Risk Factors and Clinical Outcomes in Nonagenarians with Acute Coronary Syndrome: A Case-Control Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
4.1. Risk Factors for ACS Development
4.2. Differences According to ACS Groups
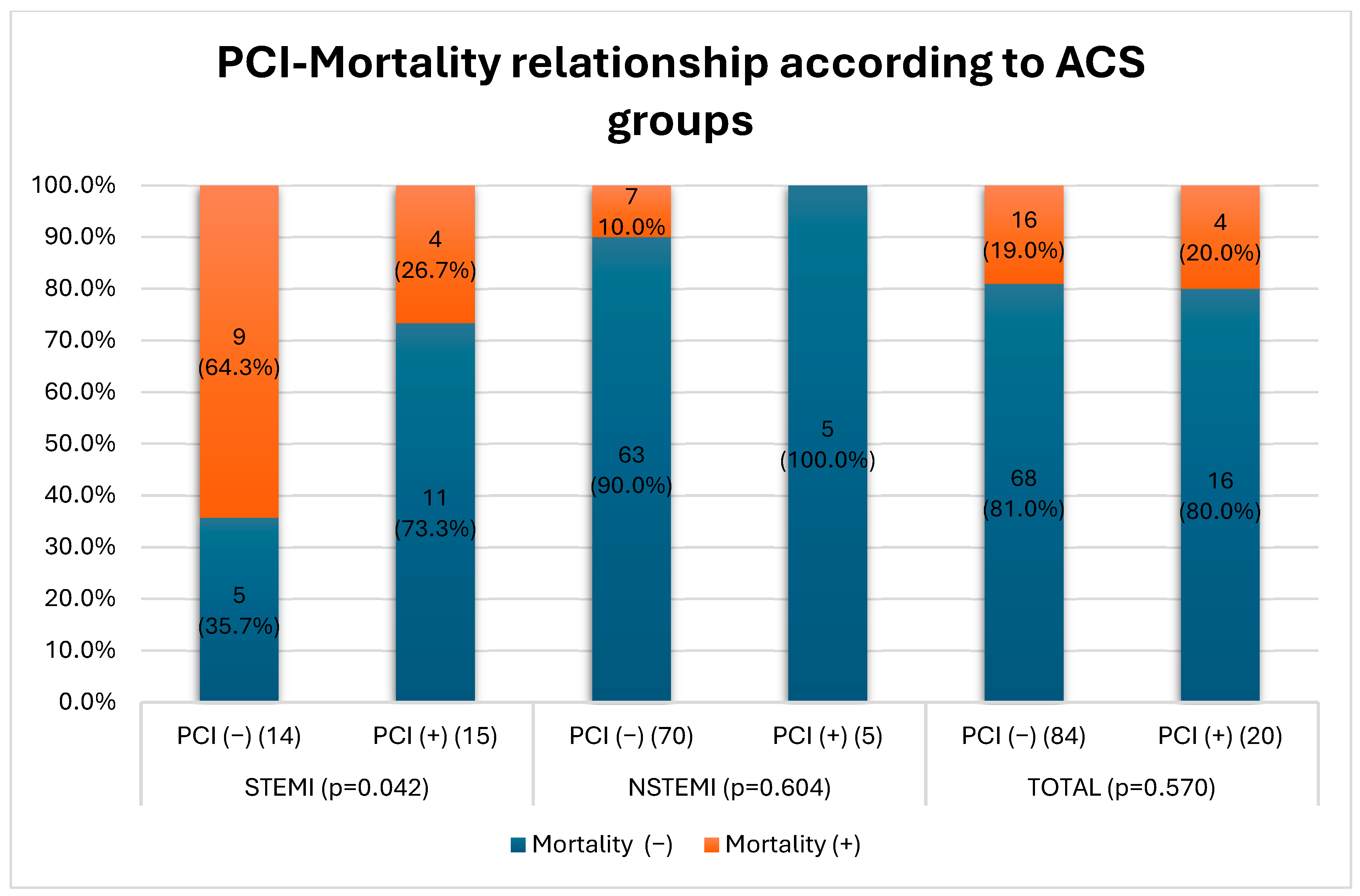
4.3. Invasive Treatment and Mortality Reduction
4.4. Limitations and Significance of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations. Population Division, Department of Economic and Social Affairs. In World Population Prospects 2024; Online Edition; United Nations: New York, NY, USA, 2024. [Google Scholar]
- Leucker, T.M.; Gerstenblith, G. (Eds.) Cardiovascular Disease in the Elderly; Contemporary Cardiology; Springer International Publishing: Cham, Switzertland, 2023; ISBN 978-3-031-16593-1. [Google Scholar]
- Mostaza, J.M.; Lahoz, C.; Salinero-Fort, M.A.; Cardenas, J. Cardiovascular Disease in Nonagenarians: Prevalence and Utilization of Preventive Therapies. Eur. J. Prev. Cardiolog. 2019, 26, 356–364. [Google Scholar] [CrossRef] [PubMed]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Beaton, A.Z.; Boehme, A.K.; Buxton, A.E.; et al. Heart Disease and Stroke Statistics—2023 Update: A Report From the American Heart Association. Circulation 2023, 147, e153–e639. [Google Scholar] [CrossRef]
- Rich, M.W. Epidemiology, Clinical Features, and Prognosis of Acute Myocardial Infarction in the Elderly. Am. J. Geri. Cardiol. 2006, 15, 7–13. [Google Scholar] [CrossRef]
- Forman, D.E.; Maurer, M.S.; Boyd, C.; Brindis, R.; Salive, M.E.; Horne, F.M.; Bell, S.P.; Fulmer, T.; Reuben, D.B.; Zieman, S. Multimorbidity in Older Adults with Cardiovascular Disease. J. Am. Coll. Cardiol. 2018, 71, 2149–2161. [Google Scholar] [CrossRef] [PubMed]
- Couture, E.L.; Farand, P.; Nguyen, M.; Allard, C.; Wells, G.A.; Mansour, S.; Rinfret, S.; Afilalo, J.; Eisenberg, M.; Montigny, M.; et al. Impact of an Invasive Strategy in the Elderly Hospitalized with Acute Coronary Syndrome with Emphasis on the Nonagenarians. Catheter. Cardiovasc. Interv. 2018, 92, E441–E448. [Google Scholar] [CrossRef]
- Shah, P.; Najafi, A.H.; Panza, J.A.; Cooper, H.A. Outcomes and Quality of Life in Patients ≥85 Years of Age With ST-Elevation Myocardial Infarction. Am. J. Cardiol. 2009, 103, 170–174. [Google Scholar] [CrossRef] [PubMed]
- Cepas-Guillén, P.L.; Echarte-Morales, J.; Caldentey, G.; Gómez, E.M.; Flores-Umanzor, E.; Borrego-Rodriguez, J.; Llagostera, M.; Viana Tejedor, A.; Vidal, P.; Benito-Gonzalez, T.; et al. Outcomes of Nonagenarians with Acute Coronary Syndrome. J. Am. Med. Dir. Assoc. 2022, 23, 81–86.e4. [Google Scholar] [CrossRef] [PubMed]
- Goel, K.; Gupta, T.; Gulati, R.; Bell, M.R.; Kolte, D.; Khera, S.; Bhatt, D.L.; Rihal, C.S.; Holmes, D.R. Temporal Trends and Outcomes of Percutaneous Coronary Interventions in Nonagenarians. JACC Cardiovasc. Interv. 2018, 11, 1872–1882. [Google Scholar] [CrossRef]
- Jokhadar, M.; Wenger, N.K. Review of the Treatment of Acute Coronary Syndrome in Elderly Patients. Clin. Interv. Aging 2009, 2009, 435–444. [Google Scholar] [CrossRef][Green Version]
- Zimmerman, F.H.; Cameron, A.; Fisher, L.D.; Grace, N. Myocardial Infarction in Young Adults: Angiographic Characterization, Risk Factors and Prognosis (Coronary Artery Surgery Study Registry). J. Am. Coll. Cardiol. 1995, 26, 654–661. [Google Scholar] [CrossRef]
- Ferrucci, L.; Fabbri, E. Inflammageing: Chronic Inflammation in Ageing, Cardiovascular Disease, and Frailty. Nat. Rev. Cardiol. 2018, 15, 505–522. [Google Scholar] [CrossRef]
- Liberale, L.; Montecucco, F.; Tardif, J.-C.; Libby, P.; Camici, G.G. Inflamm-Ageing: The Role of Inflammation in Age-Dependent Cardiovascular Disease. Eur. Heart J. 2020, 41, 2974–2982. [Google Scholar] [CrossRef] [PubMed]
- García-Blas, S.; Cordero, A.; Diez-Villanueva, P.; Martinez-Avial, M.; Ayesta, A.; Ariza-Solé, A.; Mateus-Porta, G.; Martínez-Sellés, M.; Escribano, D.; Gabaldon-Perez, A.; et al. Acute Coronary Syndrome in the Older Patient. J. Clin. Med. 2021, 10, 4132. [Google Scholar] [CrossRef] [PubMed]
- Kannel, W.B. Factors of Risk in the Development of Coronary Heart Disease—Six-Year Follow-up Experience: The Framingham Study. Ann. Intern. Med. 1961, 55, 33. [Google Scholar] [CrossRef]
- Kannel, W.B. Coronary Heart Disease Risk Factors in the Elderly. Am. J. Geriatr. Cardiol. 2002, 11, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Wenger, N.K. Dyslipidemia as a Risk Factor at Elderly Age. Am. J. Geriatr. Cardiol. 2004, 13, 4–9. [Google Scholar]
- Krumholz, H.M.; Seeman, T.E.; Merrill, S.S.; de Leon, C.F.M.; Vaccarino, V.; Silverman, D.I.; Tsukahara, R.; Ostfeld, A.M.; Berkman, L.F. Lack of Association between Cholesterol and Coronary Heart Disease Mortality and Morbidity and All-Cause Mortality in Persons Older than 70 Years. JAMA 1994, 272, 1335–1340. [Google Scholar] [CrossRef]
- Ravnskov, U.; Diamond, D.M.; Hama, R.; Hamazaki, T.; Hammarskjöld, B.; Hynes, N.; Kendrick, M.; Langsjoen, P.H.; Malhotra, A.; Mascitelli, L.; et al. Lack of an Association or an Inverse Association between Low-Density-Lipoprotein Cholesterol and Mortality in the Elderly: A Systematic Review. BMJ Open 2016, 6, e010401. [Google Scholar] [CrossRef]
- Madhavan, M.V.; Gersh, B.J.; Alexander, K.P.; Granger, C.B.; Stone, G.W. Coronary Artery Disease in Patients ≥ 80 Years of Age. J. Am. Coll. Cardiol. 2018, 71, 2015–2040. [Google Scholar] [CrossRef]
- Liu, X.-M.; Ma, C.-S.; Liu, X.-H.; Du, X.; Kang, J.-P.; Zhang, Y.; Wu, J.-H. Relationship between Red Blood Cell Distribution Width and Intermediate-Term Mortality in Elderly Patients after Percutaneous Coronary Intervention. J. Geriatr. Cardiol. 2015, 12, 17. [Google Scholar]
- Xanthopoulos, A.; Tryposkiadis, K.; Dimos, A.; Bourazana, A.; Zagouras, A.; Iakovis, N.; Papamichalis, M.; Giamouzis, G.; Vassilopoulos, G.; Skoularigis, J.; et al. Red Blood Cell Distribution Width in Elderly Hospitalized Patients with Cardiovascular Disease. World J. Cardiol. 2021, 13, 503–513. [Google Scholar] [CrossRef]
- Weijenberg, M.P.; Feskens, E.J.M.; Kromhout, D. White Blood Cell Count and the Risk of Coronary Heart Disease and All-Cause Mortality in Elderly Men. Arterioscler. Thromb. Vasc. Biol. 1996, 16, 499–503. [Google Scholar] [CrossRef]
- Yayan, J. Association of Traditional Risk Factors with Coronary Artery Disease in Nonagenarians: The Primary Role of Hypertension. Clin. Interv. Aging 2014, 9, 2003–2012. [Google Scholar] [CrossRef]
- Di Stefano, R.; Di Bello, V.; Barsotti, M.C.; Grigoratos, C.; Armani, C.; Dell’Omodarme, M.; Carpi, A.; Balbarini, A. Inflammatory Markers and Cardiac Function in Acute Coronary Syndrome: Difference in ST-Segment Elevation Myocardial Infarction (STEMI) and in Non-STEMI Models. Biomed. Pharmacother. 2009, 63, 773–780. [Google Scholar] [CrossRef]
- Sugiyama, T.; Hasegawa, K.; Kobayashi, Y.; Takahashi, O.; Fukui, T.; Tsugawa, Y. Differential Time Trends of Outcomes and Costs of Care for Acute Myocardial Infarction Hospitalizations by ST Elevation and Type of Intervention in the United States, 2001–2011. J. Am. Heart Assoc. 2015, 4, e001445. [Google Scholar] [CrossRef] [PubMed]
- Sheldon, M.; Blankenship, J.C. STEMI in Nonagenarians: Never Too Old. Catheter. Cardiovasc. Interv. 2022, 100, 17–18. [Google Scholar] [CrossRef] [PubMed]
- From, A.M.; Rihal, C.S.; Lennon, R.J.; Holmes, D.R.; Prasad, A. Temporal Trends and Improved Outcomes of Percutaneous Coronary Revascularization in Nonagenarians. JACC Cardiovasc. Interv. 2008, 1, 692–698. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kunadian, V.; Mossop, H.; Shields, C.; Bardgett, M.; Watts, P.; Teare, M.D.; Pritchard, J.; Adams-Hall, J.; Runnett, C.; Ripley, D.P.; et al. Invasive Treatment Strategy for Older Patients with Myocardial Infarction. N. Engl. J. Med. 2024, 391, 1673–1684. [Google Scholar] [CrossRef]
- Sawant, A.C.; Josey, K.; Plomondon, M.E.; Maddox, T.M.; Bhardwaj, A.; Singh, V.; Rajagopalan, B.; Said, Z.; Bhatt, D.L.; Corbelli, J. Temporal Trends, Complications, and Predictors of Outcomes Among Nonagenarians Undergoing Percutaneous Coronary Intervention. JACC Cardiovasc. Interv. 2017, 10, 1295–1303. [Google Scholar] [CrossRef]
- Tokarek, T.; Siudak, Z.; Dziewierz, A.; Rakowski, T.; Krycińska, R.; Siwiec, A.; Dudek, D. Clinical Outcomes in Nonagenarians Undergoing a Percutaneous Coronary Intervention: Data from the ORPKI Polish National Registry 2014–2016. Coron. Artery Dis. 2018, 29, 573–578. [Google Scholar] [CrossRef]
- Antonsen, L.; Jensen, L.O.; Terkelsen, C.J.; Tilsted, H.; Junker, A.; Maeng, M.; Hansen, K.N.; Lassen, J.F.; Thuesen, L.; Thayssen, P. Outcomes after Primary Percutaneous Coronary Intervention in Octogenarians and Nonagenarians with ST-segment Elevation Myocardial Infarction: From the Western Denmark Heart Registry. Catheter. Cardiovasc. Interv. 2013, 81, 912–919. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.; Jeong, M.H.; Cho, K.H.; Kim, M.C.; Sim, D.S.; Hong, Y.J.; Kim, J.H.; Ahn, Y. Outcomes of Nonagenarians with Acute Myocardial Infarction with or without Coronary Intervention. J. Clin. Med. 2022, 11, 1593. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.H.; Ahn, Y.; Kim, S.S.; Rhew, S.H.; Jeong, Y.W.; Jang, S.Y.; Cho, J.Y.; Jeong, H.C.; Park, K.-H.; Yoon, N.S.; et al. Characteristics, In-Hospital and Long-Term Clinical Outcomes of Nonagenarian Compared with Octogenarian Acute Myocardial Infarction Patients. J. Korean Med. Sci. 2014, 29, 527. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.-J.; Hou, C.J.-Y.; Chou, Y.-S.; Tsai, C.-H. Percutaneous Coronary Intervention in Nonagenarians. Acta Cardiol. Sin. 2004, 20, 73–82. [Google Scholar]
- Sahin, M.; Ocal, L.; Kalkan, A.K.; Kilicgedik, A.; Kalkan, M.E.; Teymen, B.; Arslantas, U.; Turkmen, M.M. In-Hospital and Long Term Results of Primary Angioplasty and Medical Therapy in Nonagenarian Patients with Acute Myocardial Infarction. J. Cardiovasc. Thorac. Res. 2017, 9, 147–151. [Google Scholar] [CrossRef]

| CONTROL | ACS | p | |
|---|---|---|---|
| n | 113 (52.3) | 104 (47.7) | |
| Age | 91 ± 2.2 | 91.3 ± 1.8 | 0.302 |
| Male | 40 (35.4) | 38 (36.5) | 0.861 |
| BMI | 26.6 ± 3.3 | 26.9 ± 4.8 | 0.896 |
| Smoking | 35 (31.0) | 38 (36.9) | 0.358 |
| HT | 91 (80.5) | 72 (69.9) | 0.070 |
| DM | 27 (23.9) | 25 (24.0) | 0.980 |
| Family history | 51 (45.1) | 33 (32.0) | 0.049 |
| Biochemical Parameters | |||
| Hgb(g/dL) | 12.4 ± 1.4 | 11.8 ± 1.8 | 0.008 |
| MCV (fL) | 89.6 ± 6.9 | 87.4 ± 6.8 | 0.009 |
| RDW (%) | 15.1 ± 1.9 | 15.6 ± 2.0 | 0.020 |
| WBC (103/µL) | 7.2 ± 1.7 | 10.1 ± 3.7 | <0.001 |
| PLT (103/µL) | 229.2 ± 77.9 | 232.5 ± 82.4 | 0.902 |
| MPV (fL) | 9.4 ± 1.9 | 8.7 ± 1.5 | 0.021 |
| Glucose (mg/dL) | 111.3 ± 32.0 | 152.9 ± 71.7 | <0.001 |
| HbA1c (%) | 6.23 ± 0.9 | 6.29 ± 1.01 | 0.910 |
| Creatinine (mg/dL) | 1.09 ± 0.3 | 1.16 ± 0.52 | 0.517 |
| Lipid Profiles | |||
| TC (mg/dL) | 197.9 ± 44.1 | 179.6 ± 42.7 | 0.003 |
| LDL (mg/dL) | 119.7 ±36.9 | 115.0 ± 36.2 | 0.272 |
| TG (mg/dL) | 114.6 ± 47.7 | 123.4 ± 47.7 | 0.612 |
| HDL (mg/dL) | 55.5 ± 15.9 | 38.6 ± 12.1 | <0.001 |
| AIP | 0.299 ± 0.24 | 0.485 ± 0.264 | <0.001 |
| NSTEMI | STEMI | p | |
|---|---|---|---|
| n | 75 (72.1) | 29 (27.9) | |
| Age | 91.3 ± 2.1 | 90.8 ± 1.40 | 0.442 |
| Male | 24 (32) | 14 (48.3) | 0.122 |
| BMI | 27.1 ± 5.6 | 27.4 ± 3.1 | 0.865 |
| Smoking | 26 (35.1) | 12 (41.4) | 0.555 |
| HT | 55 (74.3) | 17 (58.6) | 0.118 |
| DM | 21 (28.0) | 4 (13.8) | 0.128 |
| Family history | 15 (20.3) | 18 (62.1) | <0.001 |
| Biochemical Parameters | |||
| Hgb | 11.9 ± 1.8 | 11.2 ± 1.8 | 0.142 |
| MCV (fL) | 86.6 ± 6.7 | 87.7 ± 8.3 | 0.893 |
| RDW (%) | 15.4 ± 1.8 | 16.1 ± 2.8 | 0.324 |
| WBC (103/µL) | 9.78 ± 3.70 | 11.48 ± 4.20 | 0.030 |
| PLT (103/µL) | 233.5 ± 90.3 | 231.2 ± 59.1 | 0.798 |
| MPV (fL) | 8.93 ± 1.60 | 8.31 ± 1.03 | 0.721 |
| Glucose (mg/dL) | 152.5 ± 73.9 | 145.4 ± 67.5 | 0.364 |
| HbA1c (%) | 6.40 ± 0.99 | 6.15 ± 1.14 | 0.422 |
| Creatinine (mg/dL) | 1.12 ± 0.52 | 1.18 ± 0.48 | 0.522 |
| Lipid Profiles | |||
| TC (mg/dL) | 177.4 ± 38.7 | 187.3 ± 54.9 | 0.461 |
| LDL (mg/dL) | 112.2 ± 33.4 | 124.9 ± 44.4 | 0.167 |
| TG (mg/dL) | 127.7 ± 70.7 | 108.0 ± 41.9 | 0.285 |
| HDL (mg/dL) | 39.1 ± 12.5 | 36.9 ± 10.9 | 0.426 |
| AIP | 0.486 ± 0.284 | 0.460 ± 0.182 | 0.627 |
| CAG | 8 (10.7) | 19 (65.5) | <0.001 |
| PCI | 5 (6.7) | 15 (51.7) | <0.001 |
| Length of hospital stay (days) | 5.7 ± 4.3 | 6.6 ± 4.1 | 0.781 |
| Mortality | 7 (9.3) | 13 (44.8) | <0.001 |
| ACS | ||
|---|---|---|
| 95% CI | p | |
| Sex | 0.905 (0.482–1.699) | 0.755 |
| Family history | 0.492 (0.264–0.917) | 0.026 |
| Smoking | 1.868 (0.955–3.655) | 0.068 |
| HT | 0.525 (0.268–1.027) | 0.060 |
| DM | 1.038 (0.533–2.024) | 0.912 |
| Dyslipidemia | 1.953 (1.034–3.692) | 0.039 |
| Obesity | 1.777 (0.856–3.687) | 0.123 |
| Crude OR | Adjusted OR | ||
|---|---|---|---|
| Model 0 OR (95% CI) p-Value | Model 1 OR (95% CI) p-Value | Model 2 OR (95% CI) p-Value | |
| High LDL | 0.544 (0.287–1.033) 0.063 | 0.528 (0.277–1.009) 0.053 | 0.440 (0.222–0.872) 0.019 |
| LDL (per 10 mg/dL increase) | 1.023 (0.926–1.130) 0.656 | 1.016 (0.918–1.123) 0.765 | 0.997 (0.897–1.110) 0.963 |
| High TG | 1.054 (0.460–2.416) 0.901 | 0.980 (0.416–2.307) 0.962 | 1.047 (0.424–2.585) 0.921 |
| TG (per 10 mg/dL increase) | 1.046 (0.888–1.231) 0.594 | 1.036 (0.881–1.217) 0.669 | 1.027 (0.860–1.226) 0.770 |
| Low HDL | 5.534 (2.615–11.713) <0.001 | 5.619 (2.648–11.921) <0.001 | 5.554 (2.536–12.160) <001 |
| HDL (per 10 mg/dL increase) | 0.280 (0.143–0.546) < 0.001 | 0.271 (0.139–0.528) < 0.001 | 0.274 (0.134–0.562) < 0.001 |
| High AIP | 0.933 (0.406–2.142) 0.869 | 0.955 (0.415–2.202) 0.915 | 1.061 (0.439–2.564) 0.895 |
| AIP (per 1 unit increase) | 0.055 (0.000–12.083) 0.292 | 0.054 (0.000–11.218) 0.204 | 0.078 (0.000–25.293) 0.387 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Demirbaş, Z.E.; Zeren, G.; Can, F.; Karabay, C.Y. Risk Factors and Clinical Outcomes in Nonagenarians with Acute Coronary Syndrome: A Case-Control Study. J. Clin. Med. 2025, 14, 1761. https://doi.org/10.3390/jcm14051761
Demirbaş ZE, Zeren G, Can F, Karabay CY. Risk Factors and Clinical Outcomes in Nonagenarians with Acute Coronary Syndrome: A Case-Control Study. Journal of Clinical Medicine. 2025; 14(5):1761. https://doi.org/10.3390/jcm14051761
Chicago/Turabian StyleDemirbaş, Zeynep Ece, Gönül Zeren, Fatma Can, and Can Yücel Karabay. 2025. "Risk Factors and Clinical Outcomes in Nonagenarians with Acute Coronary Syndrome: A Case-Control Study" Journal of Clinical Medicine 14, no. 5: 1761. https://doi.org/10.3390/jcm14051761
APA StyleDemirbaş, Z. E., Zeren, G., Can, F., & Karabay, C. Y. (2025). Risk Factors and Clinical Outcomes in Nonagenarians with Acute Coronary Syndrome: A Case-Control Study. Journal of Clinical Medicine, 14(5), 1761. https://doi.org/10.3390/jcm14051761








