Prediction of Coronary Artery Spasm in Patients Without Obstructive Coronary Artery Disease Using a Comprehensive Clinical, Laboratory and Echocardiographic Risk Score
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Clinical Data
2.3. Laboratory Analysis
2.4. Coronary Angiography and Intracoronary Methylergonovine Testing
2.5. Echocardiographic Methods
2.6. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Associated Factors of CAS
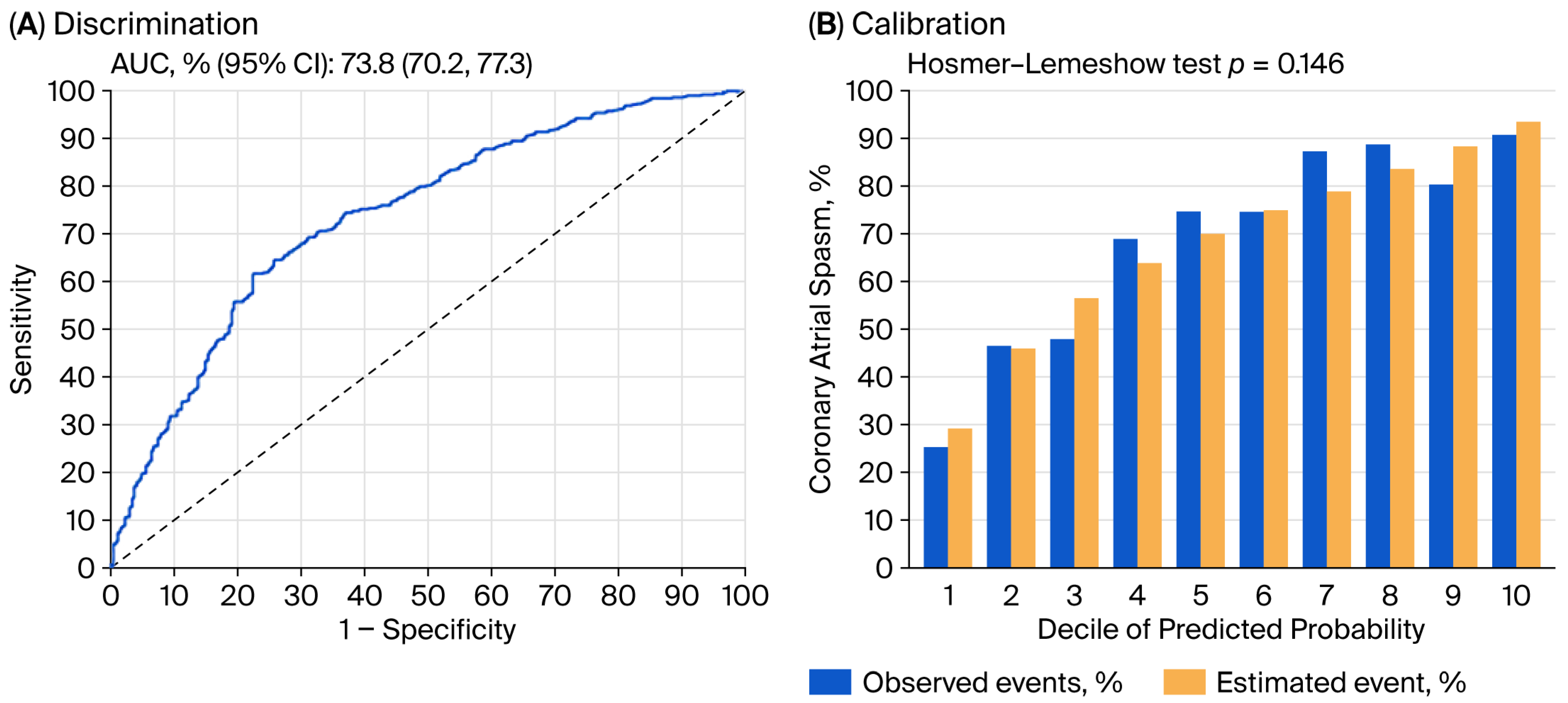
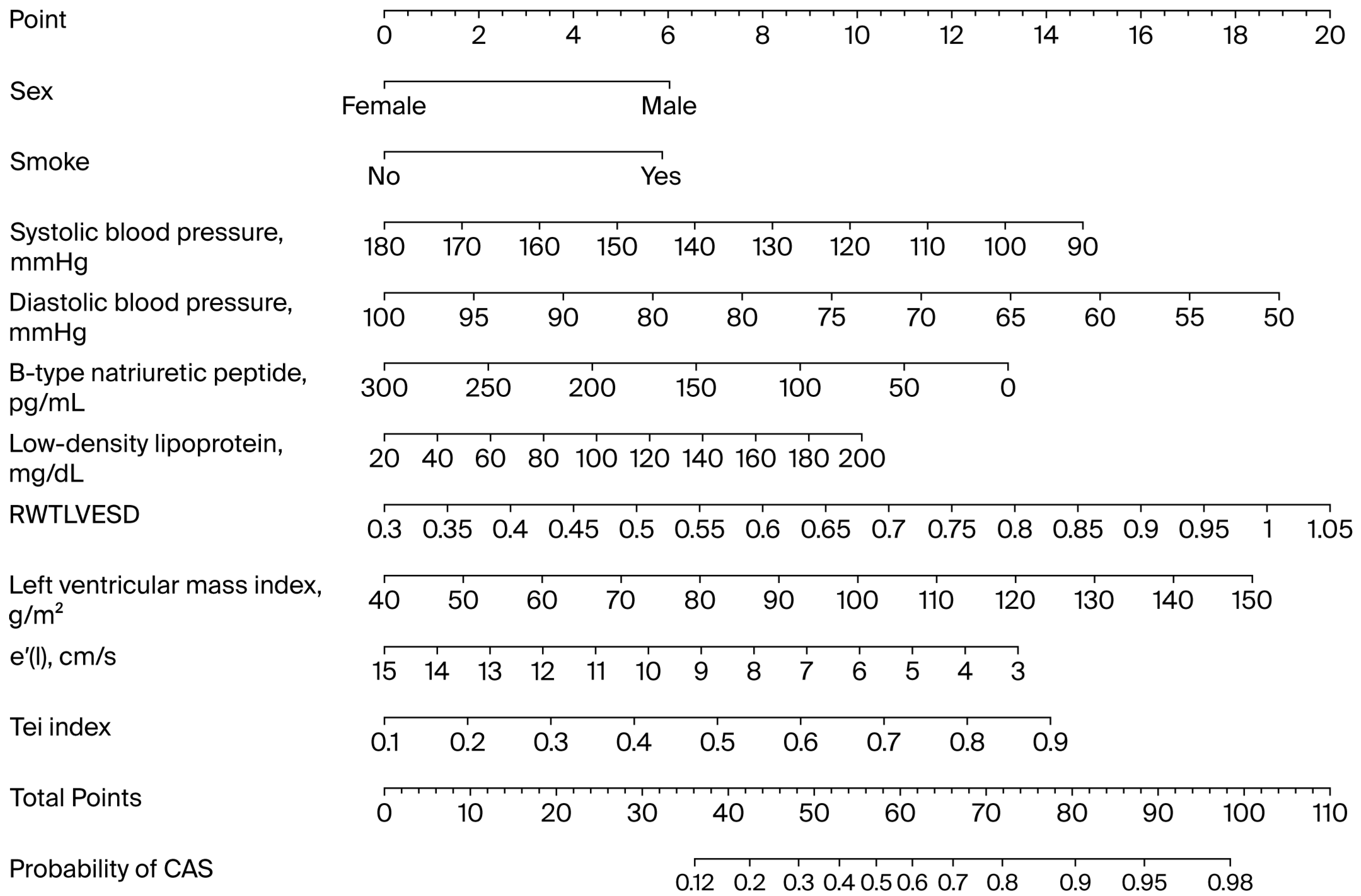
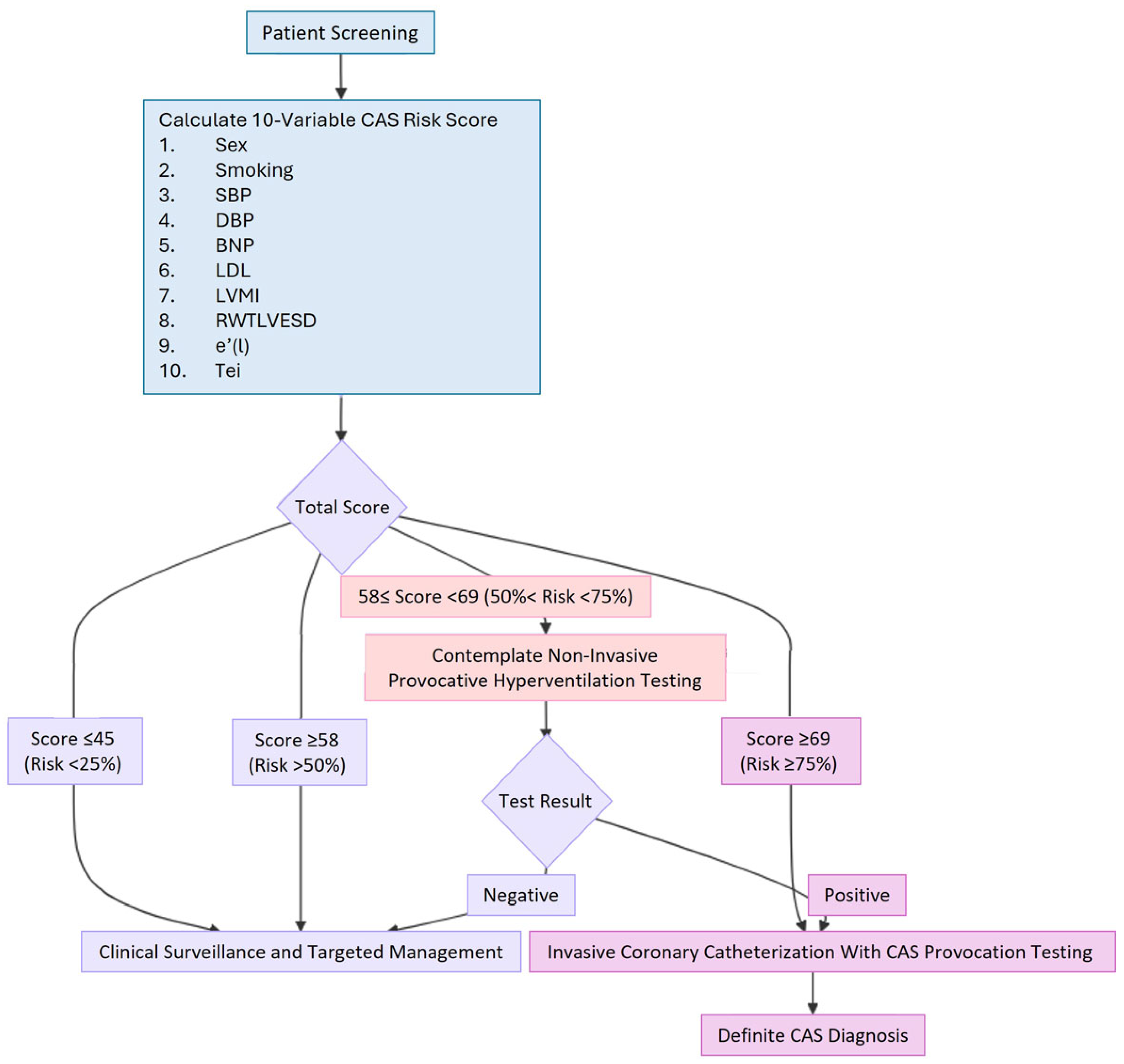
3.3. Clinical Use of the Prediction Model
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Girolamo, O.; Tavella, R.; Di Fiore, D.; Sheikh, A.; Pasupathy, S.; Ooi, E.L.; Marathe, J.A.; Zeitz, C.; Beltrame, J.F. Should the Right Coronary Artery Be Routinely Assessed During Provocative Spasm Testing? J. Clin. Med. 2025, 14, 1355. [Google Scholar] [CrossRef]
- Hung, M.Y.; Hsu, K.H.; Hung, M.J.; Cheng, C.W.; Cherng, W.J. Interactions among gender, age, hypertension and C-reactive protein in coronary vasospasm. Eur. J. Clin. Investig. 2010, 40, 1094–1103. [Google Scholar] [CrossRef] [PubMed]
- Hung, M.J.; Hu, P.; Hung, M.Y. Coronary artery spasm: Review and update. Int. J. Med. Sci. 2014, 11, 1161–1171. [Google Scholar] [CrossRef] [PubMed]
- Bitton, A.; Gaziano, T.A. The Framingham Heart Study’s impact on global risk assessment. Prog. Cardiovasc. Dis. 2010, 53, 68–78. [Google Scholar] [CrossRef]
- Lee, Y.C.; Hung, M.J.; Chen, T.H.; Mao, C.T.; Yeh, C.T.; Kounis, N.G.; Chen, I.Y.; Hu, P.; Hung, M.Y. Effects of statins in patients with coronary artery spasm: A nationwide population-based study. Clin. Transl. Sci. 2024, 17, e70087. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Qin, H.; Chen, R.; Liu, Q.; Liu, H.; Dong, S. A comprehensive clinical diagnostic score system for prediction of coronary artery spasm in patients with acute chest pain. Int. J. Cardiol. Heart Vasc. 2019, 22, 205–209. [Google Scholar] [CrossRef]
- Hung, M.J.; Mao, C.T.; Hung, M.Y.; Chen, T.H. Impact of Asthma on the Development of Coronary Vasospastic Angina: A Population-Based Cohort Study. Medicine 2015, 94, e1880. [Google Scholar] [CrossRef]
- Zellner, C.; Protter, A.A.; Ko, E.; Pothireddy, M.R.; DeMarco, T.; Hutchison, S.J.; Chou, T.M.; Chatterjee, K.; Sudhir, K. Coronary vasodilator effects of BNP: Mechanisms of action in coronary conductance and resistance arteries. Am. J. Physiol. 1999, 276, H1049–H1057. [Google Scholar] [CrossRef]
- Gohbara, M.; Iwahashi, N.; Okada, K.; Ogino, Y.; Hanajima, Y.; Kirigaya, J.; Minamimoto, Y.; Matsuzawa, Y.; Nitta, M.; Konishi, M.; et al. A Simple Risk Score to Differentiate Between Coronary Artery Obstruction and Coronary Artery Spasm of Patients With Acute Coronary Syndrome Without Persistent ST-Segment Elevation. Circ. J. 2022, 86, 1509–1518. [Google Scholar] [CrossRef]
- Bonow, R.O.; Vitale, D.F.; Bacharach, S.L.; Frederick, T.M.; Kent, K.M.; Green, M.V. Asynchronous left ventricular regional function and impaired global diastolic filling in patients with coronary artery disease: Reversal after coronary angioplasty. Circulation 1985, 71, 297–307. [Google Scholar] [CrossRef]
- Kirkpatrick, J.N.; Vannan, M.A.; Narula, J.; Lang, R.M. Echocardiography in heart failure: Applications, utility, and new horizons. J. Am. Coll. Cardiol. 2007, 50, 381–396. [Google Scholar] [CrossRef] [PubMed]
- Sekiya, M.; Funada, J.; Suzuki, J.; Watanabe, K.; Miyagawa, M.; Akutsu, H. The influence of left ventricular geometry on coronary vasomotion in patients with essential hypertension. Am. J. Hypertens. 2000, 13, 789–795. [Google Scholar] [CrossRef] [PubMed]
- Askari, A.T.; Brennan, M.L.; Zhou, X.; Drinko, J.; Morehead, A.; Thomas, J.D.; Topol, E.J.; Hazen, S.L.; Penn, M.S. Myeloperoxidase and plasminogen activator inhibitor 1 play a central role in ventricular remodeling after myocardial infarction. J. Exp. Med. 2003, 197, 615–624. [Google Scholar] [CrossRef] [PubMed]
- Wachtell, K.; Bella, J.N.; Rokkedal, J.; Palmieri, V.; Papademetriou, V.; Dahlöf, B.; Aalto, T.; Gerdts, E.; Devereux, R.B. Change in diastolic left ventricular filling after one year of antihypertensive treatment: The Losartan Intervention For Endpoint Reduction in Hypertension (LIFE) Study. Circulation 2002, 105, 1071–1076. [Google Scholar] [CrossRef]
- Ghali, J.K.; Liao, Y.; Cooper, R.S. Influence of left ventricular geometric patterns on prognosis in patients with or without coronary artery disease. J. Am. Coll. Cardiol. 1998, 31, 1635–1640. [Google Scholar] [CrossRef]
- Sharaf, B.L.; Williams, D.O.; Miele, N.J.; McMahon, R.P.; Stone, P.H.; Bjerregaard, P.; Davies, R.; Goldberg, A.D.; Parks, M.; Pepine, C.J.; et al. A detailed angiographic analysis of patients with ambulatory electrocardiographic ischemia: Results from the Asymptomatic Cardiac Ischemia Pilot (ACIP) study angiographic core laboratory. J. Am. Coll. Cardiol. 1997, 29, 78–84. [Google Scholar] [CrossRef]
- Miyao, Y.; Kugiyama, K.; Kawano, H.; Motoyama, T.; Ogawa, H.; Yoshimura, M.; Sakamoto, T.; Yasue, H. Diffuse intimal thickening of coronary arteries in patients with coronary spastic angina. J. Am. Coll. Cardiol. 2000, 36, 432–437. [Google Scholar] [CrossRef]
- Schiller, N.B.; Shah, P.M.; Crawford, M.; DeMaria, A.; Devereux, R.; Feigenbaum, H.; Gutgesell, H.; Reichek, N.; Sahn, D.; Schnittger, I.; et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J. Am. Soc. Echocardiogr. 1989, 2, 358–367. [Google Scholar] [CrossRef]
- Yao, G.H.; Zhang, M.; Yin, L.X.; Zhang, C.; Xu, M.J.; Deng, Y.; Liu, Y.; Deng, Y.B.; Ren, W.D.; Li, Z.A.; et al. Doppler Echocardiographic Measurements in Normal Chinese Adults (EMINCA): A prospective, nationwide, and multicentre study. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 512–522. [Google Scholar] [CrossRef]
- Konovalov, D.A.; Bajema, N.; Litow, B. Modified SIMPSON O(n3) algorithm for the full sibship reconstruction problem. Bioinformatics 2005, 21, 3912–3917. [Google Scholar] [CrossRef]
- Devereux, R.B.; Alonso, D.R.; Lutas, E.M.; Gottlieb, G.J.; Campo, E.; Sachs, I.; Reichek, N. Echocardiographic assessment of left ventricular hypertrophy: Comparison to necropsy findings. Am. J. Cardiol. 1986, 57, 450–458. [Google Scholar] [CrossRef]
- Sahn, D.J.; DeMaria, A.; Kisslo, J.; Weyman, A. Recommendations regarding quantitation in M-mode echocardiography: Results of a survey of echocardiographic measurements. Circulation 1978, 58, 1072–1083. [Google Scholar] [CrossRef] [PubMed]
- Reichek, N.; Devereux, R.B. Reliable estimation of peak left ventricular systolic pressure by M-mode echographic-determined end-diastolic relative wall thickness: Identification of severe valvular aortic stenosis in adult patients. Am. Heart J. 1982, 103, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Roman, M.J.; Pickering, T.G.; Schwartz, J.E.; Pini, R.; Devereux, R.B. Relation of arterial structure and function to left ventricular geometric patterns in hypertensive adults. J. Am. Coll. Cardiol. 1996, 28, 751–756. [Google Scholar] [CrossRef] [PubMed]
- Devereux, R.B.; Dahlof, B.; Levy, D.; Pfeffer, M.A. Comparison of enalapril versus nifedipine to decrease left ventricular hypertrophy in systemic hypertension (the PRESERVE trial). Am. J. Cardiol. 1996, 78, 61–65. [Google Scholar] [CrossRef]
- Wachtell, K.; Bella, J.N.; Liebson, P.R.; Gerdts, E.; Dahlöf, B.; Aalto, T.; Roman, M.J.; Papademetriou, V.; Ibsen, H.; Rokkedal, J.; et al. Impact of different partition values on prevalences of left ventricular hypertrophy and concentric geometry in a large hypertensive population: The LIFE study. Hypertension 2000, 35, 6–12. [Google Scholar] [CrossRef]
- Buakhamsri, A.; Popovic, Z.B.; Lin, J.; Lim, P.; Greenberg, N.L.; Borowski, A.G.; Tang, W.H.; Klein, A.L.; Lever, H.M.; Desai, M.Y.; et al. Impact of left ventricular volume/mass ratio on diastolic function. Eur. Heart J. 2009, 30, 1213–1221. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39.e14. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Bleeker, S.E.; Moll, H.A.; Grobbee, D.E.; Moons, K.G. Internal and external validation of predictive models: A simulation study of bias and precision in small samples. J. Clin. Epidemiol. 2003, 56, 441–447. [Google Scholar] [CrossRef]
- Sullivan, L.M.; Massaro, J.M.; D’Agostino, R.B., Sr. Presentation of multivariate data for clinical use: The Framingham Study risk score functions. Stat. Med. 2004, 23, 1631–1660. [Google Scholar] [CrossRef]
- Takagi, Y.; Takahashi, J.; Yasuda, S.; Miyata, S.; Tsunoda, R.; Ogata, Y.; Seki, A.; Sumiyoshi, T.; Matsui, M.; Goto, T.; et al. Prognostic stratification of patients with vasospastic angina: A comprehensive clinical risk score developed by the Japanese Coronary Spasm Association. J. Am. Coll. Cardiol. 2013, 62, 1144–1153. [Google Scholar] [CrossRef] [PubMed]
- Takaoka, K.; Yoshimura, M.; Ogawa, H.; Kugiyama, K.; Nakayama, M.; Shimasaki, Y.; Mizuno, Y.; Sakamoto, T.; Yasue, H. Comparison of the risk factors for coronary artery spasm with those for organic stenosis in a Japanese population: Role of cigarette smoking. Int. J. Cardiol. 2000, 72, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Corban, M.T.; Prasad, A.; Gulati, R.; Lerman, L.O.; Lerman, A. Sex-specific differences in coronary blood flow and flow velocity reserve in symptomatic patients with non-obstructive disease. EuroIntervention 2021, 16, 1079–1084. [Google Scholar] [CrossRef] [PubMed]
- Mehta, P.K.; Bess, C.; Elias-Smale, S.; Vaccarino, V.; Quyyumi, A.; Pepine, C.J.; Bairey Merz, C.N. Gender in cardiovascular medicine: Chest pain and coronary artery disease. Eur. Heart J. 2019, 40, 3819–3826. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Fearon, W.F.; Honda, Y.; Tanaka, S.; Pargaonkar, V.; Fitzgerald, P.J.; Lee, D.P.; Stefanick, M.; Yeung, A.C.; Tremmel, J.A. Effect of Sex Differences on Invasive Measures of Coronary Microvascular Dysfunction in Patients With Angina in the Absence of Obstructive Coronary Artery Disease. JACC Cardiovasc. Interv. 2015, 8, 1433–1441. [Google Scholar] [CrossRef]
- Kumar, S.; Mehta, P.K.; Eshtehardi, P.; Hung, O.Y.; Koh, J.S.; Kumar, A.; Al-Badri, A.; Rabah, R.; D’Souza, M.; Gupta, S.; et al. Functional coronary angiography in symptomatic patients with no obstructive coronary artery disease. Catheter. Cardiovasc. Interv. 2021, 98, 827–835. [Google Scholar] [CrossRef]
- Hoshino, M.; Hamaya, R.; Kanaji, Y.; Kanno, Y.; Hada, M.; Yamaguchi, M.; Sumino, Y.; Hirano, H.; Horie, T.; Usui, E.; et al. Sex Differences in Long-Term Outcomes in Patients With Deferred Revascularization Following Fractional Flow Reserve Assessment: International Collaboration Registry of Comprehensive Physiologic Evaluation. J. Am. Heart Assoc. 2020, 9, e014458. [Google Scholar] [CrossRef]
- Hung, M.Y.; Wu, Y.H.; Bamodu, O.A.; Chen, X.; Lin, Y.K.; Hu, P.; Chang, N.C.; Pang, J.S.; Yeh, C.T. Activation of the monocytic α7 nicotinic acetylcholine receptor modulates oxidative stress and inflammation-associated development of coronary artery spasm via a p38 MAP-kinase signaling-dependent pathway. Free. Radic. Biol. Med. 2018, 120, 266–276. [Google Scholar] [CrossRef]
- Hung, M.Y.; Hsu, K.H.; Hu, W.S.; Chang, N.C.; Huang, C.Y.; Hung, M.J. Gender-specific prognosis and risk impact of C-reactive protein, hemoglobin and platelet in the development of coronary spasm. Int. J. Med. Sci. 2013, 10, 255–264. [Google Scholar] [CrossRef]
- Sato, I.; Tomita, M.; Ohe, T.; Haze, K.; Shimomura, K. Age-related changes of clinical features and prevalences of coronary risk factors in Japanese patients with vasospastic angina. Chest 1986, 89, 12–19. [Google Scholar] [CrossRef]
- Sugiishi, M.; Takatsu, F. Cigarette smoking is a major risk factor for coronary spasm. Circulation 1993, 87, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.Y.; Rha, S.W.; Li, Y.J.; Poddar, K.L.; Jin, Z.; Minami, Y.; Saito, S.; Park, J.H.; Na, J.O.; Choi, C.U.; et al. Impact of hypertension on coronary artery spasm as assessed with intracoronary acetylcholine provocation test. J. Hum. Hypertens. 2010, 24, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Morita, S.; Mizuno, Y.; Harada, E.; Nakagawa, H.; Morikawa, Y.; Saito, Y.; Katoh, D.; Kashiwagi, Y.; Yoshimura, M.; Murohara, T.; et al. Differences and interactions between risk factors for coronary spasm and atherosclerosis—smoking, aging, inflammation, and blood pressure. Intern. Med. 2014, 53, 2663–2670. [Google Scholar] [CrossRef] [PubMed]
- Tschudi, M.R.; Lüscher, T.F. Age and hypertension differently affect coronary contractions to endothelin-1, serotonin, and angiotensins. Circulation 1995, 91, 2415–2422. [Google Scholar] [CrossRef]
- Fukuda, N.; Hu, W.Y.; Satoh, C.; Nakayama, M.; Kishioka, H.; Kubo, A.; Kanmatsuse, K. Contribution of synthetic phenotype on the enhanced angiotensin II-generating system in vascular smooth muscle cells from spontaneously hypertensive rats. J. Hypertens. 1999, 17, 1099–1107. [Google Scholar] [CrossRef]
- Clozel, J.P.; Sprecher, U. Influence of low perfusion pressure on effect of endothelin on coronary vascular bed. Am. J. Physiol. 1991, 260, H893–H901. [Google Scholar] [CrossRef]
- Stein, B.C.; Levin, R.I. Natriuretic peptides: Physiology, therapeutic potential, and risk stratification in ischemic heart disease. Am. Heart J. 1998, 135, 914–923. [Google Scholar] [CrossRef]
- Weber, M.; Mitrovic, V.; Hamm, C. B-type natriuretic peptide and N-terminal pro-B-type natriuretic peptide—Diagnostic role in stable coronary artery disease. Exp. Clin. Cardiol. 2006, 11, 99–101. [Google Scholar]
- Pandey, K.N. Molecular Signaling Mechanisms and Function of Natriuretic Peptide Receptor-A in the Pathophysiology of Cardiovascular Homeostasis. Front. Physiol. 2021, 12, 693099. [Google Scholar] [CrossRef]
- Kato, H.; Yasue, H.; Yoshimura, M.; Tanaka, H.; Miyao, Y.; Okumura, K.; Ogawa, H.; Nakao, K. Suppression of hyperventilation-induced attacks with infusion of B-type (brain) natriuretic peptide in patients with variant angina. Am. Heart J. 1994, 128, 1098–1104. [Google Scholar] [CrossRef]
- Kugiyama, K.; Sugiyama, S.; Soejima, H.; Kawano, H.; Sakamoto, T.; Takazoe, K.; Ogawa, H.; Doi, H.; Yasue, H. Increase in plasma levels of oxidized low-density lipoproteins in patients with coronary spastic angina. Atherosclerosis 2001, 154, 463–467. [Google Scholar] [CrossRef]
- Min, J.K.; Taylor, C.A.; Achenbach, S.; Koo, B.K.; Leipsic, J.; Nørgaard, B.L.; Pijls, N.J.; De Bruyne, B. Noninvasive Fractional Flow Reserve Derived From Coronary CT Angiography: Clinical Data and Scientific Principles. JACC Cardiovasc. Imaging 2015, 8, 1209–1222. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; Milani, R.V.; Ventura, H.O.; Cardenas, G.A.; Mehra, M.R.; Messerli, F.H. Disparate effects of left ventricular geometry and obesity on mortality in patients with preserved left ventricular ejection fraction. Am. J. Cardiol. 2007, 100, 1460–1464. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; Milani, R.V.; Ventura, H.O.; Messerli, F.H. Left ventricular geometry and mortality in patients 70 years of age with normal ejection fraction. Am. J. Cardiol. 2006, 98, 1396–1399. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.D.; Szczepaniak, L.S.; Wei, J.; Haftabaradaren, A.; Bharadwaj, M.; Sharif, B.; Mehta, P.; Zhang, X.; Thomson, L.E.; Berman, D.S.; et al. Diastolic dysfunction in women with signs and symptoms of ischemia in the absence of obstructive coronary artery disease: A hypothesis-generating study. Circ. Cardiovasc. Imaging 2014, 7, 510–516. [Google Scholar] [CrossRef]
- Park, S.M.; Wei, J.; Cook-Wiens, G.; Nelson, M.D.; Thomson, L.; Berman, D.; Handberg, E.; Petersen, J.; Anderson, D.; Pepine, C.J.; et al. Left ventricular concentric remodelling and functional impairment in women with ischaemia with no obstructive coronary artery disease and intermediate coronary flow reserve: A report from the WISE-CVD study. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 875–882. [Google Scholar] [CrossRef]
- Mogelvang, R.; Biering-Sørensen, T.; Jensen, J.S. Tissue Doppler echocardiography predicts acute myocardial infarction, heart failure, and cardiovascular death in the general population. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 1331–1337. [Google Scholar] [CrossRef]
- Turan, T.; Agac, M.T.; Aykan, A.Ç.; Kul, S.; Akyüz, A.R.; Gökdeniz, T.; Gül, İ.; Cengiz, E.; Boyacı, F.; Erkan, H.; et al. Usefulness of Heart-Type Fatty Acid-Binding Protein and Myocardial Performance Index for Early Detection of 5-Fluorouracil Cardiotoxicity. Angiology 2017, 68, 52–58. [Google Scholar] [CrossRef]
- Tei, C.; Nishimura, R.A.; Seward, J.B.; Tajik, A.J. Noninvasive Doppler-derived myocardial performance index: Correlation with simultaneous measurements of cardiac catheterization measurements. J. Am. Soc. Echocardiogr. 1997, 10, 169–178. [Google Scholar] [CrossRef]
- Fedele, D.; Cavallo, D.; Bodega, F.; Suma, N.; Canton, L.; Ciarlantini, M.; Ryabenko, K.; Amicone, S.; Marinelli, V.; Asta, C.; et al. Pathological findings at invasive assessment in MINOCA: A systematic review and meta-analysis. Heart 2025, 111, 291–299. [Google Scholar] [CrossRef]
- Chakrala, T.; Prakash, R.; Valdes, C.; Pepine, C.J.; Keeley, E.C. Circulating Biomarkers in Coronary Microvascular Dysfunction. J. Am. Heart Assoc. 2023, 12, e029341. [Google Scholar] [CrossRef]
- Skinner, J.S.; Smeeth, L.; Kendall, J.M.; Adams, P.C.; Timmis, A.; Chest Pain Guideline Development Group. NICE guidance. Chest pain of recent onset: Assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin. Heart 2010, 96, 974–978. [Google Scholar] [CrossRef]
- Dreisbach, J.G.; Nicol, E.D.; Roobottom, C.A.; Padley, S.; Roditi, G. Challenges in delivering computed tomography coronary angiography as the first-line test for stable chest pain. Heart 2018, 104, 921–927. [Google Scholar] [CrossRef]
- Popović, Z.B.; Thomas, J.D. Assessing observer variability: A user’s guide. Cardiovasc. Diagn. Ther. 2017, 7, 317–324. [Google Scholar] [CrossRef]
| Variable | Total (n = 913) | CAS (n = 645) | Control (n = 268) | p Value |
|---|---|---|---|---|
| Age, year | 56.4 ± 12.6 | 57.1 ± 11.9 | 54.8 ± 14.2 | 0.014 |
| Male | 453 (49.6) | 352 (54.6) | 101 (37.7) | <0.001 |
| Body mass index, kg/m2 | 26.1 ± 4.4 | 26.2 ± 4.2 | 25.8 ± 4.6 | 0.187 |
| Weight status | 0.097 | |||
| Normal/Lean (<23) | 226 (24.8) | 147 (22.8) | 79 (29.5) | |
| Overweight (23–24.9) | 174 (19.1) | 124 (19.2) | 50 (18.7) | |
| Obese (≥25) | 513 (56.2) | 374 (58.0) | 139 (51.9) | |
| Body surface area, m2 | 1.76 ± 0.20 | 1.77 ± 0.20 | 1.73 ± 0.21 | 0.009 |
| Smoke | 229 (25.1) | 184 (28.5) | 45 (16.8) | <0.001 |
| Diabetes mellitus | 109 (11.9) | 81 (12.6) | 28 (10.4) | 0.433 |
| Hypertension | 301 (33.0) | 220 (34.1) | 81 (30.2) | 0.279 |
| Systolic blood pressure, mmHg | 122.0 ± 18.9 | 120.2 ± 17.7 | 126.3 ± 20.9 | <0.001 |
| Diastolic blood pressure, mmHg | 74.3 ± 10.6 | 73.4 ± 10.3 | 76.6 ± 11.0 | <0.001 |
| Heart rate, bpm | 69.1 ± 11.5 | 68.7 ± 11.7 | 70.2 ± 11.1 | 0.072 |
| Serum creatinine, mg/dL | 0.86 ± 0.31 | 0.85 ± 0.27 | 0.87 ± 0.39 | 0.520 |
| Estimated glomerular filtration rate, mL/min/1.73 m2 | 91.6 ± 23.1 | 92.2 ± 22.0 | 90.1 ± 25.6 | 0.227 |
| Hemoglobin, g/dL | 13.6 ± 1.5 | 13.8 ± 1.5 | 13.3 ± 1.5 | <0.001 |
| Hematocrit, % | 40.1 ± 4.4 | 40.6 ± 4.2 | 39.0 ± 4.5 | <0.001 |
| Platelet counts, 109/L | 231.4 ± 58.7 | 232.0 ± 59.4 | 229.9 ± 57.1 | 0.618 |
| White blood cell count, 106/L | 6822.6 ± 1730.9 | 6874.0 ± 1790.0 | 6698.8 ± 1576.1 | 0.164 |
| Monocyte counts, 106/L | 495.2 ± 165.2 | 501.9 ± 168.4 | 479.2 ± 156.5 | 0.058 |
| B-type natriuretic peptide, pg/mL | 20.9 [9.0, 42.8] | 20.3 [7.6, 40.0] | 23.0 [10.3, 48.5] | 0.078 |
| High-sensitivity C-reactive protein, mg/L | 0.82 [0.40, 1.91] | 0.90 [0.40, 2.01] | 0.70 [0.39, 1.64] | 0.074 |
| High-sensitivity C-reactive protein, mg/L | 0.112 | |||
| ≤1 | 505 (55.3) | 344 (53.3) | 161 (60.1) | |
| 1–2.9 | 266 (29.1) | 192 (29.8) | 74 (27.6) | |
| ≥3 | 142 (15.6) | 109 (16.9) | 33 (12.3) | |
| Fasting glucose, mg/dL | 100.3 ± 19.5 | 101.0 ± 19.7 | 98.8 ± 18.8 | 0.118 |
| Glycated hemoglobin, % | 5.76 ± 0.66 | 5.79 ± 0.68 | 5.71 ± 0.61 | 0.112 |
| Total cholesterol, mg/dL | 170.6 ± 36.4 | 171.7 ± 36.5 | 168.0 ± 35.9 | 0.160 |
| Triglycerides, mg/dL | 122.4 ± 83.9 | 126.8 ± 86.9 | 112.0 ± 75.3 | 0.015 |
| High-density lipoprotein, mg/dL | 46.2 ± 12.8 | 45.6 ± 12.4 | 47.6 ± 13.7 | 0.033 |
| Low-density lipoprotein, mg/dL | 100.4 ± 31.2 | 101.6 ± 31.0 | 97.6 ± 31.4 | 0.075 |
| Echocardiography | ||||
| LV ejection fraction, % | 65.4 ± 6.9 | 65.6 ± 6.8 | 64.9 ± 7.3 | 0.154 |
| Fractional shortening | 0.36 ± 0.06 | 0.36 ± 0.06 | 0.36 ± 0.06 | 0.403 |
| Left atrium diameter, mm | 38.6 ± 6.1 | 38.8 ± 6.0 | 38.2 ± 6.2 | 0.159 |
| Interventricular septal thickness, mm | 9.18 ± 1.81 | 9.28 ± 1.74 | 8.95 ± 1.96 | 0.014 |
| LVEDD, mm | 44.4 ± 4.7 | 44.6 ± 4.6 | 44.1 ± 4.7 | 0.139 |
| LVESD, mm | 28.4 ± 4.2 | 28.4 ± 4.2 | 28.2 ± 4.1 | 0.406 |
| Left ventricular posterior wall, mm | 8.41 ± 1.55 | 8.63 ± 1.44 | 7.89 ± 1.66 | <0.001 |
| RWTLVEDD | 0.38 ± 0.08 | 0.39 ± 0.08 | 0.36 ± 0.08 | <0.001 |
| RWTLVESD | 0.60 ± 0.14 | 0.62 ± 0.13 | 0.57 ± 0.14 | <0.001 |
| LV mass, g | 131.3 ± 39.5 | 134.8 ± 37.9 | 122.8 ± 42.0 | <0.001 |
| LV mass index, g/m2 | 74.3 ± 19.4 | 76.0 ± 18.6 | 70.4 ± 20.9 | <0.001 |
| LV remodeling | 0.012 | |||
| Normal | 633 (69.3) | 429 (66.5) | 204 (76.1) | |
| Concentric remodeling | 239 (26.2) | 187 (29.0) | 52 (19.4) | |
| Concentric hypertrophy | 26 (2.8) | 20 (3.1) | 6 (2.2) | |
| Eccentric hypertrophy | 15 (1.6) | 9 (1.4) | 6 (2.2) | |
| Mitral inflow deceleration time, ms | 188.7 ± 34.6 | 189.9 ± 34.5 | 185.8 ± 34.9 | 0.100 |
| Isovolumic relaxation time, ms | 86.5 ± 12.6 | 87.3 ± 12.5 | 84.6 ± 12.7 | 0.003 |
| τ0l: LV relaxation time constant using lateral annulus, ms | 37.8 ± 6.8 | 38.4 ± 6.6 | 36.4 ± 7.1 | <0.001 |
| τ0m: LV relaxation time constant using medial annulus, ms | 40.4 ± 7.6 | 40.9 ± 7.3 | 39.3 ± 8.1 | 0.004 |
| E: Mitral inflow E-wave velocity, cm/s | 60.8 ± 15.5 | 59.5 ± 15.2 | 64.0 ± 15.7 | <0.001 |
| A: Mitral inflow A-wave velocity, cm/s | 59.1 ± 16.9 | 59.0 ± 16.2 | 59.3 ± 18.5 | 0.828 |
| E/A: Mitral inflow E/A ratio | 1.11 ± 0.44 | 1.08 ± 0.41 | 1.19 ± 0.51 | 0.001 |
| e′(l): Lateral mitral annular early diastolic velocity, cm/s | 7.95 ± 2.54 | 7.73 ± 2.41 | 8.47 ± 2.77 | <0.001 |
| a′(l): Lateral mitral annular late diastolic velocity, cm/s | 9.36 ± 2.26 | 9.28 ± 2.21 | 9.55 ± 2.37 | 0.103 |
| e′(m): Medial mitral annular early diastolic velocity, cm/s | 6.38 ± 1.93 | 6.27 ± 1.86 | 6.63 ± 2.08 | 0.010 |
| a′(m): Medial mitral annular late diastolic velocity, cm/s | 8.76 ± 1.72 | 8.76 ± 1.69 | 8.74 ± 1.77 | 0.863 |
| E/e′(l): Lateral mitral inflow E to e′ ratio | 8.25 ± 2.95 | 8.27 ± 2.89 | 8.20 ± 3.07 | 0.760 |
| E/e′(m): Medial mitral inflow E to e′ ratio | 10.20 ± 3.46 | 10.09 ± 3.28 | 10.46 ± 3.87 | 0.146 |
| Tei index | 0.48 ± 0.16 | 0.50 ± 0.15 | 0.45 ± 0.15 | <0.001 |
| Predictor | Odds Ratio (95% CI) | p Value |
|---|---|---|
| Age, per 10 years | 1.01 (1.003–1.03) | 0.014 |
| Male sex | 1.99 (1.48–2.66) | <0.001 |
| Body mass index, per 5 kg/m2 | 1.12 (0.95–1.32) | 0.187 |
| Weight status | ||
| Normal/Lean (<23 kg/m2) | Reference | – |
| Overweight (23–24.9 kg/m2) | 1.33 (0.87–2.04) | 0.188 |
| Obese (≥25 kg/m2) | 1.45 (1.03–2.02) | 0.031 |
| Body surface area, per 0.1 m2 | 1.10 (1.02–1.18) | 0.009 |
| Smoke | 1.98 (1.38–2.84) | <0.001 |
| Diabetes mellitus | 1.23 (0.78–1.94) | 0.371 |
| Hypertension | 1.20 (0.88–1.63) | 0.256 |
| Systolic blood pressure, per 10 mmHg | 0.85 (0.78–0.91) | <0.001 |
| Diastolic blood pressure, per 10 mmHg | 0.75 (0.65–0.86) | <0.001 |
| Heart rate, per 5 bpm | 0.95 (0.89–1.01) | 0.073 |
| Serum creatinine, per 0.1 mg/dL | 0.99 (0.94–1.03) | 0.521 |
| eGFR, per 10 mL/min/1.73 m2 | 1.04 (0.98–1.11) | 0.227 |
| Hemoglobin, per 1 g/dL | 1.23 (1.12–1.36) | <0.001 |
| Hematocrit, per 5% | 1.50 (1.27–1.77) | <0.001 |
| Platelets, per 1012/L | 1.001 (0.998–1.003) | 0.618 |
| WBC, per 109/L | 1.06 (0.98–1.15) | 0.164 |
| Monocytes, per 109/L | 1.09 (0.997–1.19) | 0.059 |
| B-type natriuretic peptide, per 1 log unit | 0.97 (0.95–0.999) | 0.041 |
| hs-CRP, mg/L | 1.003 (0.99–1.02) | 0.765 |
| High-sensitivity C-reactive protein, mg/L | ||
| ≤1 | Reference | – |
| 1–2.9 | 1.21 (0.88–1.68) | 0.245 |
| ≥3 | 1.55 (1.003–2.38) | 0.048 |
| Fasting glucose, per 10 mg/dL | 1.06 (0.98–1.15) | 0.120 |
| Glycated hemoglobin, per 0.1% | 1.02 (0.996–1.04) | 0.113 |
| Total cholesterol, per 10 mg/dL | 1.03 (0.99–1.07) | 0.160 |
| Triglycerides, per 10 mg/dL | 1.02 (1.004–1.05) | 0.016 |
| High-density lipoprotein, per 10 mg/dL | 0.89 (0.80–0.99) | 0.034 |
| Low-density lipoprotein, per 10 mg/dL | 1.04 (0.996–1.09) | 0.076 |
| LV ejection fraction, per 5% | 1.08 (0.97–1.19) | 0.154 |
| Fractional shortening, per 10% | 1.10 (0.88–1.38) | 0.402 |
| Left atrium diameter, per 5 mm | 1.09 (0.97–1.22) | 0.159 |
| Interventricular septal thickness, per 1 mm | 1.11 (1.02–1.20) | 0.014 |
| LVEDD, per 1 mm | 1.02 (0.99–1.06) | 0.139 |
| LVESD, per 1 mm | 1.02 (0.98–1.05) | 0.406 |
| Left ventricular posterior wall, per 1 mm | 1.41 (1.27–1.57) | <0.001 |
| RWTLVEDD, per 0.1 | 1.66 (1.37–2.03) | <0.001 |
| RWTLVESD, per 0.1 | 1.34 (1.19–1.50) | <0.001 |
| LV mass, per 10 g | 1.09 (1.05–1.13) | <0.001 |
| LV mass index, per 10 g/m2 | 1.18 (1.08–1.27) | <0.001 |
| LV remodeling | ||
| Normal | ref | ref |
| Concentric remodeling | 1.71 (1.21–2.43) | 0.003 |
| Concentric hypertrophy | 1.59 (0.63–4.01) | 0.330 |
| Eccentric hypertrophy | 0.71 (0.25–2.03) | 0.527 |
| Mitral inflow deceleration time, per 10 ms | 1.04 (0.99–1.08) | 0.100 |
| Isovolumic relaxation time, per 10 ms | 1.19 (1.06–1.34) | 0.003 |
| τ0l, per 10 ms | 1.55 (1.25–1.94) | <0.001 |
| τ0m, per 10 ms | 1.33 (1.09–1.62) | 0.005 |
| E, per 10 m/s | 0.83 (0.76–0.91) | <0.001 |
| A, per 10 m/s | 0.99 (0.91–1.08) | 0.828 |
| E/A, per 0.1 | 0.95 (0.92–0.98) | 0.001 |
| e′(l), per 0.1 m/s | 0.99 (0.98–0.99) | <0.001 |
| a′(l), per 0.1 m/s | 0.995 (0.99–1.001) | 0.103 |
| e′(m), per 0.1 m/s | 0.99 (0.98–0.998) | 0.011 |
| a′(m), per 0.1 m/s | 1.001 (0.99–1.01) | 0.863 |
| E/e′(l), per 0.1 | 1.001 (0.996–1.01) | 0.761 |
| E/e′(m), per 0.1 | 0.997 (0.99–1.001) | 0.146 |
| Tei index, per 0.1 | 1.22 (1.11–1.34) | <0.001 |
| Predictor | Estimate | Odds Ratio (95% CI) | p Value |
|---|---|---|---|
| Intercept | 2.13 | - | - |
| Male sex | 0.57 | 1.76 (1.26–2.47) | 0.001 |
| Smoke | 0.56 | 1.74 (1.16–2.62) | 0.008 |
| Systolic blood pressure, per 10 mmHg | −0.15 | 0.86 (0.78–0.95) | 0.002 |
| Diastolic blood pressure, per 10 mmHg | −0.36 | 0.70 (0.59–0.84) | <0.001 |
| B-type natriuretic peptide, per 10 pg/mL | −0.04 | 0.96 (0.93–0.99) | 0.016 |
| Low-density lipoprotein, per 10 mg/dL | 0.05 | 1.05 (1.001–1.11) | 0.046 |
| RWTLVESD, per 0.1 | 0.25 | 1.29 (1.14–1.46) | <0.001 |
| Left ventricular mass index, per 10 g/m2 | 0.16 | 1.17 (1.06–1.29) | 0.002 |
| e′(l), per 0.1 m/s | −0.01 | 0.99 (0.98–0.996) | 0.003 |
| Tei index, per 0.1 | 0.17 | 1.18 (1.06–1.32) | 0.003 |
| Point Values for Each Variable | Summation of Points | ||||
|---|---|---|---|---|---|
| Variable | Point | Variable | Point | Total Points | Probability of CAS |
| Sex | RWTLVESD | 36 | 0.12 | ||
| Female | 0 | <0.35 | 0 | 37 | 0.13 |
| Male | 6 | 0.35–0.39 | 1 | 38 | 0.14 |
| Smoke | 0.40–0.44 | 3 | 39 | 0.15 | |
| No | 0 | 0.45–0.49 | 4 | 40 | 0.16 |
| Yes | 6 | 0.50–0.54 | 5 | 41 | 0.18 |
| SBP, mmHg | 0.55–0.59 | 7 | 42 | 0.19 | |
| <100 | 15 | 0.60–0.64 | 8 | 43 | 0.21 |
| 100–109 | 13 | 0.65–0.69 | 9 | 44 | 0.22 |
| 110–119 | 11 | 0.70–0.74 | 11 | 45 | 0.24 |
| 120–129 | 10 | 0.75–0.79 | 12 | 46 | 0.26 |
| 130–139 | 8 | 0.80–0.84 | 13 | 47 | 0.27 |
| 140–149 | 7 | 0.85–0.89 | 15 | 48 | 0.29 |
| 150–159 | 5 | 0.90–0.94 | 16 | 49 | 0.31 |
| 160–169 | 3 | 0.95–0.99 | 17 | 50 | 0.33 |
| 170–179 | 2 | 1–1.04 | 19 | 51 | 0.35 |
| ≥180 | 0 | ≥1.05 | 20 | 52 | 0.38 |
| DBP, mmHg | LVMI, g/m2 | 53 | 0.40 | ||
| <55 | 19 | <50 | 0 | 54 | 0.42 |
| 55–59 | 17 | 50–59 | 2 | 55 | 0.44 |
| 60–64 | 15 | 60–69 | 3 | 56 | 0.47 |
| 65–69 | 13 | 70–79 | 5 | 57 | 0.49 |
| 70–74 | 11 | 80–89 | 7 | 58 | 0.51 |
| 75–79 | 9 | 90–99 | 8 | 59 | 0.54 |
| 80–84 | 8 | 100–109 | 10 | 60 | 0.56 |
| 85–89 | 6 | 110–119 | 12 | 61 | 0.58 |
| 90–94 | 4 | 120–129 | 13 | 62 | 0.61 |
| 95–99 | 2 | 130–139 | 15 | 63 | 0.63 |
| ≥100 | 0 | 140–149 | 17 | 64 | 0.65 |
| BNP, pg/mL | ≥150 | 18 | 65 | 0.67 | |
| <50 | 13 | e′(l), cm/s | 66 | 0.69 | |
| 50–99 | 11 | 3 | 13 | 67 | 0.71 |
| 100–149 | 9 | 4 | 12 | 68 | 0.73 |
| 150–199 | 7 | 5 | 11 | 69 | 0.75 |
| 200–249 | 4 | 6 | 10 | 70 | 0.77 |
| 250–299 | 2 | 7 | 9 | 71 | 0.78 |
| ≥300 | 0 | 8 | 8 | 72 | 0.80 |
| LDL, mg/dL | 9 | 7 | 73 | 0.81 | |
| <30 | 0 | 10 | 6 | 74 | 0.83 |
| 31–40 | 1 | 11 | 4 | 75 | 0.84 |
| 41–60 | 2 | 12 | 3 | 76 | 0.85 |
| 61–80 | 3 | 13 | 2 | 77 | 0.87 |
| 81–100 | 4 | 14 | 1 | 78 | 0.88 |
| 101–120 | 6 | 15 | 0 | 79 | 0.89 |
| 121–140 | 7 | Tei index | 80 | 0.90 | |
| 141–160 | 8 | <0.2 | 0 | 82 | 0.91 |
| 161–180 | 9 | 0.2 | 2 | 83 | 0.92 |
| ≥180 | 10 | 0.3 | 4 | 85 | 0.93 |
| 0.4 | 5 | 86 | 0.94 | ||
| 0.5 | 7 | 88 | 0.95 | ||
| 0.6 | 9 | 91 | 0.96 | ||
| 0.7 | 11 | 94 | 0.97 | ||
| 0.8 | 12 | 98 | 0.98 | ||
| >0.8 | 14 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.-C.; Chen, I.Y.; Hung, M.-J.; Yeh, C.-T.; Kounis, N.G.; Hu, P.; Hung, M.-Y. Prediction of Coronary Artery Spasm in Patients Without Obstructive Coronary Artery Disease Using a Comprehensive Clinical, Laboratory and Echocardiographic Risk Score. J. Clin. Med. 2025, 14, 8721. https://doi.org/10.3390/jcm14248721
Lee Y-C, Chen IY, Hung M-J, Yeh C-T, Kounis NG, Hu P, Hung M-Y. Prediction of Coronary Artery Spasm in Patients Without Obstructive Coronary Artery Disease Using a Comprehensive Clinical, Laboratory and Echocardiographic Risk Score. Journal of Clinical Medicine. 2025; 14(24):8721. https://doi.org/10.3390/jcm14248721
Chicago/Turabian StyleLee, Yu-Ching, Ian Y. Chen, Ming-Jui Hung, Chi-Tai Yeh, Nicholas G. Kounis, Patrick Hu, and Ming-Yow Hung. 2025. "Prediction of Coronary Artery Spasm in Patients Without Obstructive Coronary Artery Disease Using a Comprehensive Clinical, Laboratory and Echocardiographic Risk Score" Journal of Clinical Medicine 14, no. 24: 8721. https://doi.org/10.3390/jcm14248721
APA StyleLee, Y.-C., Chen, I. Y., Hung, M.-J., Yeh, C.-T., Kounis, N. G., Hu, P., & Hung, M.-Y. (2025). Prediction of Coronary Artery Spasm in Patients Without Obstructive Coronary Artery Disease Using a Comprehensive Clinical, Laboratory and Echocardiographic Risk Score. Journal of Clinical Medicine, 14(24), 8721. https://doi.org/10.3390/jcm14248721










