Myopia Management in Hong Kong
Abstract
1. Introduction
2. Methods
- The patient was aged 6–10 inclusively.
- The patient had at least one appointment in any year from 2017 to 2021 inclusively.
- The patient saw the same primary clinician for the majority of their appointments.
- One group is pre-myopes, and they have a refractive error ≤ +0.75D in each principal meridian; the other group is myopes and they have a refractive error of ≤−0.50D in each principal meridian.
- The patient had no significant binocular vision issues.
- The patient had correctable acuity to at least 20/30 in each eye.
- The patient had no development impairment or special needs.
- The patient had no ocular or systemic disease.
3. Data Analysis
4. Results
4.1. Demographic Characteristic Data
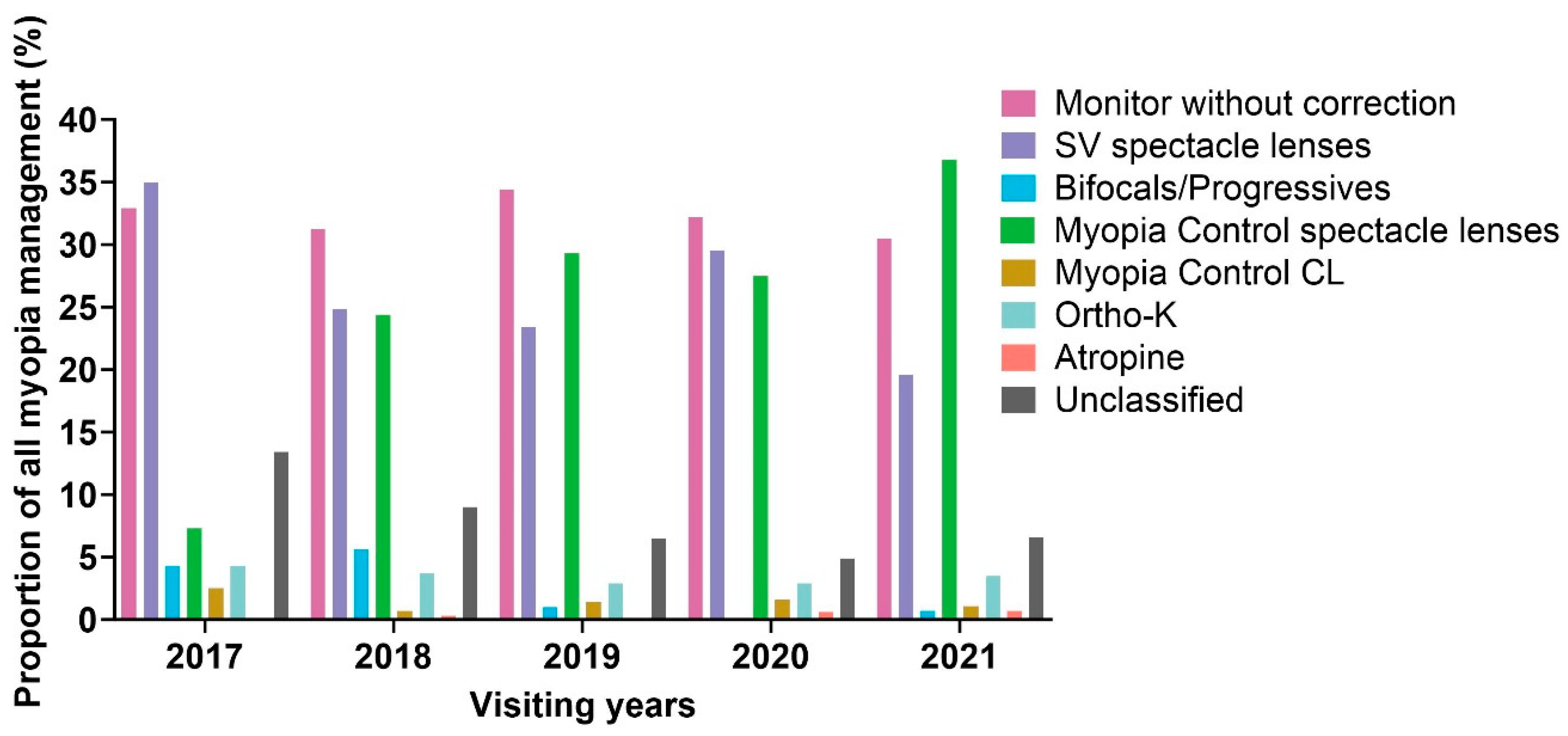
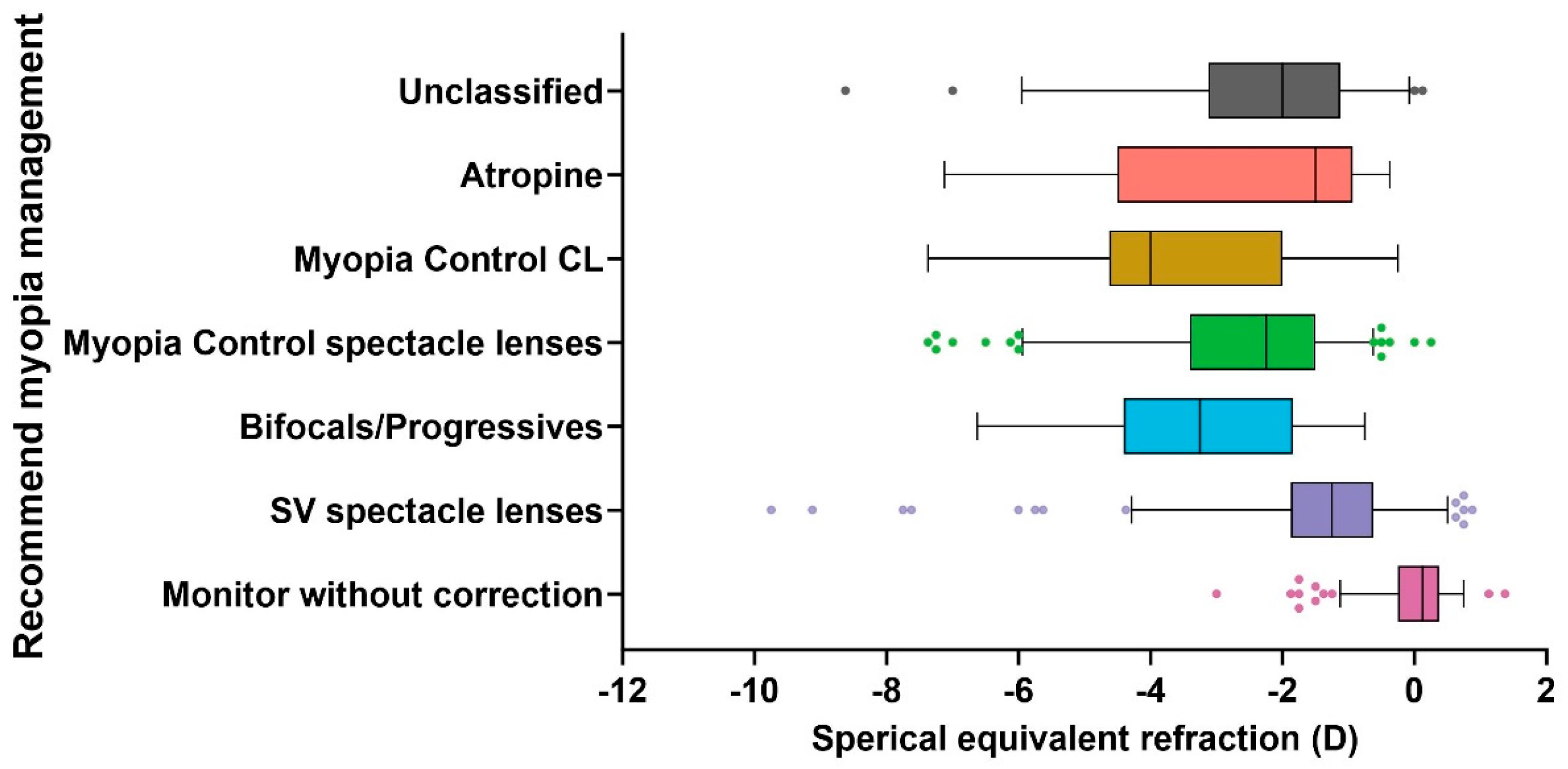
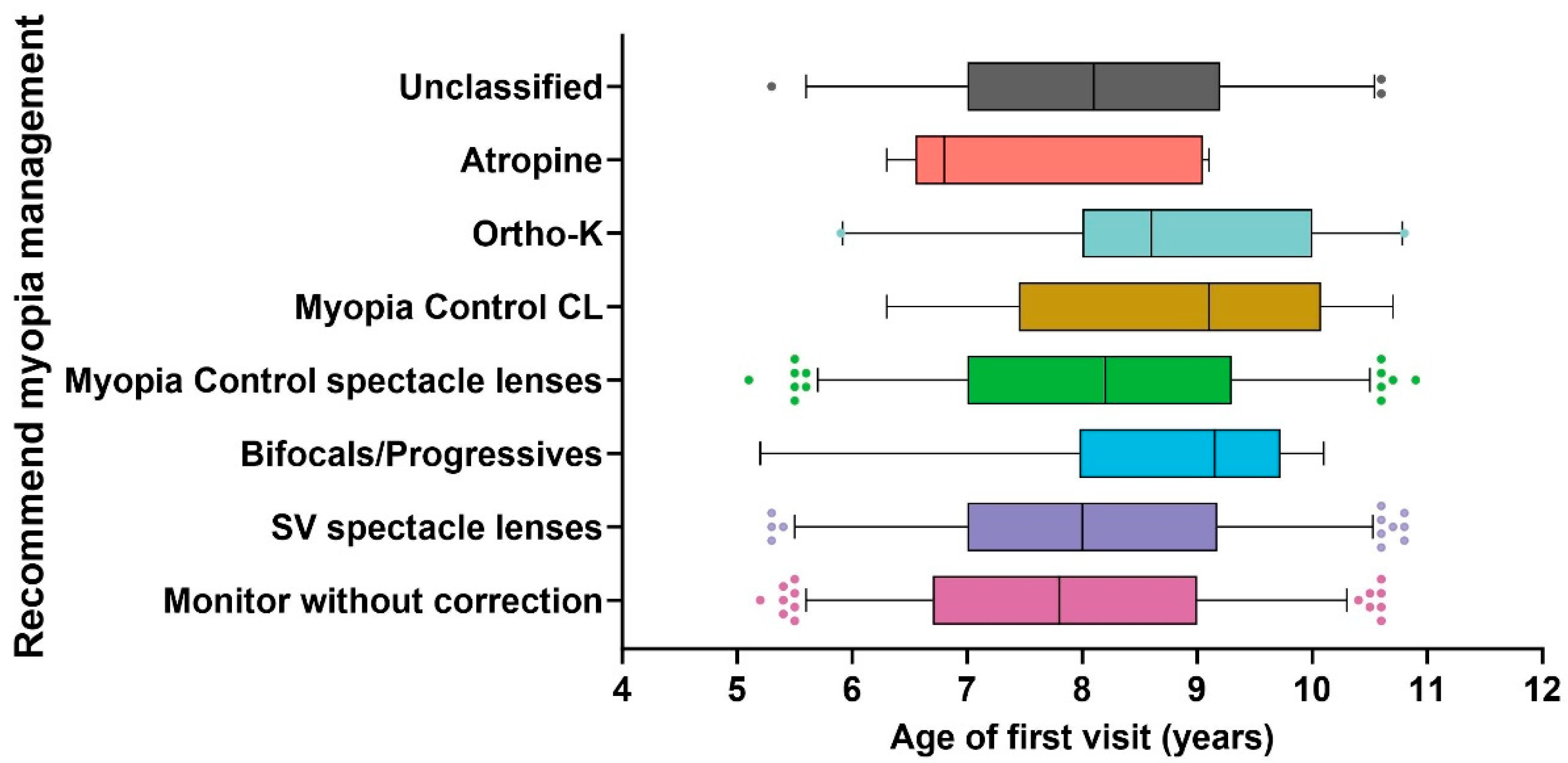
4.2. Recommended Myopia Management
4.3. The First Modification of Myopia Management
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pan, C.W.; Ramamurthy, D.; Saw, S.M. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol. Opt. 2012, 32, 3–16. [Google Scholar] [CrossRef]
- Lam, C.S.; Lam, C.H.; Cheng, S.C.; Chan, L.Y. Prevalence of myopia among Hong Kong Chinese schoolchildren: Changes over two decades. Ophthalmic Physiol. Opt. 2012, 32, 17–24. [Google Scholar] [CrossRef]
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.J.; Resnikoff, S.J.O. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Saw, S.M.; Gazzard, G.; Shih-Yen, E.C.; Chua, W.H. Myopia and associated pathological complications. Ophthalmic Physiol. Opt. 2005, 25, 381–391. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.C.; Lam, C.S.; Yap, M.K. Prevalence of myopia-related retinal changes among 12-18 year old Hong Kong Chinese high myopes. Ophthalmic Physiol. Opt. 2013, 33, 652–660. [Google Scholar] [CrossRef] [PubMed]
- Lim, M.C.; Gazzard, G.; Sim, E.L.; Tong, L.; Saw, S.M. Direct costs of myopia in Singapore. Eye 2009, 23, 1086–1089. [Google Scholar] [CrossRef] [PubMed]
- Dolgin, E. The myopia boom. Nature 2015, 519, 276. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.; Vlasak, N.; Evans, B.J.W. High myopia: Reviews of myopia control strategies and myopia complications. Ophthalmic Physiol. Opt. 2024, 44, 1248–1260. [Google Scholar] [CrossRef] [PubMed]
- Leshno, A.; Farzavandi, S.K.; Gomez-de-Liaño, R.; Sprunger, D.T.; Wygnanski-Jaffe, T.; Mezer, E. Practice patterns to decrease myopia progression differ among paediatric ophthalmologists around the world. Br. J. Ophthalmol. 2019, 104, 535–540. [Google Scholar] [CrossRef] [PubMed]
- Wolffsohn, J.S.; Calossi, A.; Cho, P.; Gifford, K.; Jones, L.; Li, M.; Lipener, C.; Logan, N.S.; Malet, F.; Matos, S.; et al. Global trends in myopia management attitudes and strategies in clinical practice. Cont. Lens Anterior Eye 2016, 39, 106–116. [Google Scholar] [CrossRef]
- Wolffsohn, J.S.; Flitcroft, D.I.; Gifford, K.L.; Jong, M.; Jones, L.; Klaver, C.C.W.; Logan, N.S.; Naidoo, K.; Resnikoff, S.; Sankaridurg, P.; et al. IMI—Myopia Control Reports Overview and Introduction. Investig. Ophthalmol. Vis. Sci. 2019, 60, M1–M19. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Pérez, C.; Villa-Collar, C.; Santodomingo-Rubido, J.; Wolffsohn, J.S. Strategies and attitudes on the management of myopia in clinical practice in Spain—2022 update. J. Optom. 2024, 17, 100496. [Google Scholar] [CrossRef] [PubMed]
- Fan, D.S.P.; Lam, D.S.C.; Lam, R.F.; Lau, J.T.F.; Chong, K.S.; Cheung, E.Y.Y.; Lai, R.Y.K.; Chew, S.-J. Prevalence, Incidence, and Progression of Myopia of School Children in Hong Kong. Investig. Ophthalmol. Vis. Sci. 2004, 45, 1071–1075. [Google Scholar] [CrossRef] [PubMed]
- Rudnicka, A.R.; Kapetanakis, V.V.; Wathern, A.K.; Logan, N.S.; Gilmartin, B.; Whincup, P.H.; Cook, D.G.; Owen, C.G. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: Implications for aetiology and early prevention. Br. J. Ophthalmol. 2016, 100, 882–890. [Google Scholar] [CrossRef] [PubMed]
- Thibos, L.N.; Wheeler, W.; Horner, D. Power vectors: An application of Fourier analysis to the description and statistical analysis of refractive error. Optom. Vis. Sci. 1997, 74, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Lam, C.S.Y.; Tang, W.C.; Tse, D.Y.; Lee, R.P.K.; Chun, R.K.M.; Hasegawa, K.; Qi, H.; Hatanaka, T.; To, C.H. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: A 2-year randomised clinical trial. Br. J. Ophthalmol. 2020, 104, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Wolffsohn, J.S.; Whayeb, Y.; Logan, N.S.; Weng, R.; the International Myopia Institute Ambassador Group. IMI—Global Trends in Myopia Management Attitudes and Strategies in Clinical Practice—2022 Update. Investig. Ophthalmol. Vis. Sci. 2023, 64, 6. [Google Scholar] [CrossRef]
- Correction of Myopia Evaluation Trial 2 Study Group for the Pediatric Eye Disease Investigator Group. Progressive-addition lenses versus single-vision lenses for slowing progression of myopia in children with high accommodative lag and near esophoria. Investig. Ophthalmol. Vis. Sci. 2011, 52, 2749–2757. [Google Scholar] [CrossRef]
- Edwards, M.H.; Li, R.W.-h.; Lam, C.S.-y.; Lew, J.K.-f.; Yu, B.S.-y. The Hong Kong progressive lens myopia control study: Study design and main findings. Investig. Ophthalmol. Vis. Sci. 2002, 43, 2852–2858. [Google Scholar]
- Cheng, X.; Brennan, N.A.; Toubouti, Y.; Greenaway, N.L. Safety of soft contact lenses in children: Retrospective review of six randomized controlled trials of myopia control. Acta Ophthalmol. 2020, 98, e346–e351. [Google Scholar] [CrossRef]
- Bullimore, M.A. The safety of soft contact lenses in children. Optom. Vis. Sci. 2017, 94, 638. [Google Scholar] [CrossRef]
- Sankaridurg, P.; Chen, X.; Naduvilath, T.; Lazon de la Jara, P.; Lin, Z.; Li, L.; Smith, E.L., 3rd; Ge, J.; Holden, B.A. Adverse events during 2 years of daily wear of silicone hydrogels in children. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom. 2013, 90, 961–969. [Google Scholar] [CrossRef] [PubMed]
- Bullimore, M.A.; Richdale, K. Incidence of Corneal Adverse Events in Children Wearing Soft Contact Lenses. Eye Contact Lens 2023, 49, 204–211. [Google Scholar] [CrossRef]
- Wagner, H.; Chalmers, R.L.; Mitchell, G.L.; Jansen, M.E.; Kinoshita, B.T.; Lam, D.Y.; McMahon, T.T.; Richdale, K.; Sorbara, L.; Group, C.S. Risk factors for interruption to soft contact lens wear in children and young adults. Optom. Vis. Sci. 2011, 88, 973–980. [Google Scholar] [CrossRef]
- Zadnik, K.; Sinnott, L.T.; Cotter, S.A.; Jones-Jordan, L.A.; Kleinstein, R.N.; Manny, R.E.; Twelker, J.D.; Mutti, D.O. Prediction of juvenile-onset myopia. JAMA Ophthalmol. 2015, 133, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Ding, X.; Guo, X.; Chen, Y.; Zhang, J.; He, M. Association of Age at Myopia Onset With Risk of High Myopia in Adulthood in a 12-Year Follow-up of a Chinese Cohort. JAMA Ophthalmol. 2020, 138, 1129–1134. [Google Scholar] [CrossRef] [PubMed]

| Parameters | Myopes | Pre-Myopes | p Value ※ |
|---|---|---|---|
| Age (year) | 8.2 ± 1.4 | 7.8 ± 1.5 | <0.001 #,* |
| AL (mm) | 24.15 ± 0.98 | 23.04 ± 0.78 | <0.001 #,* |
| BCVA | 21 ± 2 | 21 ± 2 | 0.688 # |
| Sex (Male/Female/Unknown) | 416/417/26 | 223/216/20 | 0.814 º |
| SER (D) | −2.25 ± 1.45 | −0.16 ± 1.37 | <0.001 #,* |
| J0 (D) | 0.36 ± 0.44 | 0.17 ± 0.24 | <0.001 #,* |
| J45 (D) | −0.03 ± 0.15 | −0.02 ± 0.09 | 0.037 #,* |
| Myopia Recommendation | Brand Name of the Lens |
|---|---|
| Myopia control spectacle lenses | MyoKids, MyoVision (ZEISS), MiyoSmart (HOYA), Stellest (Essilor) |
| Bifocal/progressive spectacle lenses | Myopliux (Max, Plus), KidsPro (SWISSCOAT) |
| Myopia control contact lenses | MiSight (CooperVision) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, H.-Y.; Xu, F.-Y.; Liu, K.K.K.; Chan, Y.-P.; Chow, A.; Jones, D.; Lam, C.S.Y. Myopia Management in Hong Kong. J. Clin. Med. 2025, 14, 698. https://doi.org/10.3390/jcm14030698
Zhang H-Y, Xu F-Y, Liu KKK, Chan Y-P, Chow A, Jones D, Lam CSY. Myopia Management in Hong Kong. Journal of Clinical Medicine. 2025; 14(3):698. https://doi.org/10.3390/jcm14030698
Chicago/Turabian StyleZhang, Han-Yu, Fang-Yu Xu, Kenneth Ka King Liu, Yan-Pui Chan, Amy Chow, Deborah Jones, and Carly Siu Yin Lam. 2025. "Myopia Management in Hong Kong" Journal of Clinical Medicine 14, no. 3: 698. https://doi.org/10.3390/jcm14030698
APA StyleZhang, H.-Y., Xu, F.-Y., Liu, K. K. K., Chan, Y.-P., Chow, A., Jones, D., & Lam, C. S. Y. (2025). Myopia Management in Hong Kong. Journal of Clinical Medicine, 14(3), 698. https://doi.org/10.3390/jcm14030698








