The Time to Discharge and Pain Reliever Intake Depending on the Use of a Drain After Laparoscopic Cholecystectomy
Abstract
1. Introduction
2. Materials and Methods
2.1. Current Sample
2.2. Data Analysis
3. Results
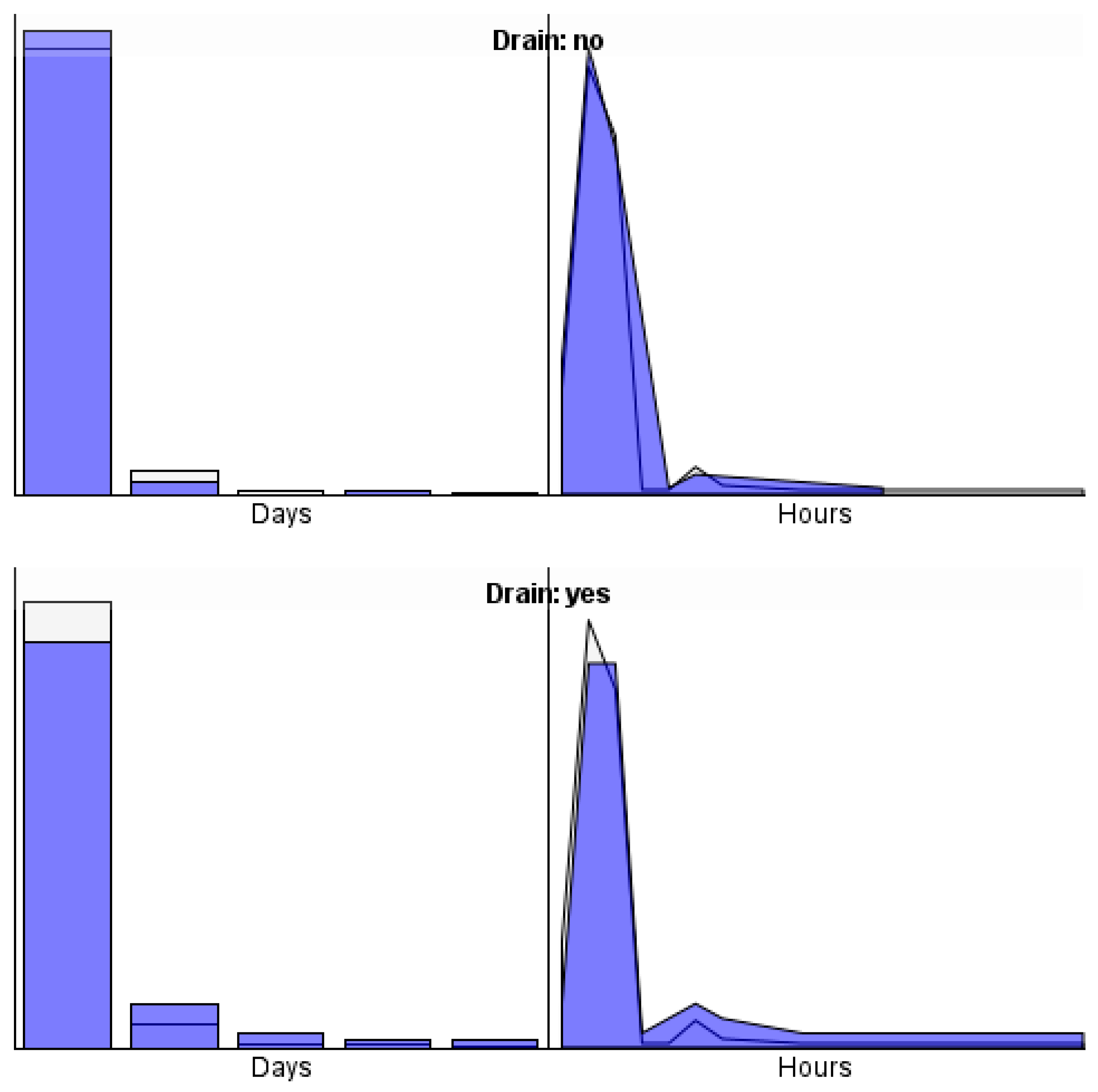
3.1. Postoperative Drain Insertion, and the Time from Surgery to Discharge
3.2. Postoperative Drain Insertion and the Intake of Pain Relievers
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Asad, U.; Wang, C.F.; Jones, M.W. Laparoscopic Cholecystectomy. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK448145/ (accessed on 2 July 2025). [PubMed]
- Feng, J.W.; Yang, X.H.; Liu, C.W.; Wu, B.Q.; Sun, D.L.; Chen, X.M.; Jiang, Y.; Qu, Z. Comparison of Laparoscopic, and Open Approach in Treating Gallbladder Cancer. J. Surg. Res. 2019, 234, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.Y.; You, Y.K.; Kim, D.G.; Lee, S.H.; Han, J.H.; Park, S.K.; Na, G.H.; Hong, T.H. Is a drain necessary routinely after laparoscopic cholecystectomy for an acutely inflamed gallbladder? A retrospective analysis of 457 cases. J. Gastrointest. Surg. Off. J. Soc. Surg. Aliment. Tract. 2014, 18, 941–946. [Google Scholar] [CrossRef] [PubMed]
- Lucarelli, P.; Picchio, M.; Martellucci, J.; De Angelis, F.; di Filippo, A.; Stipa, F.; Spaziani, E. Drain After Laparoscopic Cholecystectomy for Acute Calculous Cholecystitis. A Pilot Randomized Study. Indian J. Surg. 2015, 77 (Suppl. S2), 288–292. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gurusamy, K.S.; Koti, R.; Davidson, B.R. Routine abdominal drainage versus no abdominal drainage for uncomplicated laparoscopic cholecystectomy. Cochrane Database Syst. Rev. 2013, CD006004. [Google Scholar] [CrossRef] [PubMed]
- Tzovaras, G.; Liakou, P.; Fafoulakis, F.; Baloyiannis, I.; Zacharoulis, D.; Hatzitheofilou, C. Is there a role for drain use in elective laparoscopic cholecystectomy? A controlled randomized trial. Am. J. Surg. 2009, 197, 759–763. [Google Scholar] [CrossRef] [PubMed]
- Eldin, H.A.A.; Omran, H.M.; Rayan, M.T.; El Zohery, Y.H.A.M.; Khaliel, E.R.A. Laparoscopic Cholecystectomy with or without Abdominal Drain in Benign Non Complicated Gall Bladder Disease. QJM Int. J. Med. 2024, 117 (Suppl. S2), hcae175.278. [Google Scholar] [CrossRef]
- Picchio, M.; De Cesare, A.; Di Filippo, A.; Spaziani, M.; Spaziani, E. Prophylactic drainage after laparoscopic cholecystectomy for acute cholecystitis: A systematic review, and meta-analysis. Updates Surg. 2019, 71, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Choi, I.S.; Moon, J.I.; Yoon, D.S.; Choi, W.J.; Lee, S.E.; Sung, N.S.; Kwon, S.U.; Bae, I.E.; Roh, S.J.; et al. Optimal drain management following complicated laparoscopic cholecystectomy for acute cholecystitis: A propensity-matched comparative study. J. Minim. Invasive Surg. 2022, 25, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Mittal, S. Role of Routine Subhepatic Abdominal Drain Placement following Uncomplicated Laparoscopic Cholecystectomy: A Prospective Randomised Study. J. Clin. Diagn. Res. 2016, 10, PC03–PC05. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sarkar, S.; Kuiri, S.S.; Rajan, Y.; Kundu, K. A comparative study of laparoscopic cholecystectomy with, and without abdominal drain. Asian J. Med. Sci. 2023, 14, 229–235. [Google Scholar] [CrossRef]
- Ibrahim, A.H.; Wahab, A.W.M.A.; Ali, K.A.A.R. Use of Drain in Laparoscopic Cholecystectomy. Egypt. J. Hosp. Med. 2018, 73, 7615–7621. [Google Scholar] [CrossRef]
- El-labban, G.; Hokkam, E.; El-labban, M.; Saber, A.; Heissam, K.; El-Kammash, S. Laparoscopic elective cholecystectomy with, and without drain: A controlled randomised trial. J. Minimal Access Surg. 2012, 8, 90–92. [Google Scholar] [CrossRef] [PubMed]
- Nadeem, F.; Khan, M.R.; Naz, F.U. Comparison of mean pain scores for the patients with sub hepatic drainage to those without it after elective uncomplicated laparoscopic cholecystectomy. Pak. J. Med Sci. 2019, 35, 226–229. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Valappil, M.V.; Gulati, S.; Chhabra, M.; Mandal, A.; Bakshi, S.; Bhattacharyya, A.; Ghatak, S. Drain in laparoscopic cholecystectomy in acute calculous cholecystitis: A randomised controlled study. Postgrad. Med. J. 2020, 96, 606–609. [Google Scholar] [CrossRef] [PubMed]
- Sruthi, C.; Ashok Teja, P.; Sattar, A.; Chennupati, T.P.; Shahana, S. Prophylactic Drainage in Cholecystectomy in Uncomplicated Acute Cholecystitis. Eur. J. Cardiovasc. Med. 2023, 13, 568–575. [Google Scholar]
- Hussein, T.M. A Comparative Study of Laparoscopic Cholecystectomy with or without Drainage. Cuest. Fisioter. 2025, 54, 2732–2741. [Google Scholar] [CrossRef]
- Maurya, N.K.; Hingora, O.M.; Kumar, M.; Katiyar, A. Comparison of Postoperative Outcomes of Laparoscopic Cholecystectomy with or without Abdominal Prophylactic Drainage: A Prospective Interventional Study. J. Clin. Diagn. Res. 2023, 17, 28–31. [Google Scholar] [CrossRef]
- Saleem, H.; Saleem, A.; Siddiq, G.; Sheikh, S.S.A.; Saleem, H. Comparison of the Morbidity after Laparoscopic Cholecystectomy for Acutely Inflamed Gall Bladder with, and without Drain Insertion: A Randomized Controlled Trial. J. Rawalpindi Med. Coll. 2021, 25, 239–245. [Google Scholar] [CrossRef]
- Ko-iam, W.; Sandhu, T.; Paiboonworachat, S.; Pongchairerks, P.; Chotirosniramit, A.; Chotirosniramit, N.; Chandacham, K.; Jirapongcharoenlap, T.; Junrungsee, S. Predictive Factors for a Long Hospital Stay in Patients Undergoing Laparoscopic Cholecystectomy. Int. J. Hepatol. 2017, 2017, 5497936. [Google Scholar] [CrossRef] [PubMed]
| Drug | Unit | M | SD | min | max | n |
|---|---|---|---|---|---|---|
| Pyralgin | g | 2.67 | 2.17 | 1 | 20 | 198 |
| Paracetamol | g | 2.73 | 2.12 | 1 | 20 | 198 |
| Ibuprofen | mg | 600.00 | 500.00 | 200 | 2800 | 25 |
| Ketoprofen | mg | 100.00 | 0.00 | 100 | 100 | 5 |
| Postoperative Drain | ||||||||
|---|---|---|---|---|---|---|---|---|
| Time from | no | yes | ||||||
| surgery to discharge | M | SE | M | SE | F | df | p | η2 |
| Days | 1.05 | 0.04 | 1.27 | 0.06 | 7.94 | 1205 | 0.005 | 0.037 |
| Hours | 23.04 | 1.05 | 29.48 | 1.57 | 11.56 | 1205 | 0.001 | 0.053 |
| Postoperative Drain | ||||||||
|---|---|---|---|---|---|---|---|---|
| no | yes | |||||||
| Pain relievers | M | SE | M | SE | F | df | p | η2 |
| Pyralgin (g.) | 2.41 | 0.19 | 3.33 | 0.27 | 7.65 | 1.188 | 0.006 | 0.039 |
| Paracetamol (g.) | 2.45 | 0.18 | 3.40 | 0.27 | 8.80 | 1.188 | 0.003 | 0.045 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strzępek, Ł.; Czerw, A.; Curyło, M.; Mikos, M.; Florek, M.; Charkiewicz, D.; Partyka, O.; Pajewska, M.; Stachacz, G.; Sygit, K.; et al. The Time to Discharge and Pain Reliever Intake Depending on the Use of a Drain After Laparoscopic Cholecystectomy. J. Clin. Med. 2025, 14, 8752. https://doi.org/10.3390/jcm14248752
Strzępek Ł, Czerw A, Curyło M, Mikos M, Florek M, Charkiewicz D, Partyka O, Pajewska M, Stachacz G, Sygit K, et al. The Time to Discharge and Pain Reliever Intake Depending on the Use of a Drain After Laparoscopic Cholecystectomy. Journal of Clinical Medicine. 2025; 14(24):8752. https://doi.org/10.3390/jcm14248752
Chicago/Turabian StyleStrzępek, Łukasz, Aleksandra Czerw, Mateusz Curyło, Marcin Mikos, Maciej Florek, Dorota Charkiewicz, Olga Partyka, Monika Pajewska, Grzegorz Stachacz, Katarzyna Sygit, and et al. 2025. "The Time to Discharge and Pain Reliever Intake Depending on the Use of a Drain After Laparoscopic Cholecystectomy" Journal of Clinical Medicine 14, no. 24: 8752. https://doi.org/10.3390/jcm14248752
APA StyleStrzępek, Ł., Czerw, A., Curyło, M., Mikos, M., Florek, M., Charkiewicz, D., Partyka, O., Pajewska, M., Stachacz, G., Sygit, K., Porada, S., Gąska, I., Kaczmar, E., Grochans, E., Cybulska, A. M., Schneider-Matyka, D., Bandurska, E., Ciećko, W., Drobnik, J., ... Kozlowski, R. (2025). The Time to Discharge and Pain Reliever Intake Depending on the Use of a Drain After Laparoscopic Cholecystectomy. Journal of Clinical Medicine, 14(24), 8752. https://doi.org/10.3390/jcm14248752










