Hybrid Tightrope–PEEK Dual Fixation for Distal Biceps Tendon Reinsertion in High-Performance Athletes: A Prospective Case Series
Abstract
1. Introduction
2. Materials and Methods
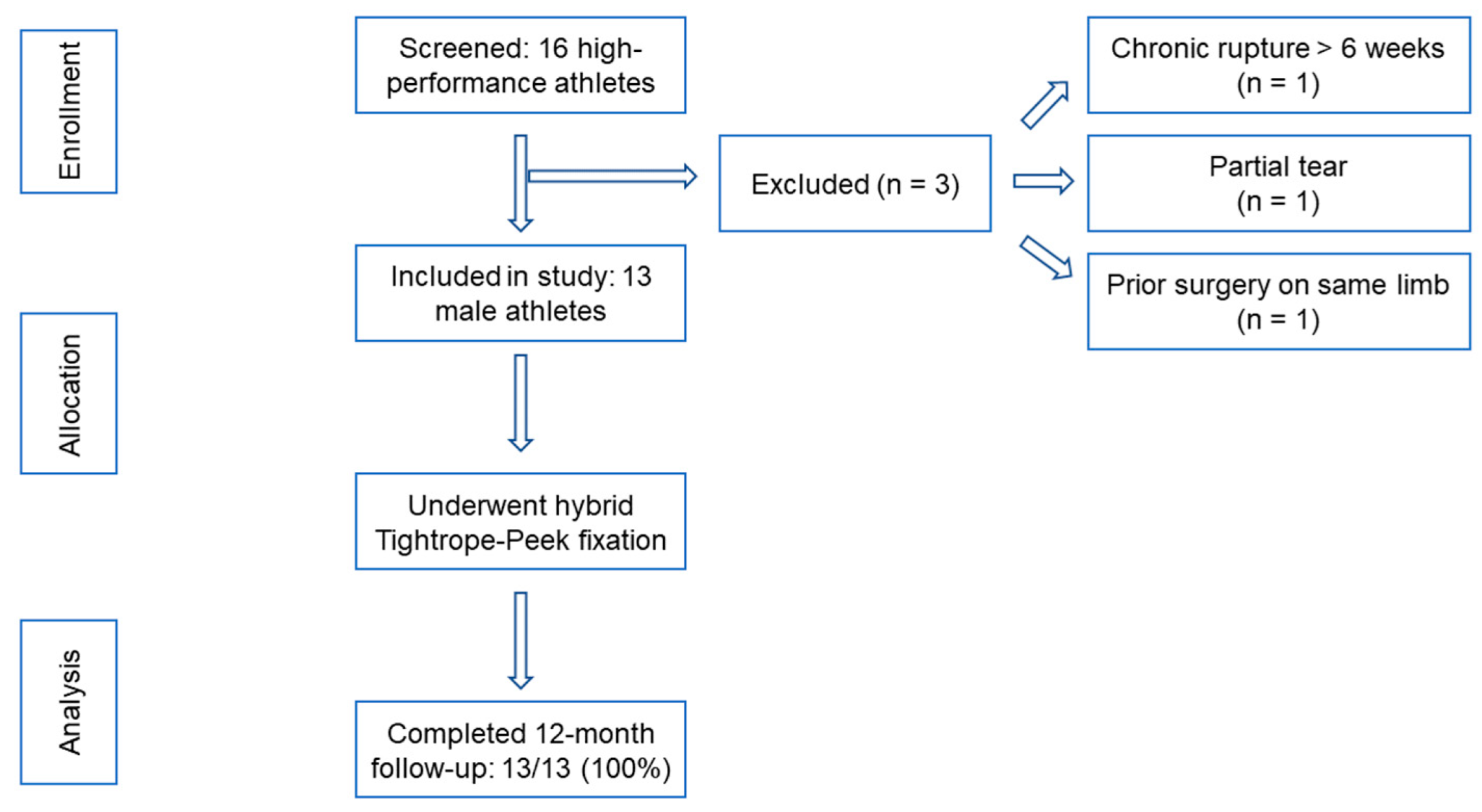
2.1. Study Design and Patient Selection
2.2. Participant Characteristics
2.3. Ethical Considerations
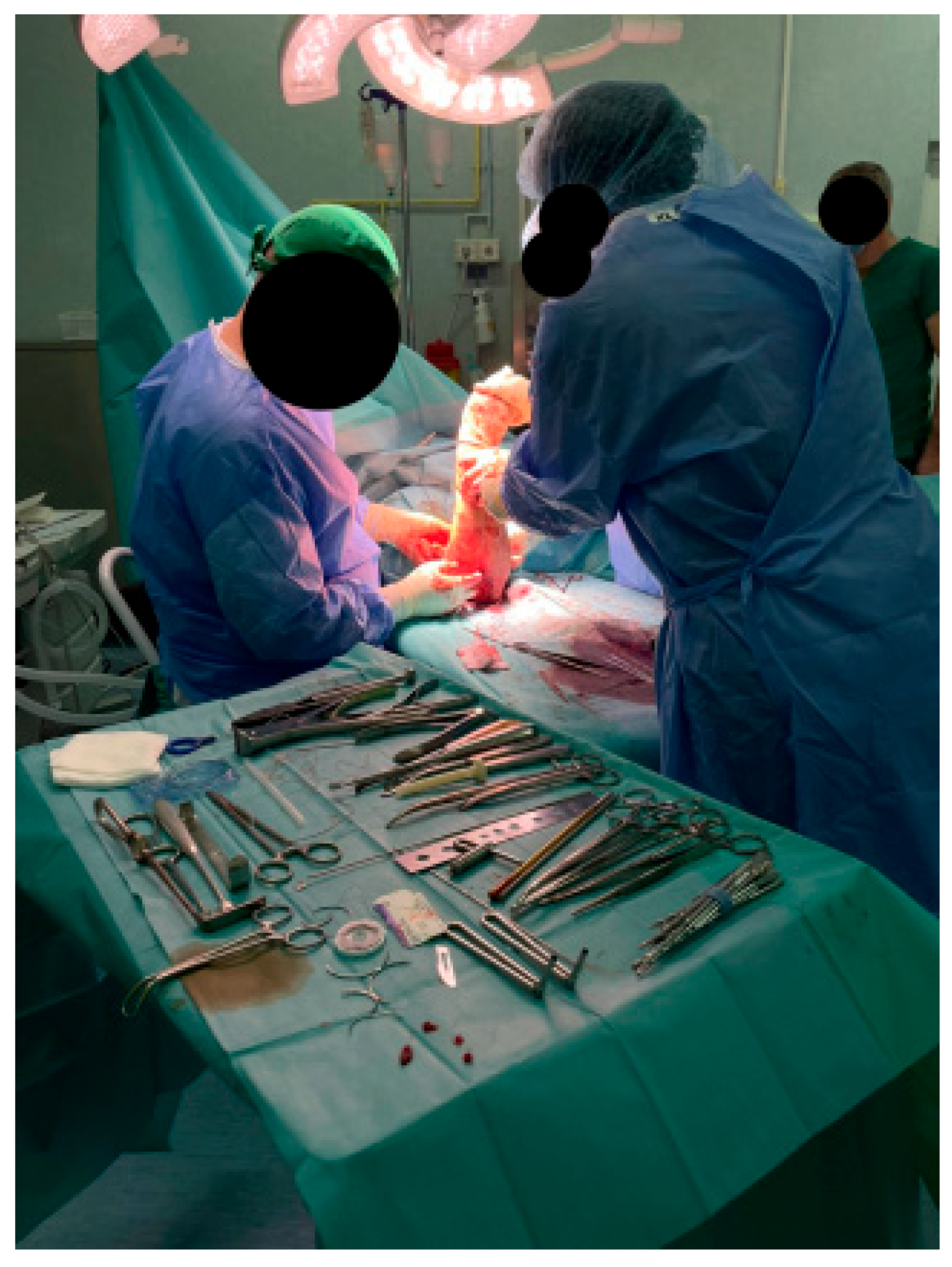
2.4. Surgical Technique and Intraoperative Technique
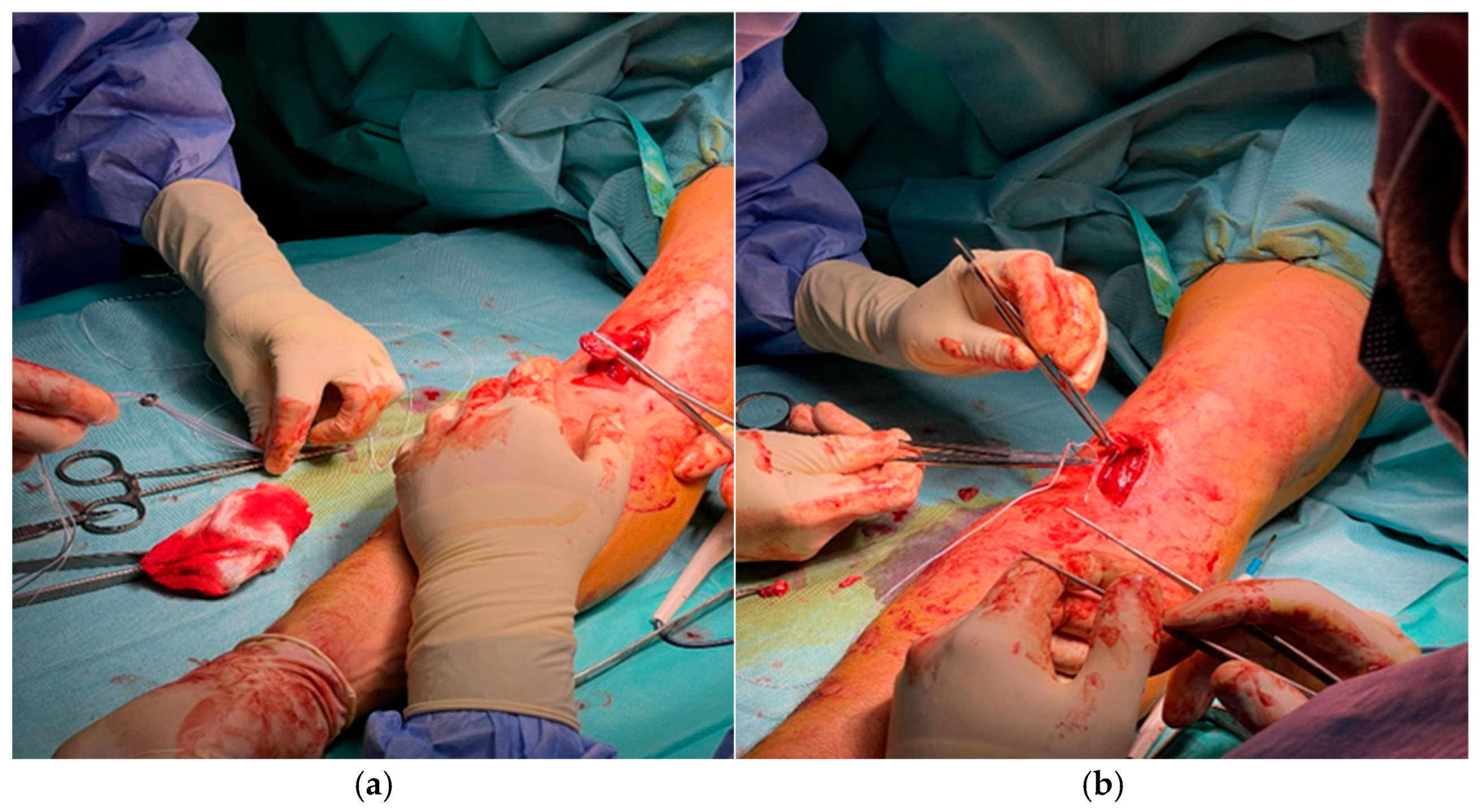
2.4.1. Exposure and Identification
2.4.2. Preparation of the Bone Bed
2.4.3. Tendon Preparation
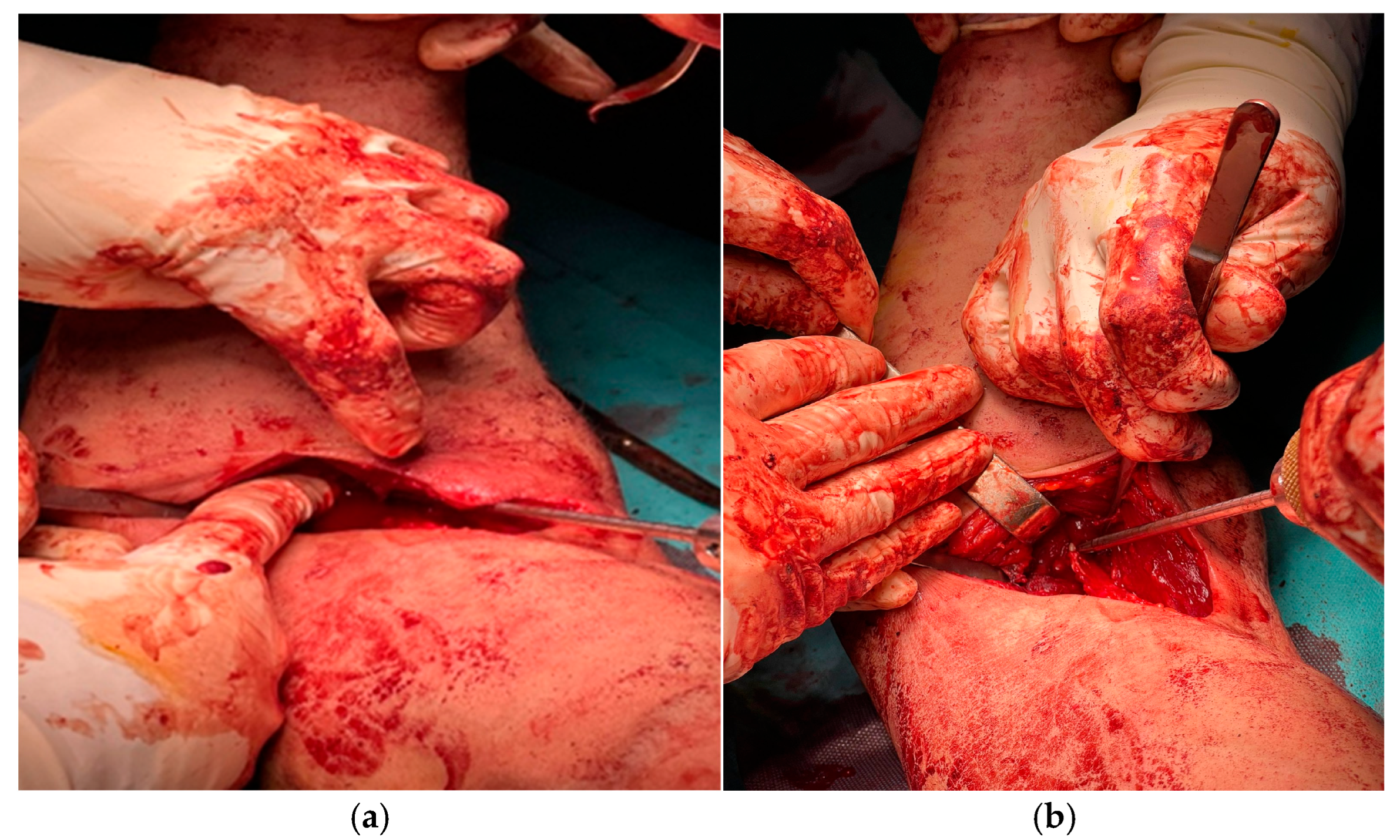
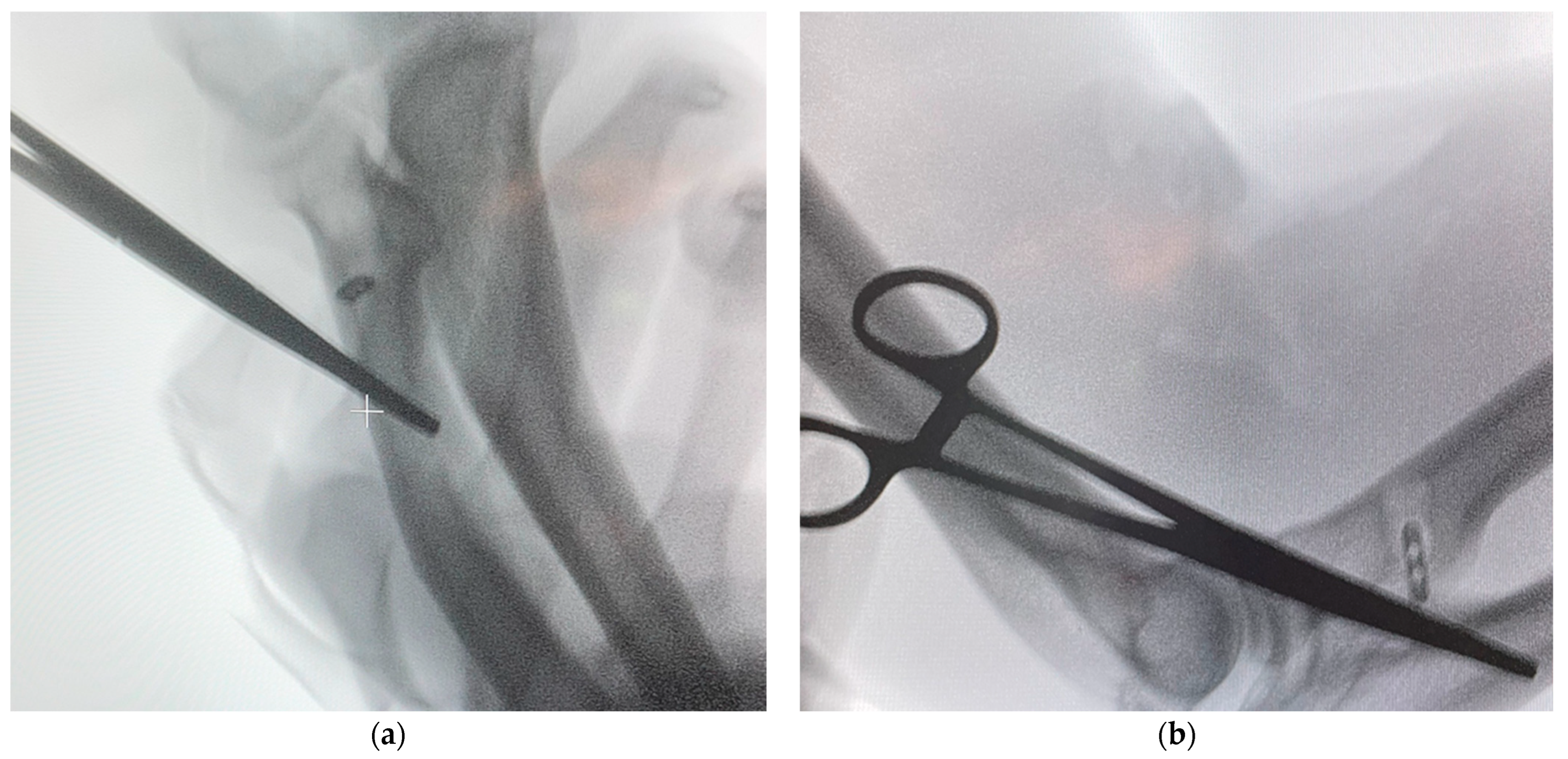
2.4.4. Dual Fixation Procedure
2.4.5. Intraoperative Evaluation
2.4.6. Closure and Immediate Postoperative Status
2.5. Postoperative Protocol and Rehabilitation
2.6. Clinical and Functional Evaluation
- Functional outcome: assessed using two validated instruments:
- Muscle strength: isometric elbow flexion and forearm supination strength were measured bilaterally using a handheld dynamometer, following standardized upper-limb strength-testing protocols [36,37]. Strength values were recorded as absolute measurements (kg or N) and as a percentage of the contralateral, non-injured side.
- Esthetic appearance: assessed through observation of biceps contour symmetry, the presence or absence of Popeye deformity, and overall cosmetic satisfaction rated by the patient using a 5-point Likert scale (1 = very poor, 5 = excellent).
- Patient satisfaction: evaluated using a 5-point Likert scale (1 = poor, 5 = excellent).
2.7. Statistical Analysis
3. Results
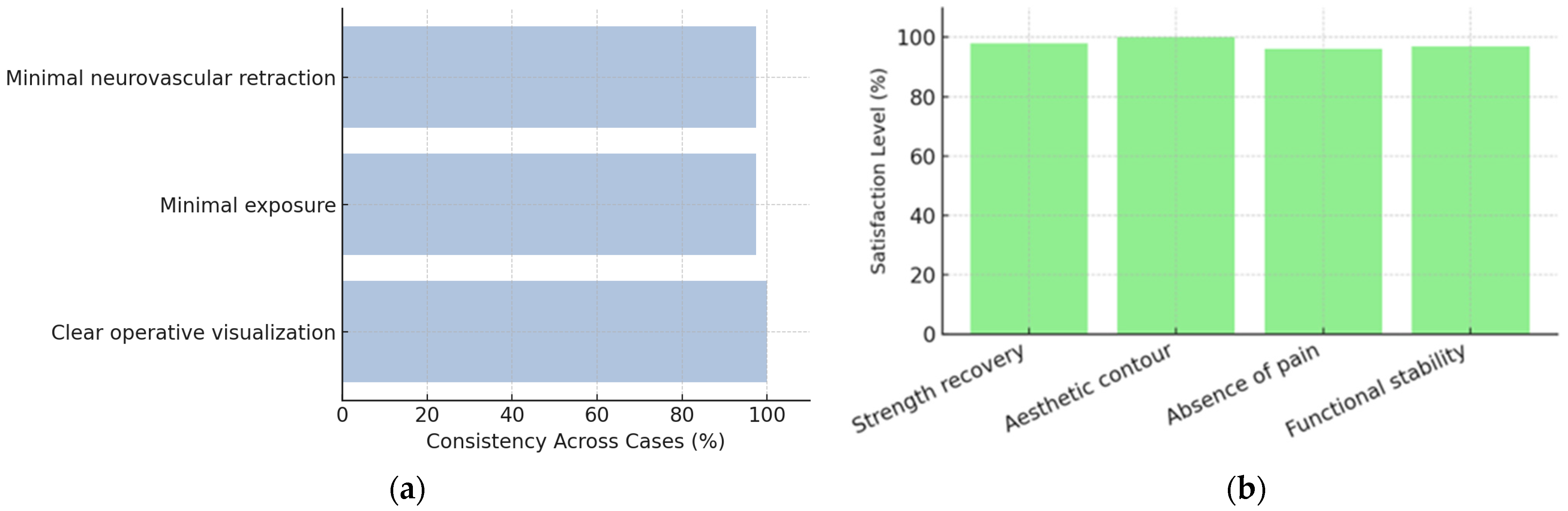
3.1. Intraoperative Findings and Fixation Stability
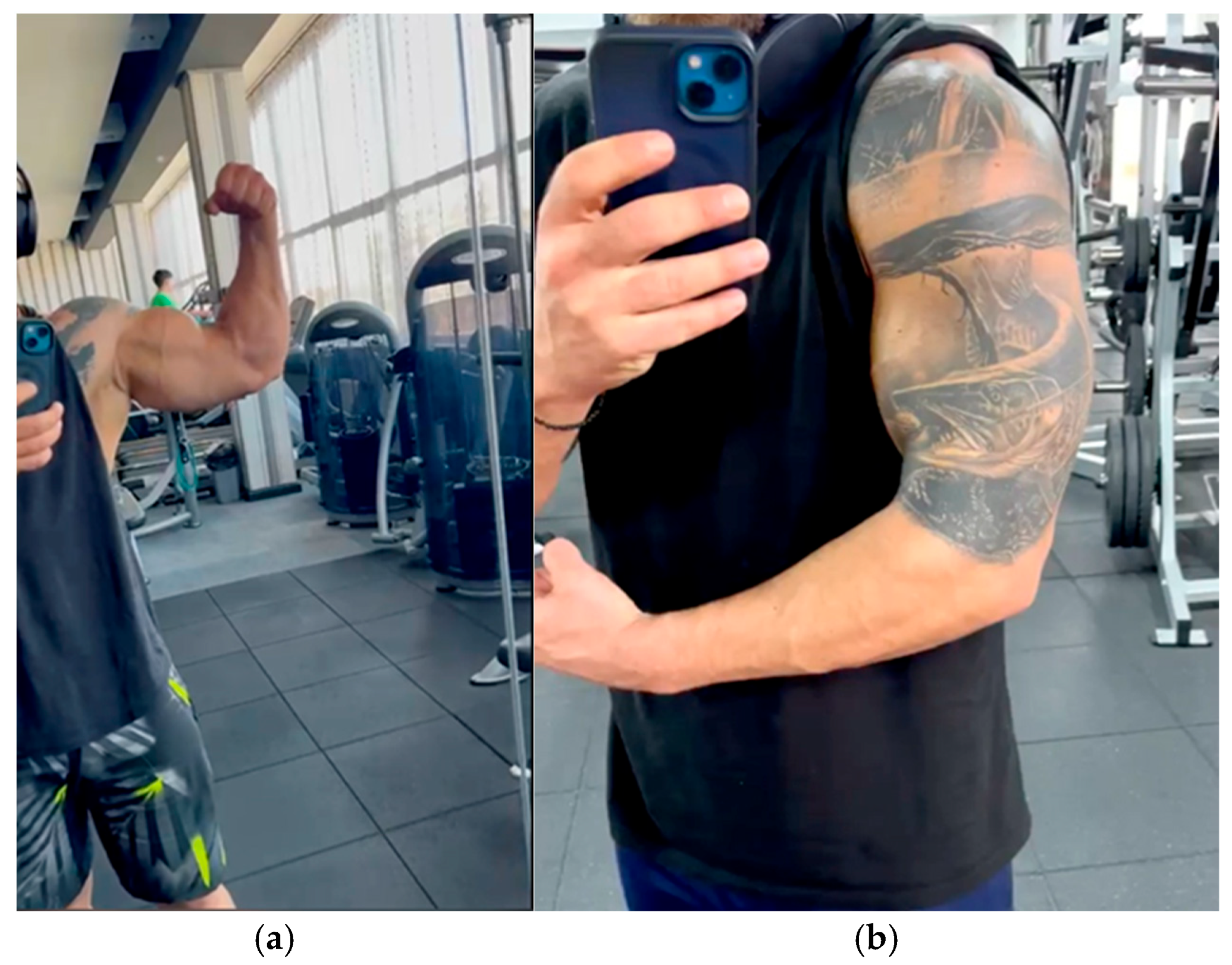
3.2. Postoperative Recovery and Visual Outcomes
3.3. Clinical and Functional Evaluation
- Pain (VAS). VAS scores decreased rapidly during follow-up, from moderate pain in the early postoperative period to complete absence of pain at 3, 6, and 12 months (Table 4). A Friedman test demonstrated a statistically significant reduction in pain across time points (χ2(3) = 36.8, p < 0.001, Kendall’s W = 0.71). Post hoc Dunn–Bonferroni comparisons confirmed significant decreases between early follow-up (6 weeks) and all subsequent evaluations.
- MEPS. MEPS values improved from “good–excellent” at 6 weeks (mean 90 ± 5) to almost maximal scores at 3, 6, and 12 months (96 ± 3, 98 ± 2, and 99 ± 1, respectively). Repeated measures ANOVA revealed a significant overall time effect (F(1.9, 22.8) = 54.2, p < 0.001, partial η2 = 0.82), with post hoc Bonferroni tests showing significant improvements between 6 weeks and 3 months, and a further increase between 3 and 6 months.
- QuickDASH. QuickDASH scores decreased from mild disability at 6 weeks (12 ± 3) to negligible functional limitation at 3, 6, and 12 months (6 ± 2, 3 ± 1, and 2 ± 1, respectively). A Friedman test confirmed a significant reduction over time (χ2(3) = 28.4, p < 0.001, Kendall’s W = 0.73), with post hoc analysis indicating significant differences between each follow-up interval.
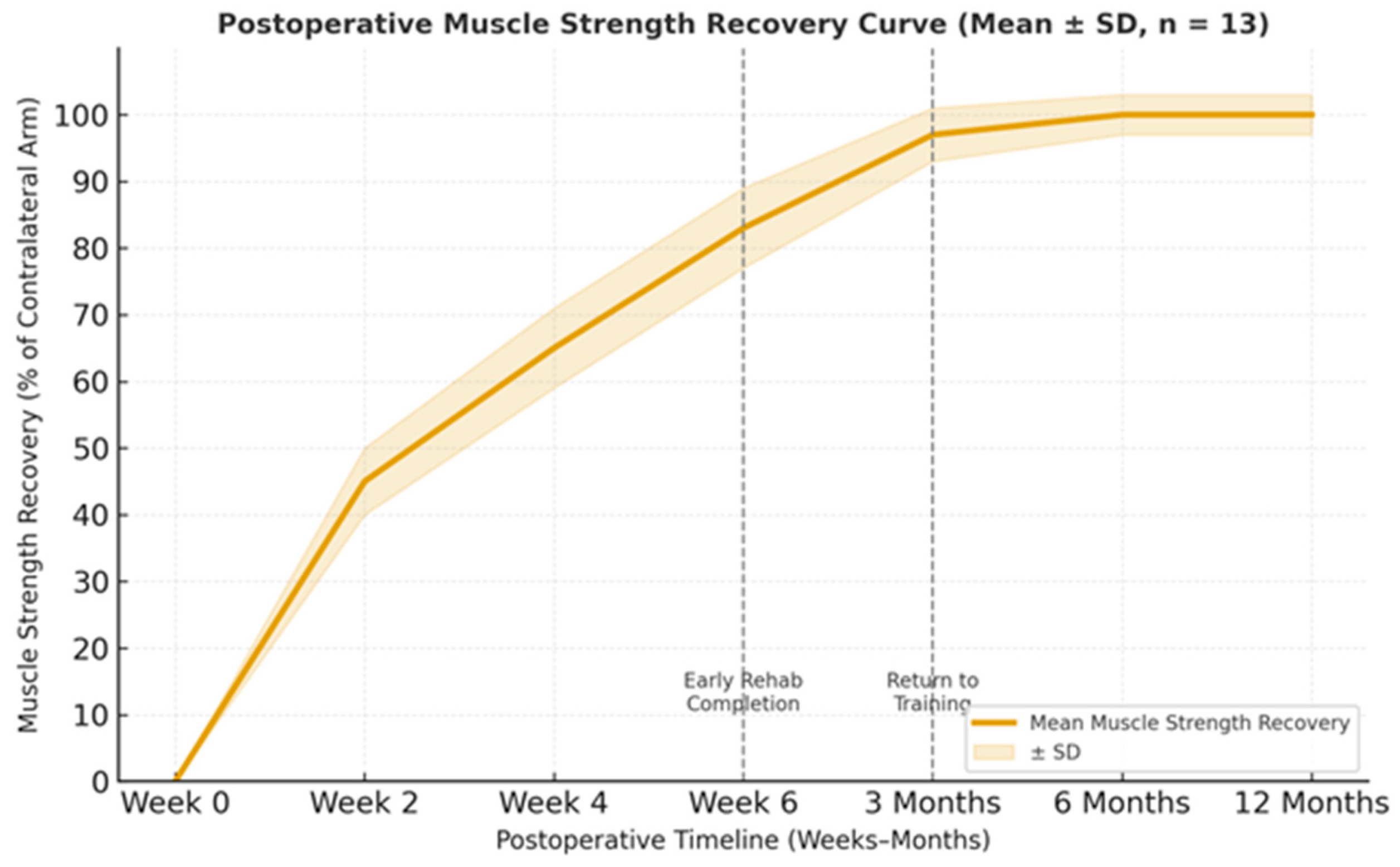
- Strength recovery. Isometric flexion and supination strength recovered from 83 ± 6% of the contralateral limb at 6 weeks to 97 ± 4% at 3 months, reaching 100% and remaining stable at 6 and 12 months. Repeated measures ANOVA showed a significant time effect for strength recovery (F(1.8, 21.6) = 48.9, p < 0.001, partial η2 = 0.80), with post hoc tests demonstrating that strength at 6 weeks was significantly lower than at 3 and 6 months.
3.4. Case-Based Observations and Clinical Evolution
3.4.1. Immediate Postoperative Phase
3.4.2. Rehabilitation and Functional Recovery
- Early Mobilization (Days 3–14): Daily supervised passive elbow flexion within a 30–110° range was initiated. All patients tolerated movement without pain, instability, or mechanical symptoms.
- Intermediate Phase (Weeks 2–6): Controlled active motion exercises were introduced, emphasizing progressive strengthening of elbow flexion and forearm supination. Isometric contractions were performed in a seated position to minimize gravitational load. By the end of this phase, all patients demonstrated symmetric joint mobility relative to the contralateral limb.
- Late Recovery (After Week 6): Graduated resistive training was progressively reintroduced, focusing on functional strength restoration rather than maximal load. Return to occupational and athletic activities occurred between 8 and 12 weeks, depending on baseline conditioning and physiotherapy adherence.
3.4.3. Esthetic and Functional Outcomes
3.4.4. Clinical Stability and Complications
3.4.5. Comparative Remarks and Procedural Insights
3.5. Functional Scores and Return-to-Play Assessment
4. Discussion
4.1. Mechanical Stability and Early Mobilization
4.2. Functional Recovery and Esthetic Outcome
4.3. Safety, Reproducibility, and Technical Feasibility
4.4. Clinical Relevance
4.5. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MEPS | Mayo Elbow Performance Score |
| QuickDASH | Disabilities of the Arm, Shoulder and Hand questionnaire |
| VAS | Visual A nalog Scale |
| PEEK | Polyether Ether Ketone |
| BMI | Body Mass Index |
References
- Caekebeke, P.; Duerinckx, J.; van Riet, R. Acute complete and partial distal biceps tendon ruptures: What have we learned? EFORT Open Rev. 2021, 6, 956–965. [Google Scholar] [CrossRef] [PubMed]
- Jaschke, M.; Rekawek, K.; Sokolowski, S.; Kolodziej, L. Distal biceps tendon rupture: A comprehensive overview. EFORT Open Rev. 2023, 8, 865–873. [Google Scholar] [CrossRef]
- Deschrijver, M.; Hautekiet, A.; Steyaert, A.; De Muynck, M.; Luypaert, E. Distal biceps tendon ruptures: More efficient diagnostics for a better outcome. Acta Orthop. Belg. 2022, 88, 160–167. [Google Scholar] [CrossRef]
- Hsu, D.; Anand, P.; Mabrouk, A.; Chang, K.V. Biceps Tendon Rupture. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK513235/ (accessed on 23 October 2025).
- Kruger, N.; Phadnis, J.; Bhatia, D.; Amarasooriya, M.; Bain, G.I. Acute distal biceps tendon ruptures: Anatomy, pathology and management—State of the art. J. ISAKOS 2020, 5, 304–313. [Google Scholar] [CrossRef]
- Goedderz, C.; Plantz, M.A.; Gerlach, E.B.; Arpey, N.C.; Swiatek, P.R.; Cantrell, C.K.; Terry, M.A.; Tjong, V.K. Determining the incidence and risk factors for short-term complications following distal biceps tendon repair. Clin. Shoulder Elb. 2022, 25, 36–41. [Google Scholar] [CrossRef]
- Cuzzolin, M.; Secco, D.; Guerra, E.; Altamura, S.A.; Filardo, G.; Candrian, C. Operative Versus Nonoperative Management for Distal Biceps Brachii Tendon Lesions: A Systematic Review and Meta-analysis. Orthop. J. Sports Med. 2021, 9, 23259671211037311. [Google Scholar] [CrossRef]
- Looney, A.M.; Day, J.; Bodendorfer, B.M.; Wang, D.; Fryar, C.M.; Murphy, J.P.; Chang, E.S. Operative vs. nonoperative treatment of distal biceps ruptures: A systematic review and meta-analysis. J. Shoulder Elb. Surg. 2022, 31, e169–e189. [Google Scholar] [CrossRef]
- Carrazana-Suarez, L.F.; Cooke, S.; Schmidt, C.C. Return to Play After Distal Biceps Tendon Repair. Curr. Rev. Musculoskelet. Med. 2022, 15, 65–74. [Google Scholar] [CrossRef]
- Oyadomari, S.; Kaplan, J.; Johnston, T.; Wang, D. Trends and complications of distal biceps tendon repair among American Board of Orthopaedic Surgery part II oral examination candidates. J. Shoulder Elb. Surg. 2023, 32, 348–352. [Google Scholar] [CrossRef] [PubMed]
- Wörner, E.; van Oost, I.; Eygendaal, D.; The, B. Higher failure rate of suture anchors in partial distal biceps tendon ruptures in comparison with Endobutton fixation. JSES Int. 2021, 5, 821–826. [Google Scholar] [CrossRef] [PubMed]
- Hogea, B.; Patrascu, J.M., Jr.; Abu-Awwad, S.A.; Suba, M.I.; Bolovan, A.; Stoianov, A.G.; Abu-Awwad, A. Comparative Analysis of Surgical Approaches for Distal Biceps Tendon Rupture: Single-Incision Technique versus Double-Incision Technique. J. Clin. Med. 2023, 12, 6423. [Google Scholar] [CrossRef]
- Lappen, S.; Geyer, S.; Kadantsev, P.; Hinz, M.; Kleim, B.; Degenhardt, H.; Imhoff, A.B.; Siebenlist, S. All-suture anchors for distal biceps tendon repair: A preliminary outcome study. Arch. Orthop. Trauma Surg. 2023, 143, 3271–3278. [Google Scholar] [CrossRef]
- Taylor, A.L.; Bansal, A.; Shi, B.Y.; Best, M.J.; Huish, E.G., Jr.; Srikumaran, U. Optimizing Fixation for Distal Biceps Tendon Repairs: A Systematic Review and Meta-regression of Cadaveric Biomechanical Testing. Am. J. Sports Med. 2021, 49, 3125–3131. [Google Scholar] [CrossRef]
- Eakin, J.L.; Whelan, R.J.; Goodrum, J.T.; Swanson, K.E. Subpectoral Biceps Tenodesis with a Bicortical Button and Proximity to the Axillary Nerve: An Anatomical Study. Osteology 2025, 5, 4. [Google Scholar] [CrossRef]
- Martinek, L.; Boháč, P.; Apostolopoulos, V.; Návrat, T.; Langer, R.; Nachtnebl, L.; Tomáš, T. Mechanical comparison of cortical button fixation, interference screw and keyhole techniques in subpectoral biceps tenodesis, including digital image correlation assessment of bone surrounding the drill hole. J. Exp. Orthop. 2025, 12, e70313. [Google Scholar] [CrossRef]
- Rutka, V.; Weppe, F.; Duprey, S.; Gras, L.L. Distal biceps tendon repair via new knotless endobutton fixation: A biomechanical study. Shoulder Elb. 2021, 13, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Bondar, L.I.; Osser, B.; Osser, G.; Mariș, M.A.; Piroș, L.E.; Almășan, R.; Toth, C.; Miuta, C.C.; Marconi, G.R.; Bouroș-Tataru, A.L.; et al. The Connection Between Depression and Ischemic Heart Disease: Analyzing Demographic Characteristics, Risk Factors, Symptoms, and Treatment Approaches to Identify Their Relationship. Clin. Pract. 2024, 14, 2166–2186. [Google Scholar] [CrossRef] [PubMed]
- Vanderlinden, A.; Carlat, R.; Vincent, B.; Detrembleur, C.; Ayong, S. Biomechanical and clinical outcomes after distal biceps tendon reattachment using an endo button technique and an interference screw. JSES Rev. Rep. Tech. 2024, 4, 743–749. [Google Scholar] [CrossRef] [PubMed]
- Eichinger, M.; Ploner, M.; Degenhart, G.; Rudisch, A.; Smekal, V.; Attal, R.; Mayr, R. Tunnel widening after ACL reconstruction with different fixation techniques: Aperture fixation with biodegradable interference screws versus all-inside technique with suspensory cortical buttons. 5-year data from a prospective randomized trial. Arch. Orthop. Trauma Surg. 2023, 143, 6707–6718. [Google Scholar] [CrossRef]
- Gao, P.; Yuan, M.; Xu, Y.; Wu, Y.; Lin, X.; Li, Y.; Li, S.; Wang, J. The safety and effectiveness comparison of Delta Medical’s PEEK interface screw and Endobutton and that of Smith & Nephew’s in arthroscopic anterior cruciate ligament reconstruction: A multicenter prospective double-blind randomized controlled clinical trial. Front. Public Health 2022, 10, 1003591. [Google Scholar] [CrossRef]
- Hochberger, F.; Hess, J.; Konrads, C.; Heinz, T.; Segatz, E.; Rudert, M.; List, K. Short-term clinical and functional outcomes of distal biceps tendon fixation: All-suture vs. titanium anchors. JSES Int. 2025, 9, 1400–1405. [Google Scholar] [CrossRef]
- Grewal, G.; Bernardoni, E.D.; Cohen, M.S.; Fernandez, J.J.; Verma, N.N.; Romeo, A.A.; Frank, R.M. Clinical Outcomes After Revision Distal Biceps Tendon Surgery. Orthop. J. Sports Med. 2021, 9, 2325967120981752. [Google Scholar] [CrossRef]
- Reinares, F.; Maza, F.; Paz, J.; Angulo, M.; Lecaros, J.J.; Ruiz Jimenez, F. Nanoscopic Distal Biceps Repair with Cortical Button and Interference Screw. Arthrosc. Tech. 2023, 12, e153–e159. [Google Scholar] [CrossRef]
- Batista, A.; Moura, N.; Sarmento, M.; Coelho, T.; Gomes, D.; Ramos, R.; Cartucho, A. Functional evaluation after cortical button fixation for distal biceps ruptures—Is there any difference between manual or non-manual workers? Rev. Esp. Cir. Ortop. Traumatol. 2024, 69, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Marconi, G.R.; Osser, B.; Osser, G.; Miuța, C.C.; Toth, C.; Ardelean, V.P.; Dicu, A.; Toderescu, C.D.; Bondar, L.I. Assessing Nutritional Knowledge and Physical Health Among Football Players: A Pilot Study from Three Sports Clubs in Western Romania. Sports 2025, 13, 16. [Google Scholar] [CrossRef]
- Khan, Z.A.; Kerzner, B.; Jackson, G.R.; Jawanda, H.S.; McCormick, J.R.; Brusalis, C.M.; Chan, J.J.; Kaplan, D.J.; Verma, N.N. Single-Incision Distal Biceps Tendon Repair with Bicortical Tensionable Locking Button Fixation. Arthrosc. Tech. 2023, 12, e2063–e2069. [Google Scholar] [CrossRef] [PubMed]
- Pitsilos, C.; Gigis, I.; Chitas, K.; Papadopoulos, P.; Ditsios, K. Systematic review of distal biceps tendon rupture in athletes: Treatment and rehabilitation. J. Shoulder Elb. Surg. 2022, 31, 1763–1772. [Google Scholar] [CrossRef]
- Koo, M.; Yang, S.-W. Visual Analogue Scale. Encyclopedia 2025, 5, 190. [Google Scholar] [CrossRef]
- Bjørnholdt, K.T.; Andersen, C.W.G. Measurement of acute postoperative pain intensity in orthopedic trials: A qualitative concept elicitation study. Acta Orthop. 2024, 95, 625–632. [Google Scholar] [CrossRef]
- Saarinen, A.J.; Uimonen, M.M.; Sandelin, H.; Toom, A.; Richter, M.; Repo, J.P. Minimal important change for the visual analogue scale foot and ankle (VAS-FA). Foot Ankle Surg. 2021, 27, 196–200. [Google Scholar] [CrossRef]
- Papen, A.; Schöttker-Königer, T.; Schäfer, A.; Morrison, F.; Hollinger, B.; Burkhart, K.J.; Nietschke, R.; Zimmerer, A.; Maffulli, N.; Migliorini, F.; et al. Reliability, validity and critical appraisal of the cross-cultural adapted German version of the Mayo Elbow Performance Score (MEPS-G). J. Orthop. Surg. Res. 2022, 17, 328. [Google Scholar] [CrossRef]
- Engelke, J.; Vorm Walde, M.; Schnetzke, M.; Grützner, P.A.; Nolte, P.C. High correlation of the subjective elbow value with Mayo Elbow Performance Score and Oxford Elbow Score in patients with elbow dislocation. JSES Int. 2023, 7, 868–871. [Google Scholar] [CrossRef]
- Zwaan, E.; Cheung, E.; IJsselmuiden, A.; Holtzer, C.; Schreuders, T.; Kofflard, M.; Alings, M.; Coert, J.H. Predictive value of the (Quick)DASH tool for upper extremity dysfunction following percutaneous coronary intervention. Patient Relat. Outcome Meas. 2022, 13, 145–155. [Google Scholar] [CrossRef]
- Chao, Z.-T.; Guo, H.-R. Reliability and validity of Quick Disabilities of the Arm, Shoulder, and Hand Questionnaire in Taiwan. Arch. Phys. Med. Rehabil. 2023, 104, e49. [Google Scholar] [CrossRef]
- Morin, M.; Hébert, L.J.; Perron, M.; Petitclerc, É.; Lake, S.R.; Duchesne, E. Psychometric properties of a standardized protocol of muscle strength assessment by hand-held dynamometry in healthy adults: A reliability study. BMC Musculoskelet. Disord. 2023, 24, 294. [Google Scholar] [CrossRef]
- Morin, M.; Duchesne, E.; Bernier, J.; Blanchette, P.; Langlois, D.; Hébert, L.J. What is known about muscle strength reference values for adults measured by hand-held dynamometry: A scoping review. Arch. Rehabil. Res. Clin. Transl. 2021, 4, 100172. [Google Scholar] [CrossRef]
- Forlenza, E.M.; Lavoie-Gagne, O.; Parvaresh, K.C.; Berlinberg, E.J.; Agarwalla, A.; Forsythe, B. Two Intramedullary and 1 Extramedullary Cortical Button, with or Without Interference Screw, Show Biomechanical Properties Superior to Native Tendon in Repair of the Distal Biceps Tendon: A Systematic Review and Network Meta-analysis of Biomechanical Performance. Arthroscopy 2023, 39, 390–401. [Google Scholar] [CrossRef]
- Benca, E.; van Knegsel, K.P.; Zderic, I.; Caspar, J.; Strassl, A.; Hirtler, L.; Fuchssteiner, C.; Gueorguiev, B.; Windhager, R.; Widhalm, H.; et al. Biomechanical evaluation of an allograft fixation system for ACL reconstruction. Front. Bioeng. Biotechnol. 2022, 10, 1000624. [Google Scholar] [CrossRef] [PubMed]
- Tagliero, A.J.; Till, S.E.; Wilbur, R.R.; Song, B.M.; Reinholz, A.K.; Johnson, A.C.; Sanchez-Sotelo, J.; Barlow, J.D.; Camp, C.L. Management of Partial-Thickness Tears of the Distal Bicep Tendon: Evaluation of 111 Patients with 10-Year Follow-up. Orthop. J. Sports Med. 2023, 11, 23259671231169202. [Google Scholar] [CrossRef] [PubMed]
- Kuan, F.C.; Hsu, K.L.; Lin, F.H.; Hong, C.K.; Chen, Y.; Shih, C.A.; Su, W.R. Biomechanical comparisons of all--suture suspensory button vs. interference screw for inlay subpectoral bicep tenodesis. J. Shoulder Elb. Surg. 2025, 34, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Osser, B.T.C.; Osser, G.; Nistor-Cseppento, C.D.; Niculescu, V.; Bondar, L.I. Student Behavior and Its Association with Multi-Device Addiction and Back Pain in Western Romania. Balneo PRM Res. J. 2025, 16, 790. [Google Scholar] [CrossRef]
- Ford, S.E.; Andersen, J.S.; Macknet, D.M.; Connor, P.M.; Loeffler, B.J.; Gaston, R.G. Major complications after distal biceps tendon repairs: Retrospective cohort analysis of 970 cases. J. Shoulder Elb. Surg. 2018, 27, 1898–1906. [Google Scholar] [CrossRef]
- Di Stefano, M.; Sensi, L.; di Bella, L.; Tucci, R.; Bazzucchi, E.; Zanna, L. Acute distal biceps tendon rupture: Retrospective analysis of two different approaches and fixation techniques. Eur. J. Orthop. Surg. Traumatol. 2022, 32, 1543–1551. [Google Scholar] [CrossRef]
- Boufadel, P.; Daher, M.; Lopez, R.; Fares, M.Y.; Lawand, J.; Khan, A.Z.; Abboud, J.A. Return to Sport After Distal Biceps Tendon Repair: A Systematic Review. Am. J. Sports Med. 2025, 53, 1769–1778. [Google Scholar] [CrossRef]
- Phelps, B.M.; Birnbrich, A.; Singer, W.; Bohle, K.; George, A.; Jack, R.A., 2nd. Postoperative rehabilitation and return to sport criteria following distal biceps tendon rupture surgery. JSES Int. 2025, 9, 929–933. [Google Scholar] [CrossRef]
- Kallhovd, G.; Lie, S.A.; Schrama, J.C.; Høvding, P.; Krukhaug, Y. Acute distal biceps tendon rupture repair comparing single versus double-incision technique: A retrospective study with follow-up. Shoulder Elb. 2025, 17585732251352745. [Google Scholar] [CrossRef]
- Castioni, D.; Mercurio, M.; Fanelli, D.; Cosentino, O.; Gasparini, G.; Galasso, O. Single- versus double-incision technique for the treatment of distal biceps tendon rupture. Bone Jt. J. 2020, 102-B, 1608–1617. [Google Scholar] [CrossRef]
- Antonacci, C.L.; Brown, S.M.; O’Brien, M.J.; Mulcahey, M.K. Prophylaxis for Heterotopic Ossification Following Distal Biceps Tendon Repair. Orthopedics 2021, 44, e588–e592. [Google Scholar] [CrossRef]
- Geuskens, W.; Caekebeke, P.; VAN Riet, R. Prevalence and clinical implications of heterotopic ossification after distal biceps tendon repair. Acta Orthop. Belg. 2023, 89, 695–700. [Google Scholar] [CrossRef] [PubMed]
- Tayyem, M.; Naji, O.; Adetokunbo, A.; Jundi, H.; Pendse, A. Retrospective Study on the Risk of Nerve Injury After Distal Biceps Tendon Repair Using Cortical Button. Cureus 2023, 15, e43512. [Google Scholar] [CrossRef] [PubMed]
- Neary, K.C.; McClish, S.J.; Khoury, A.N.; Denove, N.; Konicek, J.; Wijdicks, C.A. Biomechanical Analysis of Single Interference Screw vs Interference Screw with Cortical Button for Flexor Hallucis Longus Transfer. Foot Ankle Orthop. 2021, 6, 24730114211040445. [Google Scholar] [CrossRef] [PubMed]
- Kaarre, J.; Benvegnu, N.A.; Engler, I.D.; Nazzal, E.M.; Zsidai, B.; Senorski, E.H.; Musahl, V.; Samuelsson, K. Metal interference screw fixation combinations show high revision rates in primary hamstring tendon ACL reconstruction. BMC Musculoskelet. Disord. 2024, 25, 2. [Google Scholar] [CrossRef] [PubMed]
- Jaratjitwilai, P.; Chanlalit, C.; Sakdapanichkul, C. Dual-Incision Distal Biceps Repair Using Transosseous Technique and Cortical Fixation Button. Arthrosc. Tech. 2025, 14, 103432. [Google Scholar] [CrossRef]
- Fisher, B.T.; Chong, A.C.; Feltz, K.P.; Berglund, H.T.; Hurd, J.L. Outcomes of utilizing double-incision technique with combination of cortical button and interference screw fixation for distal biceps rupture: A case series. Shoulder Elb. 2025, 22, 17585732241312212. [Google Scholar] [CrossRef]




| Variable | Mean ± SD | Range |
|---|---|---|
| Age (years) | 32.4 ± 6.1 | 24–44 |
| Height (cm) | 178.6 ± 5.8 | 170–189 |
| Body mass (kg) | 84.2 ± 8.7 | 72–99 |
| BMI (kg/m2) | 26.3 ± 2.1 | 23.8–29.9 |
| Sport experience (years) | 8.1 ± 2.5 | 5–12 |
| Sport | n |
|---|---|
| Weightlifting | 4 |
| CrossFit | 3 |
| Combat sports | 3 |
| Bodybuilding/Fitness | 2 |
| Gymnastics | 1 |
| Parameter | 6 Weeks (Mean ± SD) | 3 Months (Mean ± SD) | 6 Months | 12 Months |
|---|---|---|---|---|
| Muscle strength recovery (% vs. contralateral arm) | 83 ± 6% | 97 ± 4% | 100% | 100% maintained |
| Elbow ROM (flexion/extension) | 130 ± 3°/0 ± 2° | Full, pain-free | Full, stable | Full, stable |
| Forearm pronation–supination | 82 ± 5°/80 ± 4° | Fully symmetric | Fully symmetric | Maintained |
| Pain during movement (VAS) | 1.2 ± 0.5 | 0 | 0 | 0 |
| Functional capacity | Light daily activities | Normal daily and occupational | Full training | Full competition |
| Tendon integrity (clinical/palpatory) | Stable, continuous | Stable | Stable | Stable |
| Esthetic outcome (biceps contour) | Good, near normal | Excellent | Excellent | Excellent |
| Complications | None | None | None | None |
| Patient satisfaction (Likert 1–5) | 4.6 ± 0.3 | 4.9 ± 0.1 | 5.0 | 5.0 |
| Outcome | Time Points Included | Test Used | Test Statistic (df) | p-Value | Effect Size | Main Finding (Post Hoc) |
|---|---|---|---|---|---|---|
| VAS | 6 w, 3 m, 6 m, 12 m | Friedman | χ2(3) = 36.8 | <0.001 | Kendall’s W = 0.71 | Significant reduction from early postop to all later timepoints |
| MEPS | 6 w, 3 m, 6 m, 12 m | RM ANOVA | F(1.9, 22.8) = 54.2 | <0.001 | ηp2 = 0.82 | Significant increase 6 w → 3 m → 6 m; plateau thereafter |
| QuickDASH | 6 w, 3 m, 6 m, 12 m | Friedman | χ2(3) = 28.4 | <0.001 | Kendall’s W = 0.73 | Significant decrease between all timepoints |
| Strength (%) | 6 w, 3 m, 6 m, 12 m | RM ANOVA | F(1.8, 21.6) = 48.9 | <0.001 | ηp2 = 0.80 | 6 w < 3 m and 6 m (p < 0.05); full recovery by 6 m |
| Time Point | MEPS (Mean ± SD) | QuickDASH (Mean ± SD) | Return-to-Activity Status | Functional Interpretation |
|---|---|---|---|---|
| 6 weeks | 90 ± 5 | 12 ± 3 | Light daily activities, early physiotherapy | Good–Excellent |
| 3 months | 96 ± 3 | 6 ± 2 | Full occupational activity, light sports | Excellent |
| 6 months | 98 ± 2 | 3 ± 1 | Unrestricted athletic participation | Excellent |
| 12 months | 99 ± 1 | 2 ± 1 | Maintained full sport performance | Excellent, sustained |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fazakas, R.; Tolan, G.A.; Osser, B.; Toth, C.; Ilia, I.; Marcu, F.M.; Pascalau, N.A.; Suciu, R.N.; Gavrila-Ardelean, L.; Bondar, L.I. Hybrid Tightrope–PEEK Dual Fixation for Distal Biceps Tendon Reinsertion in High-Performance Athletes: A Prospective Case Series. J. Clin. Med. 2025, 14, 8488. https://doi.org/10.3390/jcm14238488
Fazakas R, Tolan GA, Osser B, Toth C, Ilia I, Marcu FM, Pascalau NA, Suciu RN, Gavrila-Ardelean L, Bondar LI. Hybrid Tightrope–PEEK Dual Fixation for Distal Biceps Tendon Reinsertion in High-Performance Athletes: A Prospective Case Series. Journal of Clinical Medicine. 2025; 14(23):8488. https://doi.org/10.3390/jcm14238488
Chicago/Turabian StyleFazakas, Roland, Gloria Alexandra Tolan, Brigitte Osser, Csongor Toth, Iosif Ilia, Florin Mihai Marcu, Nicoleta Anamaria Pascalau, Ramona Nicoleta Suciu, Liviu Gavrila-Ardelean, and Laura Ioana Bondar. 2025. "Hybrid Tightrope–PEEK Dual Fixation for Distal Biceps Tendon Reinsertion in High-Performance Athletes: A Prospective Case Series" Journal of Clinical Medicine 14, no. 23: 8488. https://doi.org/10.3390/jcm14238488
APA StyleFazakas, R., Tolan, G. A., Osser, B., Toth, C., Ilia, I., Marcu, F. M., Pascalau, N. A., Suciu, R. N., Gavrila-Ardelean, L., & Bondar, L. I. (2025). Hybrid Tightrope–PEEK Dual Fixation for Distal Biceps Tendon Reinsertion in High-Performance Athletes: A Prospective Case Series. Journal of Clinical Medicine, 14(23), 8488. https://doi.org/10.3390/jcm14238488








