Patient Perspectives After Trapeziectomy Versus Carpometacarpal Prosthesis: A Qualitative Thematic Analysis of Ten Bilateral Cases
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participants and Recruitment
2.3. Data Collection
2.4. Data Analysis
2.5. Researcher Reflexivity
2.6. Ethics
3. Results
3.1. Strength
3.2. Resilience and Rehabilitation
3.3. Aesthetics
3.4. Surgical Preferences
4. Discussion
4.1. Strength and Function
4.2. Rehabilitation and Resilience
4.3. Aesthetic Perceptions
4.4. Patient Preferences and Shared Decision-Making
4.5. Long-Term Experiences
4.6. Complications and Revision Concerns
4.7. Doctor–Patient Communication and Expectations
4.8. Quality of Life and Psychosocial Impact
4.9. Strengths and Limitations
4.10. Clinical Implications
4.11. Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Unglaub, F.; Spies, C.K. Rhizarthrose—Ein Update. Orthopäde 2022, 51, 1. [Google Scholar] [CrossRef]
- Liukkonen, R.; Karjalainen, V.-L.; Kvist, R.; Vaajala, M.; Ponkilainen, V.; Karjalainen, T. Total Joint Arthroplasty for Thumb Carpometacarpal Joint Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Acta Orthop. 2024, 95, 325–332. [Google Scholar] [CrossRef]
- Bhat, S.; Weeda, L.; Seth, I.; Rozen, W.M. Comparison of Surgical Techniques and Joint Injections for Base of Thumb Osteoarthritis: A Systematic Review. J. Hand Surg. Glob. Online 2025, 7, 212–218. [Google Scholar] [CrossRef]
- Gervis, W. Osteo-Arthritis of the Trapezio-Metacarpal Joint Treated by Excision of the Trapezium. Proc. R. Soc. Med. 1947, 40, 492. [Google Scholar] [CrossRef]
- de la Caffinière, J. Total Trapezo-Metacarpal Prosthesis. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1974, 60, 299–308. [Google Scholar] [PubMed]
- Fang, E.; Behroozian, T.; Thoma, A. A Systematic Review of Systematic Reviews Comparing Simple Trapeziectomy versus Trapeziectomy with Ligament Reconstruction and Tendon Interposition for Trapeziometacarpal Osteoarthritis. J. Hand Microsurg. 2025, 17, 100160. [Google Scholar] [CrossRef]
- Wolf, J.M.; Turkiewicz, A.; Englund, M.; Karlsson, J.; Arner, M.; Atroshi, I. What Are the Patient-Reported Outcomes of Trapeziectomy and Tendon Suspension at Long-Term Follow-Up? Clin. Orthop. Relat. Res. 2021, 479, 2009–2018. [Google Scholar] [CrossRef]
- Jager, T.; Barbary, S.; Dap, F.; Dautel, G. Analyse de la douleur postopératoire et des résultats fonctionnels précoces dans le traitement de la rhizarthrose. Étude prospective comparative de 74 patientes trapézectomie-interposition vs prothèse MAIA®. Chir. Main 2013, 32, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Frey, P.-E.; Bühner, C.; Falkner, F.; Harhaus, L.; Panzram, B. Mid- and Long-Term Clinical Results of the Elektra and Moovis Prosthesis for Trapeziometacarpal Joint Replacement. BMC Musculoskelet. Disord. 2024, 25, 332. [Google Scholar] [CrossRef]
- Ulrich-Vinther, M.; Puggaard, H.; Lange, B. Prospective 1-Year Follow-Up Study Comparing Joint Prosthesis with Tendon Interposition Arthroplasty in Treatment of Trapeziometacarpal Osteoarthritis. J. Hand Surg. 2008, 33, 1369–1377. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Yoon, B.; Kim, C.; Choi, S.; Han, S. Prosthetic Replacement Has a Clinical Outcome Superior to That of Trapeziectomy with Ligament Reconstruction and Tendon Interposition: A Meta-Analysis. Orthopedics 2021, 44, e151–e157. [Google Scholar] [CrossRef]
- Latelise, B.; Ben Brahim, E.; Prasil, L.; Freslon, M. Complications of Prosthesis Versus Trapeziectomy in Trapeziometacarpal Joint Arthritis: A Systematic Review. Hand Surg. Rehabil. 2024, 43, 101672. [Google Scholar] [CrossRef] [PubMed]
- Windhofer, C.M.; Neureiter, J.; Schauer, J.; Zimmermann, G.; Hirnsperger, C. Trapeziectomy Versus Maïa Prosthesis in Trapeziometacarpal Osteoarthritis. J. Wrist Surg. 2024, 13, 142–150. [Google Scholar] [CrossRef]
- Craik, J.D.; Glasgow, S.; Andren, J.; Sims, M.; Mansouri, R.; Sharma, R.; Ellahee, N. Early Results of the ARPE Arthroplasty Versus Trapeziectomy for the Treatment of Thumb Carpometacarpal Joint Osteoarthritis. J. Hand Surg. Asian-Pac. Vol. 2017, 22, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Espino, P.; Pottier, M.; Detrembleur, C.; Goffin, D. Touch® Double Mobility Arthroplasty for Trapeziometacarpal Osteoarthritis: Outcomes for 92 Prostheses. Hand Surg. Rehabil. 2021, 40, 760–764. [Google Scholar] [CrossRef]
- Falaise, C.; Boulat, S. Five-to-8-Year Prospective Follow-up of 61 Touch® Trapeziometacarpal Prostheses. Hand Surg. Rehabil. 2025, 44, 102167. [Google Scholar] [CrossRef]
- Barret, P.C.; Hackley, D.T.; Lockhart, E.S.; Yu-Shan, A.A.; Bravo, C.J.; Apel, P.J. What Factors Influence Variability in Thumb Carpometacarpal Arthroplasty Care? A Survey of ASSH Members. Hand 2025, 20, 129–135. [Google Scholar] [CrossRef]
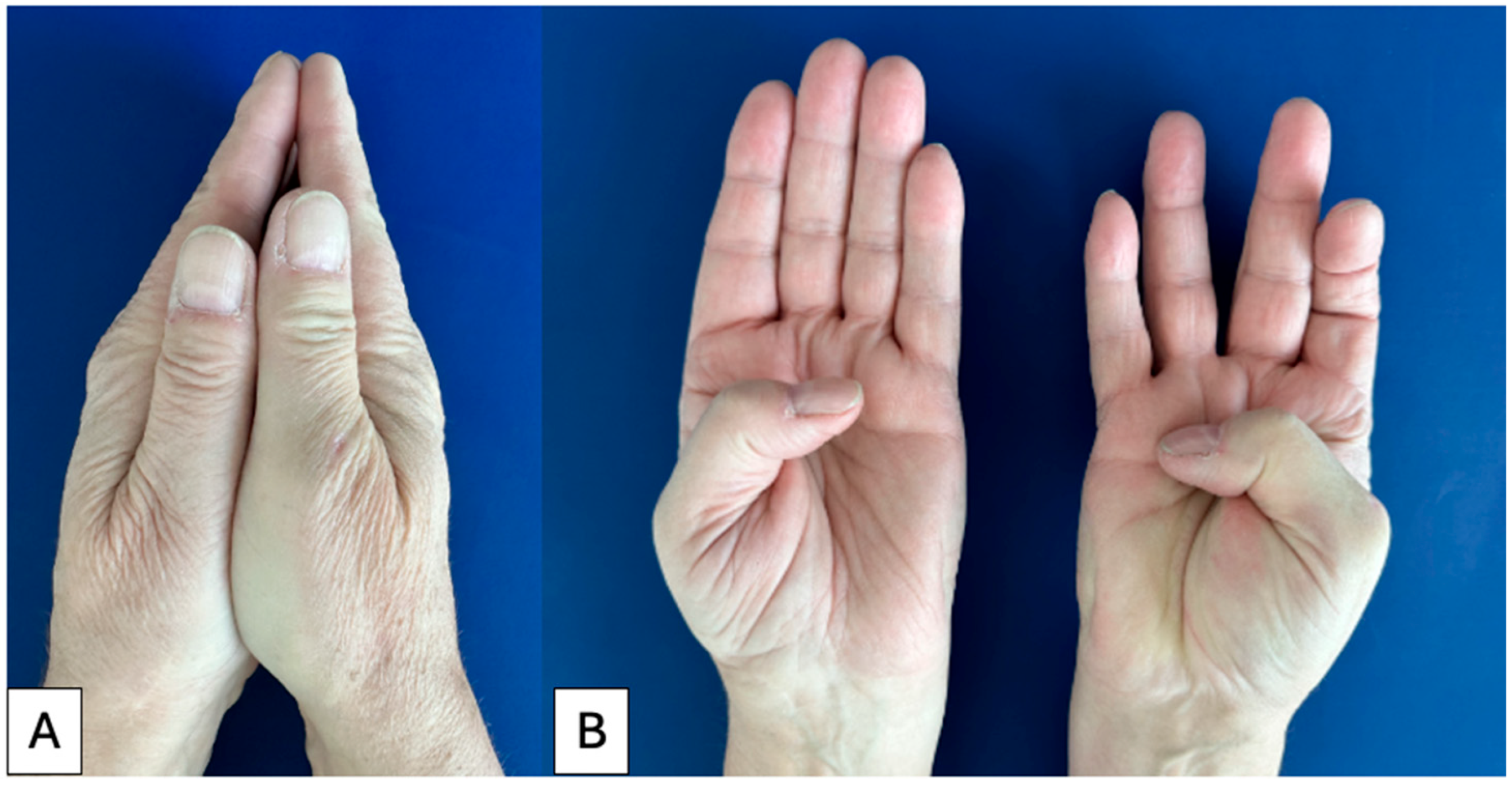
- Dietrich, L.G.; Kasparkova, K.; Silins, K.; Berner, I.; Genewein, U.; Vögelin, E. Trapeziectomy vs. Carpometacarpal Prosthesis: Two Techniques in an “In Vivo” Side-by-Side Comparison. J. Plast. Reconstr. Aesthet. Surg. 2025, 109, 249–251. [Google Scholar] [CrossRef]
- Lim, B.; Sen, S. A Cross-Sectional Quantitative Analysis of the Readability and Quality of Online Resources Regarding Thumb Carpometacarpal Joint Replacement Surgery. J. Hand Microsurg. 2024, 16, 100119. [Google Scholar] [CrossRef]
- Mousoulis, C.; Karantana, A.; Trickett, R.W.; Thomas, K.S.; Leighton, P. ‘It’s Just a Finger Isn’t It…’: Patients’ Perspectives of Recovery Following Finger Fractures and Participation in Surgical Trials—A Qualitative Interview Study. BMJ Open 2023, 13, e065185. [Google Scholar] [CrossRef]
- Hansen, A.Ø.; Kielsgaard, K.; Larsen, S.M. Management of Everyday Life After a Hand Operation—A Qualitative Study of Patients with a Weak Sense of Coherence. J. Hand Ther. 2024, 37, 625–634. [Google Scholar] [CrossRef]
- Park, M.O.; Eppler, S.L.; Chatterjee, M.; Shapiro, L.M.; Kamal, R.N.; Harris, A.H.S.; Kakar, S.; Blazar, P.; Akelman, E.; Got, C.; et al. Patient-Derived Framework for Quality in Hand Surgery: A Qualitative Analysis. J. Hand Surg. 2022, 47, 1045–1056. [Google Scholar] [CrossRef]
- Arends, G.R.; Loos, N.L.; Van Kooij, Y.E.; Tabeau, K.; De Ridder, W.A.; Selles, R.W.; Veltkamp, J.; Outcome-Based Healthcare Research Group; Wouters, R.M. What Are the Perspectives of Patients with Hand and Wrist Conditions, Chronic Pain, and Patients Recovering from Stroke on the Use of Patient and Outcome Information in Everyday Care? A Mixed-Methods Study. Qual. Life Res. 2024, 33, 2573–2587. [Google Scholar] [CrossRef] [PubMed]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the Framework Method for the Analysis of Qualitative Data in Multi-Disciplinary Health Research. BMC Med. Res. Methodol. 2013, 13, 117. [Google Scholar] [CrossRef]
- Herren, D.; Marks, M.; Neumeister, S.; Schindele, S. Short-Term Recovery After Implant Versus Resection Arthroplasty in Trapeziometacarpal Joint Osteoarthritis. J. Hand Surg. Eur. Vol. 2023, 48, 1048–1055. [Google Scholar] [CrossRef] [PubMed]
- Smeraglia, F.; Carità, E.; Frittella, G.; Tamborini, F.; Diaz, L.; Donadelli, A.; Guzzini, M. Intra-Patient Comparison of Trapeziectomy with LRTI and Dual Mobility Prosthesis for Trapeziometacarpal Osteoarthritis: A Multicenter Observational Study. Eur. J. Orthop. Surg. Traumatol. 2025, 35, 329. [Google Scholar] [CrossRef]
- Nietlispach, V.; Marks, M.; Imhof, J.; Pudic, T.; Herren, D.B. Which Would You Choose Again? Comparison of Trapeziometacarpal Implant Versus Resection Arthroplasty in the Same Patient. J. Hand Surg. Eur. Vol. 2024, 50, 178–183. [Google Scholar] [CrossRef]
- Dreant, N.; Poumellec, M.-A. Total Thumb Carpometacarpal Joint Arthroplasty: A Retrospective Functional Study of 28 MOOVIS Prostheses. Hand 2019, 14, 59–65. [Google Scholar] [CrossRef]
- Toffoli, A.; Teissier, J. MAÏA Trapeziometacarpal Joint Arthroplasty: Clinical and Radiological Outcomes of 80 Patients with More than 6 Years of Follow-Up. J. Hand Surg. 2017, 42, 838.e1–838.e8. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Z.-L.; Xie, H. Mesenchymal Stem Cell-Derived Extracellular Vesicles: A Possible Therapeutic Strategy for Orthopaedic Diseases: A Narrative Review. Biomater. Transl. 2022, 3, 175–187. [Google Scholar] [CrossRef] [PubMed]
- Borcherding, K.; Schmidmaier, G.; Hofmann, G.O.; Wildemann, B. The Rationale Behind Implant Coatings to Promote Osteointegration, Bone Healing or Regeneration. Injury 2021, 52, S106–S111. [Google Scholar] [CrossRef]
- Gu, Y.; Hu, Y.; Zhang, H.; Wang, S.; Xu, K.; Su, J. Single-cell RNA Sequencing in Osteoarthritis. Cell Prolif. 2023, 56, e13517. [Google Scholar] [CrossRef]
- Farkash, U.; Sakhnini, M.; Dreyfuss, D.; Tordjman, D.; Rotem, G.; Luria, S. Failure Rate and Early Complications of Thumb Carpometacarpal Joint Replacement—A Multicenter Retrospective Study of Two Modern Implant Designs. J. Clin. Med. 2023, 13, 121. [Google Scholar] [CrossRef]
- Guardia, C.; Moutet, F.; Corcella, D.; Forli, A.; Pradel, P. Prothèse Roseland®: Étude de qualité de vie de 68 patients avec un recul moyen de 43,8 mois. Chir. Main 2010, 29, 301–306. [Google Scholar] [CrossRef]
- Semere, A.; Vuillerme, N.; Corcella, D.; Forli, A.; Moutet, F. Results with the Roseland® HAC Trapeziometacarpal Prosthesis After more than 10 Years. Chir. Main 2015, 34, 59–66. [Google Scholar] [CrossRef]
- Bricout, M.; Rezzouk, J. Complications and Failures of the Trapeziometacarpal Maia® Prosthesis: A Series of 156 Cases. Hand Surg. Rehabil. 2016, 35, 190–198. [Google Scholar] [CrossRef]
- Raj, S.; Clay, R.; Ramji, S.; Shaunak, R.; Dadrewalla, A.; Sinha, V.; Shaunak, S. Trapeziectomy Versus Joint Replacement for First Carpometacarpal (CMC 1) Joint Osteoarthritis: A Systematic Review and Meta-Analysis. Eur. J. Orthop. Surg. Traumatol. 2022, 32, 1001–1021. [Google Scholar] [CrossRef] [PubMed]
- Cerlier, A.; Guinard, D.; Gay, A.M.; Legré, R. Outcomes of Secondary Trapeziectomy After Revision of Trapeziometacarpal Implants: A Retrospective Comparative Matched Study. J. Hand Surg. Eur. Vol. 2021, 46, 1096–1100. [Google Scholar] [CrossRef] [PubMed]
| Gender | Age | Time Since Surgery (Years) Trapeziectomy | Time Since Surgery (Years) Prosthesis | Dominant Hand | |
|---|---|---|---|---|---|
| Patient 1 | female | 75 | 25 (right) | 3.8 (left) | right |
| Patient 2 | female | 68 | 7.8 (left) | 6.9 (right) | right |
| Patient 3 | male | 64 | 7.6 (left) | 4.9 (right) | left |
| Patient 4 | female | 76 | 6.6 (left) | 6.5 (right) | right |
| Patient 5 | male | 70 | 14.7 (left) | 6.8 (right) | right |
| Patient 6 | female | 68 | 9.4 (left) | 5.8 (right) | right |
| Patient 7 | female | 63 | 11.6 (right) | 0.8 (left) | right |
| Patient 8 | male | 73 | 14 (left) | 2.9 (right) | left |
| Patient 9 | female | 77 | 8.8 (right) | 1.1 (left) | right |
| Patient 10 | female | 74 | 7.6 (right) | 0.7 (left) | right |
| Theme | Subthemes | Illustrative Quotations |
|---|---|---|
| Strength | Perceived stronger prosthesis side; Adequacy for daily tasks; Fatigue differences | “My prosthetic thumb is noticeably stronger.” (female) “Both sides are sufficient for daily life.” (female) “The trapeziectomy side tires faster.” (male) |
| Rehabilitation and resilience | Faster recovery with prosthesis; Reduced therapy burden; Long-term endurance differences | “After the prosthesis, I needed far less therapy.” (male) “Only three therapy sessions, and I was back to normal.” (female) “The trapeziectomy hand sets the limits for carrying weight.” (female) |
| Aesthetics | Dissatisfaction after trapeziectomy (shortening, collapse, swelling); Natural appearance with prosthesis; Psychosocial impact | “The sunken thumb is aesthetically unappealing.” (female) “The prosthesis feels like a normal thumb.” (male) “I prefer the prosthetic thumb and hide the other one.” (female) |
| Surgical preference | Hypothetical choice for prosthesis; Faster recovery; Reversibility and reliability | “I would choose the prosthesis again without hesitation.” (female) “Recovery was significantly shorter with prosthesis.” (male) “Why choose a solution with no point of return?” (male) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dietrich, L.G.; Rinaldi, V.; Vögelin, E. Patient Perspectives After Trapeziectomy Versus Carpometacarpal Prosthesis: A Qualitative Thematic Analysis of Ten Bilateral Cases. J. Clin. Med. 2025, 14, 8375. https://doi.org/10.3390/jcm14238375
Dietrich LG, Rinaldi V, Vögelin E. Patient Perspectives After Trapeziectomy Versus Carpometacarpal Prosthesis: A Qualitative Thematic Analysis of Ten Bilateral Cases. Journal of Clinical Medicine. 2025; 14(23):8375. https://doi.org/10.3390/jcm14238375
Chicago/Turabian StyleDietrich, Léna G., Valeria Rinaldi, and Esther Vögelin. 2025. "Patient Perspectives After Trapeziectomy Versus Carpometacarpal Prosthesis: A Qualitative Thematic Analysis of Ten Bilateral Cases" Journal of Clinical Medicine 14, no. 23: 8375. https://doi.org/10.3390/jcm14238375
APA StyleDietrich, L. G., Rinaldi, V., & Vögelin, E. (2025). Patient Perspectives After Trapeziectomy Versus Carpometacarpal Prosthesis: A Qualitative Thematic Analysis of Ten Bilateral Cases. Journal of Clinical Medicine, 14(23), 8375. https://doi.org/10.3390/jcm14238375







