The Inlay Technique in Alveolar Ridge Augmentation: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
((inlay [tiab] OR sandwich [tiab] OR interpositional [tiab])AND (technique [tiab] OR approach [tiab] OR procedure [tiab] OR graft [tiab] OR)) AND (oral [tiab] OR alveolar [tiab] OR maxillofacial [tiab] OR dental [tiab] OR “Oral Surgical Procedures” [MeSH])
2.2. Inclusion and Exclusion Criteria
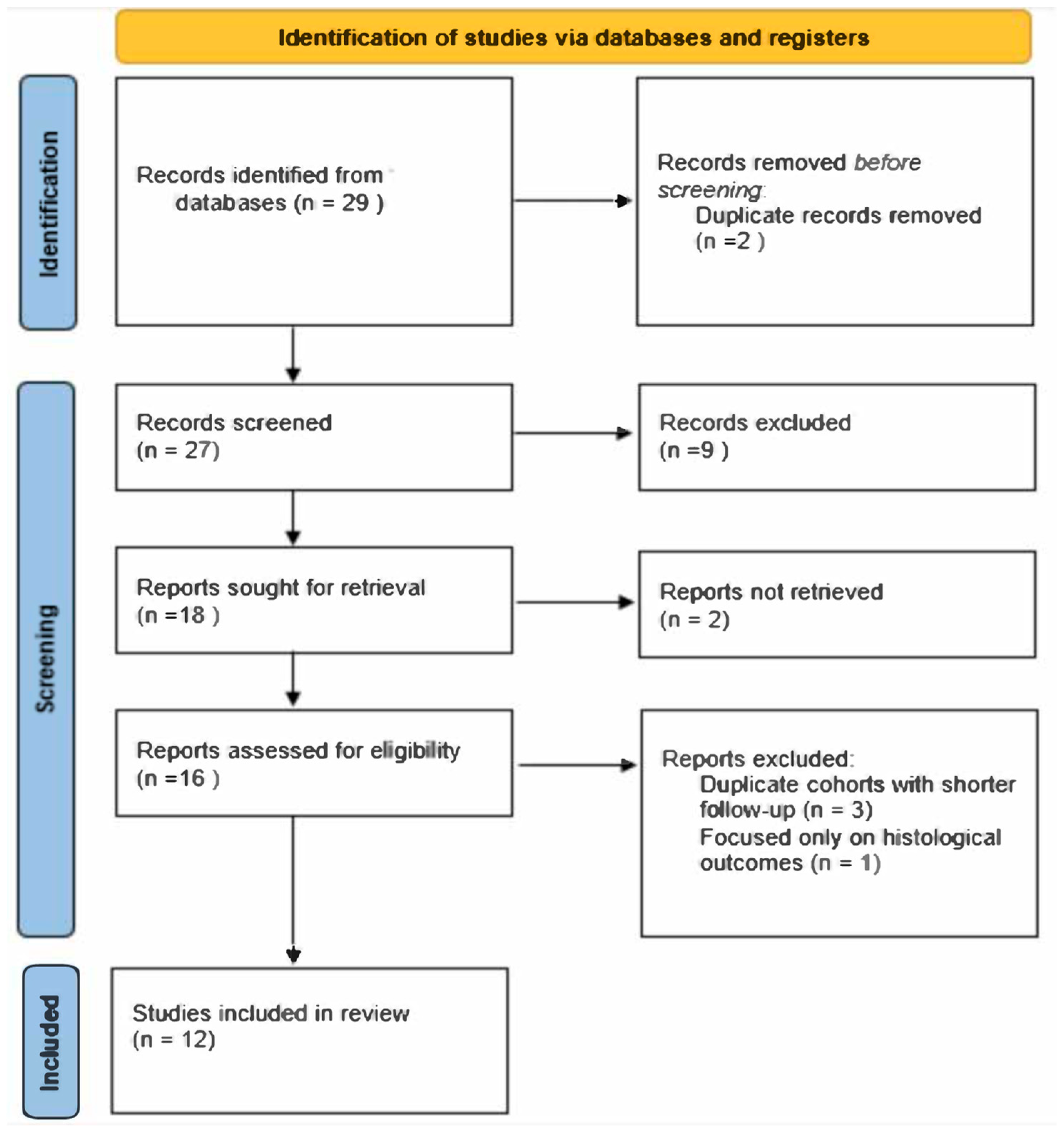
2.3. Article Selection Process
2.4. Data Extraction and Quality Assessment
3. Results
3.1. Implant Survival Rate
3.2. Vertical Bone Gain
3.3. Complications
3.4. Marginal Bone Loss (MBL)
3.5. Study Limitation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MBL | Marginal bone loss |
| RCT | Randomized controlled trial |
| CI | Confidence interval |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| CAD/CAM | Computer-aided design/computer-aided manufacturing |
References
- Cucchi, A.; Maiani, F.; Franceschi, D.; Sassano, M.; Fiorino, A.; Urban, I.A.; Corinaldesi, G. The influence of vertical ridge augmentation techniques on peri-implant bone loss: A systematic review and meta-analysis. Clin. Implant. Dent. Relat. Res. 2024, 26, 15–65. [Google Scholar] [CrossRef] [PubMed]
- Keestra, J.A.; Barry, O.; Jong Ld Wahl, G. Long-term effects of vertical bone augmentation: A systematic review. J. Appl. Oral. Sci. 2016, 24, 3–17. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alotaibi, F.F.; Rocchietta, I.; Buti, J.; D’Aiuto, F. Comparative evidence of different surgical techniques for the management of vertical alveolar ridge defects in terms of complications and efficacy: A systematic review and network meta-analysis. J. Clin. Periodontol. 2023, 50, 1487–1519. [Google Scholar] [CrossRef] [PubMed]
- Rossi, R.; Memè, L.; Strappa, E.M.; Bambini, F. Restoration of Severe Bone and Soft Tissue Atrophy by Means of a Xenogenic Bone Sheet (Flex Cortical Sheet): A Case Report. Appl. Sci. 2023, 13, 692. [Google Scholar] [CrossRef]
- Sheikh, Z.; Sima, C.; Glogauer, M. Bone Replacement Materials and Techniques Used for Achieving Vertical Alveolar Bone Augmentation. Materials 2015, 8, 2953–2993. [Google Scholar] [CrossRef]
- Aloy-Prósper, A.; Carramolino-Cuéllar, E.; Peñarrocha-Oltra, D.; Soto-Peñaloza, D.; Peñarrocha-Diago, M. Intraoral onlay block bone grafts versus cortical tenting technique on alveolar ridge augmentations: A systematic review. Med. Oral. Patol. Oral. Cir. Bucal. 2022, 27, e181–e190. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Urban, I.; Montero, E.; Sanz-Sánchez, I.; Palombo, D.; Monje, A.; Tommasato, G.; Chiapasco, M. Minimal invasiveness in vertical ridge augmentation. Periodontol. 2000 2023, 91, 126–144. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Urban, I.; Monje, A.; Kunrath, M.F.; Dahlin, C. Guided bone regeneration in implant dentistry: Basic principle, progress over 35 years, and recent research activities. Periodontol. 2000 2023, 93, 9–25. [Google Scholar] [CrossRef] [PubMed]
- De Santis, D.; Sinigaglia, S.; Pancera, P.; Faccioni, P.; Luciano, U.; Setti, A.P.; Bursi, P.; Nocini, R.; Nocini, P.F.; Bertossi, D. An overview of guided bone regeneration. J. Biol. Regul. Homeost. Agents. 2019, 33, 49–53. [Google Scholar] [PubMed]
- Merli, M.; Aquilanti, L.; Merli, M.; Mariotti, G.; Rappelli, G. The TACOS Technique: A Stepwise Protocol for Alveolar Ridge Augmentation Using Customized Titanium Mesh. Medicina 2025, 61, 58. [Google Scholar] [CrossRef]
- Happe, A.; Blender, S.M.; Luthardt, R.G.; Rudolph, H.; Kuhn, K. Digital Evaluation of Vertical Ridge Augmentation with the Modified Shell Technique Using a Xenogeneic Bone Lamina: A Case Series. J. Clin. Med. 2023, 12, 7013. [Google Scholar] [CrossRef]
- Perret, F.; D’Aprile, E.; De Stavola, L. The “White Layer Approach”: A Graftless Gingival Augmentation Technique following Vertical GBR with Occlusive Titanium Barriers. Medicina 2023, 59, 1694. [Google Scholar] [CrossRef]
- Sáez-Alcaide, L.M.; González Gallego, B.; Fernando Moreno, J.; Moreno Navarro, M.; Cobo-Vázquez, C.; Cortés-Bretón Brinkmann, J.; Meniz-García, C. Complications associated with vertical bone augmentation techniques in implant dentistry: A systematic review of clinical studies published in the last ten years. J. Stomatol. Oral. Maxillofac. Surg. 2023, 124, 101574. [Google Scholar] [CrossRef]
- Ravidà, A.; Serroni, M.; Borgnakke, W.S.; Romandini, M.; Wang, I.I.; Arena, C.; Annunziata, M.; Cecoro, G.; Saleh, M.H.A. Short (≤6 mm) compared with ≥10-mm dental implants in different clinical scenarios: A systematic review of randomized clinical trials with meta-analysis, trial sequential analysis and quality of evidence grading. J. Clin. Periodontol. 2024, 51, 936–965. [Google Scholar] [CrossRef] [PubMed]
- Schettler, D.; Holtermann, W. Clinical and experimental results of a sandwich-technique for mandibular alveolar ridge augmentation. J. Maxillofac. Surg. 1977, 5, 199–202. [Google Scholar] [CrossRef] [PubMed]
- Sailer, H.F. A new method of inserting endosseous implants in totally atrophic maxillae. J. Craniomaxillofac Surg. 1989, 17, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Starch-Jensen, T.; Nielsen, H.B. Sandwich osteotomy of the atrophic posterior mandible with interpositional autogenous bone block graft compared with bone substitute material: A systematic review and meta-analysis. Br. J. Oral. Maxillofac. Surg. 2020, 58, e237–e247. [Google Scholar] [CrossRef] [PubMed]
- Elnayef, B.; Monje, A.; Gargallo-Albiol, J.; Galindo-Moreno, P.; Wang, H.L.; Hernández-Alfaro, F. Vertical Ridge Augmentation in the Atrophic Mandible: A Systematic Review and Meta-Analysis. Int. J. Oral. Maxillofac. Implants. 2017, 32, 291–312. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Al-Dubai, M.; Mounir, R.; Ali, S.; Mounir, M. Maxillary vertical alveolar ridge augmentation using sandwich osteotomy technique with simultaneous versus delayed implant placement: A proof of principle randomized clinical trial. Clin. Implant. Dent. Relat. Res. 2023, 25, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Moussa, A.K.; Shawky, M.; Aly, L.A.A.; Mounir, M.; Esmael, W.F. Assessment of bone gain and neurosensory affection with the sandwich osteotomy technique for vertically deficient posterior mandible using a full digital workflow versus conventional protocol: A randomized split mouth study. Clin. Implant. Dent. Relat. Res. 2024, 26, 621–630. [Google Scholar] [CrossRef] [PubMed]
- Bernardi, S.; Gatto, R.; Severino, M.; Botticelli, G.; Caruso, S.; Rastelli, C.; Lupi, E.; Roias, A.Q.; Iacomino, E.; Falisi, G. Short Versus Longer Implants in Mandibular Alveolar Ridge Augmented Using Osteogenic Distraction: One-Year Follow-up of a Randomized Split-Mouth Trial. J. Oral. Implantol. 2018, 44, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Bolle, C.; Felice, P.; Barausse, C.; Pistilli, V.; Trullenque-Eriksson, A.; Esposito, M. 4 mm long vs longer implants in augmented bone in posterior atrophic jaws: 1-year post-loading results from a multicentre randomised controlled trial. Eur. J. Oral. Implantol. 2018, 11, 31–47. [Google Scholar] [PubMed]
- Esposito, M.; Barausse, C.; Pistilli, R.; Piattelli, M.; Di Simone, S.; Ippolito, D.R.; Felice, P. Posterior atrophic jaws rehabilitated with prostheses supported by 5 × 5 mm implants with a nanostructured calcium-incorporated titanium surface or by longer implants in augmented bone. Five-year results from a randomised controlled trial. Int. J. Oral. Implant. 2019, 12, 39–54. [Google Scholar] [PubMed]
- Felice, P.; Pistilli, R.; Barausse, C.; Piattelli, M.; Buti, J.; Esposito, M. Posterior atrophic jaws rehabilitated with prostheses supported by 6-mm-long 4-mm-wide implants or by longer implants in augmented bone. Five-year post-loading results from a within-person randomised controlled trial. Int. J. Oral. Implant. 2019, 12, 57–72. [Google Scholar] [PubMed]
- Felice, P.; Barausse, C.; Pistilli, R.; Ippolito, D.R.; Esposito, M. Five-year results from a randomised controlled trial comparing prostheses supported by 5-mm long implants or by longer implants in augmented bone in posterior atrophic edentulous jaws. Int. J. Oral Implantol. 2019, 12, 25–37. [Google Scholar] [PubMed]
- Felice, P.; Barausse, C.; Pistilli, R.; Ippolito, D.R.; Esposito, M. Short implants versus longer implants in vertically augmented posterior mandibles: Result at 8 years after loading from a randomised controlled trial. Eur. J. Oral. Implantol. 2018, 11, 385–395. [Google Scholar] [PubMed]
- Nazzal, S.Q.; Al-Dubai, M.; Mounir, R.; Ali, S.; Mounir, M. Maxillary vertical alveolar ridge augmentation using computer-guided sandwich osteotomy technique with simultaneous implant placement versus conventional technique: A pilot study. Clin. Implant. Dent. Relat. Res. 2021, 23, 842–850. [Google Scholar] [CrossRef] [PubMed]
- El Hadidy, M.S.; Mounir, M.; Abou-Elfetouh, A.; Barakat, A. Assessment of vertical ridge augmentation and labial prominence using buccal versus palatal approaches for maxillary segmental sandwich osteotomy (inlay technique): A randomized clinical trial. Clin. Implant. Dent. Relat. Res. 2018, 20, 722–728. [Google Scholar] [CrossRef] [PubMed]
- El Zahwy, M.; Taha, S.A.A.K.; Mounir, R.; Mounir, M. Assessment of vertical ridge augmentation and marginal bone loss using autogenous onlay vs inlay grafting techniques with simultaneous implant placement in the anterior maxillary esthetic zone: A randomized clinical trial. Clin. Implant. Dent. Relat. Res. 2019, 21, 1140–1147. [Google Scholar] [CrossRef] [PubMed]
- Mounir, M.; Mounir, S.; Abou-Elfetouh, A.; Shaker, M.A. Assessment of vertical ridge augmentation in anterior aesthetic zone using onlay xenografts with titanium mesh versus the inlay bone grafting technique: A randomized clinical trial. Int. J. Oral. Maxillofac. Surg. 2017, 46, 1458–1465. [Google Scholar] [CrossRef] [PubMed]
- Chiapasco, M.; Zaniboni, M.; Boisco, M. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin. Oral. Implant. Res. 2006, 17 (Suppl. S2), 136–159. [Google Scholar] [CrossRef] [PubMed]
- Atef, M.; Osman, A.H.; Hakam, M. Autogenous interpositional block graft vs onlay graft for horizontal ridge augmentation in the mandible. Clin. Implant. Dent. Relat. Res. 2019, 21, 678–685. [Google Scholar] [CrossRef] [PubMed]
- Aghaloo, T.L.; Moy, P.K. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int. J. Oral. Maxillofac. Implant. 2007, 22, 49–70, Erratum in: Int. J. Oral. Maxillofac. Implant. 2008, 23, 56. [Google Scholar] [PubMed]
- Bera, R.N.; Tandon, S.; Singh, A.K.; Bhattacharjee, B.; Pandey, S.; Chirakkattu, T. Sandwich osteotomy with interpositional grafts for vertical augmentation of the mandible: A meta-analysis. Natl. J. Maxillofac. Surg. 2022, 13, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Laino, L.; Iezzi, G.; Piattelli, A.; Lo Muzio, L.; Cicciù, M. Vertical ridge augmentation of the atrophic posterior mandible with sandwich technique: Bone block from the chin area versus corticocancellous bone block allograft—Clinical and histological prospective randomized controlled study. Biomed. Res. Int. 2014, 2014, 982104. [Google Scholar] [CrossRef] [PubMed]
- Fekry, Y.E.; Mahmoud, N.R. Vertical ridge augmentation of atrophic posterior mandible with corticocancellous onlay symphysis graft versus sandwich technique: Clinical and radiographic analysis. Odontology 2023, 111, 993–1002. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Grusovin, M.G.; Kwan, S.; Worthington, H.V.; Coulthard, P. Interventions for replacing missing teeth: Bone augmentation techniques for dental implant treatment. Cochrane Database Syst. Rev. 2008, 16, CD003607, Erratum in: Cochrane Database Syst Rev. 2009, 7, CD003607. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekaran, D.; Chinnaswami, R.; Malathi, N.; Jayakumar, N.D. Treatment Outcome of Using Guided Bone Regeneration for Bone Augmentation for the Placement of Dental Implants—A Systematic Review. J. Pharm. Bioallied Sci. 2024, 16 (Suppl. S4), S3068–S3070. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sabri, H.; Heck, T.; Manouchehri, N.; Alhachache, S.; Calatrava, J.; Misch, C.M.; Wang, H.L. Bone augmentation using titanium mesh: A systematic review and meta-analysis. Int. J. Oral. Implant. 2024, 17, 251–269. [Google Scholar] [PubMed]
- Robert, L.; Aloy-Prósper, A.; Arias-Herrera, S. Vertical augmentation of the atrofic posterior mandibular ridges with onlay grafts: Intraoral blocks vs. guided bone regeneration. Syst. Rev. J. Clin. Exp. Dent. 2023, 15, e357–e365. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Koo, H.; Hwang, J.; Choi, B.J.; Lee, J.W.; Ohe, J.Y.; Jung, J. Comparison of vertical bone resorption following various types of autologous block bone grafts. Maxillofac. Plast. Reconstr. Surg. 2023, 45, 38. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Saletta, J.M.; Garcia, J.J.; Caramês, J.M.M.; Schliephake, H.; da Silva Marques, D.N. Quality assessment of systematic reviews on vertical bone regeneration. Int. J. Oral. Maxillofac. Surg. 2019, 48, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Urban, I.A.; Montero, E.; Monje, A.; Sanz-Sánchez, I. Effectiveness of vertical ridge augmentation interventions: A systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46 (Suppl. S21), 319–339. [Google Scholar] [CrossRef] [PubMed]
- Abu-Mostafa, N.A.; Alotaibi, Y.N.; Alkahtani, R.N.; Almutairi, F.K.; Alfaifi, A.A.; Alshahrani, O.D. The Outcomes of Vertical Alveolar Bone Augmentation by Guided Bone Regeneration with Titanium Mesh: A Systematic Review. J. Contemp. Dent. Pract. 2022, 23, 1280–1288. [Google Scholar] [CrossRef] [PubMed]
- Atieh, M.A.; Alsabeeha, N.H.; Payne, A.G.; Ali, S.; Faggion, C.M.J.; Esposito, M. Interventions for replacing missing teeth: Alveolar ridge preservation techniques for dental implant site development. Cochrane Database Syst. Rev. 2021, 4, CD010176. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| Title | Year | Authors | Study Design | Participants | Follow-Up | Comparison | Implant Survival Rate | MBL at Follow-Up | Complications | Average Vertical Bone Gain |
|---|---|---|---|---|---|---|---|---|---|---|
| Assessment of vertical ridge augmentation in anterior aesthetic zone using onlay xenografts with titanium mesh versus the inlay bone grafting technique: A randomized clinical trial | 2017 | Mounir et al. [32] | RCT | 16 patients, 40 implants | 6 months postoperative | Onlay vs. inlay bone grafting | Not reported | Not reported | 1 dehiscence in the onlay group | 20.7% (onlay), 31.6% (inlay). No difference between groups (p = 0.2) |
| Short Versus Longer Implants in Mandibular Alveolar Ridge Augmented Using Osteogenic Distraction: One-Year Follow-up of a Randomized Split-Mouth Trial | 2018 | Bernardi et al. [23] | Split-mouth RCT | 36 patients, 170 implants | 1 year post-loading | 6 mm vs. 10 mm implants | 94.2% for 6 mm implants, 84.5% for 10 mm implants (p = 0.5705) | Similar in both groups | 22/36 patients with complications in augmented sites. Higher at augmented sites (p < 0.05) | Not reported |
| 4 mm long vs. longer implants in augmented bone in posterior atrophic jaws: 1-year post-loading results from a multicentre randomised controlled trial | 2018 | Bolle et al. [24] | Multicenter RCT | 80 patients (40 in mandible) | 1 year post-loading | 4 mm vs. >10 mm implants in augmented sites | No difference in implant failure (p = 1) | Less bone loss with short implants in mandible (0.40 mm vs. 0.52 mm) (p = 0.006) | 9/20 complications in augmented sites and fewer complications with short implants (p = 0.003) | Not reported |
| Short implants versus longer implants in vertically augmented posterior mandibles: result at 8 years after loading from a randomised controlled trial | 2018 | Felice et al. [28] | RCT | 60 patients | 8 years | 6.6 mm long implants vs. 9.6 mm or longer implants in augmented sites | 5 failures in short implants vs. 3 failures in augmented sites (p = 1) | Short implant: 1.58 mm MBL compared with 2.46 mm in the augmented group | More complications in augmented patients (27 in 22 augmented patients vs. 9 in 8 patients of the short implant group) (p < 0.001) | Not reported |
| Assessment of vertical ridge augmentation and labial prominence using buccal versus palatal approaches for maxillary segmental sandwich osteotomy (inlay technique): A randomized clinical trial | 2018 | El Hadidy et al. [30] | RCT | 16 patients, 40 implants | 4 months postoperative | Buccal vs. palatal approach | Not reported | Not reported | No complications | 79.9% (buccal), 76.5% (palatal). No significant difference (p = 0.43) |
| Five-year results from a randomised controlled trial comparing prostheses supported by 5-mm long implants or by longer implants in augmented bone in posterior atrophic edentulous jaws | 2019 | Felice, Barausse et al. [27] | RCT (split-mouth) | 30 patients (15 in mandible and 15 in maxilla)—56 implants | 5 years post-loading | 5 mm vs. >10 mm implants in augmented sites | No difference in implant failure (p = 1) | Short implants: 1.72 mm MBL compared with 2.10 mm in the augmented group (p = 0.022) | 12 patients with 14 complications in augmented sites. No difference compared with short implants | Not reported |
| Posterior atrophic jaws rehabilitated with prostheses supported by 6-mm-long 4-mm-wide implants or by longer implants in augmented bone. Five-year post-loading results from a within-person randomised controlled trial | 2019 | Felice, Pistilli et al. [26] | Within-person RCT | 40 patients (20 in mandible and 20 in maxilla)—88 implants | 5 years post-loading | 6 × 4 mm vs. >10 mm implants in augmented sites | No difference in implant failure (p = 1) | Short implants: 1.34 ± 0.35 mm MBL compared with 2.11 ± 0.59 mm in the augmented group (p = 0.003) | 14 patients with 19 complications in augmented sites. No difference compared with short implants (p = 0.118) | Not reported |
| Posterior atrophic jaws rehabilitated with prostheses supported by 5 × 5 mm implants with a nanostructured calcium-incorporated titanium surface or by longer implants in augmented bone. Five-year results from a randomised controlled trial | 2019 | Esposito et al. [25] | RCT | 80 patients (40 in mandible)—63 implants | 5 years post-loading | 5 × 5 mm vs. >10 mm implants in augmented sites | No difference in implant failure (p = 0.609) | Short implant: 1.22 mm MBL compared with 1.70 mm in the augmented group (p = 0.004) | More complications in augmented site compared to short implant in mandible (0.013) | Not reported |
| Assessment of vertical ridge augmentation and marginal bone loss using autogenous onlay vs. inlay grafting techniques with simultaneous implant placement in the anterior maxillary esthetic zone: A randomized clinical trial | 2019 | El Zahwy et al. [31] | RCT | 16 patients, 40 implants | 6 months postoperative | Onlay vs. inlay grafting | Not reported | Crestal bone loss: 4.77 mm in onlay vs. 1.65 mm in inlay (p < 0.05) | Onlay group: 12 complications. Inlay group: No complications | 3.34 mm (inlay), −0.02 mm (onlay) (p < 0.05) |
| Maxillary vertical alveolar ridge augmentation using computer-guided sandwich osteotomy technique with simultaneous implant placement versus conventional technique: A pilot study | 2021 | Nazzal et al. [29] | RCT (pilot study) | 12 patients | 4 months postoperative | Computer-guided vs. conventional sandwich osteotomy | Not reported | Not reported | 1 complication in study group. Significantly reduced palatal tipping with computer-guided technique (p < 0.001) | 4.4 mm (guided), 3.9 mm (conventional) |
| Maxillary vertical alveolar ridge augmentation using sandwich osteotomy technique with simultaneous versus delayed implant placement: A proof of principle randomized clinical trial | 2022 | Al-Dubai et al. [21] | RCT | 16 patients, 35 implants | 4 months postoperative | Simultaneous vs. delayed implant placement | 100% | Not reported | 1 complication in the control group | 4.04 mm (simultaneous), 3.86 mm (delayed). No significant difference (p = 0.518) |
| Assessment of bone gain and neurosensory affection with the sandwich osteotomy technique for vertically deficient posterior mandible using a full digital workflow versus conventional protocol: A randomized split mouth study | 2024 | Moussa et al. [22] | Split-mouth RCT | 10 patients, 40 implants | 4 months postoperative | Digital workflow vs. conventional sandwich osteotomy | Not reported | Not reported | 1 case of dehiscence (resolved) | 3.76 mm (digital), 2.69 mm (conventional) (p = 0.001) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barausse, C.; Tayeb, S.; Pellegrino, G.; Bonifazi, L.; Mancuso, E.; Ratti, S.; Galvani, A.; Pistilli, R.; Felice, P. The Inlay Technique in Alveolar Ridge Augmentation: A Systematic Review. J. Clin. Med. 2025, 14, 1684. https://doi.org/10.3390/jcm14051684
Barausse C, Tayeb S, Pellegrino G, Bonifazi L, Mancuso E, Ratti S, Galvani A, Pistilli R, Felice P. The Inlay Technique in Alveolar Ridge Augmentation: A Systematic Review. Journal of Clinical Medicine. 2025; 14(5):1684. https://doi.org/10.3390/jcm14051684
Chicago/Turabian StyleBarausse, Carlo, Subhi Tayeb, Gerardo Pellegrino, Lorenzo Bonifazi, Edoardo Mancuso, Stefano Ratti, Andrea Galvani, Roberto Pistilli, and Pietro Felice. 2025. "The Inlay Technique in Alveolar Ridge Augmentation: A Systematic Review" Journal of Clinical Medicine 14, no. 5: 1684. https://doi.org/10.3390/jcm14051684
APA StyleBarausse, C., Tayeb, S., Pellegrino, G., Bonifazi, L., Mancuso, E., Ratti, S., Galvani, A., Pistilli, R., & Felice, P. (2025). The Inlay Technique in Alveolar Ridge Augmentation: A Systematic Review. Journal of Clinical Medicine, 14(5), 1684. https://doi.org/10.3390/jcm14051684








