Efficacy and Safety of Early Mobilization and Factors Associated with Rehabilitation After Stroke—Review
Abstract
1. Introduction
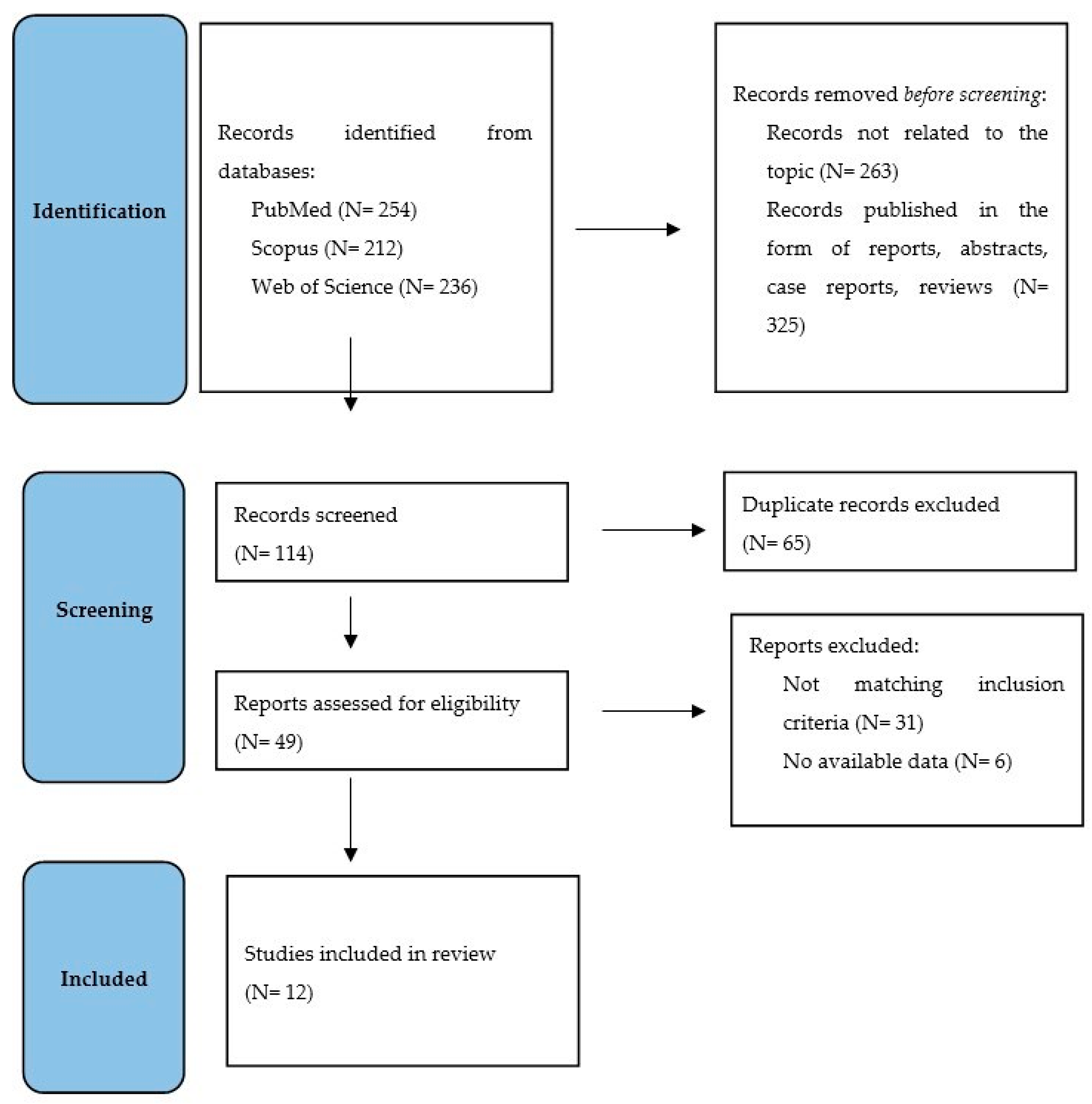
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
3. Results
3.1. Overview of Studies
3.2. Characteristics of the Studies of Early Rehabilitation After Stroke
3.3. Characteristics of the Studies of Factors Associated with Rehabilitation After Stroke
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Stroke Association. About Stroke. Available online: https://www.stroke.org/en/about-stroke (accessed on 10 November 2024).
- World Health Organization. Stroke, Cerebrovascular Accident. Available online: https://www.emro.who.int/health-topics/stroke-cerebrovascular-accident/index.html (accessed on 11 November 2024).
- Soto-Cámara, R.; González-Santos, J.; González-Berna, J.; Trejo-Gabriel-Galán, J.M. Factors associated with a rapid call for assistance for patients with ischemic stroke. Emergencias 2020, 32, 33–39. [Google Scholar] [PubMed]
- Chohan, S.A.; Venkatesh, P.K.; How, C.H. Long-term complications of stroke and secondary prevention: An overview for primary care physicians. Singap. Med. J. 2019, 60, 616–620. [Google Scholar] [CrossRef] [PubMed]
- James, J.; Purcell, D.; McGlinchey, M.P. Exploring physiotherapy staff’s perceptions of physiotherapy delivery in acute stroke rehabilitation. Clin. Rehabil. 2025, 39, 99–108. [Google Scholar] [CrossRef]
- Dohle, C.; Schrader, M. Neurorehabilitation. Nervenarzt 2024, 95, 1148–1157. [Google Scholar] [CrossRef]
- Johnson, A.J.; Dudley, W.N.; Wideman, L.; Schulz, M. Physiological Risk Profiles and Allostatic Load: Using Latent Profile Analysis to Examine Socioeconomic Differences in Physiological Patterns of Risk. Eur. J. Environ. Public Health 2019, 3, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Katan, M.; Luft, A. Global Health Neurology. Semin. Neurol. 2018, 38, 208–211. [Google Scholar] [CrossRef]
- Bernhardt, J.; Indredavik, B.; Dewey, H.; Langhorne, P.; Lindley, R.; Donnan, G.; Thrift, A.; Collier, J. Mobilisation ‘in bed’ is not mobilisation. Cerebrovasc. Dis. 2007, 24, 157–158. [Google Scholar] [CrossRef]
- Coleman, E.R.; Moudgal, R.; Lang, K.; Hyacinth, H.I.; Awosika, O.O.; Kissela, B.M.; Feng, W. Early Rehabilitation After Stroke: A Narrative Review. Curr. Atheroscler. Rep. 2017, 19, 59. [Google Scholar] [CrossRef]
- National Institutes of Health. Critical Time Window for Rehabilitation After a Stroke. Available online: https://www.nih.gov/news-events/nih-research-matters/critical-time-window-rehabilitation-after-stroke (accessed on 28 November 2024).
- Bernhardt, J.; English, C.; Johnson, L.; Cumming, T.B. Early mobilization after stroke: Early adoption but limited evidence. Stroke 2015, 46, 1141–1146. [Google Scholar] [CrossRef] [PubMed]
- Langhorne, P.; Wu, O.; Rodgers, H.; Ashburn, A.; Bernhardt, J. A Very Early Rehabilitation Trial after stroke (AVERT): A Phase III, multicentre, randomised controlled trial. Health Technol. Assess. 2017, 21, 1–120. [Google Scholar] [CrossRef] [PubMed]
- Herisson, F.; Godard, S.; Volteau, C.; Le Blanc, E.; Guillon, B.; Gaudron, M.; SEVEL Study Group. Early Sitting in Ischemic Stroke Patients (SEVEL): A randomized controlled trial. PLoS ONE. 2016, 11, e149466. [Google Scholar] [CrossRef]
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (2020). Available online: https://www.prisma-statement.org (accessed on 28 November 2024).
- Poletto, S.R.; Rebello, L.C.; Valença, M.J.; Rossato, D.; Almeida, A.G.; Brondani, R.; Chaves, M.L.; Nasi, L.A.; Martins, S.C. Early mobilization in ischemic stroke: A pilot randomized trial of safety and feasibility in a public hospital in Brazil. Cerebrovasc. Dis. Extra 2015, 5, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Cumming, T.B.; Churilov, L.; Collier, J.; Donnan, G.; Ellery, F.; Dewey, H.; Langhorne, P.; Lindley, R.I.; Moodie, M.; Thrift, A.G.; et al. Early mobilization and quality of life after stroke: Findings from AVERT. Neurology 2019, 93, e717–e728. [Google Scholar] [CrossRef]
- Radford, K.A.; Wright-Hughes, A.; Thompson, E.; Clarke, D.; Phillips, J.; Holmes, J.; Powers, K.E.; Trusson, D.; Craven, K.; Watkins, C.L.; et al. Effectiveness of early vocational rehabilitation versus usual care to support RETurn to work After stroKE: A pragmatic, parallel arm multi-centre, randomised-controlled trial. Int. J. Stroke 2024, 17474930241306693. [Google Scholar] [CrossRef]
- Yen, H.C.; Pan, G.S.; Jeng, J.S.; Chen, W.S. Impact of Early Mobilization on Patients With Acute Ischemic Stroke Treated With Thrombolysis or Thrombectomy: A Randomized Controlled Trial. Neurorehabilit. Neural Repair 2024, 15459683241236443. [Google Scholar] [CrossRef]
- Yen, H.C.; Jeng, J.S.; Chen, W.S.; Pan, G.S.; Chuang Pt Bs, W.Y.; Lee, Y.Y.; Teng, T. Early Mobilization of Mild-Moderate Intracerebral Hemorrhage Patients in a Stroke Center: A Randomized Controlled Trial. Neurorehabilit. Neural Repair 2020, 34, 72–81. [Google Scholar] [CrossRef]
- Wang, W.; Wei, M.; Cheng, Y.; Zhao, H.; Du, H.; Hou, W.; Yu, Y.; Zhu, Z.; Qiu, L.; Zhang, T.; et al. Safety and Efficacy of Early Rehabilitation After Stroke Using Mechanical Thrombectomy: A Pilot Randomized Controlled Trial. Front. Neurol. 2022, 13, 698439. [Google Scholar] [CrossRef] [PubMed]
- Gnanaprakasam, A.; Solomon, J.M.; Roy, A.K.; Deshmukh, A.S.; Karthikbabu, S. Association between depression and adherence to upper limb exercises among community-dwelling stroke survivors: A cross-sectional study. Health Sci. Rep. 2024, 7, e70133. [Google Scholar] [CrossRef] [PubMed]
- Kamo, T.; Momosaki, R.; Suzuki, K.; Asahi, R.; Azami, M.; Ogihara, H.; Nishida, Y. Effectiveness of Intensive Rehabilitation Therapy on Functional Outcomes After Stroke: A Propensity Score Analysis Based on Japan Rehabilitation Database. J. Stroke Cerebrovasc. Dis. 2019, 28, 2537–2542. [Google Scholar] [CrossRef]
- Tan, M.; Li, H.; Wang, X. Analysis of the current status of rehabilitation motivation and its influencing factors in older adults with stroke: A cross-sectional study. Front. Aging Neurosci. 2023, 15, 1186681. [Google Scholar] [CrossRef]
- Wattanapan, P.; Lukkanapichonchut, P.; Massakulpan, P.; Suethanapornkul, S.; Kuptniratsaikul, V. Effectiveness of Stroke Rehabilitation Compared between Intensive and Nonintensive Rehabilitation Protocol: A Multicenter Study. J. Stroke Cerebrovasc. Dis. 2020, 29, 104809. [Google Scholar] [CrossRef] [PubMed]
- Tang, Z.; Su, W.; Liu, T.; Lu, H.; Liu, Y.; Li, H.; Han, K.; Moneruzzaman, M.; Long, J.; Liao, X.; et al. Prediction of poststroke independent walking using machine learning: A retrospective study. BMC Neurol. 2024, 24, 332. [Google Scholar] [CrossRef]
- Kennedy, C.; Bernhardt, J.; Churilov, L.; Collier, J.M.; Ellery, F.; Rethnam, V.; Carvalho, L.B.; Donnan, G.A.; Hayward, K.S. Factors associated with time to independent walking recovery post-stroke. J. Neurol. Neurosurg. Psychiatry 2021, 92, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Aoyagi, Y.; Saito, A.; Iwasawa, T.; Ohashim, M. Rehabilitation Therapy for Acute Brain Disease. No Shinkei Geka 2023, 51, 1122–1129. [Google Scholar] [CrossRef] [PubMed]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2019, 50, e344–e418. [Google Scholar] [CrossRef]
- Tong, Y.; Cheng, Z.; Rajah, G.B.; Duan, H.; Cai, L.; Zhang, N.; Du, H.; Geng, X.; Ding, Y. High Intensity Physical Rehabilitation Later Than 24 h Post Stroke Is Beneficial in Patients: A Pilot Randomized Controlled Trial (RCT) Study in Mild to Moderate Ischemic Stroke. Front. Neurol. 2019, 10, 113. [Google Scholar] [CrossRef]
- Meléndez-Oliva, E.; Martínez-Pozas, O.; Cuenca-Zaldívar, J.N.; Villafañe, J.H.; Jiménez-Ortega, L.; Sánchez-Romero, E.A. Efficacy of Pulmonary Rehabilitation in Post-COVID-19: A Systematic Review and Meta-Analysis. Biomedicines 2023, 11, 2213. [Google Scholar] [CrossRef] [PubMed]
- Vloothuis, J.D.; Mulder, M.; Veerbeek, J.M.; Konijnenbelt, M.; Visser-Meily, J.M.; Ket, J.C.; Kwakkel, G.; van Wegen, E.E. Caregiver-mediated exercises for improving outcomes after stroke. Cochrane Database Syst. Rev. 2016, 12, CD011058. [Google Scholar] [CrossRef] [PubMed]
- Scarpino, M.; Grippo, A.; Campagnini, S.; Hakiki, B.; Maiorelli, A.; Sodero, A.; Guolo, E.; Mannini, A.; Macchi, C.; Cecchi, F. Stroke-related epilepsy in the rehabilitation setting: Insights from the inpatient post-stroke rehabilitation study—RIPS. Epilepsy Behav. Rep. 2024, 28, 100713. [Google Scholar] [CrossRef]
- Mangalabarathi, N.; Devi, B.; Chinnathambi, K.; Nirmala, C. Effectiveness of Nurse-Led Stroke Rehabilitation on Awareness, Activities of Daily Living and Coping in Stroke Patients at a Tertiary Care Hospital in India. Cureus 2024, 16, e72843. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.J.; Chang, S.C.; Lin, L.C.; Cheng, C.H.; Chang, Y.H.; Pei, Y.C. Therapeutic effects of powered exoskeletal robot-assisted gait training in inpatients in the early stage after stroke: A pilot case-controlled study. J. Neuroeng. Rehabil. 2024, 21, 206. [Google Scholar] [CrossRef]
- Borboni, A.; Villafañe, J.H.; Mullè, C.; Valdes, K.; Faglia, R.; Taveggia, G.; Negrini, S. Robot-Assisted Rehabilitation of Hand Paralysis After Stroke Reduces Wrist Edema and Pain: A Prospective Clinical Trial. J. Manip. Physiol. Ther. 2017, 40, 21–30. [Google Scholar] [CrossRef]
| Author, Year | Population | Age (Mean ± SD) | Measure | Start-Up Time of Early Rehabilitation | Characteristic of the Study Group | Assessment of Safety and Efficacy of Early Rehabilitation After Stroke |
|---|---|---|---|---|---|---|
| Yen et al., 2024 [19] | 122 (N = 60 patients after intravenous thrombolysis and N = 62 mechanical thrombectomy) | -- | FIM-motor, PASS; evaluated 2 weeks, 4 weeks, and 3 months post-stroke | 24–72 h | The study included patients with first acute ischemic stroke treated with thrombolysis or thrombectomy. The rehabilitation in this study lasted 30 min/day, 5 days/week until discharge. |
|
| Radford et al., 2024 [18] | 583 (N = 324 qualified for Early Stroke Specialist Vocational Rehabilitation plus usual care and N = 259 qualified for usual care alone) | 54.0 ± 11.12 | self-reported at 3, 6, and 12 months return-to-work for ≥2 h per week at 12 months | within 12 weeks of stroke | Eligible participants were in work at stroke onset. Patients included in the study were hospitalized with new stroke and within 12 weeks of stroke. |
|
| Yen et al., 2020 [20] | 60 (N = 30 early mobilization group, N = 30 standard early rehabilitation) | standard early rehabilitation—59.33 ± 13.13, early mobilization—58.77 ± 11.68 | FIM-motor, PASS, FAC; evaluated 2 weeks, 4 weeks, and 3 months post-stroke | 24–72 h | Participants ≤ 24 h after acute intracerebral hemorrhage were recruited. Early mobilization and standard group 30 min/day, 5 days/week until discharge. Inclusion criteria: a first-time primary acute intracerebral hemorrhage with unilateral hemiparesis/hemiplegia confirmed via computed tomography, complete independence in ADL before stroke, no contraindications to rehabilitation within 72 h of stroke onset. |
|
| Wang et al., 2022 [21] | 103 (N = 52 early rehabilitation group, N = 51 conventional rehabilitation group) | early rehabilitation group 58 years (48–66.8) and conventional rehabilitation group—62 years (55–69) | mortality, mRS of 0–2, the incidence of non-fatal complications, BI scores; evaluated 3 months and 1 year post-stroke | within 48 h | Patients who met the study criteria, i.e., have undergone mechanical thrombectomy, with a history of stroke with an accompanying neurological deficit were included. The first out-of-bed exercises were performed within 48 h of stroke symptom onset. Early rehabilitation for a minimum of 5–10 min per session, with four sessions per day for ≥4 days a week until discharge. |
|
| Poletto et al., 2015 [16] | 37 (N = 18 early mobilization, N = 19 standard care) | 65 years (mean) | NIHSS, mRS, activities of daily living, the modified BI; evaluated on day 14 or at discharge, 3 months | within 48 h | The study included patients with ischemic stroke confirmed by CT or MRI within 48 h of symptom onset. Early rehabilitation was performed 5 times a week, once a day, for approximately 30 min. |
|
| Cumming et al., 2019 [17] | 2104 (N = 1054 very early and more frequent mobilization, N = 1050 usual care) | intervention group—70.3 ± 13.0, usual care—70.9 ± 12.6 | AQoL-4D at 12-months | within 24 h | Participants were recruited within 24 h of a confirmed stroke (first or recurrent, ischemic or hemorrhagic). The criteria for very early mobilization were considered to be: implementation of rehabilitation within 24 h of the stroke occurrence, out-of-bed activity, usual care plus 3 out-of-bed sessions per day. |
|
| Author, Year | Population | Age | Measure | Characteristic of the Study Group | Assessment of Factors Associated with Post-Stroke Rehabilitation |
|---|---|---|---|---|---|
| Gnanaprakasam et al., 2024 [22] | 215 | 54.41 ± 13.60 | Patient Health Questionnaire-9, Stroke-Specific Measure of Adherence to Home-based Exercises, Fugl–Meyer Assessment-Upper Extremity | This study was conducted among 215 community-dwelling stroke survivors undergoing motor rehabilitation between February 2021 and January 2023. |
|
| Tang et al., 2024 [26] | 778 | 59.00 (49.00–68.00) | independent walking at discharge was investigated | Participants were eligible for inclusion with a diagnosis of first-ever unilateral cerebral stroke and were unable to walk independently at admission and their Functional Ambulatory Category score was ≤3. Additionally, patients diagnosed with other underlying neurological diseases and/or disturbances of consciousness and/or unstable vital signs and the length of stay was <14 days were excluded. |
|
| Tan et al., 2023 [24] | 350 | 60–69 years—21.4% of patients; 70–79 years—35.1%; ≥80 years—43.4% | Multidimensional Scale of Perceived Social Support, Questionnaire of Exercise Adherence, Tampa scale of kinesiophobia, Motivation in stroke patients for rehabilitation scale | The study included patients hospitalized in the stroke rehabilitation unit. The inclusion criteria for the participants were: age ≥ 60 years, diagnosis stroke, able to communicate normally, and conscious. |
|
| Kennedy et al., 2021 [27] | 2100 | 72.5 years | days to walking 50 m unassisted, tested from 24 h to 3 months post-stroke | Participants were eligible for inclusion with a diagnosis of first or recurrent stroke and admitted to a hospital within 24 h of stroke onset. |
|
| Wattanapan et al., 2020 [25] | 780 | 61.9 ± 13.3 | EQ-5D-3L and BI at admission and at discharge | Patients were classified into two groups: intensive or non-intensive rehabilitation. Intensive rehabilitation included patients who could tolerate rehabilitation for at least 3 h per day, 5 days per week. |
|
| Kamo et al., 2019 [23] | 2325 | 76.8 ± 7.1 | FIM | This study included patients with a diagnosis of stroke. The inclusion criteria for the participants were: aged more than equal to 65 years, stayed in rehabilitation hospital less than 180 days, had complete data. Patients were classified into two groups: intensive rehabilitation therapy and usual rehabilitation. The intensive rehabilitation therapy group included 862 stroke patients who performed more than 15 h of rehabilitation therapy per week in cooperation with a physiotherapist, occupational therapist, and/or speech therapist. |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Filipska-Blejder, K.; Jaracz, K.; Ślusarz, R. Efficacy and Safety of Early Mobilization and Factors Associated with Rehabilitation After Stroke—Review. J. Clin. Med. 2025, 14, 1585. https://doi.org/10.3390/jcm14051585
Filipska-Blejder K, Jaracz K, Ślusarz R. Efficacy and Safety of Early Mobilization and Factors Associated with Rehabilitation After Stroke—Review. Journal of Clinical Medicine. 2025; 14(5):1585. https://doi.org/10.3390/jcm14051585
Chicago/Turabian StyleFilipska-Blejder, Karolina, Krystyna Jaracz, and Robert Ślusarz. 2025. "Efficacy and Safety of Early Mobilization and Factors Associated with Rehabilitation After Stroke—Review" Journal of Clinical Medicine 14, no. 5: 1585. https://doi.org/10.3390/jcm14051585
APA StyleFilipska-Blejder, K., Jaracz, K., & Ślusarz, R. (2025). Efficacy and Safety of Early Mobilization and Factors Associated with Rehabilitation After Stroke—Review. Journal of Clinical Medicine, 14(5), 1585. https://doi.org/10.3390/jcm14051585








