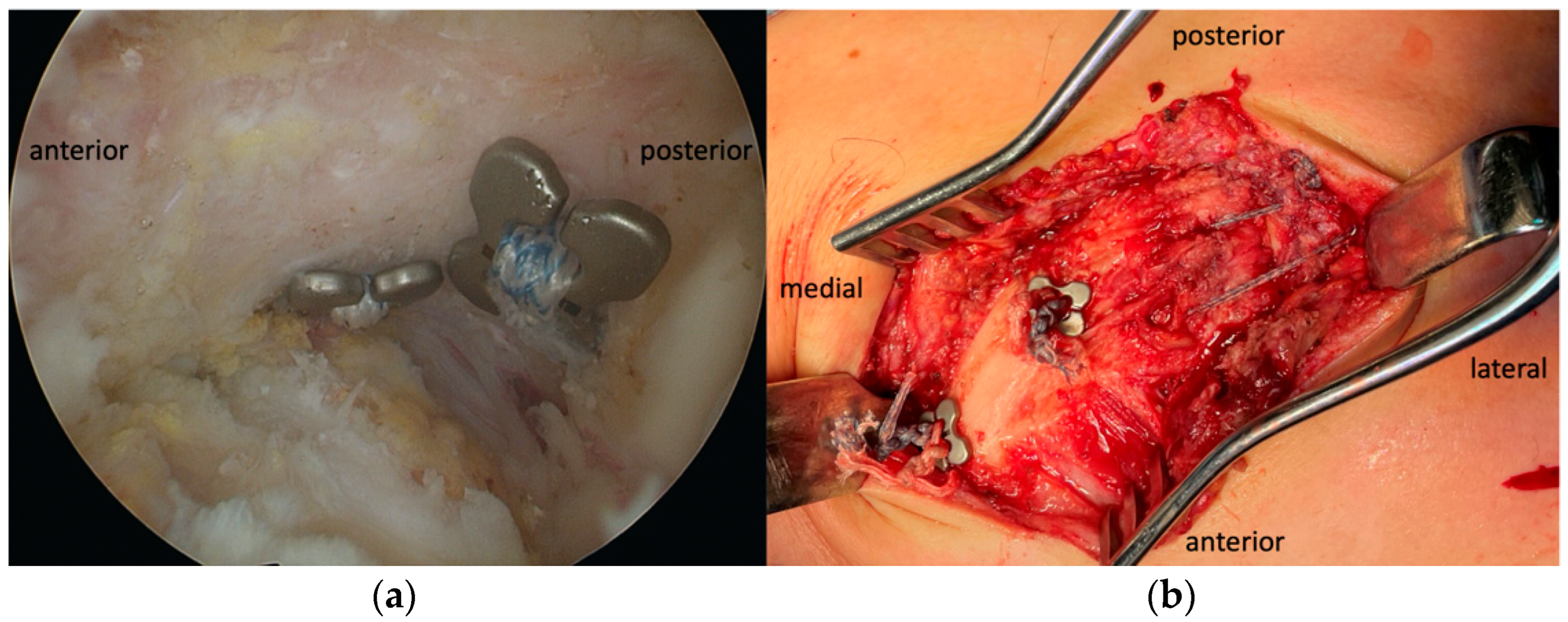
2.2. Surgical Technique
2.3. Postoperative Rehabilitation
2.4. Clinical Assessment
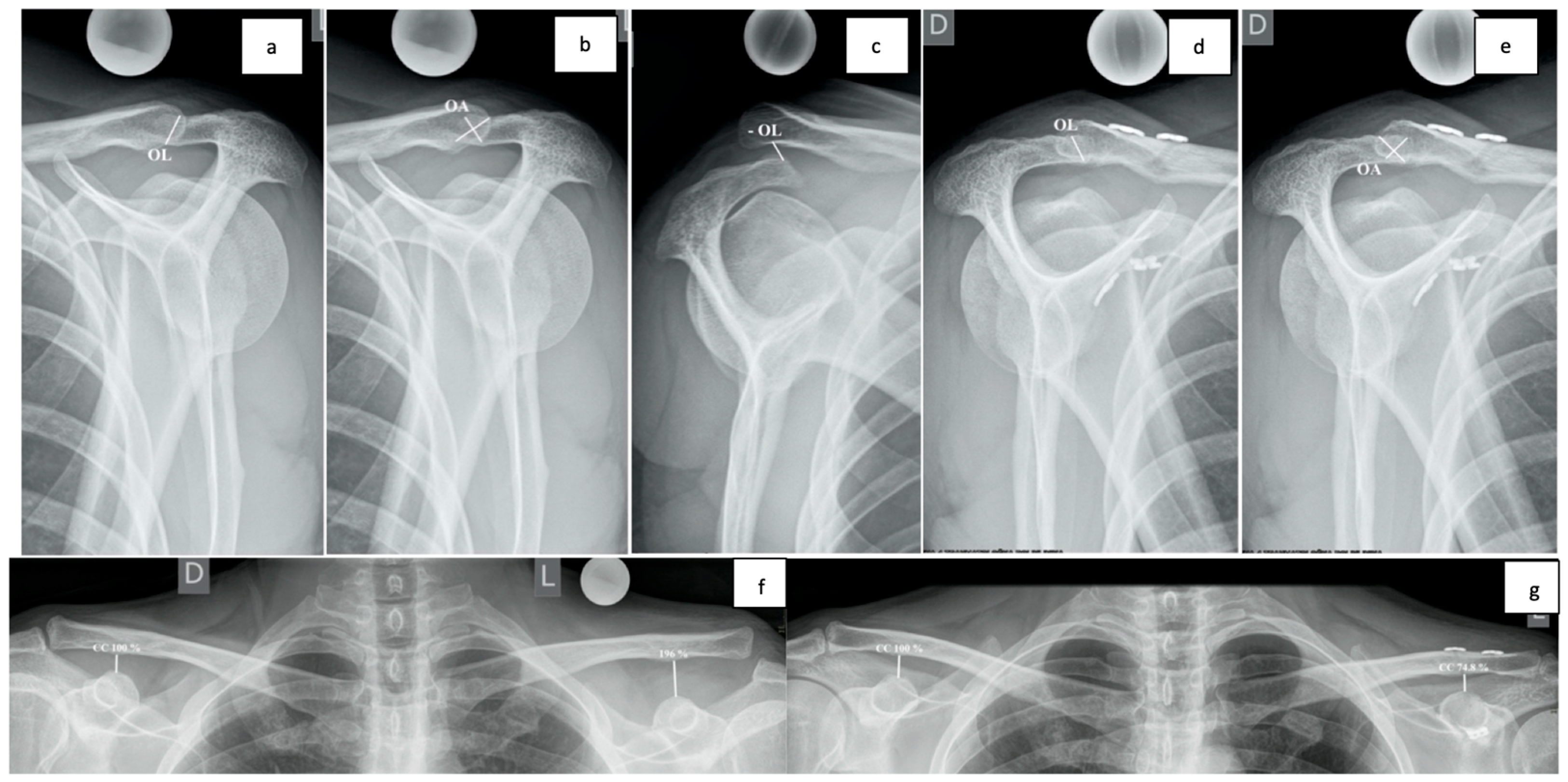
2.5. Radiological Assessment
2.6. General Assesment
2.7. Statistical Analysis
3. Results
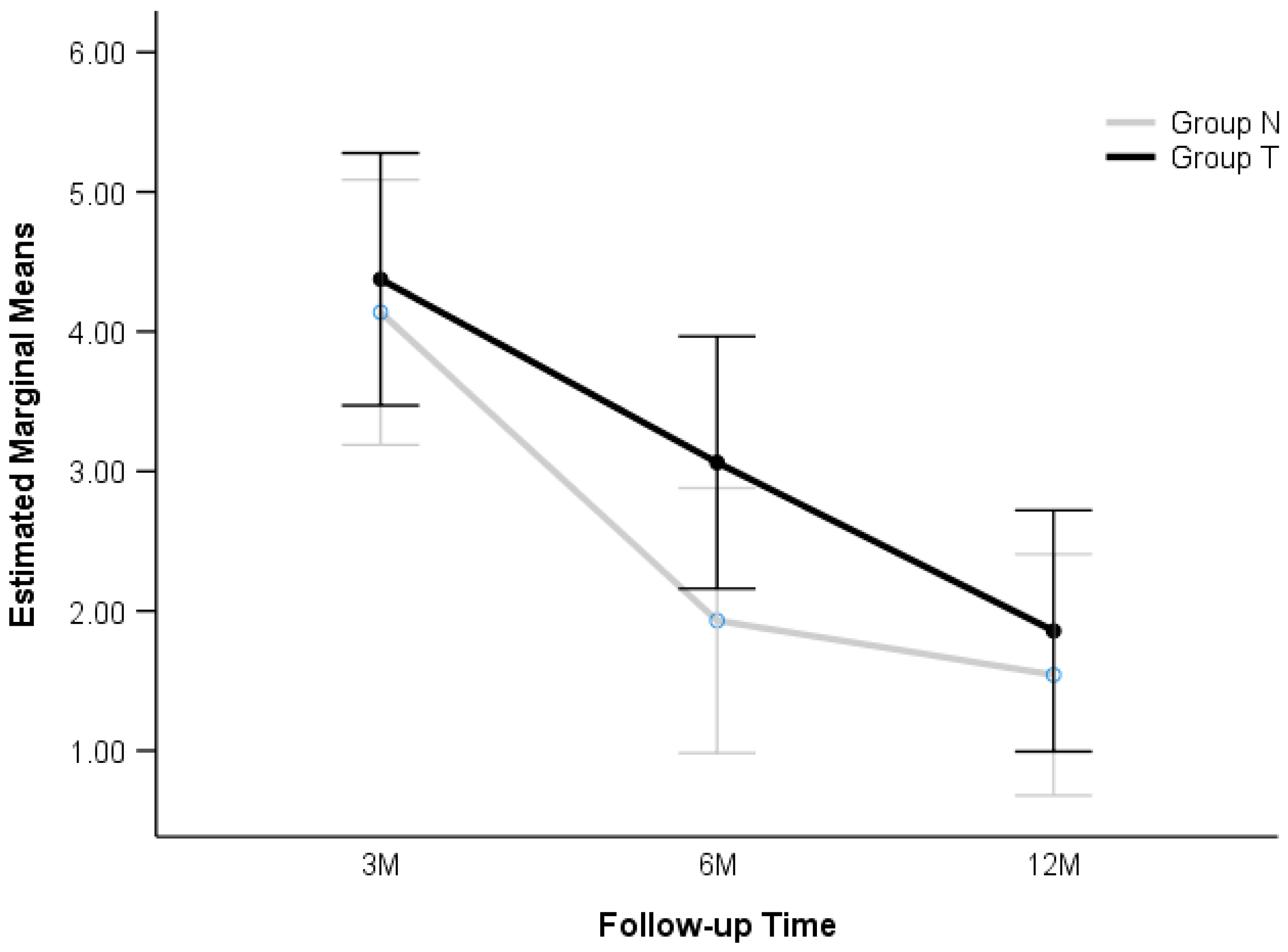
3.1. Functional Results
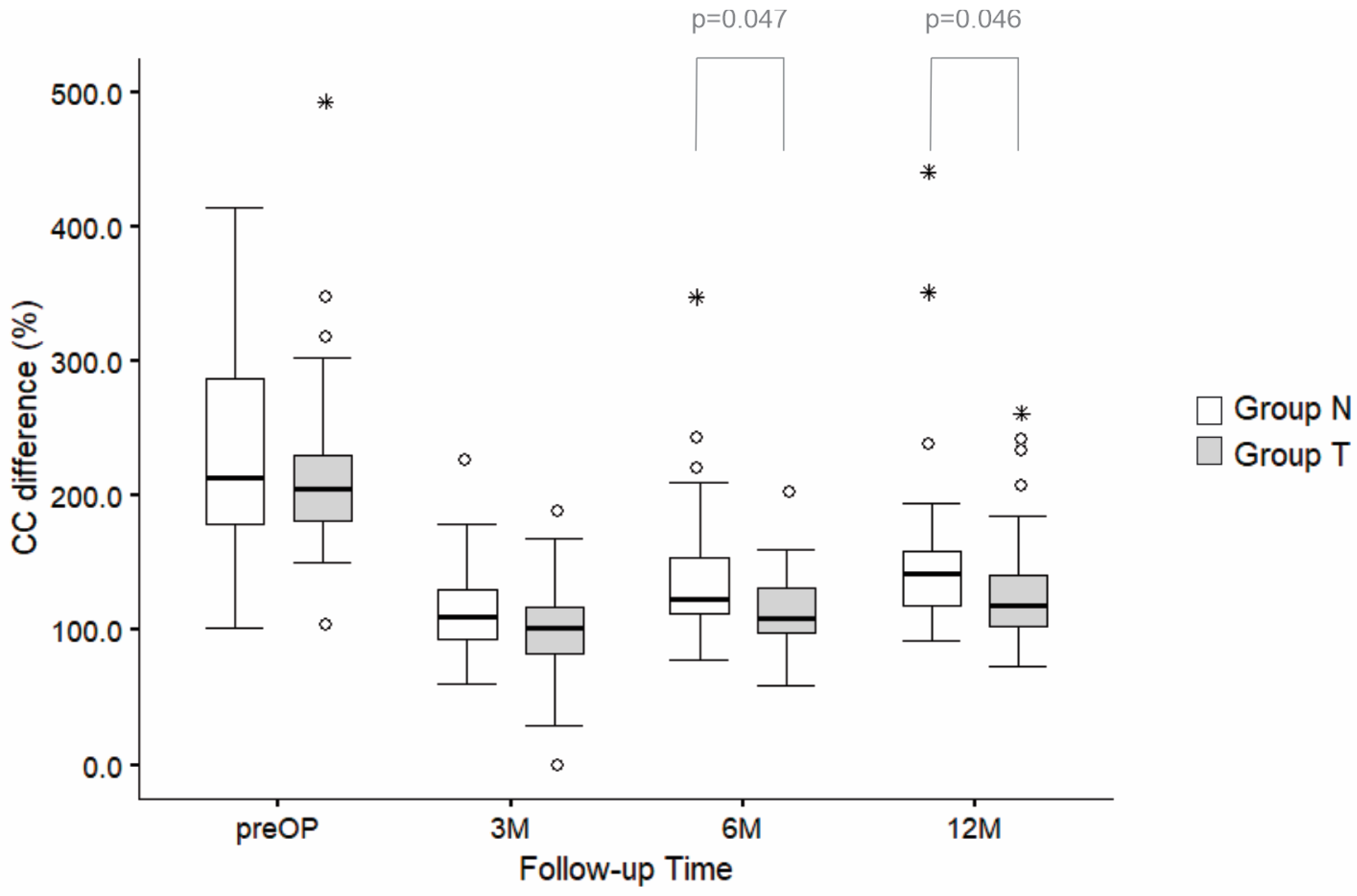
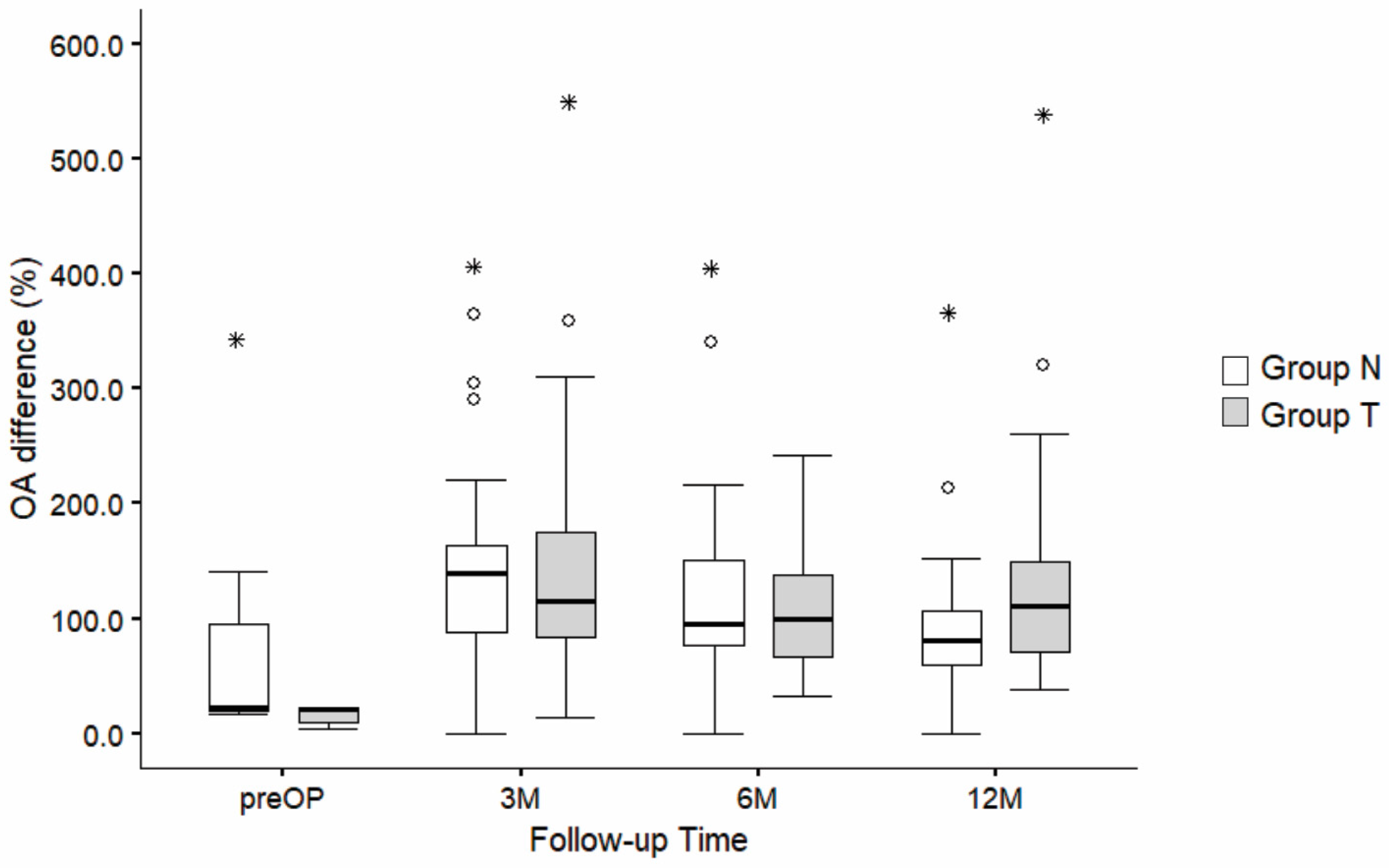
3.2. Radiological Results
3.3. CC Measurements
3.4. OL and OA Measurements
3.5. Complications
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mazzocca, A.D.; Arciero, R.A.; Bicos, J. Evaluation and Treatment of Acromioclavicular Joint Injuries. Am. J. Sports Med. 2007, 35, 316–329. [Google Scholar] [CrossRef] [PubMed]
- Pallis, M.; Cameron, K.L.; Svoboda, S.J.; Owens, B.D. Epidemiology of Acromioclavicular Joint Injury in Young Athletes. Am. J. Sports Med. 2012, 40, 2072–2077. [Google Scholar] [CrossRef] [PubMed]
- Nordqvist, A.; Petersson, C.J. Incidence and causes of shoulder girdle injuries in an urban population. J. Shoulder Elb. Surg. 1995, 4, 107–112. [Google Scholar] [CrossRef]
- Fraser-Moodie, J.A.; Shortt, N.L.; Robinson, C.M. Injuries to the acromioclavicular joint. J. Bone Jt. Surg. 2008, 90, 697–707. [Google Scholar] [CrossRef]
- Chillemi, C.; Franceschini, V.; Dei Giudici, L.; Alibardi, A.; Salate Santone, F.; Ramos Alday, L.J.; Osimani, M. Epidemiology of Isolated Acromioclavicular Joint Dislocation. Emerg. Med. Int. 2013, 2013, 171609. [Google Scholar] [CrossRef]
- Beitzel, K.; Cote, M.P.; Apostolakos, J.; Solovyova, O.; Judson, C.H.; Ziegler, C.G.; Edgar, C.M.; Imhoff, A.B.; Arciero, R.A.; Mazzocca, A.D. Current Concepts in the Treatment of Acromioclavicular Joint Dislocations. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 387–397. [Google Scholar] [CrossRef] [PubMed]
- Berthold, D.P.; Muench, L.N.; Dyrna, F.; Mazzocca, A.D.; Garvin, P.; Voss, A.; Scheiderer, B.; Siebenlist, S.; Imhoff, A.B.; Beitzel, K. Current concepts in acromioclavicular joint (AC) instability—A proposed treatment algorithm for acute and chronic AC-joint surgery. BMC Musculoskelet. Disord. 2022, 23, 1078. [Google Scholar] [CrossRef]
- Saccomanno, M.F.; Sircana, G.; Cardona, V.; Vismara, V.; Scaini, A.; Salvi, A.G.; Galli, S.; Marchi, G.; Milano, G. Biologic and synthetic ligament reconstructions achieve better functional scores compared to osteosynthesis in the treatment of acute acromioclavicular joint dislocation. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 2175–2193. [Google Scholar] [CrossRef]
- Stein, T.; Müller, D.; Blank, M.; Reinig, Y.; Saier, T.; Hoffmann, R.; Welsch, F.; Schweigkofler, U. Stabilization of Acute High-Grade Acromioclavicular Joint Separation: A Prospective Assessment of the Clavicular Hook Plate Versus the Double Double-Button Suture Procedure. Am. J. Sports Med. 2018, 46, 2725–2734. [Google Scholar] [CrossRef]
- Dyrna, F.; Berthold, D.P.; Feucht, M.J.; Muench, L.N.; Martetschläger, F.; Imhoff, A.B.; Mazzocca, A.D.; Beitzel, K. The importance of biomechanical properties in revision acromioclavicular joint stabilization: A scoping review. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3844–3855. [Google Scholar] [CrossRef]
- Choi, S.W.; Lee, T.J.; Moon, K.H.; Cho, K.J.; Lee, S.Y. Minimally Invasive Coracoclavicular Stabilization with Suture Anchors for Acute Acromioclavicular Dislocation. Am. J. Sports Med. 2008, 36, 961–965. [Google Scholar] [CrossRef] [PubMed]
- Beitzel, K.; Mazzocca, A.D.; Bak, K.; Itoi, E.; Kibler, W.B.; Mirzayan, R.; Imhoff, A.B.; Calvo, E.; Arce, G.; Shea, K. ISAKOS Upper Extremity Committee Consensus Statement on the Need for Diversification of the Rockwood Classification for Acromioclavicular Joint Injuries. Arthrosc. J. Arthrosc. Relat. Surg. 2014, 30, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Aliberti, G.M.; Kraeutler, M.J.; Trojan, J.D.; Mulcahey, M.K. Horizontal Instability of the Acromioclavicular Joint: A Systematic Review. Am. J. Sports Med. 2020, 48, 504–510. [Google Scholar] [CrossRef]
- Beris, A.; Lykissas, M.; Kostas-Agnantis, I.; Vekris, M.; Mitsionis, G.; Korompilias, A. Management of acute acromioclavicular joint dislocation with a double-button fixation system. Injury 2013, 44, 288–292. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, M.I.; Peebles, L.A.; Provencher, M.T.; LaPrade, R.F. Acromioclavicular and Coracoclavicular Ligament Reconstruction for Acromioclavicular Joint Instability. JBJS Essent. Surg. Tech. 2019, 9, e32. [Google Scholar] [CrossRef]
- Kraus, N.; Minkus, M.; Scheibel, M. Schultereckgelenksprengungen: Wann und wie sollten sie behandelt werden? Trauma Berufskrankh. 2014, 16, 251–257. [Google Scholar] [CrossRef]
- Martetschläger, F.; Tauber, M.; Habermeyer, P.; Selim, H.A. Arthroscopic Coracoclavicular and Acromioclavicular Stabilization of Acute Acromioclavicular Joint Dislocation By Suspensory Fixation System. Arthrosc. Tech. 2019, 8, e611–e615. [Google Scholar] [CrossRef]
- Scheibel, M.; Dröschel, S.; Gerhardt, C.; Kraus, N. Arthroscopically Assisted Stabilization of Acute High-Grade Acromioclavicular Joint Separations. Am. J. Sports Med. 2011, 39, 1507–1516. [Google Scholar] [CrossRef]
- Minkus, M.; Kraus, N.; Hann, C.; Scheibel, M. Arthroscopic Reconstruction After Acute Acromioclavicular Separation Injuries. JBJS Essent. Surg. Tech. 2017, 7, e7. [Google Scholar] [CrossRef]
- Theopold, J.; Schöbel, T.; Fischer, J.-P.; Löffler, S.; Osterhoff, G.; Schleifenbaum, S.; Hepp, P. Acromioclavicular joint reconstruction: An additional acromioclavicular cerclage does not improve horizontal stability in double coraco-clavicular tunnel technique. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3827–3834. [Google Scholar] [CrossRef]
- Maziak, N.; Audige, L.; Hann, C.; Minkus, M.; Scheibel, M. Factors Predicting the Outcome After Arthroscopically Assisted Stabilization of Acute High-Grade Acromioclavicular Joint Dislocations. Am. J. Sports Med. 2019, 47, 2670–2677. [Google Scholar] [CrossRef]
- Cisneros, L.N.; Reiriz, J.S. Prevalence of remaining horizontal instability in high-grade acromioclavicular joint injuries surgically managed. Eur. J. Orthop. Surg. Traumatol. 2017, 27, 323–333. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, K.; Craig, E.V.; An, K.N.; Cofield, R.H.; Chao, E.Y. Biomechanical study of the ligamentous system of the acromioclavicular joint. J. Bone Jt. Surg. 1986, 68, 434–440. [Google Scholar] [CrossRef]
- Dawson, P.A.; Adamson, G.J.; Pink, M.M.; Kornswiet, M.; Lin, S.; Shankwiler, J.A.; Lee, T.Q. Relative contribution of acromioclavicular joint capsule and coracoclavicular ligaments to acromioclavicular stability. J. Shoulder Elb. Surg. 2009, 18, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Debski, R.E.; Parsons, I.M.; Woo, S.L.-Y.; Fu, F.H. Effect of Capsular Injury on Acromioclavicular Joint Mechanics. J. Bone Jt. Surg. Am. Vol. 2001, 83, 1344–1351. [Google Scholar] [CrossRef] [PubMed]
- Dyrna, F.G.E.; Imhoff, F.B.; Voss, A.; Braun, S.; Obopilwe, E.; Apostolakos, J.M.; Morikawa, D.; Comer, B.; Imhoff, A.B.; Mazzocca, A.D.; et al. The Integrity of the Acromioclavicular Capsule Ensures Physiological Centering of the Acromioclavicular Joint Under Rotational Loading. Am. J. Sports Med. 2018, 46, 1432–1440. [Google Scholar] [CrossRef] [PubMed]
- Zumstein, M.A.; Schiessl, P.; Ambuehl, B.; Bolliger, L.; Weihs, J.; Maurer, M.H.; Moor, B.K.; Schaer, M.; Raniga, S. New quantitative radiographic parameters for vertical and horizontal instability in acromioclavicular joint dislocations. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 125–135. [Google Scholar] [CrossRef]
- Murphy, R.J.; Moor, B.K.; Lesniewski, P.J.; Hayoz, A.; Alcantara, W.; Zumstein, M.A. Evaluation of the Circles Measurement and the ABC Classification of Acromioclavicular Joint Injuries. Am. J. Sports Med. 2021, 49, 1619–1625. [Google Scholar] [CrossRef]
- Minkus, M.; Hann, C.; Scheibel, M.; Kraus, N. Quantification of dynamic posterior translation in modified bilateral Alexander views and correlation with clinical and radiological parameters in patients with acute acromioclavicular joint instability. Arch. Orthop. Trauma Surg. 2017, 137, 845–852. [Google Scholar] [CrossRef]
- Kraus, N.; Hann, C.; Gerhardt, C.; Scheibel, M. Dynamic instability of the acromioclavicular joint: A new classification for acute AC joint separation. Obere Extrem. 2018, 13, 279–285. [Google Scholar] [CrossRef]
- Saier, T.; Venjakob, A.J.; Minzlaff, P.; Föhr, P.; Lindell, F.; Imhoff, A.B.; Vogt, S.; Braun, S. Value of additional acromioclavicular cerclage for horizontal stability in complete acromioclavicular separation: A biomechanical study. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 1498–1505. [Google Scholar] [CrossRef] [PubMed]
- Jordan, R.W.; Malik, S.; Bentick, K.; Saithna, A. Acromioclavicular joint augmentation at the time of coracoclavicular ligament reconstruction fails to improve functional outcomes despite significantly improved horizontal stability. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3747–3763. [Google Scholar] [CrossRef] [PubMed]
- Sumanont, S.; Nopamassiri, S.; Boonrod, A.; Apiwatanakul, P.; Boonrod, A.; Phornphutkul, C. Acromioclavicular joint dislocation: A Dog Bone button fixation alone versus Dog Bone button fixation augmented with acromioclavicular repair—A finite element analysis study. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 1095–1101. [Google Scholar] [CrossRef] [PubMed]
- Hann, C.; Kraus, N.; Minkus, M.; Maziak, N.; Scheibel, M. Combined arthroscopically assisted coraco- and acromioclavicular stabilization of acute high-grade acromioclavicular joint separations. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 212–220. [Google Scholar] [CrossRef]
- Rosso, C.; Martetschläger, F.; Saccomanno, M.F.; Voss, A.; Lacheta, L.; ESA DELPHI Consensus Panel; Ângelo, A.C.; Antonogiannakis, E.; Azevedo, C.; Bak, K.; et al. High degree of consensus achieved regarding diagnosis and treatment of acromioclavicular joint instability among ESA-ESSKA members. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 2325–2332. [Google Scholar] [CrossRef]
- Barwood, S.A.; French, J.A.; Watson, L.A.; Balster, S.M.; Hoy, G.A.; Pizzari, T. The Specific AC Score (SACS): A new and validated method of assessment of isolated acromioclavicular joint pathology. J. Shoulder Elb. Surg. 2018, 27, 2214–2223. [Google Scholar] [CrossRef]
- Kukkonen, J.; Kauko, T.; Vahlberg, T.; Joukainen, A.; Äärimaa, V. Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. J. Shoulder Elb. Surg. 2013, 22, 1650–1655. [Google Scholar] [CrossRef]
- Bain, G.I.; Phadnis, J.; Itoi, E.; Di Giacomo, G.; Sugaya, H.; Sonnabend, D.H.; McLean, J. Shoulder crane: A concept of suspension, stability, control and motion. J. ISAKOS 2019, 4, 63–70. [Google Scholar] [CrossRef]
- Voss, A.; Löffler, T.; Reuter, S.; Imhoff, A.B.; Kellner, R.; Csapo, R.; Braun, S. Additional acromioclavicular cerclage limits lateral tilt of the scapula in patients with arthroscopically assisted coracoclavicular ligament reconstruction. Arch. Orthop. Trauma Surg. 2021, 141, 1331–1338. [Google Scholar] [CrossRef]
- Ângelo, A.C.; Maia Dias, C.; De Campos Azevedo, C. Combined Vertical, Horizontal, and Rotational Acromioclavicular Joint Stabilization: “Closing the Circle” Technique. Arthrosc. Tech. 2022, 11, e1479–e1486. [Google Scholar] [CrossRef]
- Minkus, M.; Maziak, N.; Moroder, P.; Scheibel, M. Arthroscopic low-profile reconstruction for acute acromioclavicular joint instability. Obere Extrem. 2019, 14, 60–65. [Google Scholar] [CrossRef]
- Gowd, A.K.; Liu, J.N.; Cabarcas, B.C.; Cvetanovich, G.L.; Garcia, G.H.; Manderle, B.J.; Verma, N.N. Current Concepts in the Operative Management of Acromioclavicular Dislocations: A Systematic Review and Meta-analysis of Operative Techniques. Am. J. Sports Med. 2019, 47, 2745–2758. [Google Scholar] [CrossRef] [PubMed]
- Berthold, D.P.; Muench, L.N.; Kadantsev, P.; Siebenlist, S.; Scheiderer, B.; Mazzocca, A.D.; Calvo, E.; Imhoff, A.B.; Beitzel, K.; Hinz, M. The importance of a structured failure analysis in revision acromioclavicular joint surgery: A multi-rater agreement on the causes of stabilization failure from the ISAKOS shoulder committee. J. ISAKOS 2023, 8, 425–429. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.-J.; Kim, N.-K. Complications After Arthroscopic Coracoclavicular Reconstruction Using a Single Adjustable–Loop-Length Suspensory Fixation Device in Acute Acromioclavicular Joint Dislocation. Arthrosc. J. Arthrosc. Relat. Surg. 2015, 31, 816–824. [Google Scholar] [CrossRef]
- Clavert, P.; Meyer, A.; Boyer, P.; Gastaud, O.; Barth, J.; Duparc, F. Complication rates and types of failure after arthroscopic acute acromioclavicular dislocation fixation. Prospective multicenter study of 116 cases. Orthop. Traumatol. Surg. Res. 2015, 101, S313–S316. [Google Scholar] [CrossRef]

| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
|
|
|
|
|
|
|
|
| Characteristic | Group N | Group T | p-Value |
|---|---|---|---|
| Gender (male:female) | 34:1 | 35:0 | / |
| Age (mean ± SD; years) | 42 ± 11 | 42 ± 11 | 0.889 |
| BMI (mean ± SD; kg/m2) | 27 ± 3 | 27 ± 3 | 0.680 |
| Time from injury to surgery (mean ± SD; days) | 10 ± 5 | 12 ± 6 | 0.381 |
| Side of injury (right:left; n (%)) | 19 (27.1): 16 (22.9) | 20 (28.6): 15 (21.4) | 0.500 |
| Rockwood classification (IIIb:V; n (%)) | 9 (12.9): 26 (37.1) | 12 (17.1): 23 (32.9) | 0.603 |
| Incidence of comorbidities (n (%)) | 6 (8.6) | 2 (2.9) | 0.133 |
| Smoking (n (%)) | 1 (1.4) | 1 (1.4) | 0.754 |
| Characteristic | Group N Mean ± SD | Group T Mean ± SD | p-Value |
|---|---|---|---|
| Constant (3 M) | 66 ± 18 | 62 ± 16 | 0.251 |
| Constant (6 M) | 83 ± 11 | 81 ± 10 | 0.309 |
| Constant (12 M) | 89 ± 9 | 89 ± 10 | 0.664 |
| SACS (3 M) | 36 ± 22 | 36 ± 18 | 0.787 |
| SACS (6 M) | 23 ± 16 | 24± 18 | 0.745 |
| SACS (12 M) | 14 ± 10 | 16 ± 13 | 0.518 |
| Clinical Horizontal Stability Assessment | Group N | Group T | p-Value |
|---|---|---|---|
| Stable (n (%)) | 19 (27.9%) | 28 (41.2%) | 0.061 |
| Partially unstable (n (%)) | 12 (17.6%) | 5 (7.4%) | |
| Completely unstable (n (%)) | 3 (4.4%) | 1 (1.5%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ambrožič, M.; Cimerman, M.; Omahen, K.; Jaklič, M.; Kralj-Iglič, V.; Kovačič, L. No Short-Term Effects of Acromioclavicular Joint Augmentation in Acute Acromioclavicular Joint Stabilization Surgery: A Randomized Controlled Clinical Trial on 70 Patients. J. Clin. Med. 2025, 14, 3161. https://doi.org/10.3390/jcm14093161
Ambrožič M, Cimerman M, Omahen K, Jaklič M, Kralj-Iglič V, Kovačič L. No Short-Term Effects of Acromioclavicular Joint Augmentation in Acute Acromioclavicular Joint Stabilization Surgery: A Randomized Controlled Clinical Trial on 70 Patients. Journal of Clinical Medicine. 2025; 14(9):3161. https://doi.org/10.3390/jcm14093161
Chicago/Turabian StyleAmbrožič, Miha, Matej Cimerman, Kristjan Omahen, Martina Jaklič, Veronika Kralj-Iglič, and Ladislav Kovačič. 2025. "No Short-Term Effects of Acromioclavicular Joint Augmentation in Acute Acromioclavicular Joint Stabilization Surgery: A Randomized Controlled Clinical Trial on 70 Patients" Journal of Clinical Medicine 14, no. 9: 3161. https://doi.org/10.3390/jcm14093161
APA StyleAmbrožič, M., Cimerman, M., Omahen, K., Jaklič, M., Kralj-Iglič, V., & Kovačič, L. (2025). No Short-Term Effects of Acromioclavicular Joint Augmentation in Acute Acromioclavicular Joint Stabilization Surgery: A Randomized Controlled Clinical Trial on 70 Patients. Journal of Clinical Medicine, 14(9), 3161. https://doi.org/10.3390/jcm14093161






