Evaluation, Management and Therapeutic Approach of Cardiovascular–Kidney–Metabolic Syndrome: A Multidisciplinary Delphi Expert Consensus
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
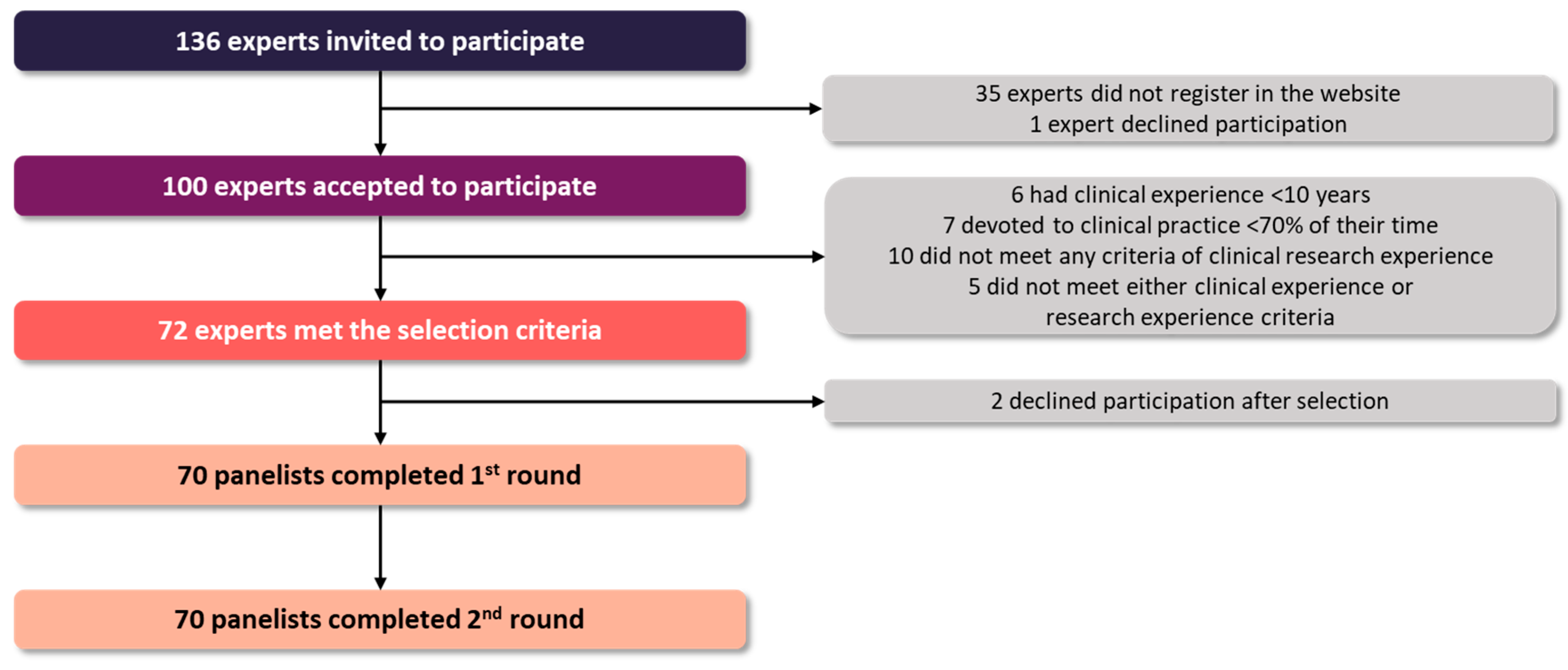
2.2. Selection of Experts
2.3. Development of the Questionnaire
2.4. Consensus Level
2.5. Statistical Analysis
3. Results
3.1. Overall Results
3.2. Evaluation of Patients with CKM Syndrome
3.3. Overall Management of Patients with CKM Syndrome
3.4. Therapeutic Approach for Patients with CKM Syndrome
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ndumele, C.E.; Rangaswami, J.; Chow, S.L.; Neeland, I.J.; Tuttle, K.R.; Khan, S.S.; Coresh, J.; Mathew, R.O.; Baker-Smith, C.M.; Carnethon, M.R.; et al. Cardiovascular-kidney-metabolic health: A presidential advisory from the American heart association. Circulation 2023, 148, 1606–1635. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.E.; Joo, J.; Kuku, K.O.; Downie, C.; Hashemian, M.; Powell-Wiley, T.M.; Shearer, J.J.; Roger, V.L. Prevalence, disparities, and mortality of cardiovascular-kidney-metabolic syndrome in US adults, 2011–2018. Am. J. Med. 2025, 138, 970–979.e7. [Google Scholar] [CrossRef] [PubMed]
- Zhu, R.; Wang, R.; He, J.; Wang, L.; Chen, H.; Niu, X.; Sun, Y.; Guan, Y.; Gong, Y.; Zhang, L.; et al. Prevalence of cardiovascular-kidney-metabolic syndrome stages by social determinants of health. JAMA Netw. Open 2024, 7, e2445309. [Google Scholar] [CrossRef] [PubMed]
- Ji, H.; Sabanayagam, C.; Matsushita, K.; Cheng, C.Y.; Rim, T.H.; Sheng, B.; Li, H.; Tham, Y.C.; Cheng, S.; Wong, T.Y. Sex differences in cardiovascular-kidney-metabolic syndrome: 30-year us trends and mortality risks-brief report. Arterioscler. Thromb. Vasc. Biol. 2025, 45, 157–161. [Google Scholar] [CrossRef]
- Minhas, A.M.K.; Mathew, R.O.; Sperling, L.S.; Nambi, V.; Virani, S.S.; Navaneethan, S.D.; Shapiro, M.D.; Abramov, D. Prevalence of the cardiovascular-kidney-metabolic syndrome in the United States. J. Am. Coll. Cardiol. 2024, 83, 1824–1826. [Google Scholar] [CrossRef]
- Ferdinand, K.C.; Norris, K.C.; Rodbard, H.W.; Trujillo, J.M. Humanistic and economic burden of patients with cardiorenal metabolic conditions: A systematic review. Diabetes Ther. 2023, 14, 1979–1996. [Google Scholar] [CrossRef]
- Nichols, G.A.; Amitay, E.L.; Chatterjee, S.; Steubl, D. Health care costs associated with the development and combination of cardio-renal-metabolic diseases. Kidney360 2023, 4, 1382–1388. [Google Scholar] [CrossRef]
- Claudel, S.E.; Schmidt, I.M.; Waikar, S.S.; Verma, A. Cumulative incidence of mortality associated with cardiovascular-kidney-metabolic (CKM) syndrome. J. Am. Soc. Nephrol. 2025, 36, 1343–1351. [Google Scholar] [CrossRef]
- Bansal, N.; Weiner, D.; Sarnak, M. Cardiovascular-kidney-metabolic health syndrome: What does the American heart association framework mean for nephrology? J. Am. Soc. Nephrol. 2024, 35, 649–652. [Google Scholar] [CrossRef]
- Lee, C.H.; Tan, G.; Tang, S.C.W.; Ng, Y.W.; Lee, M.K.Y.; Chan, J.W.M.; Chan, T.M. Incorporating the cardiovascular-kidney-metabolic health framework into the local healthcare system: A position statement from the Hong Kong College of Physicians. Hong Kong Med. J. 2025, 31, 58–64. [Google Scholar] [CrossRef]
- Jones, J.; Hunter, D. Consensus methods for medical and health services research. Br. Med. J. 1995, 311, 376–380. [Google Scholar] [CrossRef] [PubMed]
- Shang, Z. Use of Delphi in health sciences research: A narrative review. Medicine 2023, 102, e32829. [Google Scholar] [CrossRef]
- Nasa, P.; Jain, R.; Juneja, D. Delphi methodology in healthcare research: How to decide its appropriateness. World J. Methodol. 2021, 11, 116–129. [Google Scholar] [CrossRef]
- Gorriz, J.L.; Gil, F.A.; Lopez, M.A.B.; Soto, A.B.; Cabrera, F.J.C.; Cisneros, A.; Guerrero, S.C.; Conejos, M.D.; Cabello, I.E.; Planelles, M.C.F.; et al. Improvement in the detection, diagnosis, and early treatment of chronic kidney disease in Spain. The IntERKit project. Nefrologia (Engl. Ed.) 2025, 45, 351–359. [Google Scholar] [CrossRef]
- Neeland, I.J.; Al-Kindi, S.G.; Tashtish, N.; Eaton, E.; Friswold, J.; Rahmani, S.; White-Solaru, K.T.; Rashid, I.; Berg, D.; Rana, M.; et al. Lessons learned from a patient-centered, team-based intervention for patients with type 2 diabetes at high cardiovascular risk: Year 1 results from the CINEMA program. J. Am. Heart Assoc. 2022, 11, e024482. [Google Scholar] [CrossRef]
- Martínez-González, N.A.; Berchtold, P.; Ullman, K.; Busato, A.; Egger, M. Integrated care programmes for adults with chronic conditions: A meta-review. Int. J. Qual. Health Care 2014, 26, 561–570. [Google Scholar] [CrossRef] [PubMed]
- Lobo-Prat, D.; Sainz, L.; Laiz, A.; De Dios, A.; Fontcuberta, L.; Fernández, S.; Masip, M.; Riera, P.; Pagès-Puigdemont, N.; Ros, S.; et al. Designing an integrated care pathway for spondyloarthritis: A Lean Thinking approach. J. Eval. Clin. Pract. 2025, 31, e14132. [Google Scholar] [CrossRef]
- Marques, M.; Cobo, M.; Lopez-Sanchez, P.; Garcia-Magallon, B.; Salazar, M.L.S.; Lopez-Ibor, J.V.; Janeiro, D.; Garcia, E.; Briales, P.S.; Montero, E.; et al. Multidisciplinary approach to patients with heart failure and kidney disease: Preliminary experience of an integrated cardiorenal unit. Clin. Kidney J. 2023, 16, 2100–2107. [Google Scholar] [CrossRef] [PubMed]
- Gamez, M.A.; Palomas, J.L.B.; Mayoral, A.R.; Manzanares, R.G.; Garcia, J.M.; Rodriguez, N.R.; Somoza, F.J.E.; Fillat, A.C.; Padial, L.R.; Sanchez, M.A. Outcomes of patients with heart failure followed in units accredited by the SEC-Excelente-IC quality program according to the type of unit. Rev. Esp. Cardiol. (Engl. Ed.) 2025, 78, 12–21. [Google Scholar] [CrossRef]
- Orozco-Beltran, D.; Cos-Claramunt, F.X. Primary care diabetes in Spain. Prim. Care Diabetes 2008, 2, 101–103. [Google Scholar] [CrossRef]
- Ciciurkaite, G.; Moloney, M.E.; Brown, R.L. The incomplete medicalization of obesity: Physician office visits, diagnoses, and treatments, 1996–2014. Public Health Rep. 2019, 134, 141–149. [Google Scholar] [CrossRef]
- Szymanski, R.; Abraham, M.; Childs, W.; Le, K.; Velez, C.; Vaughn, I.; Lamerato, L.; Budzynska, K. Factors associated with receiving an obesity diagnosis and obesity-related treatment for patients with obesity class II and III within a single integrated health system. Prev. Med. Rep. 2024, 46, 102879. [Google Scholar] [CrossRef]
- Zhang, N.; Liu, X.; Wang, L.; Zhang, Y.; Xiang, Y.; Cai, J.; Xu, H.; Xiao, X.; Zhao, X. Lifestyle factors and their relative contributions to longitudinal progression of cardio-renal-metabolic multimorbidity: A prospective cohort study. Cardiovasc. Diabetol. 2024, 23, 265. [Google Scholar] [CrossRef]
- Kim, B.S.; Kim, H.J.; Kim, H.; Lee, J.; Ahn, S.B.; Shin, J.H.; Lim, Y.H. Hepatic steatosis in cardiovascular-kidney-metabolic syndrome: Fatty liver index as a predictor of cardiovascular outcomes. Eur. J. Prev. Cardiol. 2025, zwaf396. [Google Scholar] [CrossRef]
- Agarwal, R.; Fouque, D. The foundation and the four pillars of treatment for cardiorenal protection in people with chronic kidney disease and type 2 diabetes. Nephrol. Dial. Transplant. 2023, 38, 253–257. [Google Scholar] [CrossRef]
- Braunwald, E. From cardiorenal to cardiovascular-kidney-metabolic syndromes. Eur. Heart J. 2025, 46, 682–684. [Google Scholar] [CrossRef] [PubMed]
- Zannad, F.; Sanyal, A.J.; Butler, J.; Miller, V.; Harrison, S.A. Integrating liver endpoints in clinical trials of cardiovascular and kidney disease. Nat. Med. 2024, 30, 2423–2431. [Google Scholar] [CrossRef] [PubMed]
- Lo, K.B.; Iskarous, K.; Sankaranarayanan, R. Sodium glucose cotransporter 2 inhibitors across the spectrum of cardiovascular kidney metabolic syndrome. Cardiol. Clin. 2025, 43, 403–414. [Google Scholar] [CrossRef]
- Guerrero-Mauvecin, J.; Villar-Gomez, N.; Mino-Izquierdo, L.; Povo-Retana, A.; Ramos, A.M.; Ruiz-Hurtado, G.; Sanchez-Nino, M.D.; Ortiz, A.; Sanz, A.B. Antioxidant effects of SGLT2 inhibitors on cardiovascular-kidney-metabolic (CKM) syndrome. Antioxidants 2025, 14, 701. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Peterson, E.; Pagidipati, N. Barriers to prescribing glucose-lowering therapies with cardiometabolic benefits. Am. Heart J. 2020, 224, 47–53. [Google Scholar] [CrossRef]
- Singh, T.; Li, T.; Mandelbrot, D.; Astor, B.C.; Mehr, A.P. Prescribing patterns for sodium-glucose cotransporter 2 inhibitors: A survey of nephrologists. Kidney Int. Rep. 2023, 8, 1669–1671. [Google Scholar] [CrossRef]
- Ozaki, A.F.; Ko, D.T.; Chong, A.; Fang, J.; Atzema, C.L.; Austin, P.C.; Stukel, T.A.; Tu, K.; Udell, J.A.; Naimark, D.; et al. Prescribing patterns and factors associated with sodium-glucose cotransporter-2 inhibitor prescribing in patients with diabetes mellitus and atherosclerotic cardiovascular disease. CMAJ Open 2023, 11, E494–E503. [Google Scholar] [CrossRef]
- Neves, J.S.; Leite, A.R.; Marcelino, M.; Melo, M.; Freitas, P.; Ramalho, C.; Calcada, E. Trends in antidiabetic drug use in Portugal: 8 years real-world data from a nationwide retrospective observational study (2017–2024) (TREND-8 study). Diabetes Obes. Metab. 2025, 27, 4022–4028. [Google Scholar] [CrossRef]
- Esteban-Fernandez, A.; Gomez-Otero, I.; Lopez-Fernandez, S.; Santamarta, M.R.; Pastor-Perez, F.J.; Fluvia-Brugues, P.; Perez-Rivera, J.A.; Lopez, A.L.; Garcia-Pinilla, J.M.; Palomas, J.L.B.; et al. Influence of the medical treatment schedule in new diagnoses patients with heart failure and reduced ejection fraction. Clin. Res. Cardiol. 2024, 113, 1171–1182. [Google Scholar] [CrossRef] [PubMed]
- Eckel, R.H.; Blaha, M.J. Cardiometabolic Medicine: A Call for a New Subspeciality Training Track in Internal Medicine. Am. J. Med. 2019, 132, 788–790. [Google Scholar] [CrossRef] [PubMed]
- Shapiro Michael, D.; Maron David, J.; Morris Pamela, B.; Kosiborod, M.; Sandesara Pratik, B.; Virani Salim, S.; Khera, A.; Ballantyne Christie, M.; Baum Seth, J.; Sperling Laurence, S.; et al. Preventive Cardiology as a Subspecialty of Cardiovascular Medicine. J. Am. Coll. Cardiol. 2019, 74, 1926–1942. [Google Scholar] [CrossRef] [PubMed]
- Rangaswami, J.; Tuttle, K.; Vaduganathan, M. Cardio-Renal-Metabolic Care Models. Circ. Cardiovasc. Qual. Outcomes 2020, 13, e007264. [Google Scholar] [CrossRef]
- Greene, S.J.; Fonarow, G.C.; Butler, J. Sodium-glucose cotransporter 2 inhibitors for heart failure with mildly reduced or preserved ejection fraction: Time to deliver implementation. Eur. J. Heart Fail. 2022, 24, 1902–1905. [Google Scholar] [CrossRef]
- Fernandez-Fernandez, B.; Gorriz, J.L.; Cebrian-Cuenca, A.; Fácila, L.; Fernandez Rodriguez, J.M.; Maraver, M.P.; Ortiz, A. From Evidence to Action: Advancing Timely Implementation of Triple Therapy in Type 2 Diabetes Mellitus and CKD. Kidney Int. Rep. 2025; in press. [Google Scholar] [CrossRef]
- SCORE2 working group and ESC Cardiovascular risk collaboration. SCORE2 risk prediction algorithms: New models to estimate 10-year risk of cardiovascular disease in Europe. Eur. Heart J. 2021, 42, 2439–2454. [CrossRef]
- SCORE2-OP working group and ESC Cardiovascular risk collaboration. SCORE2-OP risk prediction algorithms: Estimating incident cardiovascular event risk in older persons in four geographical risk regions. Eur. Heart J. 2021, 42, 2455–2467. [CrossRef] [PubMed]
- SCORE2-Diabetes Working Group and the ESC Cardiovascular Risk Collaboration. SCORE2-Diabetes: 10-year cardiovascular risk estimation in type 2 diabetes in Europe. Eur. Heart J. 2023, 44, 2544–2556. [CrossRef]
- Matsushita, K.; Kaptoge, S.; Hageman, S.H.J.; Sang, Y.; Ballew, S.H.; Grams, M.E.; Surapaneni, A.; Sun, L.; Arnlov, J.; Bozic, M.; et al. Including measures of chronic kidney disease to improve cardiovascular risk prediction by SCORE2 and SCORE2-OP. Eur. J. Prev. Cardiol. 2023, 30, 8–16. [Google Scholar] [CrossRef]
- Khan, S.S.; Coresh, J.; Pencina, M.J.; Ndumele, C.E.; Rangaswami, J.; Chow, S.L.; Palaniappan, L.P.; Sperling, L.S.; Virani, S.S.; Ho, J.E.; et al. Novel Prediction Equations for Absolute Risk Assessment of Total Cardiovascular Disease Incorporating Cardiovascular-Kidney-Metabolic Health: A Scientific Statement From the American Heart Association. Circulation 2023, 148, 1982–2004. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Zhou, P.; Fan, F.; Hao, Y.; Zhao, W.; Wang, Z.; Deng, X.; Deng, Q.; Hao, Y.; Yang, N.; et al. A simple score, CKM(2)S(2)-BAG, to predict cardiovascular risk with cardiovascular-kidney-metabolic health metrics. iScience 2025, 28, 112780. [Google Scholar] [CrossRef]
- López Gómez, H.J.; García-Foncillas López, R. Cross-Sectional Study of Attendance at a Primary Care Consultation in a Social Security Health System. Fam. Med. Prim. Care Open Access 2025, 9, 276. [Google Scholar] [CrossRef]
- Guilabert, M.; Sanchez-Garcia, A.; Asencio, A.; Marrades, F.; Garcia, M.; Mira, J.J.; Dafo, C. Challenges and strategies to recover and dynamize primary care: SWOT-CAME analysis in a health department. Aten. Primaria 2024, 56, 102809. [Google Scholar] [CrossRef]
- Vara-Ortiz, M.A.; Marcos-Alonso, S.; Fabrellas-Padres, N. Experience of primary care nurses applying nurse-led management of patients with acute minor illnesses. Int. J. Nurs. Pract. 2024, 30, e13216. [Google Scholar] [CrossRef]
- Ferreira, J.P.; Zannad, F. We need simpler and more integrated guidelines in cardio-kidney-metabolic diseases. JACC Heart Fail. 2025, 13, 371–374. [Google Scholar] [CrossRef]
- Handelsman, Y.; Anderson, J.E.; Bakris, G.L.; Ballantyne, C.M.; Bhatt, D.L.; Bloomgarden, Z.T.; Bozkurt, B.; Budoff, M.J.; Butler, J.; Cherney, D.Z.I.; et al. DCRM 2.0: Multispecialty practice recommendations for the management of diabetes, cardiorenal, and metabolic diseases. Metabolism 2024, 159, 155931. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Lei, L.; Wang, W.; Ding, W.; Yu, Y.; Pu, B.; Peng, Y.; Li, Y.; Zhang, L.; Guo, Y. Social risk profile and cardiovascular-kidney-metabolic syndrome in US adults. J. Am. Heart Assoc. 2024, 13, e034996. [Google Scholar] [CrossRef] [PubMed]
- Cotton, A.; Salerno, P.R.; Deo, S.V.; Virani, S.S.; Nasir, K.; Neeland, I.; Rajagopalan, S.; Sattar, N.; Al-Kindi, S.; Elgudin, Y.E. The association between county-level social determinants of health and cardio-kidney-metabolic disease attributed all-cause mortality in the US: A cross sectional analysis. Am. J. Med. Sci. 2025, 369, 491–497. [Google Scholar] [CrossRef] [PubMed]
| Statement/Recommendation | Round | CAR | END | FM | IM | NEPH | Global | Median | Result |
|---|---|---|---|---|---|---|---|---|---|
| 01. The concept of CKM syndrome is intended to facilitate the multidisciplinary care process of patients with a clinical management approach based on the cardiovascular–renal–metabolic continuum. | 2 | 100% | 100% | 89% | 92% | 100% | 96% | 9 | CONSENSUS |
| 02. CKM syndrome is defined as a complex systemic entity resulting from the multidirectional pathophysiological interaction between metabolic risk factors, CKD and the cardiovascular system, which multiply the risks of the development and progression of each condition, as well as an increased risk of cardiovascular and renal events. | 1 | 100% | 100% | 84% | 92% | 93% | 93% | 9 | CONSENSUS |
| 03. The basis of CKM syndrome focuses on excess and/or dysfunction of adipose tissue, which leads to a pro-inflammatory, pro-oxidative, and insulin-resistant state that accelerates metabolic damage and increases the risk of cardiovascular and kidney disease. | 2 | 100% | 100% | 84% | 92% | 93% | 93% | 8 | CONSENSUS |
| 04a. CKM syndrome includes both people at risk for CVD due to the presence of metabolic risk factors, CKD, or both, as well as people with existing CVD potentially related to metabolic risk factors or CKD. | 2 | 100% | 100% | 89% | 92% | 79% | 91% | 9 | LACK OF CONSENSUS |
| 04b. CKM syndrome includes individuals at risk for CVD due to the presence of metabolic risk factors, CKD, or both. | 2 | 92% | 100% | 84% | 83% | 93% | 90% | 8 | CONSENSUS |
| 04c. CKM syndrome includes people with existing CVD potentially related to metabolic risk factors or CKD, or both. | 2 | 100% | 100% | 89% | 92% | 86% | 93% | 8 | CONSENSUS |
| 05. Screening for CKM syndrome should be performed for patients with at least one risk factor associated with any of the CKM conditions and structured based on each of the CKM conditions, regardless of the specialist who performs it. | 2 | 100% | 100% | 89% | 100% | 93% | 96% | 9 | CONSENSUS |
| 06. Physical evaluation should include measurement of blood pressure, body mass index, abdominal circumference, cardiopulmonary auscultation, and detection of peripheral edema. | 1 | 100% | 100% | 95% | 83% | 86% | 93% | 8 | CONSENSUS |
| 07. Basic laboratory tests should include blood glucose, hemoglobin A1c, lipid profile, glomerular filtration rate (eGFR), urine albumin, and FIB-4. | 2 | 100% | 92% | 89% | 83% | 100% | 93% | 9 | CONSENSUS |
| 08. Depending on the clinical context, electrocardiogram and, if available, echocardioscopy should be performed to evaluate cardiac function and detect arrhythmias or ventricular hypertrophy. | 2 | 100% | 92% | 95% | 92% | 100% | 96% | 9 | CONSENSUS |
| 09. In patients with at least one of the CKM conditions, the presence of the other two conditions should be proactively analyzed. | 1 | 100% | 100% | 95% | 100% | 100% | 99% | 9 | CONSENSUS |
| 10. The cardiovascular condition of CKM syndrome is present when subclinical conditions or clinical cardiovascular events related to atherosclerotic cardiovascular disease, coronary heart disease, heart failure, or atrial fibrillation are determined. | 1 | 100% | 92% | 89% | 100% | 86% | 93% | 8 | CONSENSUS |
| 11. The renal condition of CKM syndrome is present when eGFR < 60 mL/min/1.73 m2 or albumin/creatinine ratio > 30 mg/g is/are maintained for at least 3 months. | 1 | 100% | 100% | 84% | 100% | 100% | 96% | 9 | CONSENSUS |
| 12. The metabolic condition of CKM syndrome is present when overweight/obesity, abdominal obesity, and/or dysfunctional adipose tissue (manifested as prediabetes) are diagnosed, with or without the presence of other metabolic risk factors (hypertriglyceridemia, high blood pressure, metabolic syndrome, or diabetes). | 1 | 92% | 83% | 84% | 100% | 93% | 90% | 8 | CONSENSUS |
| 13a. An app aimed at health care professionals would favor the diagnosis, treatment and monitoring of CKM patients. | 2 | 77% | 50% | 79% | 75% | 79% | 73% | 8 | LACK OF CONSENSUS |
| 13b. An app aimed at patients would favor the diagnosis, treatment and monitoring of CKM patients. | 2 | 38% | 50% | 58% | 58% | 50% | 51% | 7 | LACK OF CONSENSUS |
| 14. Patients with CKM should be classified into different stages according to their cardiovascular–renal risk to facilitate their management by health care professionals. | 1 | 100% | 100% | 89% | 92% | 100% | 96% | 8 | CONSENSUS |
| 15. Stages 0–4 * established by the AHA presidential advisory are appropriate for patients with CKM. * 0, no cardiometabolic risk factors; 1, excessive or dysfunctional adiposity; 2, metabolic risk factors and/or CKD; 3, subclinical CVD in CKM; 4, clinical CVD in CKM. | 2 | 92% | 100% | 79% | 92% | 93% | 90% | 8 | LACK OF CONSENSUS |
| 16. Creating a basic analytical profile of CKM syndrome would help diagnose patients with risk factors. | 1 | 100% | 92% | 84% | 92% | 100% | 93% | 9 | CONSENSUS |
| 17. The key parameters for diagnosing CKM syndrome should be systematically included in any analysis and be updated in computer systems with appropriate periodicity. | 1 | 100% | 92% | 84% | 92% | 93% | 91% | 8,5 | CONSENSUS |
| 18. It should be encouraged that, in the presence of anomalies in the basic analytical parameters, the electronic health record should generate alerts to identify CKM patients. | 1 | 100% | 100% | 89% | 92% | 93% | 94% | 9 | CONSENSUS |
| 19. It should be encouraged that computer systems should allow coding of a diagnosis of CKM syndrome. | 1 | 100% | 100% | 84% | 100% | 93% | 94% | 9 | CONSENSUS |
| 20. Laboratory services should be involved in improving the available resources in terms of computer systems and requests for tests. | 1 | 100% | 100% | 95% | 92% | 93% | 96% | 9 | CONSENSUS |
| 21. Health care managers must be involved in improving the available resources to allow an optimal care model for patients with CKM syndrome. | 1 | 100% | 100% | 95% | 92% | 100% | 97% | 9 | CONSENSUS |
| Statement/Recommendation | Round | CAR | END | PC | IM | NEPH | Global | Median | Result |
|---|---|---|---|---|---|---|---|---|---|
| 22. Priority should be given to an early and comprehensive approach from the specialty that receives the patient to improve the quality of care regardless of the reason for consultation or admission. | 1 | 100% | 100% | 95% | 100% | 86% | 96% | 9 | CONSENSUS |
| 23. The aim of any intervention is to prevent the progression and delay the development of complications from the onset of CKM syndrome. | 1 | 100% | 100% | 95% | 100% | 93% | 97% | 9 | CONSENSUS |
| 24. The management of CKM patients is conditioned by the different clinical scenarios and comorbidities they present. | 1 | 92% | 100% | 95% | 100% | 93% | 96% | 9 | CONSENSUS |
| 25. Elderly or frail CKM patients require their management to be adapted to their situation. | 1 | 100% | 100% | 95% | 100% | 93% | 97% | 9 | CONSENSUS |
| 26. Integrated care circuits must be established with multidisciplinary reference teams that establish efficient and agile communication channels. | 2 | 100% | 100% | 89% | 83% | 100% | 94% | 9 | CONSENSUS |
| 27. Optimal patient care must be provided, reducing their passage through several specialists to those situations in which it is beneficial for the patient, based on preestablished criteria (advanced stages, instability, etc.) | 1 | 100% | 92% | 95% | 100% | 100% | 97% | 9 | CONSENSUS |
| 28. Multidisciplinary face-to-face consultations reinforce the optimal approach for patients with CKM. | 2 | 100% | 83% | 89% | 83% | 86% | 89% | 9 | CONSENSUS |
| 29. The referents of each specialty must respond quickly to the interconsultations from other specialties, and the queries of other doctors from their own specialty. | 1 | 100% | 100% | 89% | 83% | 100% | 94% | 9 | CONSENSUS |
| 30. Basic quality indicators must be established to assess the results of the implemented measures objectively. | 2 | 100% | 100% | 95% | 100% | 93% | 97% | 9 | CONSENSUS |
| 31. Nurses should play an active role in screening for CKM syndrome. | 2 | 100% | 100% | 79% | 100% | 100% | 94% | 9 | LACK OF CONSENSUS |
| 32. The role of the nursing staff is key in terms of anamnesis, basic physical examination, hygienic–dietetic–sanitary recommendations, and education of the patient with CKM syndrome. | 1 | 85% | 83% | 95% | 92% | 86% | 89% | 9 | CONSENSUS |
| 33. Nurses should play an active role in the follow-up plans of patients with CKM in coordination with physicians. | 1 | 92% | 100% | 89% | 100% | 93% | 94% | 9 | CONSENSUS |
| 34. Family physicians must play a leading role in the coordination among specialties in the management of patients with CKM. | 1 | 92% | 100% | 89% | 83% | 86% | 90% | 9 | CONSENSUS |
| 35. Telemedicine should help to improve patient engagement in self-management of the disease and in communication with the health care professional. | 2 | 100% | 92% | 84% | 100% | 86% | 91% | 9 | CONSENSUS |
| 36. Clinical records in a single computer system easily consulted and accessible by all specialists must be ensured. | 1 | 100% | 100% | 95% | 100% | 100% | 99% | 9 | CONSENSUS |
| 37. Education of the general population regarding the primordial prevention * of risk factors associated with the onset of CKM syndrome should be reinforced. * “Primordial prevention” refers to preventing the occurrence of risk factors before they develop. According to the American Heart Association (AHA), primordial prevention includes creating and maintaining conditions that minimize the occurrence of disease risk factors, as part of a broader approach to reducing the burden of cardiovascular disease. (“Value of primordial and primary prevention for cardiovascular disease: a policy statement from the American Heart Association” W. Weintraub, S. Daniels, L. Burke + 8 more · 23 Aug 2011). | 1 | 100% | 92% | 84% | 100% | 86% | 91% | 9 | CONSENSUS |
| 38. Patient health education should be reinforced so that they understand CKM syndrome and its inherent risks, as well as to empower them in their self-care and to comply with the recommendations from the health professionals. | 1 | 100% | 100% | 95% | 100% | 100% | 99% | 9 | CONSENSUS |
| 39. Training of all health professionals on CKM syndrome and its associated risks should be encouraged. | 1 | 100% | 100% | 95% | 100% | 93% | 97% | 9 | CONSENSUS |
| 40. Managers’ knowledge of the CKM syndrome and its implications should be reinforced. | 1 | 100% | 100% | 89% | 100% | 100% | 97% | 9 | CONSENSUS |
| Statement/Recommendation | Round | CAR | END | PC | IM | NEPH | Global | Median | Result |
|---|---|---|---|---|---|---|---|---|---|
| 41. Preventive measures should be adopted for patients with at least one risk factor associated with any of the CKM conditions. | 1 | 100% | 100% | 89% | 100% | 93% | 96% | 9 | CONSENSUS |
| 42. The diagnosis of CKM syndrome should involve continuous follow-up with a stipulated periodicity depending on the stage and clinical situation of the patient to evaluate the evolution and adjust treatment. | 1 | 100% | 100% | 89% | 100% | 100% | 97% | 9 | CONSENSUS |
| 43. Control goals for each CKM condition according to stage and clinical situations should be established. | 1 | 100% | 100% | 100% | 100% | 100% | 100% | 9 | CONSENSUS |
| 44. The interventions to be carried out for each CKM condition should be established according to the stage of the CKM syndrome and clinical situations. | 1 | 100% | 100% | 95% | 100% | 100% | 99% | 9 | CONSENSUS |
| 45. In subjects without any CKM risk factors, cardiovascular–renal–metabolic health maintenance measures should be implemented from an early age aimed at primordial prevention *. * “Primordial prevention” refers to preventing the occurrence of risk factors before they develop. According to the American Heart Association (AHA), primordial prevention includes the creation and maintenance of conditions that minimize the occurrence of disease risk factors, as part of a broader approach to reducing the burden of cardiovascular disease (“Value of primordial and primary prevention for cardiovascular disease: a policy statement from the American Heart Association” W. Weintraub, S. Daniels, L. Burke + 8 more · 23 Aug 2011) | 1 | 92% | 100% | 84% | 92% | 93% | 91% | 9 | CONSENSUS |
| 46. In patients with at least one risk factor associated with CKM syndrome *, primordial prevention of other risk factors associated with it should be carried out. * Alterations in glucose metabolism, alterations in kidney function; sleep disorders; gestational diabetes; early menopause; adverse effects on pregnancy; mental health or psychosocial problems; drug, alcohol or tobacco use; sedentary lifestyle or poor eating habits. | 1 | 100% | 100% | 95% | 100% | 100% | 99% | 9 | CONSENSUS |
| 47. A comprehensive and intensive approach should be adopted in patients with CKM, regardless of the overt CKM condition(s). | 2 | 100% | 100% | 95% | 92% | 93% | 96% | 9 | CONSENSUS |
| 48. The pharmacological approach to each CKM condition must be carried out based on the corresponding guidelines, protocols, or recommendations related to each of them. | 1 | 100% | 100% | 95% | 100% | 93% | 97% | 9 | CONSENSUS |
| 49. Lifestyle measures should be implemented from the early stages of CKM syndrome. | 1 | 100% | 100% | 95% | 92% | 100% | 97% | 9 | CONSENSUS |
| 50. Intensive weight loss should be emphasized at any stage of CKM syndrome. | 2 | 100% | 100% | 95% | 92% | 86% | 94% | 9 | CONSENSUS |
| 51. Drugs with demonstrated cardiovascular, renal, and/or metabolic benefits * should be administered from the early stages of CKM syndrome, within their authorized indications. * Drugs such as SGLT2i, GLP-1RA, statins and other lipid-lowering agents, ACEi/ARB, MRA, etc. | 1 | 100% | 83% | 95% | 83% | 93% | 91% | 9 | CONSENSUS |
| 52. Drugs with demonstrated cardiovascular, renal, and/or metabolic benefits * should be administered even when patients are in advanced stages of CKM syndrome, according to the established objectives, within their authorized indications. * Drugs such as SGLT2i, GLP-1AR, statins and other lipid-lowering agents, ACEi/ARB, MRA, etc. | 1 | 85% | 92% | 95% | 100% | 93% | 93% | 9 | CONSENSUS |
| 53. All patients with CKM and a cardiovascular event should be included in a comprehensive cardiac rehabilitation program tailored to their needs. | 2 | 100% | 100% | 89% | 92% | 86% | 93% | 9 | CONSENSUS |
| 54. A validated app would facilitate staging of patients with CKM, assessing their cardiovascular–renal risk, updating their control objectives, and proposing measures to be implemented. | 2 | 92% | 83% | 74% | 83% | 100% | 86% | 8 | LACK OF CONSENSUS |
| 55. Actions related to telemedicine should be recommended according to the stage of the patients with CKM and their psychosocial conditions. | 2 | 100% | 92% | 79% | 100% | 100% | 93% | 8 | LACK OF CONSENSUS |
| 56. Telemonitoring should be implemented to detect decompensations early as well as avoid hospitalizations and consultations. | 2 | 92% | 100% | 84% | 100% | 100% | 94% | 8 | CONSENSUS |
| 57. The creation of an analytical profile of CKM syndrome would help to better assess the risk of these patients throughout follow-up. | 1 | 100% | 100% | 84% | 92% | 100% | 94% | 9 | CONSENSUS |
| 58. Computer systems should alert on the measures to be implemented to help achieve the control and monitoring objectives. | 1 | 100% | 100% | 84% | 100% | 93% | 94% | 9 | CONSENSUS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orozco-Beltrán, D.; Quiroga, B.; Esteban-Fernández, A.; Lorenzo Almorós, A.; Bellido, V.; Benedito Pérez de Inestrosa, T.; de Haro, R.; Taboada, X.; Romero-Vigara, J.C. Evaluation, Management and Therapeutic Approach of Cardiovascular–Kidney–Metabolic Syndrome: A Multidisciplinary Delphi Expert Consensus. J. Clin. Med. 2025, 14, 8930. https://doi.org/10.3390/jcm14248930
Orozco-Beltrán D, Quiroga B, Esteban-Fernández A, Lorenzo Almorós A, Bellido V, Benedito Pérez de Inestrosa T, de Haro R, Taboada X, Romero-Vigara JC. Evaluation, Management and Therapeutic Approach of Cardiovascular–Kidney–Metabolic Syndrome: A Multidisciplinary Delphi Expert Consensus. Journal of Clinical Medicine. 2025; 14(24):8930. https://doi.org/10.3390/jcm14248930
Chicago/Turabian StyleOrozco-Beltrán, Domingo, Borja Quiroga, Alberto Esteban-Fernández, Ana Lorenzo Almorós, Virginia Bellido, Teresa Benedito Pérez de Inestrosa, Rubén de Haro, Xoana Taboada, and Juan Carlos Romero-Vigara. 2025. "Evaluation, Management and Therapeutic Approach of Cardiovascular–Kidney–Metabolic Syndrome: A Multidisciplinary Delphi Expert Consensus" Journal of Clinical Medicine 14, no. 24: 8930. https://doi.org/10.3390/jcm14248930
APA StyleOrozco-Beltrán, D., Quiroga, B., Esteban-Fernández, A., Lorenzo Almorós, A., Bellido, V., Benedito Pérez de Inestrosa, T., de Haro, R., Taboada, X., & Romero-Vigara, J. C. (2025). Evaluation, Management and Therapeutic Approach of Cardiovascular–Kidney–Metabolic Syndrome: A Multidisciplinary Delphi Expert Consensus. Journal of Clinical Medicine, 14(24), 8930. https://doi.org/10.3390/jcm14248930





