Gender Differences in Clinical Practice Regarding Coronary Heart Disease: A Systematic Review
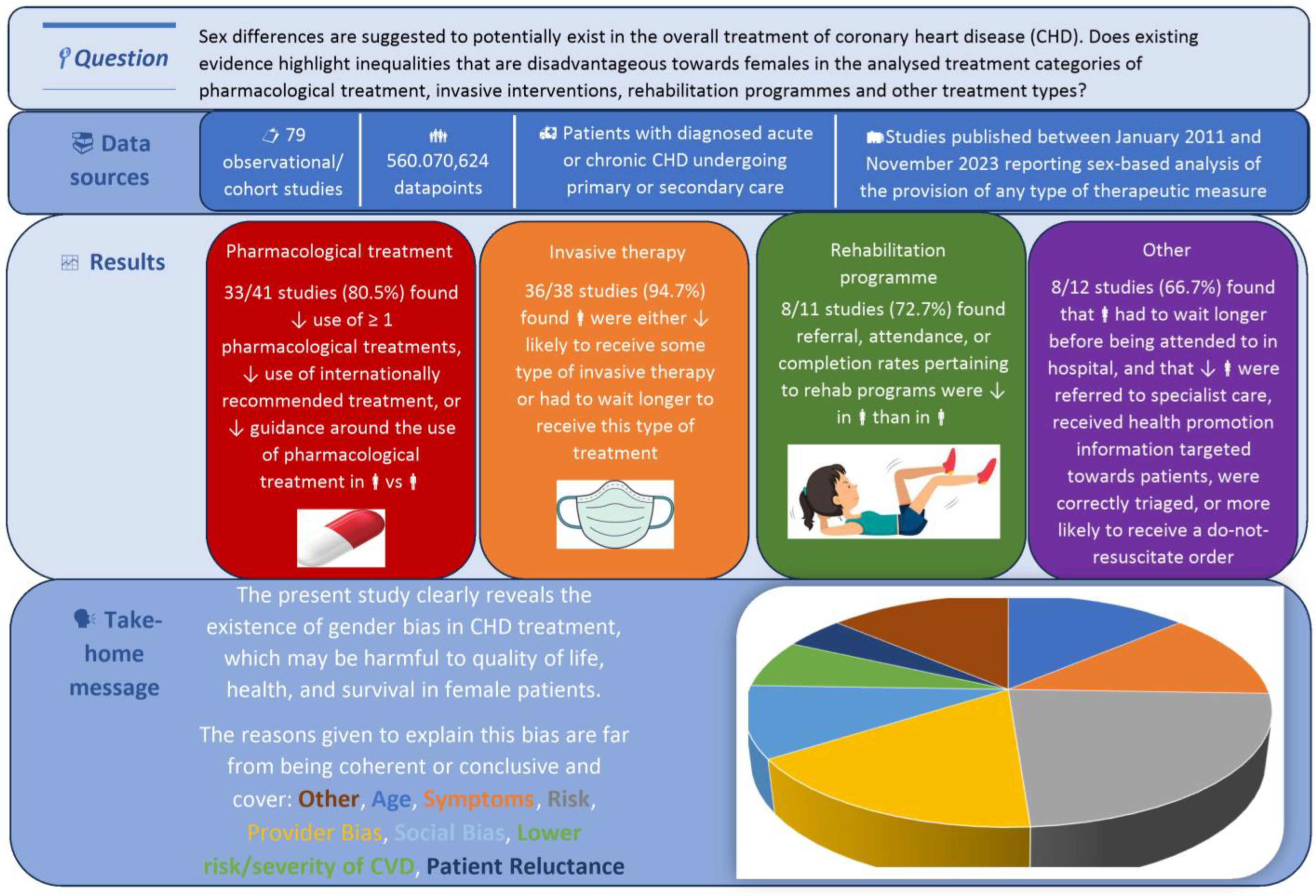
Abstract
1. Introduction
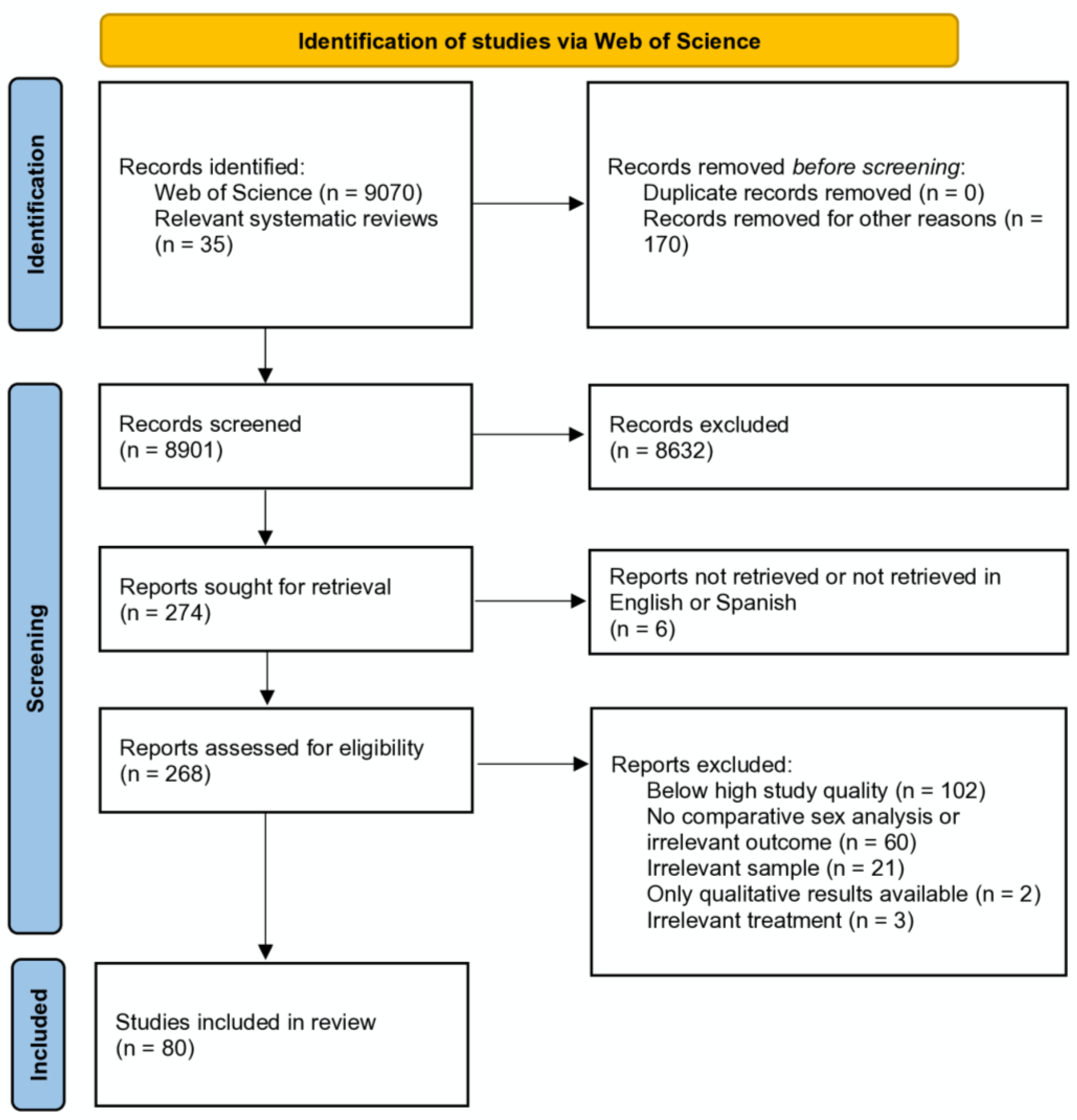
2. Materials and Methods
Study Quality
3. Results
3.1. Use of Pharmacological Treatment
| Author | Title | Year | Sample | Context | Design | Time-Frame | Treatment | Main Findings |
|---|---|---|---|---|---|---|---|---|
| [13] | Statin use in outpatients with obstructive coronary artery disease | 2011 | 38,775 patients with obstructive CVD | The US between 1 July 2009 and 30 June 2010 | Longitudinal registry PINNACLE | Statins and other medication | Male sex was a predictor of statin use. | |
| [14] | Bridging the gender gap: Insights from a contemporary analysis of sex-related differe… | 2012 | 14,196 ACS STEMI patients | Data from four Canadian registries between 1999 and 2008 | Prospective, multi-centre, and observational | Aspirin, ticlopidine/clopidogrel, heparin, and GPIIb/IIIa inhibitors | Fewer women received thienopyridines, heparin, or glycoprotein IIb/IIIa inhibitors. | |
| [15] | Statin prescription for patients with atherosclerotic cardiovascular disease from n… | 2019 | 8468 CVD patients (29.3% women) | Two national surveys between 2011 and 2015 in the US | Cross-sectional and retrospective | Statins | Men were more likely to receive a statin prescription. The effect persisted after adjusting for those with coronary disease. | |
| [16] | Sex differences in in-hospital management and outcomes of patients with acute coronary syndrome | 2019 | 82,196 ACS patients from 192 hospitals | AHA and Chinese Society of Cardiology national registry between 2014 and 2018 | Prospective and observational | ACE inhibitors/ARBs, beta blockers, statins, and heparin | Fewer women received acute treatment based on scientific evidence, anti-platelet therapy, enzyme inhibitors, and statins. The likelihood of receiving pharmacological treatment was greater in men than in women in the over-65s. In the under-65s, men received more thromolytic drugs than women. | |
| [17] | Temporal trends in the incidence, treatment patterns, and outcomes of coronary artery disease and peripheral … | 2020 | 231,120 ACS patients | 4.6 million individuals from the UK between 2006 and 2015 | National, representative, observational digital registries | Statins | Fewer statins were prescribed in women. | |
| [18] | Trends in use of high-intensity statin therapy after myocardial infarction, 2011 to 2014 | 2017 | 42,893 MarketScan patients and 75,096 Medicare patients | Health insurance claimants after suffering CHD, the US, 2011 to 2014 | Observational | Hospital discharge | Statins | More men received high-intensity statin prescriptions than women. |
| [19] | National trends and disparities in statin use for ischemic heart disease from 2006 to 2018: Insights from National Ambul… | 2022 | 542,704,112 outpatient CHD appointments | National Ambulatory Medical Care Survey (NAMCS), the US, Jan 2006 to Dec 2018 | Retrospective analysis | During outpatient appointment | Statins | Male sex was associated with a greater likelihood of statin use. |
| [20] | Treatment gaps, 1-year readmission and mortality following myocardial infarction by diabetes status, sex and so… | 2022 | 43,272 patients after MI | All MI survivors in Victoria, Australia, Jul 2012-Jun 2017 | Observational cohort | One year | Cardioprotective medications | Males were more likely to be dispensed cardioprotective medications at or within 90 days of discharge. |
| [21] | Sex differences in time trends in acute coronary syndrome management and in 12-month lethality: Data from the Frenc… | 2022 | 3196 patients with first ACS | All patients (aged 35–74) form MONICA registries in France, Jan-Dec 2006 or Oct 2015-March 2016 | Observational cohort | Twelve months in 2006 or six months in 2016 | Beta blockers, platelet aggregation inhibitors, statins, ACE inhibitors, and anticoagulants | Prescriptions of platelet aggregation inhibitors and statins were still more frequently provided to men than to women in 2016, independently of confounders. |
| [22] | Sex differences in characteristics, treatments, and outcomes among patients hospitalized for non–ST-segm… | 2022 | 4611 NSTEMI patients (39.8% women) | 151 Chinese hospitals, nationally representative of patients admitted in 2006, 2011, and 2015 | 2-stage random sampling design | In hospital | Aspirin, clopidogrel/ticagrelor, dual antiplatelet therapy, β-blockers, ACE inhibitor/ARB, statins, and parenteral anticoagulant | Women were less likely to receive treatments than men, with significant differences for aspirin in 2015. |
| [23] | Trends in provision of medications and lifestyle counseling in ambulatory settings by gender and race f… | 2023 | 11,033 appointments for adults with atherosclerotic cardiovascular disease | Nationally representative ambulatory care, the US, 2006–2016 | Cross-sectional | In clinic | Statin therapy and aspirin prescription | Women were less likely than men to receive statin therapy and aspirin prescription. |
| [24] | Population-wide cohort study of statin use for the secondary cardiovascular disease prevention in Scotland in 20… | 2022 | 167,978 patients with an ASCVD event | Linked National Health Service Scotland administrative data, 2009–2017 | National retrospective cohort | Average: 4.6 years | Statins | Women were less likely to initiate therapy. |
| [25] | Persisting gender differences and attenuating age differences in cardiovascular drug use for prevention and t… | 2013 | 1,230,290 patients from primary care and 15,651 patients from secondary care | PHARMO database between 1998 and 2010, Holland | Cohort and observational | 36 months | Lipid-lowering drugs, blood-pressure lowering drugs, beta blockers, and antithrombotics | In primary care, fewer women used lipid-lowering drugs. During hospitalisation, fewer women used cardiovascular drugs. In secondary care (36 months after discharge), young women used fewer drugs in general. |
| [26] | Age and gender differences in medical adherence after myocardial infarction: Wome… | 2018 | 59,534 patients (34% women) | Dutch health insurance register from 2012 and 2013 | Retrospective, cohort, and observational | One year | Aspirin, P2y12-inhibitors, statin, beta blockers, ACE-/AT2-inhibitors, vitamin K antagonists, novel oral anticoagulant | There was lower use of five indicated drug treatments in women; differences were more evident in those with NSTEMI. |
| [27] | Dyslipidemia management in patients with coronary artery disease. Data from the POLASPIRE survey | 2021 | 1236 CHD patients (29% women) | Poland, within the prior 6 to 24 months | Cross-sectional and multi-centre | Six–eighteen months after hospital discharge | Statins and other medications | Male sex was correlated with statin prescriptions at discharge. |
| [28] | Drivers of the sex disparity in statin therapy in patients with coronary artery disease: A cohort study | 2016 | 24,338 CHD patients (9006 [37%] women) | Between 2000 and 2011 at two academic medical centres in Boston | Retrospective cohort | Followed for at least one year | Statins | Women were less likely to either have initiated statin therapy or to have persistent statin therapy at the end of follow-up. |
| [29] | Tackling inequalities: are secondary prevention therapies for reducing post-in… | 2014 | 1327 patients discharged after a heart attack | Municipality of Rovigo, Italy, between January 2002 and November 2009 | Retrospective cohort and observational | Average follow-up: 3.39 years | ACE inhibitors, beta blockers, platelet aggregation inhibitors, statins, omega-3 triglycerides, and anticoagulants | Women were less likely to use statins and anti-platelet drugs. |
| [30] | Age and sex inequalities in the prescription of evidence-based pharmacological therapy follo… | 2014 | 747 STEMI patients and 1364 NSTEMI patients (67% men) | 10 Portuguese hospitals, 2008–2009 | Consecutive cases and observational | Hospital discharge | Aspirin, clopidogrel, beta blockers, ACE inhibitor/ARB, and statins | There was a lower likelihood of women receiving aspirin and clopidogrel at discharge. |
| [31] | Sex differences in the treatment and outcome of Korean patients with acute m… | 2015 | 85,329 MI patients | Korean hospitals between 2003 and 2007 | Retrospective and observational cohort | 30 days | Aspirin, thrombolytic drugs, beta blockers, and cholesterol-lowering drugs | After adjustment, men were more likely to receive pharmacological treatments. |
| [32] | Investigating the prevalence, predictors, and prognosis of suboptimal statin use early af… | 2017 | 1005 ACS NSTEMI patients | 16 hospitals in the UK between 2008 and 2013 | Prospective and cohort | Median follow-up: 16 months | Intensive statin therapy | Female sex was a predictor of the underuse of optimal statin treatment (reduced doses, cessation, changing to a less potent statin, non-compliance with treatment). |
| [33] | Predictors of nonuse of a high-potency statin after an acute coronary syndrome: Insights from the stabilization of plaq… | 2017 | 12,446 ACS patients | 36 countries between 2009 and 2011 | Retrospective analysis of data from a double-blind, controlled, and randomised study | Three months | Statins and high-intensity statins | Female sex predicted the non-use of statins. Patients not treated with high-intensity statins were more likely to be women. |
| [34] | Differences in management and outcomes for men and women with ST-elevation myocardial infarction | 2018 | 2898 STEMI patients (715 women) | Registry of 41 Australian hospitals between February 2009 and May 2016 | Cohort, prospective, and observational | Six months | Aspirin, second antiplatelet, beta blockers, ACE inhibitor/ARB, and statins | At discharge, fewer women received beta blockers and statins. |
| [35] | Gender-related differences in antiplatelet therapy and impact on 1-year clinical outc… | 2019 | 840 ACS patients (26% women) | 8 centres between January 2014 and December 2016 | Multi-centre registry and observational | Follow-up: one year | Dual anti-platelet therapy, ticagrelor, clopidogrel, and Prasugrel | Drug-eluting stents and dual anti-platelet therapy were used more in men than in women. |
| [36] | Trends in gender differences in cardiac care and outcome after acute myocardial infarction in western Sweden: A report fro… | 2015 | 48,118 MI patients (35.4% women) | Cardiac units in Sweden between January 1995 and October 2014 | National registry and observational | In hospital, at thirty days and at one year | Acetylsalicylic acid, aniplatelets, beta blockers, ACE inhibitor/ARB, oral anticoagulants, statins, IV diuretics, and IV inotropes | Compared to men, women younger than 60 were less likely to receive indicated treatment at discharge (beta blockers, ECAn or angiotensin receptor inhibitors, statins, and P2y12 antagonists). |
| [37] | Long-term quality of prescription for ST-segment elevation myocardial infarction (STEMI) patients: A real world… | 2020 | 361 STEMI patients | A hospital in Switzerland between 2014 and 2016 | Prospective and observational | At discharge and after one year | Aspirin, P2y12 inhibitors, statin, ACEn inhibitors, and beta blockers | Female sex was a predictor of not receiving an appropriate prescription at discharge, but it was not a predictor after one year. |
| [38] | Gender difference in secondary prevention of cardiovascular disease and outcomes following the survival of acut… | 2021 | 9283 discharged ACS patients | 43 Australian hospitals between 2009 and 2018 | Observational and prospective | Six and thirteen months | Aspirin, lipid-lowering therapy, anti-platelet drugs, beta blockers, and enzyme inhibitors | After one year, women were less likely to be taking more than 75% of examined medications. |
| [39] | Sex differences in distribution, management and outcomes of combined ischemic-bleeding … | 2021 | 584,360 ACS patients | Hospitals in the UK between January 2010 and December 2017 | Retrospective | ACE inhibitors, beta blockers, statins, antiplatelets, aspirin, P2y12 inhibitor, and DAPT | In high-risk patients, women were less likely to receive guideline-recommended treatment (dual anti-platelet therapy). | |
| [40] | Sex disparities in post-acute myocardial infarction pharmacologic treatment init… | 2015 | 12,261 MI survivors (3783 women) | Registries from British Colombia between 2007 and 2009 | Retrospective, populational, and cohort | One year after discharge | Prescriptions for ACEn inhibitors, beta blockers, and statins | Young men were more likely than women to start treatment. There were no sex differences in treatment compliance. |
| [41] | Clinical implications of switching from intensive to moderate statin therapy after acute coronary syndromes | 2011 | 1321 CHD patients (886 men) | All patients discharged from an Italian unit after a CHD in a 6.5-year period | Cohort and observational | 12 months | Intensive versus moderate statins | Statin therapy was more likely to be changed from a high intensity to a moderate intensity in women. |
| [42] | Sex differences in treatment and prognosis of acute coronary syndrome with inter… | 2018 | 1214 patients (24% women) | One Spanish centre, January 2013 to January 2016 | Prospective, consecutive, cohort, and observational | Ticagrelor/Prasugrel, ACE inhibitors, beta blockers, and statins | Fewer women received potent anti-platelet drugs. | |
| [43] | Prasugrel for Japanese patients with ischemic heart disease in long-term clinical practice (PR… | 2020 | 4155 patients treated for CVD | Japan between 1 June 2015 and 31 May 2018 | Observational | One year | Prasugrel and aspirin | Female sex predicted that treatment was employed for less than 360 days. |
| [44] | Gender disparities in evidence-based statin therapy in patients with cardiovascular disease | 2015 | 972,532 CVD patients | 130 US healthcare units for veterans between October 2010 and September 2011 | National cohort and observational | Statins | Women were less likely to receive statins or high-intensity statins. Female sex was an independent predictor of not receiving statins or high-intensity statins, with significant variability as a function of the unit. | |
| [45] | Incidence, predictors, and clinical impact of early prasugrel cessation in patients with ST-elevation myocardial … | 2018 | 1830 patients (17% women) treated with stents | All patients at Bern University Hospital, Switzerland, in 2009 | Two prospective registries and a clinical trial | One year | Prasugrel after stenting | Female sex predicted the discontinuation or interruption of treatment and cessation of Prasugrel for any reason. |
| [46] | No gender differences in prognosis and preventive treatment in patients with A… | 2012 | 1595 patients (834 women) hospitalised with MI with no significant stenoses found in coronarography | Danish registers between 2005 and 2007 | National cohort | 60 days after discharge | Lipid inhibitors, beta blockers, cloridogrel, and aspirin | More women took lipid inhibitors; there were no other sex differences. |
| [47] | Medical care of acute myocardial infarction patients in a resource limiting country,… | 2019 | 1106 patients (67.3% men) | A hospital in Trinidad between March 2011 and March 2015 | Retrospective, cross-sectional, and observational | Different medications and therapies | No sex difference was found in medication use, although there were few data for women. | |
| [48] | Sex differences in cardiac medication use post-catheterization in patients undergoing coronary angiography | 2017 | All angina patients treated with angiography in British Columbia (n = 7.535) | British Columbia between January 2008 and March 2010 | Observational | Three months prior to and three months after treatment | ACEn inhibitors, angiotensin receptor blockers, calcium channel blockers, beta blockers, statins, and anti-platelet agents | There were no significant differences according to sex. |
| [49] | Propensity score-matched analysis of effects of clinical characteristics and treatment… | 2011 | 3510 consecutive patients (32% women) after MI | 10 cardiology centres in eastern France between January 2006 and December 2007 | Observational and two paired cohorts | 30 days | Aspirin, clopidogrel, ACE inhibitor/ARB, beta blockers, and statins | Women received less medical treatment. After adjustment, this effect disappeared. |
| [50] | Medical treatment in coronary patients: Is there still a gender gap? Results from European S… | 2020 | 8261 patients (25.8% women) | ESC EORP EUROASPIRE V survey of 131 centres in 27 countries, 2017–2017 | Cross-sectional and observational | Six months and two years | Aspirin/other antiplatelets, beta blockers, ACE inhibitors/ARB, ACE-I, ARB, statins, anticoagulants, calcium channel blockers, diuretics, glucose-lowering drugs, insulin, antidepressants, and anti-anxiety drugs | Generally, there were no sex differences in the number of prescriptions or medication use. Fewer women were prescribed statins but more women were prescribed diuretics. |
| [51] | Sex differences in the treatment and outcome of patients with acute coronary … | 2014 | 32,821 ACS patients (8884 women) treated with PCI with ischemic bleeding risk | Taiwan between January 2006 and December 2007 | Retrospective cohort and observational | Follow-up: minimum of one year | Aspirin, clopidogrel, beta blockers, ACE inhibitor/ARB, and statins | Women were less likely to receive aspirin and clopidogrel but more likely to receive beta blockers and statins. |
3.2. Invasive Treatments, Percutaneous Coronary Interventions (PCIs) or Surgery, and Thrombolytic Reperfusion Therapy in Both Acute and Chronic Stages
| Author | Title | Year | Sample | Context | Design | Time-Frame | Treatment | Main Findings |
|---|---|---|---|---|---|---|---|---|
| [16] | Sex differences in in-hospital management and outcomes of patients with acute coronary syndrome | 2019 | 82,196 ACS patients from 192 hospitals | AHA and the Chinese Society of Cardiology national registry between 2014 and 2018 | Prospective and observational | Reperfusion therapy | Women were less likely to have received reperfusion treatment for STEMI, including PCI. | |
| [20] | Treatment gaps, 1-year readmission and mortality following myocardial infarction by diabetes status, sex and so… | 2022 | 43,272 patients after MI | All survivors of MI in Victoria, Australia, July 2012–June 2017 | Observational cohort | One year | PCI and CABG | Females were less likely to receive either PCI or CABG. |
| [21] | Sex differences in time trends in acute coronary syndrome management and in 12-month lethality: Data from the Frenc… | 2022 | 3196 ACS patients | All patients (aged 35–74) from the MONICA registries, France, January–December 2006 or October 2015–March 2016 | Observational cohort | Twelve months in 2006 or six months in 2016 | Revascularisation | Revascularisation treatment was still more frequently provided to men than to women in 2016, independently of confounders. |
| [22] | Sex differences in characteristics, treatments, and outcomes among patients hospitalized for non–ST-segm… | 2022 | 4611 NSTEMI patients (39.8% women) | 151 Chinese hospitals with patients admitted in 2006, 2011, and 2015 | Two-stage random sampling design | In hospital | PCI and other invasive strategies | Women were less likely to receive treatments than men, with significant differences for PCI and invasive strategies in 2011 and 2015. |
| [31] | Sex differences in the treatment and outcome of Korean patients with acute m… | 2015 | 85,329 MI patients | Korean hospitals between 2003 and 2007 | Retrospective, cohort, and observational | 30 days | Coronary angiography, cardiac catheterisation, PCI, and CABG | After adjustment, fewer women than men received catheterisation, grafts, and PCI. |
| [34] | Differences in management and outcomes for men and women with ST-elevation myocardial infarction | 2018 | 2898 STEMI patients (715 women) | A registry of 41 Australian hospitals between February 2009 and May 2016 | Cohort, prospective, and observational | Follow-up: six months | Coronary angiography, total revascularisation, timely revascularisation, PCI, thrombolysis, and CABG | Women were less likely to have received treatment with PCI or CABG, coronary angiography, or revascularisation. |
| [35] | Gender-related differences in antiplatelet therapy and impact on 1-year clinical outc… | 2019 | 840 ACS patients (26% women) | Eight Italian centres between January 2014 and December 2016 | Multi-centre registry and observational | One year | Drug-eluting stents | Drug-eluting stents were used more in men than in women. |
| [36] | Trends in gender differences in cardiac care and outcome after acute myocardial infarction in western Sweden: A report fro… | 2015 | 48,118 MI patients (35.4% women) | Cardiac units in Sweden between January 1995 and October 2014 | National registry and observational | In hospital, after thirty days and one year | Coronary angiography and PCI (reperfusion treatment) | Women with STEMI were less likely to undergo coronary angiography than men with STEMI in adjusted analysis. |
| [39] | Sex differences in distribution, management and outcomes of combined ischemic-bleeding … | 2021 | 584,360 ACS patients | Hospitals in the UK between January 2010 and December 2017 | Retrospective | Guideline-recommended therapies | In high-risk patients, women were less likely to receive guideline-recommended therapies (revascularisation, PCI, and graft). | |
| [47] | Medical care of acute myocardial infarction patients in a resource limiting country,… | 2019 | 1106 patients (67.3% men) | One hospital in Trinidad between March 2011 and March 2015 | Retrospective, cross-sectional, and observational | Therapies, surgery, and thrombolysis | Generally, surgery was reported to be little used. More men were treated with thrombolysis. | |
| [49] | Propensity score-matched analysis of effects of clinical characteristics and treatment… | 2011 | 3510 patients (32% women) after MI | Consecutive cases between January 2006 and December 2007 from 10 cardiology centres in eastern France | Observational and two matched cohorts | 30 days | PCI, CABG, thrombolysis, and other reperfusion | Fewer women were treated with angiography and reperfusion, even after adjustment. |
| [52] | Does prior coronary artery bypass surgery alter the gender gap in patients presenting wit… | 2012 | 16,750 ACS patients | The registry of a hospital in Doha, Qatar, between January 1991 and December 2010 | Retrospective, observational, and cohort | Thrombolysis, PCI, and reperfusion | Women were less likely to receive reperfusion and early invasive therapies. | |
| [53] | Disparities by race, ethnicity, and sex in treating acute coronary syndromes | 2012 | 20,604 Medicare claimants (health insurance) with ACS | A US registry in 2001 | Retrospective and observational | Coronary revascularisation | Women presented lower rates than men of any type of revascularisation. Black women had the lowest rates. | |
| [54] | Do clinical factors explain persistent sex disparities in the use of acute reperfusion ther… | 2013 | 32,676 STEMI patients | Sweden between 2004 and 2008 | Retrospective | Reperfusion therapy | Reperfusion therapy used less in women; reasons varied as a function of age. | |
| [55] | Gender, socioeconomic position, revascularization procedures and mortality in patients presenting with STE… | 2014 | 5792 MI patients | A database from Piedmont, Italy, between January 2008 and December 2008 | Observational | In hospital and after one year | PCI | Women were less likely to receive revascularisation. |
| [56] | Clinical profile of patients with no-reperfusion therapy in Bosnia and Herzegovina and … | 2014 | 633 STEMI patients | 14 hospitals in Bosnia and Serbia between October 2012 and September 2013 | Observational registry | Reperfusion | Female sex was an independent predictor of reperfusion. | |
| [57] | Gender difference in treatment and mortality of patients with ST-segment elevation myocardial infarction admitte… | 2015 | 8404 STEMI patients | A government registry of 136 hospitals in Victoria between July 2005 and June 2010 | Retrospective | Five years | Angioplasty, stent, and CABG | Proportionately fewer women received reperfusion treatment for STEMI. |
| [58] | Gender differences in the prevalence and treatment of coronary chronic total occlusions | 2016 | 1690 patients with chronic total occlusion and 7682 control | Three units in Canada between Mar 2008 and June 2009 | Retrospective, Canadian registry and multi-centre | Revascularisation | The PCI rate in patients was similar between men and women. Fewer women received a bypass graft and, of those receiving a bypass graft, fewer women received revascularisation. | |
| [59] | Revascularization treatment of emergency patients with acute ST-segment elevation myocardial infarction in Switz… | 2016 | 9696 cases (71.6% received revascularisation; 29.2% women) | A Swiss national registry, 300 hospitals, 2010–2011 | Observational | Revascularisation | Female sex was a predictor of not receiving revascularisation. | |
| [60] | Reperfusion therapy for ST-elevation acute myocardial infarction in Eastern Europe: the ISACS-TC registry | 2016 | 7982 STEMI patients | 57 hospitals in Eastern European countries between January 2010 and February 2015 | Observational | 30 days | Reperfusion compared with no reperfusion | Female sex was the strongest predictor of no reperfusion. |
| [61] | Gender based differences in drug eluting stent implantation—data from the German ALKK… | 2017 | 100,704 cases | A national registry of 28 centres in Germany between 2005 and 2009 | Prospective and observational | Drug-eluting stents | There were lower rates of drug-eluting stent use in women; this difference was significant in the over-70s. | |
| [62] | Sex-related inequalities in management of patients with acute coronary syndrome—r… | 2018 | 1757 discharged ACS NSTEMI patients and 1184 STEMI patients | 10 Portuguese hospitals between 2008 and 2010 | Consecutive cases, retrospective, and observational | Revascularisation and reperfusion | In STEMI patients, women were less likely to receive an angiography, even after adjustment, and less likely to receive revascularisation, but not after adjustment. | |
| [63] | Sex, race, and insurance status differences in hospital treatment and outcomes foll… | 2018 | 38,163 OHCA patients (42% women) | The Californian regional registry between 2011 and 2015 | Retrospective | Five years | Treatment in a specialised PCI unit | Female sex was a predictor of lower rates of treatment at a PCI unit and with catheterisation. |
| [64] | Usage of PCI and long-term cardiovascular risk in post-myocardial infarction patient… | 2019 | 32,909 MI patients | Finland between 2009 and 2012 | Observational, retrospective cohort | Minimum of one year | PCI | Female sex was an independent predictor of not receiving PCI. |
| [65] | Healthcare disparities for women hospitalized with myocardial infarction and angina | 2020 | 7878 patients hospitalised due to MI or angina (40% women) | The national Scottish registry between 1 October 2013 and 30 June 2016 | Registry and observational | At discharge, six months, and one year | PCI and other coronary angiography | Women were more likely to receive guideline-recommended therapy prior to hospitalisation and more likely to receive an invasive intervention upon arrival. Fewer women received an angiography or PCI and guideline-recommended therapy after MI. |
| [66] | Age-related sex differences in clinical presentation, management, and outcomes i… | 2020 | 15,532 hospitalised ACS patients | Seven registries from the Persian Gulf between 2005 and 2017 | Multi-register | One year | Revascularisation | In patients younger than 65, women were less likely than men to receive thrombolytic therapy and PCI. |
| [67] | Treatment effect of percutaneous coronary intervention in men versus w… | 2021 | 413,500 (30.7% women) STEMI patients | A national database, the US, between January 2016 and December 2018 | Observational | Primary PCI | Women were less likely to receive angiography and PCI. | |
| [68] | Age and sex differences and temporal trends in the use of invasive and noninvasive procedures in patients hospi… | 2022 | 1681 men and 1154 women with initial acute MI | All medical centres in central Massachusetts, 2005–2018 | Observational | In hospital | Echocardiography, coronary angiography, PCI, and coronary artery bypass graft surgery | Fewer women underwent cardiac catheterisation, PCI, and coronary artery bypass graft surgery. |
| [69] | Women are less likely to survive AMI presenting with out-of-hospital cardiac arrest: A nationwide study | 2022 | 16,278 acute MI patients (22.7% women) | The MINAP registry, the UK, 2010–2017 | Population-based retrospective cohort study | In hospital | Coronary angiography, PCI, coronary artery bypass graft, and myocardial revascularisation | Women were less likely to receive dual antiplatelet therapy, beta blockers, ACE inhibitors, coronary angiography, and PCI. After adjustment, women had greater odds of receiving coronary angiography and coronary artery bypass graft. |
| [70] | Sex disparities in diagnostic evaluation and revascularization in patients with acute myocardial infarct… | 2023 | 9,259,932 acute MI patients | A national database of all inpatient discharges from nonfederal hospitals in the US, 2005–2019 | Observational cohort; 15 years divided into five 3-year periods | In hospital | PCI and CABG | Women received significantly less PCI and CABG than men in all time periods. In STEMI patients but not in NSTEMI patients, these disparities decreased over time. After all adjustments, gender disparities remained significant for all procedures in NSTEM and STEMI patients in the most recent period. |
| [71] | Comparisons of the uptake and in-hospital outcomes associated with second-gener… | 2016 | 1,129,122 men and 538,835 women | The CathICP registry, the US, between July 2009 and March 2013 | Observational, real-life cohort | PCI with second-generation drug-eluting stents | Second-generation stents were used more in men than in women during the first 1.5 years of the study; after this period, no differences emerged. | |
| [72] | Evaluation of gender differences in door-to-balloon time in ST-elevation myocardial infarction | 2013 | 735 STEMI patients | 2006–2010; two STEMI PCI centres based in tertiary care hospitals in Adelaide. | Prospectively designed registry | In hospital | Timely care provision and time to balloon | Women experienced delays in code-to-balloon and, thus, DTB time. After multivariate adjustment, independent determinants of DTB time included female gender. |
| [73] | Association between gender and shortterm outcome in patients with ST elevation my… | 2017 | 1862 STEMI patients | An international registry between September 2011 and October 2013 | Multi-centre, randomised, and double-blinded | 30 days | Time to procedure | Women experienced greater delays between symptoms and echography and between PCI and angiography following PCI. |
| [74] | Time to reperfusion in high-risk patients with myocardial infarction undergoing primar… | 2019 | 1340 STEMI patients | 18 Portuguese centres between 2011 and 2016 | Observational | Reperfusion with PCI | Greater delays were found in women and, resultantly, time to revascularisation was longer in women than in men. | |
| [75] | Sex differences in time to primary percutaneous coronary intervention and ou… | 2022 | 1244 STEMI patients treated with PCI (24% female) | One tertiary referral centre in Australia, 1 January 2010 to 31 December 2019 | Cohort of consecutive cases | 10 years | PCI | There were longer median times in females and females were less likely to receive FMC-to-ballon times of less than 90 mins. There were significantly longer total and direct STB, FMCTB, and DTB durations for females. There were significant differences in geometric mean times from symptom onset to FMC and table to balloon. |
| [76] | Revascularization trends in patients with diabetes mellitus and multivessel coronary arte… | 2016 | 29,769 MI patients from 539 hospitals | The US between July 2008 and December 2014 | Observational comparison of two treatments | Bypass graft (the most indicated) compared with PCI (the least indicated) | Female sex predicted PCI use over bypass graft. | |
| [77] | Disparities in drug-eluting stent utilization in patients with acute ST-elevation myocardial infarction: An analysis of the … | 2022 | 1,189,237 ± 18,498.93 inpatient visits with STEMI and PCI (>70% men) | 2009 to 2018, the US National Inpatient Sample database | Retrospective | In hospital | Stents | Women were more likely to undergo DES implantation. |
| [78] | Gender differences in patient and system delay for primary percutaneous coronary intervention: current trends i… | 2019 | 4360 patients (967 women) | A Swiss STEMI healthcare network (24 hospitals) between January 2000 and December 2016 | Observational | 24 h (from symptoms to PCI) | General healthcare and PCI within 24 h after symptom onset | There was no difference in time taken to seek assistance and receive PCI according to sex. |
3.3. Rehabilitation Programmes and Other Interventions
| Author | Title | Year | Sample | Context | Design | Time-Frame | Treatment | Main Findings |
|---|---|---|---|---|---|---|---|---|
| Rehabilitation programmes | ||||||||
| [16] | Sex differences in in-hospital management and outcomes of patients with acute coronary syndrome | 2019 | 82,196 ACS patients from 192 hospitals | AHA and the Chinese Society of Cardiology national registry between 2014 and 2018 | Prospective | Rehabilitation programme | Fewer women received counselling to quit smoking and rehabilitation. | |
| [21] | Sex differences in time trends in acute coronary syndrome management and in 12-month lethality: Data from the Frenc… | 2022 | 3196 patients with first ACS | All patients (aged 35–74) from MONICA registries, France, January–December 2006 or October 2015–March 2016 | Observational cohort | Twelve months in 2006 or six months in 2016 | Functional rehabilitation | Functional rehabilitation was still more frequently provided to men than to women in 2016, independently of confounders. |
| [34] | Differences in management and outcomes for men and women with ST-elevation myocardial infarction | 2018 | 2898 STEMI patients (715 women) | A registry of 41 Australian hospitals between February 2009 and May 2016 | Cohort, prospective, and observational | Six months | Cardiac rehabilitation referral | At discharge, fewer women were referred to a rehabilitation programme. |
| [79] | Trends and disparities in referral to cardiac rehabilitation after percutane… | 2011 | 145,661 patients following PCI | 31 hospitals in Michigan between 2003 and 2008 | Observational registry | Six years | Rehabilitation programme | There was a lower referral rate in women. |
| [80] | Predictors of cardiac rehabilitation referral, enrolment and completion af… | 2021 | 666 heart attack patients (66% men) | Hospitalisations at a single centre in Holland in 2015 or 2016 | Retrospective cohort | Maximum of six months after the event | Rehabilitation programme | Non-referral was associated with the female sex. |
| [81] | Cardiac rehabilitation attendance and outcomes in coronary artery disease patients | 2012 | 5886 patients (20.8% women) after angiography | Calgary, Canada, between 1996 and 2009 | Prospective cohort | Programme start and 12 weeks later | 12-week cardiac rehabilitation programme | Women were less likely to finish rehabilitation. |
| [82] | Predictors of early and late enrollment in cardiac rehabilitation, among those r… | 2012 | 2096 patients after a heart attack | A registry of 19 centres in the US (PREMIER) | Prospective andobservational | One and six months | Rehabilitation programmes | Women were less likely to participate in the programme one month after the start. |
| [83] | Factors associated with non-attendance at exercise-based cardiac rehabilitation | 2019 | 31,297 patients | The SWEDEHEART national registry, 2010–2016 | Observational | Six weeks and one year | Rehabilitation programme | It was more likely that women attended the rehabilitation programme. |
| [84] | Participation in cardiac rehabilitation, readmissions, and death after acute myocardial infarction | 2014 | 2991 heart attack patients | A single hospital in Minnesota between January 1987 and September 2010 | Population-based surveillance study | Rehabilitation programme | 1569 (52.5%) participated in rehabilitation; the male participation rate decreased throughout the study. | |
| [85] | Yoga-based cardiac rehabilitation after acute myocardial infarction: A randomized trial | 2020 | 3959 heart attack patients | 24 centres in India | Randomised trial | Median: 22 months; minimum: 6 months | Yoga programme (n = 1970) compared with traditional treatment plus education (n = 1989) | There was no difference in session attendance according to sex. |
| Other | ||||||||
| [23] | Trends in provision of medications and lifestyle counseling in ambulatory settings by gender and race f… | 2023 | 11,033 visits by adults with CHD | Nationally representative ambulatory care, US, 2006–2016 | Cross-sectional | In clinic | Lifestyle counselling (e.g., nutrition, exercise, weight reduction) | This was lower in women but not significantly. |
| [63] | Sex, race, and insurance status differences in hospital treatment and outcomes foll… | 2018 | 38,163 patients after OHCA (42% women) | A Californian regional registry between 2011 and 2015 | Retrospective | Five years | Resuscitation | Women had increased odds of receiving a do-not-resuscitate order within one day of admission. |
| [68] | Age and sex differences and temporal trends in the use of invasive and noninvasive procedures in patients hospi… | 2022 | 1681 men and 1154 women with initial acute MI | All medical centres in central Massachusetts, 2005–2018 | Observational | In hospital | Exercise stress testing | There were no sex differences in the receipt of echocardiography and exercise stress testing. |
| [72] | Evaluation of gender differences in door-to-balloon time in ST-elevation myocardial infarction | 2013 | 735 STEMI patients | 2006-2010, two STEMI PCI centres based in tertiary care hospitals in Adelaide. | Prospectively designed registry | In hospital | Timely care provision | Women experienced longer delays in door-to-code time. |
| [86] | Delayed care and mortality among women and men with myocardial infarction | 2017 | 6022 STEMI patients | An international registry of 41 hospitals between October 2010 and April 2016 | Stratified analysis | 30 days | Hospital care provision | Despite there being no differences in time from symptom onset to seeking assistance, women experienced longer symptom-onset-to-hospital-arrival times. |
| [87] | Association of door-in to door-out time with reperfusion delays and outcomes among … | 2011 | 14,821 STEMI patients | 298 STEMI units in the US between January 2007 and March 2010 | Cohort and retrospective | Referral time | Female sex predicted having a referral time (from hospital arrival to being sent to receive reperfusion) longer than 30 min. | |
| [88] | Sex bias in admission to tertiary-care centres for acute myocardial infarction and cardiogenic shock | 2021 | 340,490 STEMI patients (29.2% female) | Spanish national database, 2003 to 2015 | Observational, retrospective study | In hospital | Referral to revascularisation-capable hospital | Women were less frequently admitted to a revascularisation-capable hospital or hospitals with ICCUs than men. |
| [89] | Gender disparities in patient education provided during patient visits with a diagnosis… | 2019 | 17,332 CVD patients | National survey, the US, 2005–2014 | Retrospective, cross-sectional, and observational | Education | Women were less likely than men to receive education targeted towards patients. Female sex was an independent predictor of not receiving education. | |
| [90] | Effect of patient sex on triage for ischaemic heart disease and treatment onset times: A retr… | 2014 | 21,080 MI patients | 34 Australian intensive care units between 2005 and 2010 | Retrospective | Triage, treatment | More men than women were correctly sent to triage. Time to treatment was shorter in men than in women. | |
| [91] | Social determinants of clinical visits after left main percutaneous coronary intervention versus coronary … | 2023 | 3816 patients after left main PCI or CABG | A single centre, January 2015 to December 2022 | Observational | Seven years | Clinic visits | Female gender was a strong predictor of having a follow-up visit. |
| [92] | Uptake of prescription smoking cessation pharmacotherapies after hospitalization for major cardiovascular disease | 2022 | 20,162 smokers with major CVD (31% female) | All hospitalisations New South Wales, Australia, July 2013–December 2018 | Population-based cohort study | 90 days post-discharge | Smoking cessation pharmacotherapy (SCP) | Females were more likely than males to be dispensed an SCP prescription; however, this was not maintained after adjusting for potential confounders. |
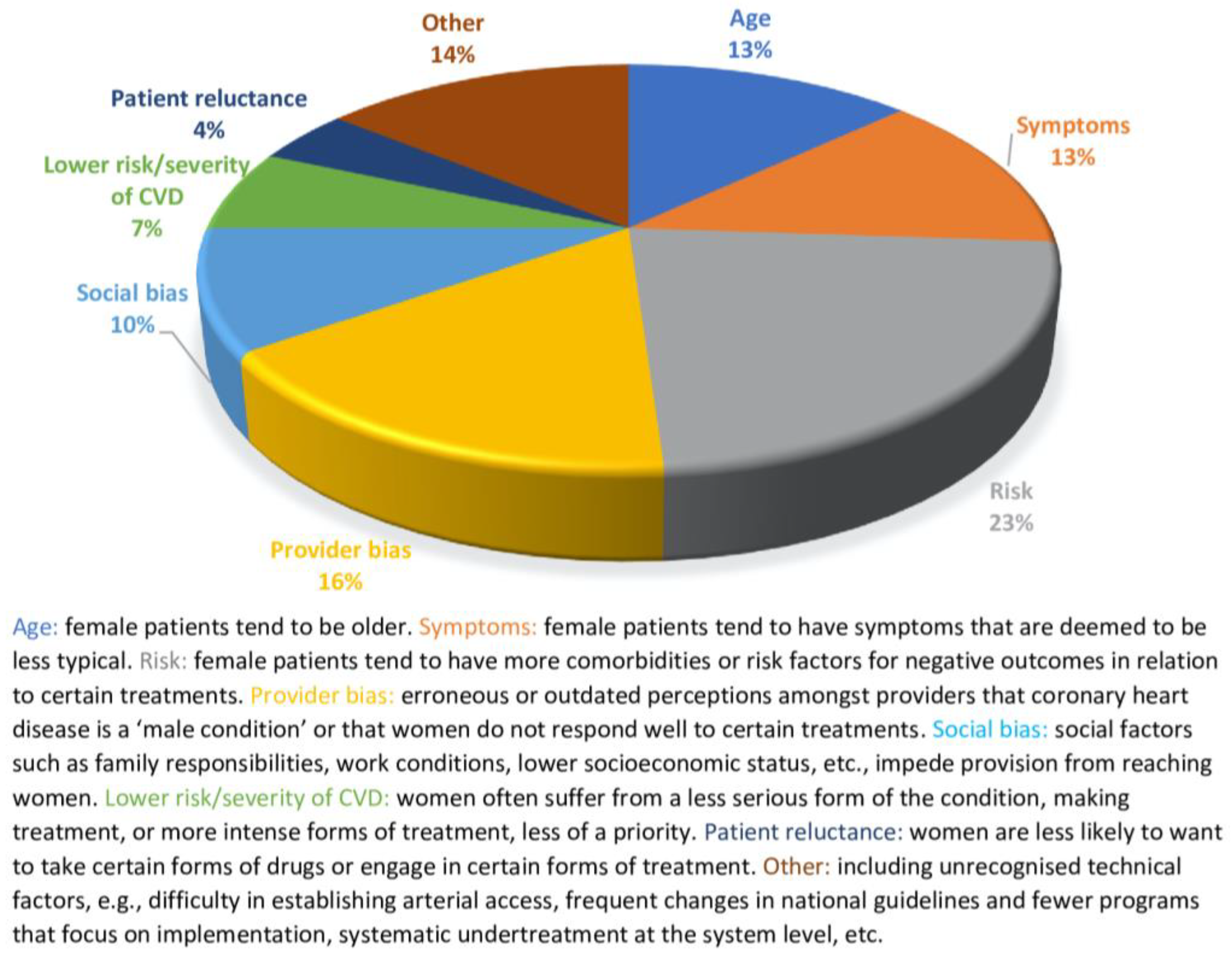
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| CHD | coronary heart disease |
| CVD | cardiovascular disease |
| ACE | angiotensin-converting enzyme |
| PCI | percutaneous coronary intervention |
| DAPT | dual antiplatelet therapy |
| STEMI | ST-segment-elevation myocardial infarction |
References
- Mensah, G.A.; Fuster, V.; Murray, C.J.L.; Roth, G.A. Global burden of cardiovascular diseases and risks, 1990–2022. J. Am. Coll. Cardiol. 2023, 82, 2350–2473. [Google Scholar] [CrossRef]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Beaton, A.Z.; Boehme, A.K.; Buxton, A.E.; et al. Heart disease and stroke statistics—2023 update: A report from the American Heart Association. Circulation 2023, 147, E93–E621. [Google Scholar] [CrossRef] [PubMed]
- Paradossi, U.; Taglieri, N.; Massarelli, G.; Bruno, A.; Taddei, A.; Nardi, E.; Ghetti, G.; Palmerini, T.; Trianni, G.; Mazzone, A.; et al. Female gender and mortality in ST-segment-elevation myocardial infarction treated with primary PCI. J. Cardiovasc. Med. 2022, 23, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Townsend, N.; Kazakiewicz, D.; Wright, L.F.; Timmis, A.; Huculeci, R.; Torbica, A.; Gale, C.P.; Achenbach, S.; Weidinger, F.; Vardas, P. Epidemiology of cardiovascular disease in Europe. Nat. Rev. Cardiol. 2022, 19, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Cushman, M.; Shay, C.M.; Howard, V.J.; Jiménez, M.C.; Lewey, J.; McSweeney, J.C.; Newby, L.K.; Poudel, R.; Reynolds, H.R.; Rexrode, K.M.; et al. Ten-year differences in women’s awareness related to coronary heart disease: Results of the 2019 American Heart Association National Survey—A Special Report from the American Heart Association. Circulation 2021, 143, E239–E248. [Google Scholar] [CrossRef]
- Woodward, M. Cardiovascular disease and the female disadvantage. Int. J. Environ. Res. Public Health 2019, 16, 1165. [Google Scholar] [CrossRef]
- Jin, X.; Chandramouli, C.; Allocco, B.; Gong, E.; Lam, C.S.P.; Yan, L.L. Women’s participation in cardiovascular clinical trials from 2010 to 2017. Circulation 2020, 141, 540–548. [Google Scholar] [CrossRef] [PubMed]
- Daponte-Codina, A.; Knox, E.C.; Mateo-Rodriguez, I.; Seims, A.; Regitz-Zagrosek, V.; Maas, A.H.E.M.; White, A.; Barnhoorn, F.; Rosell-Ortiz, F. Gender and social inequalities in awareness of coronary artery disease in European countries. Int. J. Environ. Res. Public Health 2022, 19, 1388. [Google Scholar] [CrossRef]
- Warren, J. Remarks on angina pectoris. N. Engl. J. Med. Surg. 1812, 1, 1–11. [Google Scholar] [CrossRef]
- Moscucci, F.; Lavalle, F.; Campanale, A.; Politi, C.; Baggio, G.; Sciomer, S. Acute coronary syndromes: The gender gap in the new ESC guidelines still remains unfilled. J. Sex-Gender-Specif. Med. 2023, 9, 107–109. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’Connell, J.; Robertson, J. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 8 January 2025).
- Arnold, S.V.; Spertus, J.A.; Tang, F.; Krumholz, H.M.; Borden, W.B.; Farmer, S.A.; Ting, H.H.; Chan, P.S. Statin use in outpatients with obstructive coronary artery disease. Circulation 2011, 124, 2405–2410. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Poon, S.; Goodman, S.G.; Yan, R.T.; Bugiardini, R.; Bierman, A.S.; Eagle, K.A.; Johnston, N.; Huynh, T.; Grondin, F.R.; Schenck-Gustafsson, K.; et al. Bridging the gender gap: Insights from a contemporary analysis of sex-related differences in the treatment and outcomes of patients with acute coronary syndromes. Am. Heart J. 2012, 163, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Vatcheva, K.P.; Aparicio, V.; Araya, A.; Gonzalez, E.; Laing, S.T. Statin Prescription for Patients with Atherosclerotic Cardiovascular Disease from National Survey Data. Am. J. Cardiol. 2019, 124, 1–7. [Google Scholar] [CrossRef]
- Hao, Y.; Liu, J.; Liu, J.; Yang, N.; Smith, S.C.; Huo, Y.; Fonarow, G.C.; Ge, J.; Taubert, K.A.; Morgan, L.; et al. Sex differences in in-hospital management and outcomes of patients with acute coronary syndrome: Findings from the CCC Project. Circulation 2019, 139, 1776–1785. [Google Scholar] [CrossRef] [PubMed]
- Sundaram, V.; Bloom, C.; Zakeri, R.; Halcox, J.; Cohen, A.; Bowrin, K.; Briere, J.B.; Banerjee, A.; Simon, D.I.; Cleland, J.G.F.; et al. Temporal trends in the incidence, treatment patterns, and outcomes of coronary artery disease and peripheral artery disease in the UK, 2006–2015. Eur. Heart J. 2020, 41, 1636–1649. [Google Scholar] [CrossRef]
- Rosenson, R.S.; Farkouh, M.E.; Mefford, M.; Bittner, V.; Brown, T.M.; Taylor, B.; Monda, K.L.; Zhao, H.; Dai, Y.; Muntner, P. Trends in use of high-intensity statin therapy After myocardial infarction, 2011 to 2014. J. Am. Coll. Cardiol. 2017, 69, 2696–2706. [Google Scholar] [CrossRef] [PubMed]
- Minhas, A.M.K.; Ijaz, S.H.; Javed, N.; Sheikh, A.B.; Jain, V.; Michos, E.D.; Greene, S.J.; Fudim, M.; Warraich, H.J.; Shapiro, M.D.; et al. National trends and disparities in statin use for ischemic heart disease from 2006 to 2018: Insights from National Ambulatory Medical Care Survey. Am. Heart J. 2022, 252, 60–69. [Google Scholar] [CrossRef]
- Morton, J.I.; Ilomäki, J.; Wood, S.J.; Bell, J.S.; Huynh, Q.; Magliano, D.J.; Shaw, J.E. Treatment gaps, 1-year readmission and mortality following myocardial infarction by diabetes status, sex and socioeconomic disadvantage. J. Epidemiol. Community Health 2022, 76, 637–645. [Google Scholar] [CrossRef]
- Gauthier, V.; Montaye, M.; Ferrières, J.; Kai, S.H.Y.; Biasch, K.; Moitry, M.; Amouyel, P.; Dallongeville, J.; Meirhaeghe, A. Sex differences in time trends in acute coronary syndrome management and in 12-month lethality: Data from the French MONICA registries. Int. J. Cardiol. 2022, 361, 103–108. [Google Scholar] [CrossRef]
- Guo, W.; Du, X.; Gao, Y.; Hu, S.; Lu, Y.; Dreyer, R.P.; Li, X.; Spatz, E.S.; Masoudi, F.A.; Krumholz, H.M.; et al. Sex differences in characteristics, treatments, and outcomes among patients hospitalized for non-ST-segment-elevation myocardial infarction in China: 2006 to 2015. Circ. Cardiovasc. Qual. Outcomes 2022, 15, 405–415. [Google Scholar] [CrossRef] [PubMed]
- Mufarreh, A.; Shah, A.J.; Vaccarino, V.; Kulshreshtha, A. Trends in provision of medications and lifestyle counseling in ambulatory settings by gender and race for patients with atherosclerotic cardiovascular disease, 2006–2016. JAMA Netw. Open 2023, 6, E2251156. [Google Scholar] [CrossRef] [PubMed]
- Thalmann, I.; Preiss, D.; Schlackow, I.; Gray, A.; Mihaylova, B. Population-wide cohort study of statin use for the secondary cardiovascular disease prevention in Scotland in 2009–2017. Heart 2023, 109, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Koopman, C.; Vaartjes, I.; Heintjes, E.M.; Spiering, W.; Dis, I.; Herings, R.M.C.; Bots, M.L. Persisting gender differences and attenuating age differences in cardiovascular drug use for prevention and treatment of coronary heart disease, 1998–2010. Eur. Heart J. 2013, 34, 3198–3205. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Eindhoven, D.C.; Hilt, A.D.; Zwaan, T.C.; Schalij, M.J.; Borleffs, C.J.W. Age and gender differences in medical adherence after myocardial infarction: Women do not receive optimal treatment—The Netherlands claims database. Eur. J. Prev. Cardiol. 2018, 25, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Jankowski, P.; Kozieł, P.; Setny, M.; Paniczko, M.; Haberka, M.; Banach, M.; De Bacquer, D.; De Backer, G.; Kotseva, K.; Wood, D.; et al. Dyslipidemia management in patients with coronary artery disease. Data from the POLASPIRE survey. J. Clin. Med. 2021, 10, 3711. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Plutzky, J.; Shubina, M.; Turchin, A. Drivers of the sex disparity in statin therapy in patients with coronary artery disease: A cohort study. PLoS ONE 2016, 11, e0155228. [Google Scholar] [CrossRef] [PubMed]
- Buja, A.; Boemo, D.G.; Furlan, P.; Bertoncello, C.; Casale, P.; Baldovin, T.; Marcolongo, A.; Baldo, V. Tackling inequalities: Are secondary prevention therapies for reducing post-infarction mortality used without disparities? Eur. J. Prev. Cardiol. 2014, 21, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Pereira, M.; Araújo, C.; Dias, P.; Lunet, N.; Subirana, I.; Marrugat, J.; Capewell, S.; Bennett, K.; Azevedo, A. Age and sex inequalities in the prescription of evidence-based pharmacological therapy following an acute coronary syndrome in Portugal: The EURHOBOP study. Eur. J. Prev. Cardiol. 2014, 21, 1401–1408. [Google Scholar] [CrossRef][Green Version]
- Hong, J.S.; Kang, H.C. Sex differences in the treatment and outcome of Korean patients with acute myocardial infarction using the Korean National Health Insurance Claims Database. Medicine 2015, 94, e1401. [Google Scholar] [CrossRef]
- Turner, R.M.; Yin, P.; Hanson, A.; FitzGerald, R.; Morris, A.P.; Stables, R.H.; Jorgensen, A.L.; Pirmohamed, M. Investigating the prevalence, predictors, and prognosis of suboptimal statin use early after a non-ST elevation acute coronary syndrome. J. Clin. Lipidol. 2017, 11, 204–214. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Eisen, A.; Cannon, C.P.; Braunwald, E.; Steen, D.L.; Zhou, J.; Goodrich, E.L.; Im, K.A.; Dalby, A.J.; Spinar, J.; Daga, S.; et al. Predictors of nonuse of a high-potency statin after an acute coronary syndrome: Insights from the stabilization of plaques using darapladib-thrombolysis in myocardial infarction 52 (SOLID-TIMI 52) trial. J. Am. Heart Assoc. 2017, 6, e004332. [Google Scholar] [CrossRef] [PubMed]
- Khan, E.; Brieger, D.; Amerena, J.; Atherton, J.J.; Chew, D.P.; Farshid, A.; Ilton, M.; Juergens, C.P.; Kangaharan, N.; Rajaratnam, R.; et al. Differences in management and outcomes for men and women with ST-elevation myocardial infarction. Med. J. Aust. 2018, 209, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Cirillo, P.; Di Serafino, L.; Patti, G.; Antonucci, E.; Calabrò, P.; Gresele, P.; Palareti, G.; Pengo, V.; Pignatelli, P.; Marcucci, R. Gender-related differences in antiplatelet therapy and impact on 1-Year clinical outcome in patients presenting with ACS: The START ANTIPLATELET Registry. Angiology 2019, 70, 257–263. [Google Scholar] [CrossRef]
- Redfors, B.; Angerås, O.; Råmunddal, T.; Petursson, P.; Haraldsson, I.; Dworeck, C.; Odenstedt, J.; Ioaness, D.; Ravn-Fischer, A.; Wellin, P.; et al. Trends in gender differences in cardiac care and outcome after acute myocardial infarction in western Sweden: A report from the Swedish Web System for Enhancement of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies (SWEDEH. J. Am. Heart Assoc. 2015, 4, e001995. [Google Scholar] [CrossRef] [PubMed]
- Bruggmann, C.; Iglesias, J.F.; Gex-Fabry, M.; Fesselet, R.; Vogt, P.; Sadeghipour, F.; Voirol, P. Long-term quality of prescription for ST-segment elevation myocardial infarction (STEMI) patients: A real world 1-year follow-up study. Am. J. Cardiovasc. Drugs 2020, 20, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Hyun, K.; Negrone, A.; Redfern, J.; Atkins, E.; Chow, C.; Kilian, J.; Rajaratnam, R.; Brieger, D. Gender difference in secondary prevention of cardiovascular disease and outcomes following the survival of acute coronary syndrome. Heart Lung Circ. 2021, 30, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, M.O.; Rashid, M.; Timmis, A.; Clarke, S.; Lawson, C.; Michos, E.D.; Kwok, C.S.; De Belder, M.; Valgimigli, M.; Mamas, M.A. Sex differences in distribution, management and outcomes of combined ischemic-bleeding risk following acute coronary syndrome. Int. J. Cardiol. 2021, 329, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Smolina, K.; Ball, L.; Humphries, K.H.; Khan, N.; Morgan, S.G. Sex disparities in post-acute myocardial infarction pharmacologic treatment initiation and adherence: Problem for young women. Circ. Cardiovasc. Qual. Outcomes 2015, 8, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Colivicchi, F.; Tubaro, M.; Santini, M. Clinical implications of switching from intensive to moderate statin therapy after acute coronary syndromes. Int. J. Cardiol. 2011, 152, 56–60. [Google Scholar] [CrossRef]
- Ruiz-Pizarro, V.; Ferrera, C.; Gómez-Polo, J.C.; Palacios-Rubio, J.; Rico-García Amado, C.; Fernández-Ortiz, A.; Viana-Tejedor, A. Sex differences in treatment and prognosis of acute coronary syndrome with interventional management. Cardiovasc. Revasc. Med. 2019, 20, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Kitazono, T.; Kozuma, K.; Sekine, T.; Nakamura, S.; Shiosakai, K.; Iizuka, T. Prasugrel for Japanese patients with ischemic heart disease in long-term clinical practice (PRASFIT-PRACTICE II). Circ. J. 2020, 84, 101–108. [Google Scholar] [CrossRef]
- Virani, S.S.; Woodard, L.D.; Ramsey, D.J.; Urech, T.H.; Akeroyd, J.M.; Shah, T.; Deswal, A.; Bozkurt, B.; Ballantyne, C.M.; Petersen, L.A. Gender disparities in evidence-based statin therapy in patients with cardiovascular disease. Am. J. Cardiol. 2015, 115, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Koskinas, K.C.; Zanchin, T.; Klingenberg, R.; Gencer, B.; Temperli, F.; Baumbach, A.; Roffi, M.; Moschovitis, A.; Muller, O.; Tüller, D.; et al. Incidence, predictors, and clinical impact of early prasugrel cessation in patients with ST-elevation myocardial infarction. J. Am. Heart Assoc. 2018, 7, e008085. [Google Scholar] [CrossRef] [PubMed]
- Hansen, K.W.; Hvelplund, A.; Abildstrøm, S.Z.; Prescott, E.; Madsen, M.; Madsen, J.K.; Jensen, J.S.; Thuesen, L.; Thayssen, P.; Tilsted, H.H.; et al. No gender differences in prognosis and preventive treatment in patients with AMI without significant stenoses. Eur. J. Prev. Cardiol. 2012, 19, 746–754. [Google Scholar] [CrossRef] [PubMed]
- Bahall, M.; Seemungal, T.; Khan, K.; Legall, G. Medical care of acute myocardial infarction patients in a resource limiting country, Trinidad: A cross-sectional retrospective study. BMC Health Serv. Res. 2019, 19, 501. [Google Scholar] [CrossRef]
- Galway, S.; Adatia, F.; Grubisic, M.; Lee, M.; Daniele, P.; Humphries, K.H.; Sedlak, T.L. Sex differences in cardiac medication use post-catheterization in patients undergoing coronary angiography for stable angina with nonobstructive coronary artery disease. J. Women’s Health 2017, 26, 976–983. [Google Scholar] [CrossRef]
- Schiele, F.; Meneveau, N.; Seronde, M.F.; Descotes-Genon, V.; Chopard, R.; Janin, S.; Briand, F.; Guignier, A.; Ecarnot, F.; Bassand, J.P. Propensity score-matched analysis of effects of clinical characteristics and treatment on gender difference in outcomes after acute myocardial infarction. Am. J. Cardiol. 2011, 108, 789–798. [Google Scholar] [CrossRef] [PubMed]
- Vynckier, P.; Ferrannini, G.; Rydén, L.; Tokgözoğlu, L.; Bruthans, J.; Kotseva, K.; Wood, D.; De Backer, T.; Gevaert, S.; De Bacquer, D.; et al. Medical treatment in coronary patients: Is there still a gender gap? Results from European Society of Cardiology EUROASPIRE V Registry. Cardiovasc. Drugs Ther. 2021, 35, 801–808. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.F.; Shen, L.J.; Hsiao, F.Y.; Gau, C.S.; Wu, F.L.L. Sex differences in the treatment and outcome of patients with acute coronary syndrome after percutaneous coronary intervention: A population-based study. J. Women’s Health 2014, 23, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Al-Aqeedi, R.F.; Al Suwaidi, J.; Singh, R.; Al Binali, H.A. Does prior coronary artery bypass surgery alter the gender gap in patients presenting with acute coronary syndrome? A 20-year retrospective cohort study. BMJ Open 2012, 2, e001969. [Google Scholar] [CrossRef]
- Freund, K.M.; Jacobs, A.K.; Pechacek, J.A.; White, H.F.; Ash, A.S. Disparities by race, ethnicity, and sex in treating acute coronary syndromes. J. Women’s Health 2012, 21, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Johnston, N.; Bornefalk-Hermansson, A.; Schenck-Gustafsson, K.; Held, C.; Goodman, S.G.; Yan, A.T.; Bierman, A.S. Do clinical factors explain persistent sex disparities in the use of acute reperfusion therapy in STEMI in Sweden and Canada? Eur. Heart J. Acute Cardiovasc. Care 2013, 2, 350–358. [Google Scholar] [CrossRef] [PubMed]
- Gnavi, R.; Rusciani, R.; Dalmasso, M.; Giammaria, M.; Anselmino, M.; Roggeri, D.P.; Roggeri, A. Gender, socioeconomic position, revascularization procedures and mortality in patients presenting with STEMI and NSTEMI in the era of primary PCI. Differences or inequities? Int. J. Cardiol. 2014, 176, 724–730. [Google Scholar] [CrossRef] [PubMed]
- Trninic, D.; Dilic, M.; Vasiljevic, Z.; Kulic, M.; Srdić, S.; Dobrijević, N.; Sabanovic-Bajramovic, N.; Begic, A.; Kukavica, N.; Vukcevic, V.; et al. Clinical profile of patients with no-reperfusion therapy in Bosnia and Herzegovina and Serbia. Eur. Heart J. Suppl. 2014, 16, A67–A73. [Google Scholar] [CrossRef]
- Kuhn, L.; Page, K.; Rahman, M.A.; Worrall-Carter, L. Gender difference in treatment and mortality of patients with ST-segment elevation myocardial infarction admitted to Victorian public hospitals: A retrospective database study. Aust. Crit. Care 2015, 28, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Wolff, R.; Fefer, P.; Knudtson, M.L.; Cheema, A.N.; Galbraith, P.D.; Sparkes, J.D.; Wright, G.A.; Wijeysundera, H.C.; Strauss, B.H. Gender differences in the prevalence and treatment of coronary chronic total occlusions. Catheter. Cardiovasc. Interv. 2016, 87, 1063–1071. [Google Scholar] [CrossRef]
- Berlin, C.; Jüni, P.; Endrich, O.; Zwahlen, M. Revascularization treatment of emergency patients with acute ST-segment elevation myocardial infarction in Switzerland: Results from a nationwide, cross-sectional study in Switzerland for 2010–2011. PLoS ONE 2016, 11, e0153326. [Google Scholar] [CrossRef]
- Cenko, E.; Ricci, B.; Kedev, S.; Vasiljevic, Z.; Dorobantu, M.; Gustiene, O.; Knežević, B.; Miličić, D.; Dilic, M.; Trninic, D.; et al. Reperfusion therapy for ST-elevation acute myocardial infarction in Eastern Europe: The ISACS-TC registry. Eur. Heart J. Qual. Care Clin. Outcomes 2016, 2, 45–51. [Google Scholar] [CrossRef]
- Russ, M.A.; Wackerl, C.; Zeymer, U.; Hochadel, M.; Kerber, S.; Zahn, R.; Zrenner, B.; Topp, H.; Schächinger, V.; Weber, M.A. Gender based differences in drug eluting stent implantation—Data from the German ALKK registry suggest underuse of DES in elderly women. BMC Cardiovasc. Disord. 2017, 17, 68. [Google Scholar] [CrossRef] [PubMed]
- Araújo, C.; Pereira, M.; Laszczyńska, O.; Dias, P.; Azevedo, A. Sex-related inequalities in management of patients with acute coronary syndrome—Results from the EURHOBOP study. Int. J. Clin. Pract. 2018, 72, e13049. [Google Scholar] [CrossRef]
- Casey, S.D.; Mumma, B.E. Sex, race, and insurance status differences in hospital treatment and outcomes following out-of-hospital cardiac arrest. Resuscitation 2018, 126, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Kytö, V.; Prami, T.; Khanfir, H.; Hasvold, P.; Reissell, E.; Airaksinen, J. Usage of PCI and long-term cardiovascular risk in post-myocardial infarction patients: A nationwide registry cohort study from Finland. BMC Cardiovasc. Disord. 2019, 19, 123. [Google Scholar] [CrossRef]
- Jackson, A.M.; Zhang, R.; Findlay, I.; Robertson, K.; Lindsay, M.; Morris, T.; Forbes, B.; Papworth, R.; Mcconnachie, A.; Mangion, K.; et al. Healthcare disparities for women hospitalized with myocardial infarction and angina. Eur. Heart J. Qual. Care Clin. Outcomes 2020, 6, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Shehab, A.; Bhagavathula, A.S.; Alhabib, K.F.; Ullah, A.; Al Suwaidi, J.; Almahmeed, W.; AlFaleh, H.; Zubaid, M. Age-related sex differences in clinical presentation, management, and outcomes in ST-segment–elevation myocardial infarction: Pooled analysis of 15 532 patients from 7 Arabian Gulf registries. J. Am. Heart Assoc. 2020, 9, e013880. [Google Scholar] [CrossRef] [PubMed]
- Sulaiman, S.; Kawsara, A.; Mohamed, M.O.; Van Spall, H.G.C.; Sutton, N.; Holmes, D.R.; Mamas, M.A.; Alkhouli, M. Treatment effect of percutaneous coronary intervention in men versus women with st-segment–elevation myocardial infarction. J. Am. Heart Assoc. 2021, 10, e021638. [Google Scholar] [CrossRef] [PubMed]
- Tran, V.H.; Mehawej, J.; Abboud, D.M.; Tisminetzky, M.; Hariri, E.; Filippaios, A.; Gore, J.M.; Yarzebski, J.; Goldberg, J.H.; Lessard, D.; et al. Age and Sex Differences and Temporal Trends in the Use of Invasive and Noninvasive Procedures in Patients with acute myocardial infarction. J. Am. Heart Assoc. 2022, 11, e025605. [Google Scholar] [CrossRef] [PubMed]
- Dafaalla, M.; Rashid, M.; Van Spall, H.G.C.; Mehta, L.; Parwani, P.; Sharma, G.; Palmer, R.B.; Moledina, S.; Volgman, A.S.; Mamas, M.A. Women are less likely to survive AMI presenting with out-of-hospital cardiac arrest: A nationwide study. Mayo Clin. Proc. 2022, 97, 1608–1618. [Google Scholar] [CrossRef]
- Ashraf, M.; Jan, M.F.; Bajwa, T.K.; Carnahan, R.; Zlochiver, V.; Allaqaband, S.Q. Sex disparities in diagnostic evaluation and revascularization in patients with acute myocardial infarction—A 15-year nationwide study. J. Am. Heart Assoc. 2023, 12, e027716. [Google Scholar] [CrossRef] [PubMed]
- Baber, U.; Giustino, G.; Wang, T.; Grines, C.; McCoy, L.A.; Saha-Chaudhuri, P.; Best, P.; Skelding, K.A.; Ortega, R.; Chieffo, A.; et al. Comparisons of the uptake and in-hospital outcomes associated with second-generation drug-eluting stents between men and women: Results from the CathPCI Registry. Coron. Artery Dis. 2016, 27, 442–448. [Google Scholar] [CrossRef] [PubMed]
- Dreyer, R.P.; Beltrame, J.F.; Tavella, R.; Air, T.; Hoffmann, B.; Pati, P.K.; Di Fiore, D.; Arstall, M.; Zeitz, C. Evaluation of gender differences in door-to-balloon time in st-elevation myocardial infarction. Heart Lung Circ. 2013, 22, 861–869. [Google Scholar] [CrossRef] [PubMed]
- Venetsanos, D.; Sederholm Lawesson, S.; Alfredsson, J.; Janzon, M.; Cequier, A.; Chettibi, M.; Goodman, S.G.; Van’t Hof, A.W.; Montalescot, G.; Swahn, E. Association between gender and short-term outcome in patients with ST elevation myocardial infraction participating in the international, prospective, randomised Administration of Ticagrelor in the catheterisation Laboratory or in the Ambulance for New ST. BMJ Open 2017, 7, e015241. [Google Scholar] [CrossRef] [PubMed]
- Calé, R.; Pereira, H.; Pereira, E.; Vitorino, S.; de Mello, S. Time to reperfusion in high-risk patients with myocardial infarction undergoing primary percutaneous coronary intervention. Rev. Port. Cardiol. 2019, 38, 637–646. [Google Scholar] [CrossRef] [PubMed]
- Savage, M.L.; Hay, K.; Murdoch, D.J.; Walters, D.L.; Denman, R.; Ranasinghe, I.; Raffel, C. Sex differences in time to primary percutaneous coronary intervention and outcomes in patients presenting with ST-segment elevation myocardial infarction. Catheter. Cardiovasc. Interv. 2022, 100, 520–529. [Google Scholar] [CrossRef] [PubMed]
- Pandey, A.; McGuire, D.K.; De Lemos, J.A.; Das, S.R.; Berry, J.D.; Brilakis, E.S.; Banerjee, S.; Marso, S.P.; Barsness, G.W.; Simon, D.J.N.; et al. Revascularization trends in patients with diabetes mellitus and multivessel coronary artery disease presenting with non-ST elevation myocardial infarction. Circ. Cardiovasc. Qual. Outcomes 2016, 9, 197–205. [Google Scholar] [CrossRef]
- Bhasin, V.; Hiltner, E.; Singh, A.; Elsaid, O.; Awasthi, A.; Kassotis, J.; Sethi, A. Disparities in drug-eluting stent utilization in patients with acute ST-elevation myocardial infarction: An analysis of the National Inpatient Sample. Angiology 2023, 74, 774–782. [Google Scholar] [CrossRef] [PubMed]
- Meyer, M.R.; Bernheim, A.M.; Kurz, D.J.; O’Sullivan, C.J.; Tüller, D.; Zbinden, R.; Rosemann, T.; Eberli, F.R. Gender differences in patient and system delay for primary percutaneous coronary intervention: Current trends in a Swiss ST-segment elevation myocardial infarction population. Eur. Heart J. Acute Cardiovasc. Care 2019, 8, 283–290. [Google Scholar] [CrossRef]
- Aragam, K.G.; Moscucci, M.; Smith, D.E.; Riba, A.L.; Zainea, M.; Chambers, J.L.; Share, D.; Gurm, H.S. Trends and disparities in referral to cardiac rehabilitation after percutaneous coronary intervention. Am. Heart J. 2011, 161, 544–551. [Google Scholar] [CrossRef]
- Brouwers, R.W.M.; Houben, V.J.G.; Kraal, J.J.; Spee, R.F.; Kemps, H.M.C. Predictors of cardiac rehabilitation referral, enrolment and completion after acute myocardial infarction: An exploratory study. Neth. Heart J. 2021, 29, 151–157. [Google Scholar] [CrossRef]
- Martin, B.J.; Hauer, T.; Arena, R.; Austford, L.D.; Galbraith, P.D.; Lewin, A.M.; Knudtson, M.L.; Ghali, W.A.; Stone, J.A.; Aggarwal, S.G. Cardiac rehabilitation attendance and outcomes in coronary artery disease patients. Circulation 2012, 126, 677–687. [Google Scholar] [CrossRef]
- Parashar, S.; Spertus, J.A.; Tang, F.; Bishop, K.L.; Vaccarino, V.; Jackson, C.F.; Boyden, T.F.; Sperling, L. Predictors of early and late enrollment in cardiac rehabilitation, among those referred, after acute myocardial infarction. Circulation 2012, 126, 1587–1595. [Google Scholar] [CrossRef]
- Borg, S.; Öberg, B.; Leosdottir, M.; Lindolm, D.; Nilsson, L.; Bäck, M. Factors associated with non-attendance at exercise-based cardiac rehabilitation. BMC Sports Sci. Med. Rehabil. 2019, 11, 13. [Google Scholar] [CrossRef]
- Dunlay, S.M.; Pack, Q.R.; Thomas, R.J.; Killian, J.M.; Roger, V.L. Participation in cardiac rehabilitation, readmissions and death after acute myocardial infarction. Am. J. Med. 2014, 127, 538–546. [Google Scholar] [CrossRef]
- Prabhakaran, D.; Chandrasekaran, A.M.; Singh, K.; Mohan, B.; Chattopadhyay, K.; Chadha, D.S.; Negi, P.C.; Bhat, P.; Sadananda, K.S.; Ajay, V.S.; et al. Yoga-based cardiac rehabilitation after acute myocardial infarction: A randomized trial. J. Am. Coll. Cardiol. 2020, 75, 1551–1561. [Google Scholar] [CrossRef] [PubMed]
- Bugiardini, R.; Ricci, B.; Cenko, E.; Vasiljevic, Z.; Kedev, S.; Davidovic, G.; Zdravkovic, M.; Miličić, D.; Dilic, M.; Manfrini, O.; et al. Delayed care and mortality among women and men with myocardial infarction. J. Am. Heart Assoc. 2017, 6, e005968. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.Y.; Nallamothu, B.K.; Krumholz, H.M.; Li, S.; Roe, M.T.; Jollis, J.G.; Jacobs, A.K.; Holmes, D.R.; Peterson, E.D.; Ting, H.H. Association of door-in to door-out time with reperfusion delays and outcomes among patients transferred for primary percutaneous coronary intervention. JAMA J. Am. Med. Assoc. 2011, 305, 2540–2547. [Google Scholar] [CrossRef] [PubMed]
- Sambola, A.; Elola, F.J.; Buera, I.; Fernández, C.; Bernal, J.L.; Ariza, A.; Brindis, R.; Bueno, H.; Rodríguez-Padial, L.; Marín, F.; et al. Sex bias in admission to tertiary-care centres for acute myocardial infarction and cardiogenic shock. Eur. J. Clin. Investig. 2021, 51, e13526. [Google Scholar] [CrossRef]
- Hilleary, R.S.; Jabusch, S.M.; Zheng, B.; Jiroutek, M.R.; Carter, C.A. Gender disparities in patient education provided during patient visits with a diagnosis of coronary heart disease. Women’s Health 2019, 15, 1–9. [Google Scholar] [CrossRef]
- Kuhn, L.; Page, K.; Rolley, J.X.; Worrall-Carter, L. Effect of patient sex on triage for ischaemic heart disease and treatment onset times: A retrospective analysis of Australian emergency department data. Int. Emerg. Nurs. 2014, 22, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Ashfaq, F.; Noor, T.A.; Ashraf, S.; Sohail, H.; Malik, J.; Ashraf, A.; Ashraf, W. Social determinants of clinical visits after left main percutaneous coronary intervention versus coronary artery bypass grafting. Curr. Probl. Cardiol. 2023, 48, 101722. [Google Scholar] [CrossRef]
- Robijn, A.L.; Woodward, M.; Pearson, S.A.; Hsu, B.; Chow, C.K.; Filion, K.B.; Jorm, L.; Havard, A. Uptake of prescription smoking cessation pharmacotherapies after hospitalization for major cardiovascular disease. Eur. J. Prev. Cardiol. 2022, 29, 2173–2182. [Google Scholar] [CrossRef] [PubMed]
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.-A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur. Heart J. 2023, 44, 3720–3826. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Celutkiene, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Marx, N.; Federici, M.; Schütt, K.; Müller-Wieland, D.; Ajjan, R.A.; Antunes, M.J.; Christodorescu, R.M.; Crawford, C.; Di Angelantonio, E.; Eliasson, B.; et al. 2023 ESC Guidelines for the management of cardiovascular disease in patients with diabetes. Eur. Heart J. 2023, 44, 4043–4140. [Google Scholar] [CrossRef] [PubMed]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary. A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, e563–e595. [Google Scholar] [CrossRef] [PubMed]
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: Executive summary: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022, 1, e1–e19. [Google Scholar] [CrossRef] [PubMed]
- Mosca, L.; Benjamin, E.J.; Berra, K.; Bezanson, J.L.; Dolor, R.J.; Lloyd-Jones, D.M.; Newby, L.K.; Piña, I.L.; Roger, V.L.; Shaw, L.J.; et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women-2011 update: A guideline from the American Heart Association. Circulation 2011, 123, 1243–1262. [Google Scholar] [CrossRef]
- Zhao, M.; Woodward, M.; Vaartjes, I.; Millett, E.R.C.; Klipstein-Grobusch, K.; Hyun, K.; Carcel, C.; Peters, S.A.E. Sex differences in cardiovascular medication prescription in primary care: A systematic review and meta-analysis. J. Am. Heart Assoc. 2020, 9, e014742. [Google Scholar] [CrossRef]
- Welch, L.C.; Lutfey, K.E.; Gerstenberger, E.; Grace, M. Gendered uncertainty and variation in physicians’ decisions for coronary heart disease: The double-edged sword of “atypical symptoms”. J. Health Soc. Behav. 2012, 53, 313–328. [Google Scholar] [CrossRef]
- Lichtman, J.H.; Leifheit-Limson, E.C.; Safdar, B.; Bao, H.; Krumholz, H.M.; Lorenze, N.P.; Daneshvar, M.; Spertus, J.A.; D’Onofrio, G. Sex differences in the presentation and perception of symptoms among young patients with myocardial infarction: Evidence from the VIRGO study. Circulation 2018, 137, 781–790. [Google Scholar] [CrossRef] [PubMed]
- Lutfey, K.E.; Link, C.; Grant, R.W.; Marceau, M.P.; McKinlay, J.B. Is certainty more important than diagnosis for understanding race and gender disparities?: An experiment using coronary heart disease and depression case vignettes. Health Policy 2009, 89, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Maserejian, N.N.; Link, C.L.; Lutfey, K.L.; Marceau, L.D.; McKinlay, J.B. Disparities in physicians’ interpretations of heart disease symptoms by patient gender: Results of a video vignette factorial experiment. J. Women’s Health 2009, 18, 1661–1667. [Google Scholar] [CrossRef] [PubMed]
- Chan, P.S.; Oetgen, W.J.; Buchanan, D.; Mitchell, K.; Fiocchi, F.F.; Tang, F.; Jones, P.G.; Breeding, T.; Thrutchley, D.; Rumsfeld, J.S.; et al. Cardiac performance measure compliance in outpatients. The American College of Cardiology and National Cardiovascular Data Registry’s PINNACLE (Practice Innovation and Clinical Excellence) Program. J. Am. Coll. Cardiol. 2010, 56, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Beckstead, J.W.; Pezzo, M.V.; Beckie, T.M.; Shahraki, F.; Kentner, A.C.; Grace, S.L. Physicians’ tacit and stated policies for determining patient benefit and referral to cardiac rehabilitation. Med. Decis. Mak. 2014, 34, 63–74. [Google Scholar] [CrossRef]
- Tsui, K.Y.; Segaram, S.S.; Jamnik, V.; Wu, G.; Grace, S.L. Variation in patient perceptions of healthcare provider endorsement of cardiac rehabilitation courtney. J. Cardiopulm. Rehabil. Prev. 2012, 32, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Lichtman, J.H.; Leifheit-Limson, E.C.; Watanabe, E.; Allen, N.B.; Garavalia, B.; Garavalia, L.S.; Spertus, J.A.; Krumholz, H.M.; Curry, L.A. Symptom recognition and healthcare experiences of young women with acute myocardial infarction. Circ. Cardiovasc. Qual. Outcomes 2015, 8, S31–S38. [Google Scholar] [CrossRef]
- Chiaramonte, G.R.; Friend, R. Medical students’ and residents’ gender bias in the diagnosis, treatment, and interpretation of coronary heart disease symptoms. Health Psychol. 2006, 25, 255–266. [Google Scholar] [CrossRef]
- Biddle, C.; Fallavollita, J.A.; Homish, G.G.; Orom, H. Gender bias in clinical decision making emerges when patients with coronary heart disease symptoms also have psychological symptoms. Heart Lung 2019, 48, 331–338. [Google Scholar] [CrossRef]
- Gulati, M.; Levy, P.D.; Mukherjee, D.; Amsterdam, E.; Bhatt, D.L.; Birtcher, K.K.; Blankstein, R.; Boyd, J.; Bullock-Palmer, R.P.; Conejo, T.; et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2021, 78, e187–e285. [Google Scholar] [CrossRef] [PubMed]
- Regitz-Zagrosek, V.; Gebhard, C. Gender medicine: Effects of sex and gender on cardiovascular disease manifestation and outcomes. Nat. Rev. Cardiol. 2023, 20, 236–247. [Google Scholar] [CrossRef]
- Healy, B. The Yentl syndrome. N. Engl. J. Med. 1991, 325, 274–276. [Google Scholar] [CrossRef] [PubMed]
| Article | Conclusion | Justification |
|---|---|---|
| [13] | Male sex was associated with statin treatment. Patients not treated with statins were more likely to be female. | Reasons were undocumented. Possibilities are less medical insurance in females or less likely to have lipid level > 100 mg/dL (with this often being applied as a limit for prescribing statin therapy). |
| [14] | Fewer women were treated with thienopyridines, heparin, and glycoprotein IIb/IIIa inhibitors compared to men. Female gender was independently associated with a lower in-hospital use of coronary angiography. | The underestimation of patient risk was the most common reason for not pursuing an invasive strategy in both men and women. |
| [15] | After adjusting for covariates, males had higher odds of statin prescription in coronary heart disease patients. | Not documented. |
| [16] | Eligible women were less likely to receive evidence-based acute treatments, rehabilitation, and reperfusion treatments. | Women were presented to hospitals for STEMI treatment 1.4 h later than men. Though analysis was conducted on eligible patients with treatment indications and adjusted for clinical factors, women were older and had worse clinical profiles than men. Worse clinical profiles contribute to an increased risk of adverse outcomes which are associated with undertreatment, partly for fear of complications (e.g., higher risk of bleeding) and partly because of the lack of evidence from randomised clinical trials in these groups. |
| [17] | Long-term statin prescriptions were less common in women. | Female gender has been shown to be a risk factor for statin-induced myalgias, which could lead to early discontinuation. Intense media publicity of exaggerated side effects of statins may have a negative impact on the continuation of statins, with more profound effects on women. |
| [18] | Factors associated with filling high-intensity statin prescriptions included male sex. | This may reflect variation in the use of evidence-based therapies across hospitals and providers or the use of intensive medical management for select high-risk patients. |
| [19] | Male sex was associated with a greater likelihood of statin utilisation. | Not documented. |
| [20] | Females were less likely to receive PCI and CABG. | Stark differences in treatment between males and females reflected an excess risk of readmission and mortality following an MI in males. |
| [21] | Revascularisation treatment, prescriptions of platelet aggregation inhibitors, statins, and functional rehabilitation were more frequently provided to men than women. | Women were less likely to have multiple injuries than men, which might explain (at least in part) sex differences in reperfusion therapy. Studies have suggested that a higher haemorrhagic risk and the presence of relative contraindications could explain the difference in the prescription of platelet aggregation inhibitors. The lack of the universality of the health system and of a clearly specified care pathway for ACS is a baseless argument for gender differences based on what is found here. |
| [22] | Among patients without contraindications, women were less likely to receive treatments than men. In particular, we found that the use of invasive strategies (which included PC) was lower in women. | Women less often presented with chest discomfort than men. Lower eGFR levels in women than men may also partly explain sex differences. The reasons for women less often undergoing an invasive strategy may relate to the differences in baseline characteristics and physician recognition of NSTEMI in women. |
| [23] | Women were less likely than men to receive medications for secondary prevention. | There are frequent changes in national guidelines and fewer programmes that focus on implementation. |
| [24] | Characteristics associated with lower odds of statin therapy initiation included female sex. | This may be due to misperceptions of adverse effects of statins and uncertainty among both patients and prescribers about statin efficacy in women and older patients. |
| [25] | During hospital admission for an ACS, the proportion of women that used cardiovascular drugs was lower than that of men. | There were differences in the severity of the ACS and comorbidities and differences in the prescription attitude of physicians or differences in attitude to taking the drugs by patients. |
| [26] | The use of all five indicated drugs and PCI was higher in male patients compared to females. | Not documented. Generally, symptom patterns are more atypical in women, making it more difficult to diagnose cardiac pathology. Women are considered at a lower risk of acute MI, which makes physicians less aware of the risk of new cardiovascular events, causing lower medical adherence. Once acute MI has occurred, young women are at a high risk of complications. Also, trials have enrolled few women; however, benefits concerning safety and outcomes have been observed regardless of gender. |
| [27] | Male sex was related to the prescription of statins at discharge. | Not documented. |
| [28] | Women were less likely to either have initiated statin therapy or to have persistent statin therapy at the end of follow-up. | The older age at CAD onset in women may have contributed to the sex disparities in statin therapy. Women were less likely to be evaluated by a cardiologist, which may have contributed to sex disparity in statin use given that cardiologist evaluation contributed to statin use in general. Differences in reported adverse events to statin treatment was a significant contributor to the sex disparity in statin therapy. |
| [29] | Women were less likely to be prescribed statins and antiplatelet drugs. | It is impossible to judge from our data whether this difference is due to physicians taking a different attitude to prescribing statins for the two genders or to men and women responding differently to the offer of statin treatment. |
| [30] | Women were less likely to be discharged with aspirin and clopidogrel. | Women with an ACS diagnosis are more likely to be older than men and to have diabetes, hypertension, heart failure, or other comorbidities. |
| [31] | Proportionally fewer female patients underwent invasive procedures. | Findings show the possibility that health inequality in female patients with AMI arises from social inequality rather than biological differences such as age and severity. Females severely trail males in economic participation and opportunity, educational attainment, health and survival, and political empowerment. Furthermore, the cause of myocardial infarction in females is less well understood than in males. Also, most of the information and educational materials available to the public focus on AMI symptoms in males. |
| [32] | Factors associated in multivariable analysis with suboptimal statin occurrence included female sex. | Not documented. |
| [33] | Selected patient factors associated with the non-use of high-potency statins included female sex. | The study highlights the need to educate physicians and mentions reluctance to treating high-risk patients with a high-intensity regimen. |
| [34] | Women with STEMI were less likely to have undergone coronary angiography or revascularisation and have received timely revascularisation or primary PCI and less likely to receive some elements of secondary preventive treatment, including b-blockers and statins, and referral to cardiac rehabilitation. | Women presented with ACS later in life than men and had more comorbid conditions, especially diabetes and hypertension, but women with STEMI in every GRACE risk score quartile received less comprehensive. assessment and treatment. Undertreatment in the population examined might have been caused by poor awareness that women with STEMI are generally at a higher risk or by a preference for subjectively determining risk rather than applying more reliable, objective risk prediction tools. |
| [35] | PCI and DES were more often used in males. Males were more often treated with dual antiplatelet therapy. | Not documented. Generally, there is a perception of the risk of bleeding. |
| [36] | Women were less likely to be prescribed evidence-based treatment at discharge (b-blockers, angiotensin-converting enzyme inhibitors, or angiotensin receptor blockers, statins, and P2y12 antagonists). Also, women with STEMI were less likely than men to undergo coronary angiography and PCI. | There is systematic undertreatment. We cannot rule out that findings reflect a sexist bias. Effective measures within the healthcare system are needed to neutralise the undertreatment of women after MI. |
| [37] | Female sex was a predictor of the incomplete prescription of guideline medications at discharge. | The disparity between men and women occur mainly with the prescription of statins, with women receiving medium- or low-intensity statin therapy more often than men. Reasons for this are yet to be elucidated, with the hypothesis that there is a perceived risk for adverse outcomes after. ACS is lower in young women because of a traditional school of thought dictating that cardiovascular disease is primarily a male disease. |
| [38] | Women had lower odds of attending cardiac rehabilitation and using secondary prevention medications. | There was a combination of financial, social, and psychological reasons. Lower socioeconomic status in women may have led to difficulties in adhering to secondary prevention care due to the out-of-pocket cost. |
| [39] | In the dual-high risk group, females were less likely to receive guideline-recommended therapy. | Traditionally, lower rates of invasive management in females have been attributed to differences in baseline risk for further bleeding and ischemia compared to males. This is likely due to physicians’ preference for a conservative management strategy in this group to avoid commitment to long-term DAPT in the case of PCI, although there is emerging evidence to support short-term DAPT in high-bleeding-risk patients, regardless of the complexity of their PCI procedure. However, these concerns do not justify differences in [the receipt of guideline-recommended therapy between sexes of the same combined risk group. Guidelines do not provide recommendations on how patients at a high risk of both ischemic and major bleeding complications should be managed. |
| [40] | Younger men were significantly more likely than younger women to initiate appropriate treatment. There was no significant sex difference in adherence to medication therapy. | Cardiovascular disease among younger women has only recently received research attention. Perceptions of risk for adverse outcomes in physicians and patients is still skewed for younger women, who are seen as healthy and at low risk. |
| [41] | Female gender was associated with a higher probability of a switch to a less effective statin. | In all cases, the decision to switch to a less intensive lipid-lowering intervention was taken by primary care physicians, either following the occurrence of side effects or for safety concerns. |
| [42] | A lower proportion of women received high-potency antiplatelet agents. | There were greater hemorrhagic risk scores among women. Several relative contraindications to high-potency antiplatelet drugs, such as advanced age, hypertension, and small body size, were more common among women. |
| [43] | Female sex predicted the discontinuation of DAPT. | The duration of DAPT may have been shortened during the early treatment phase because of concerns regarding the risk of bleeding. |
| [44] | In adjusted models, female gender was independently associated with a lower likelihood of receiving statins or high-intensity statins. | Our results do not explain why clinicians are less likely to use statins or high-intensity statins in female patients with CVD. This could reflect providers’ perception of a lower risk of recurrent CVD events in female patients with CVD despite results showing that women have a higher overall illness burden. The lower use of statins and high-intensity statins in female patients with CVD may also represent healthcare providers’ perception of a lower benefit from statins in females. Findings also fail to explain whether patient preferences or differences in the side effects of high-intensity statins explain sex differences. However, it is known that the side effects of these druges do not differ according to sex. |
| [45] | Independent predictors of any prasugrel cessation included female sex. | Female sex previously emerged as an independent predictor of bleeding in prasugrel-treated patients. The leading cause of prasugrel disruption (in all patients) was cessation because of unjustified patient decision. |
| [46] | After adjustment, lipid-lowering drugs, beta blockers, clopidogrel, and aspirin were all redeemed equally. | |
| [47] | There was no difference in pharmaceutical use but more men were treated with thrombolysis. | It may be because of the earlier recognition of MI and less distractions to reaching hospitals. |
| [48] | No important sex differences. | Results may indicate increased awareness that women have adverse outcomes similar to and, in some cases, worse than men and also the recognition that females have higher rates of hypertension and/or microvascular disease or coronary vasospasm underlying their stable angina. |
| [49] | Compared to men, women were 10 years older, had more comorbidities, less often underwent angiography and reperfusion, and received less medical treatment. | The less frequent use of invasive procedures in women was not only related to age and baseline characteristics but also reflected systematic undertreatment. |
| [50] | Women were less likely to receive statins. Overall, no gender differences were found in the total daily dose intake. Women were less likely to undergo revascularisation. | A possible explanation could be that women were less likely to adhere to statins because of more side effects. However, no gender differences were observed in self-reported medication adherence, statin intolerance, or patient refusal to take statins. It is possible that women did not require a revascularisation procedure because of the presentation and severity of the underlying disease. |
| [51] | Some drugs were favoured in men and others were favoured in women. | Findings do not imply ‘inequality’, which may be due to the fact that existing guidelines are based on trials with a higher percentage of men. Women may be more vulnerable to the adverse effects of drug therapy, and disease-specific guidelines do not take into account sex differences in ACS patients. |
| [52] | Women were less likely to receive reperfusion and early invasive therapies. | Women with or without prior CABG were older and had a higher risk profile than men. Women with prior CABG need to be more represented in studies. |
| [53] | After controlling for demographics and comorbidities, ethnic minorities and women had lower rates of revascularisation compared to white men. | Sex bias in use of aggressive treatment may play a role. |
| [54] | Reperfusion therapy was used less often in women. | In older women, there was disparate use often explained by adjusting for age and associated comorbidities in women; however, even after controlling for these factors, sex disparities persisted, which may suggest a biassed management of older women. In younger women, disparities were more difficult to explain, the most explanatory factor was the recognition of atypical symptoms. |
| [55] | After adjustment for age, comorbidity, and hospital characteristics, women had a lower probability of undergoing revascularisation procedures. | Women may present with “atypical” symptoms and physicians’ recommendations for cardiac catheterisation may also differ. Rather than lower access to effective treatment for women, we might be witnessing the overuse of revascularisation procedures in men. |
| [56] | Female sex was an independent variable associated with no-reperfusion therapy. | Not documented. |
| [57] | Both younger and older women received less frequent angioplasty with stents and more often received no reperfusion treatment than men in corresponding age groups. | There was an under-investigation of older women who were the largest group. A higher proportion of younger women in this study lived in rural areas than younger men and fewer older women were English-speaking compared to their older male cohort. |
| [58] | Rates of PCI in the CTO group were similar between genders; however, women with CTO were treated significantly less by CABG compared to men. Moreover, compared to male patients, significantly fewer women undergoing CABG had the revascularisation of the CTO artery. | Although female gender was an independent predictor of medical management, other adverse characteristics, including older age and higher comorbidities, were likely contributing factors. It is also possible that smaller distal vessels may be more common in women with CTOs. |
| [59] | Patients were less likely to receive revascularisation if they were female. | Not documented. |
| [60] | A factor associated with not attempting reperfusion therapy was female sex. | Recent data indicate that women are more likely to exceed in-hospital and pre-hospital time guidelines for p-PCI with consequent higher chance of missing the opportunity for reperfusion. |
| [61] | Although women had smaller vessel sizes, they received DES less often compared to men. | There was an intention to prevent bleeding complications in women by the use of BMS instead of DES. |
| [62] | In a real-life setting, women with STEMI/NC ACS were less likely than men to be managed invasively. | Not documented. Generally, factors related to healthcare systems (delay between symptom onset and seeking help) and patients (e.g., women’s own preferences) influence ability to perceive, seek, reach, pay for, and engage in healthcare and the ability of the system to fulfil patient needs. |
| [63] | Female sex was independently associated with lower rates of treatment at a 24/7 PCI centre and lower rates of cardiac catheterisation. | Given that their survival with good neurological outcomes is only slightly worse, interventional cardiologists may appropriately select women who are most likely to benefit from cardiac catheterisation. Female patients may manifest more atypical symptoms than men preceding OHCA, leading to the delayed recognition of cardiac aetiology and delayed transfer to a 24/7 PCI centre. |
| [64] | Female sex was an independent factor for not undergoing PCI. | Less serious cardiac events were probable in women. |
| [65] | Women were less likely to receive an indicated therapy prior to hospitalisation and to receive an invasive intervention upon arrival. Fewer women received angiography or PCI and an indicated therapy following MI. | Differences in admission route due to greater diagnostic uncertainty amongst women reduces the chance of revascularisation. Delays in time between symptom onset and first contact with medical services mean that the benefits of emergent coronary revascularisation are less certain. Emergency care decisions regarding coronary angiography and PCI in women may be influenced by smaller coronary anatomy, more technically challenging vascular access (the excess door-to-balloon time seen in older women in this study may reflect this), and a greater risk of procedure-related complications and post-procedural mortality. |
| [66] | Younger women with STEMI were more likely to seek acute medical care and less likely to receive thrombolytic therapies or primary PCI and guideline-recommended pharmacotherapy than men. | Less than 50% of women received an ECG within ten minutes, suggesting that sex differences exist in the diagnosis of STEMI, possibly due to the poor recognition of atypical symptoms. |
| [67] | Women were less likely to undergo angiography or PCI. | There was a notion that women suffer worse outcomes, though this was found to not be true. |
| [68] | A smaller proportion of women underwent cardiac catheterisation, percutaneous coronary intervention, and coronary artery bypass graft surgery. | A lack of typical chest pain and delays in seeking acute medical care among women may not result in indications for the receipt of coronary angiography or coronary reperfusion therapy, which are symptom- and time-dependent. This would explain why no sex differences were found in use of echocardiography or exercise stress testing, as these procedures do not depend on the presence of chest pain symptoms. |
| [69] | Women experienced longer call-to-hospital-arrival time and were less likely to receive DAPT, beta blockers, ACE inhibitors, coronary angiography, and PCI. After adjustment, women had significantly lower odds of receiving coronary angiography and CABG. | Not documented. Generally, unconscious bias among physicians and higher mortality rates in women act as competing risk factors. There is hesitancy to expose women to provide resuscitation. |
| [70] | There was sex disparity in diagnostic angiography, PCI, and CABG use favouring men. | There are sex-based biological differences. |
| [71] | Second-generation DES use was significantly less frequent among women. | Differences came from the first 1.5 years of the study when there was less awareness of benefits in women. |
| [72] | Upon hospital arrival, women experienced delays in door-to-code, code-to-balloon, and thus DTB time. After multivariate adjustment, independent determinants of DTB time included female gender. | Women tended to have less peak ST-elevation than men in this study and this may have contributed to delayed ECG interpretation. LTB time was significantly delayed in women, which may indicate that unrecognised technical factors contribute to delayed DTB time. These may include difficulty in establishing arterial access, the catheter engagement of the infarct-related artery, the passage of the guidewire/balloon through the coronary occlusion, or even balloon inflation itself. |
| [74] | Median system delay and revascularisation delay were longer in women. | Not documented. Generally, later diagnosis due to atypical symptoms or higher prevalence of acute coronary syndrome without obstructive coronary disease, suggesting negative discrimination by the healthcare system. |
| [75] | There were longer median times in females and females were less likely to receive FMC-to-ballon times of less than 90 mins. There were significantly longer total and direct STB, FMCTB, and DTB durations for females. There were significant differences in geometric mean times from symptom onset to FMC. | A greater proportion of females presented after 3 h from symptom onset. There was variability in symptoms between men and women, with women experiencing a wider variety and less common symptoms occurring more often. There were lower rates of initial successful radial arterial approaches in females. |
| [76] | Females were more likely to receive an inappropriate treatment. | Not documented. |
| [77] | Women were more likely to undergo DES implantation. | Not documented. |
| [78] | System delay was unaffected by sex in the multivariate model. | |
| [79] | Male gender was associated with significant increased referral to rehabilitation in all hospitals. | Differences were concentrated in the lowest-referring hospitals with the lowest-referring hospitals serving proportionally more female and minority patients than the highest-referring hospitals. |
| [80] | Non-referral was independently associated with female sex. | Limited capacity at CR facilities or a lack of reimbursement for specific subgroups may also lead to lower referral rates. Also, studies have suggested that some physicians believe that women benefit less from CR. |
| [81] | Subjects who completed CR were more likely to be male. | Socioeconomic status and lower levels of education have been associated with poor attendance. |
| [82] | Females were less likely to participate in cardiac rehabilitation at 1 month. | Studies have suggested that women are more likely to have barriers related to transportation, family responsibilities, comorbidities, and perceiving exercise as tiring. |
| [83] | Male sex was a predictor of non-attendance. | Sweden is one of the world’s most gender-equal countries regarding typical barriers to women (family obligations, caretaking responsibilities, and multiple role conflicts). |
| [84] | Participation in rehab decreased in men but not in women over the study period. | Not documented. |
| [85] | There was no difference in attendance at Yoga-CaRe sessions by sex. | |
| [86] | Despite similar delays in seeking care, the overall time from symptom onset to hospital presentation was longer for women than men. | Differential treatment and triage strategies used by first responders and transfer procedures between hospitals. Longer delays on the part of the health system than on the part of patients, most likely a delay in diagnosis by the provider. |
| [87] | Significant factors associated with a DIDO time greater than 30 min included female sex. | The study states that the magnitude of this contribution of sex was small and did not discuss it further. |
| [88] | Women were less often admitted to revascularisation-capable hospitals than men. | Age played an important role in admission to a revascularisation capable hospital or ICCU centre. |
| [89] | Females had 0.86 times the odds of receiving patient education compared to males. | This may have been partially attributable to clinicians following the USPSTF guidelines for lipid screening that were less aggressive for females. |
| [90] | Proportionately more men were triaged correctly for AMI than women. Across all triage categories, average treatment time was faster for men than women. When incorrectly triaged, treatment time for men was faster than for women. | A correct triage score was vital for treatment time and more women were incorrectly triaged. |
| [91] | Female gender was a strong predictor of having a follow-up visit. | Not discussed regarding sex. Structural barriers to healthcare access were discussed generally. |
| [92] | Females were more likely than males to be dispensed a prescription smoking cessation programme (SCP). | Sex difference did not persist after adjustment for mood disorders and prior use of prescription SCP. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Knox, E.C.L.; Mateo-Rodríguez, I.; Daponte-Codina, A.; Rosell-Ortiz, F.; Solá-Muñoz, S.; Codina-Rodríguez, A.; Bueno, H.; Ruiz-Azpiazu, J.I. Gender Differences in Clinical Practice Regarding Coronary Heart Disease: A Systematic Review. J. Clin. Med. 2025, 14, 1583. https://doi.org/10.3390/jcm14051583
Knox ECL, Mateo-Rodríguez I, Daponte-Codina A, Rosell-Ortiz F, Solá-Muñoz S, Codina-Rodríguez A, Bueno H, Ruiz-Azpiazu JI. Gender Differences in Clinical Practice Regarding Coronary Heart Disease: A Systematic Review. Journal of Clinical Medicine. 2025; 14(5):1583. https://doi.org/10.3390/jcm14051583
Chicago/Turabian StyleKnox, Emily Caitlin Lily, Inmaculada Mateo-Rodríguez, Antonio Daponte-Codina, Fernando Rosell-Ortiz, Silvia Solá-Muñoz, Antía Codina-Rodríguez, Héctor Bueno, and José Ignacio Ruiz-Azpiazu. 2025. "Gender Differences in Clinical Practice Regarding Coronary Heart Disease: A Systematic Review" Journal of Clinical Medicine 14, no. 5: 1583. https://doi.org/10.3390/jcm14051583
APA StyleKnox, E. C. L., Mateo-Rodríguez, I., Daponte-Codina, A., Rosell-Ortiz, F., Solá-Muñoz, S., Codina-Rodríguez, A., Bueno, H., & Ruiz-Azpiazu, J. I. (2025). Gender Differences in Clinical Practice Regarding Coronary Heart Disease: A Systematic Review. Journal of Clinical Medicine, 14(5), 1583. https://doi.org/10.3390/jcm14051583








