Impact of Mandibular Advancement Therapy on Occlusal Plane Orientation and Incisor Inclination in Obstructive Sleep Apnea Patients: A Retrospcetive Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Autodesk Meshxmixer
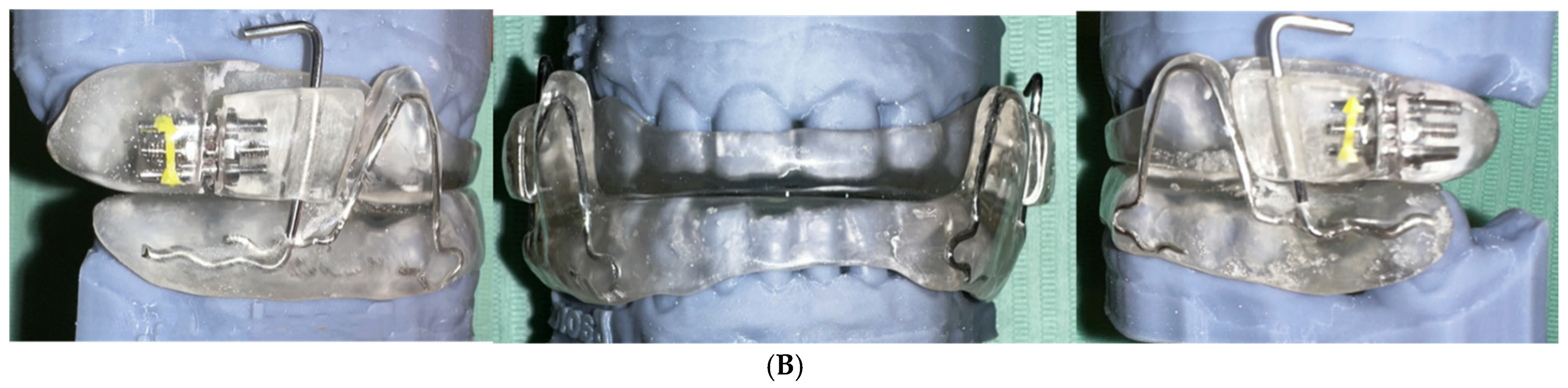
2.2. IMYS Appliance
2.3. Statistical Analysis
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Iannella, G.; Pace, A.; Bellizzi, M.G.; Magliulo, G.; Greco, A.; De Virgilio, A.; Croce, E.; Gioacchini, F.M.; Re, M.; Costantino, A.; et al. The Global Burden of Obstructive Sleep Apnea. Diagnostics 2025, 15, 1088. [Google Scholar] [CrossRef] [PubMed]
- Senaratna, C.V.; Perret, J.L.; Lodge, C.J.; Lowe, A.J.; Campbell, B.E.; Matheson, M.C.; Hamilton, G.S.; Dharmage, S.C. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med. Rev. 2017, 34, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Ciavarella, D.; Lorusso, M.; Campobasso, A.; Cazzolla, A.P.; Montaruli, G.; Burlon, G.; Lo Muzio, E.; Laurenziello, M.; Tepedino, M. Craniofacial morphology in Obstructive Sleep Apnea patients. J. Clin. Exp. Dent. 2023, 15, e999–e1006. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Lu, Q.; Li, S.; Pu, Z.; Gao, F.; Zhou, B. Risk factors associated with the severity of obstructive sleep apnea syndrome among adults. Sci. Rep. 2020, 10, 13508. [Google Scholar] [CrossRef]
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.M.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pepin, J.L.; et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. Lancet Respir. Med. 2019, 7, 687–698. [Google Scholar] [CrossRef]
- Eckert, D.J. Phenotypic approaches to obstructive sleep apnoea—New pathways for targeted therapy. Sleep Med. Rev. 2018, 37, 45–59. [Google Scholar] [CrossRef]
- Pham, L.V.; Jun, J.; Polotsky, V.Y. Obstructive sleep apnea. Handb. Clin. Neurol. 2022, 189, 105–136. [Google Scholar] [CrossRef]
- Patil, S.P.; Schneider, H.; Schwartz, A.R.; Smith, P.L. Adult obstructive sleep apnea: Pathophysiology and diagnosis. Chest 2007, 132, 325–337. [Google Scholar] [CrossRef]
- Gili, T.; Di Carlo, G.; Capuani, S.; Auconi, P.; Caldarelli, G.; Polimeni, A. Complexity and data mining in dental research: A network medicine perspective on interceptive orthodontics. Orthod. Craniofac Res. 2021, 24 (Suppl. 2), 16–25. [Google Scholar] [CrossRef]
- Gottlieb, D.J.; Punjabi, N.M. Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA 2020, 323, 1389–1400. [Google Scholar] [CrossRef]
- Weaver, T.E.; Grunstein, R.R. Adherence to continuous positive airway pressure therapy: The challenge to effective treatment. Proc. Am. Thorac. Soc. 2008, 5, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Johal, A.; Hamoda, M.M.; Almeida, F.R.; Marklund, M.; Tallamraju, H. The role of oral appliance therapy in obstructive sleep apnoea. Eur. Respir. Rev. 2023, 32, 220257. [Google Scholar] [CrossRef] [PubMed]
- Ghazal, A.; Jonas, I.; Rose, E. Dental Side Effects of Mandibular Advancement Appliances-A2-year Follow-up. J. Orofac. Orthop. 2008, 69, 437–447. [Google Scholar] [CrossRef] [PubMed]
- Christino, M.; Vinha, P.P.; Faria, A.C.; Garcia, D.M.; de Mello-Filho, F.V. Impact of counterclockwise rotation of the occlusal plane on the mandibular advancement, pharynx morphology, and polysomnography results in maxillomandibular advancement surgery for the treatment of obstructive sleep apnea patients. Sleep Breath. 2021, 25, 2307–2313. [Google Scholar] [CrossRef]
- Mayoral, P.; Lagravere, M.O.; Miguez-Contreras, M.; Garcia, M. Antero-posterior mandibular position at different vertical levels for mandibular advancing device design. BMC Oral Health 2019, 19, 85. [Google Scholar] [CrossRef]
- Uyaner, A.; Schneider, H.; Parikh, A.; Paeske-Hinz, K.; Konermann, A. Mandibular Advancement Devices in OSA Patients: Impact on Occlusal Dynamics and Tooth Alignment Modifications-A Pilot Prospective and Retrospective Study. Dent. J. 2024, 12, 370. [Google Scholar] [CrossRef]
- Machado, C.A.O.; de Resende, C.; Stuginski-Barbosa, J.; Porporatti, A.L.; Carra, M.C.; Michelloti, A.; Boucher, Y.; Simamoto Junior, P.C. Association between obstructive sleep apnea and temporomandibular disorders: A meta-analysis. J. Oral Rehabil. 2024, 51, 2220–2233. [Google Scholar] [CrossRef]
- Lee, Y.H.; Jeon, S.; Auh, Q.S.; Chung, E.J. Automatic prediction of obstructive sleep apnea in patients with temporomandibular disorder based on multidata and machine learning. Sci. Rep. 2024, 14, 19362. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef]
- Ciavarella, D.; Ferrara, D.; Fanelli, C.; Montaruli, G.; Burlon, G.; Laurenziello, M.; Lo Russo, L.; Esperouz, F.; Tepedino, M.; Lorusso, M. Evaluation of sleep position shifts in patients with obstructive sleep apnea syndrome with the use of a mandibular advancement device. Front. Dent. Med. 2025, 6, 1524334. [Google Scholar] [CrossRef]
- Ishida, E.; Kunimatsu, R.; Medina, C.C.; Iwai, K.; Miura, S.; Tsuka, Y.; Tanimoto, K. Dental and Occlusal Changes during Mandibular Advancement Device Therapy in Japanese Patients with Obstructive Sleep Apnea: Four Years Follow-Up. J. Clin. Med. 2022, 11, 7539. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis. Curr. Dir. Psychol. Sci. 1992, 1, 98–101. [Google Scholar] [CrossRef]
- Houston, W.J. The analysis of errors in orthodontic measurements. Am. J. Orthod. 1983, 83, 382–390. [Google Scholar] [CrossRef]
- Dahlberg, G. Statistical Methods for Medical and Biological Students; G. Allen & Unwin Limited: Crows Nest, NSW, Australia, 1940. [Google Scholar]
- Uniken Venema, J.A.M.; Rosenmoller, B.; de Vries, N.; de Lange, J.; Aarab, G.; Lobbezoo, F.; Hoekema, A. Mandibular advancement device design: A systematic review on outcomes in obstructive sleep apnea treatment. Sleep Med. Rev. 2021, 60, 101557. [Google Scholar] [CrossRef]
- Chen, A.; Burger, M.S.; Rietdijk-Smulders, M.; Smeenk, F. Mandibular advancement device: Effectiveness and dental side effects. A Real-Life Study Cranio 2022, 40, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Ciavarella, D.; Ferrara, D.; Fanelli, C.; Esperouz, F.; Burlon, C.; Burlon, G.; Russo, L.; Tepedino, M.; Lorusso, M. Effects of Mandibular Advancement Device on Cardiovascular and Respiratory Parameters in OSA Patients. Oral 2025, 5, 62. [Google Scholar] [CrossRef]
- Ciavarella, D.; Fanelli, C.; Suriano, C.; Campobasso, A.; Lorusso, M.; Ferrara, D.; Maci, M.; Esposito, R.; Tepedino, M. Curve of Spee modification in different vertical skeletal patterns after clear aligner therapy: A 3D set-up retrospective study. Prog. Orthod. 2024, 25, 5. [Google Scholar] [CrossRef] [PubMed]
- Staderini, E.; Chiusolo, G.; Guglielmi, F.; Papi, M.; Perini, G.; Tepedino, M.; Gallenzi, P. Effects of Thermoforming on the Mechanical, Optical, Chemical, and Morphological Properties of PET-G: In Vitro Study. Polymers 2024, 16, 203. [Google Scholar] [CrossRef]
- Ciavarella, D.; Lorusso, M.; Fanelli, C.; Cazzolla, A.P.; Maci, M.; Ferrara, D.; Lo Muzio, L.; Tepedino, M. The Correlation between Mandibular Arch Shape and Vertical Skeletal Pattern. Medicina 2023, 59, 1926. [Google Scholar] [CrossRef] [PubMed]
- Ciavarella, D.; Lorusso, M.; Fanelli, C.; Ferrara, D.; Laurenziello, M.; Montaruli, G.; Esposito, R.; Tepedino, M. Evaluation of occlusal force in Class II subdivision malocclusion. J. Oral Rehabil. 2024, 51, 1813–1820. [Google Scholar] [CrossRef]
- Doff, M.H.; Finnema, K.J.; Hoekema, A.; Wijkstra, P.J.; de Bont, L.G.; Stegenga, B. Long-term oral appliance therapy in obstructive sleep apnea syndrome: A controlled study on dental side effects. Clin. Oral Investig. 2013, 17, 475–482. [Google Scholar] [CrossRef]
- Marklund, M.; Franklin, K.A.; Persson, M. Orthodontic side-effects of mandibular advancement devices during treatment of snoring and sleep apnoea. Eur. J. Orthod. 2001, 23, 135–144. [Google Scholar] [CrossRef]
- Chen, Y.; Alhozgi, A.I.; Almeida, F.R. Dentoskeletal changes of long-term oral appliance treatment in patients with obstructive sleep apnea: A systematic review and meta-analysis. J. Prosthodont. 2025, 34, 62–79. [Google Scholar] [CrossRef]
- Linsen, S.S.; Meyer, A.; Daratsianos, N.; Kares, A. 3-D changes in tooth position after treatment with mandibular advancement devices -a retrospective study in a non-university setting. BMC Oral Health 2025, 25, 543. [Google Scholar] [CrossRef]
- Camacho-Alvarez, F.E.; Martinez-Contreras, S.P.; Rodriguez-Chavez, J.A.; Martinez-Suarez, G.; Gonzalez-Aragon Pineda, A.E.; Ramos-Montiel, R.R.; Ramirez-Martinez, C.M.; Sanchez-Garcia, S.; Cruz-Hervert, L.P.; Jimenez-Corona, M.E. Characteristics of the Occlusal Plane Associated with Unilateral and Bilateral Articular Eminence Inclination: A Cross-Sectional CBCT Study. Dent. J. 2024, 12, 316. [Google Scholar] [CrossRef]
- Raja, V.K.; Anbarasu, P.; Dinesh, S.S.; Subramanian, S.K.; Eisenhuth, G.; Eisenhuth, S.; Eisenhuth, C.; Bhandi, S. An Evaluation of the Relationship between Condylar Guidance, Occlusal Plane Orientation, Cuspal Inclination, and Compensatory Curves in Permanent Dentition. J. Contemp. Dent. Pr. 2025, 26, 377–382. [Google Scholar] [CrossRef]
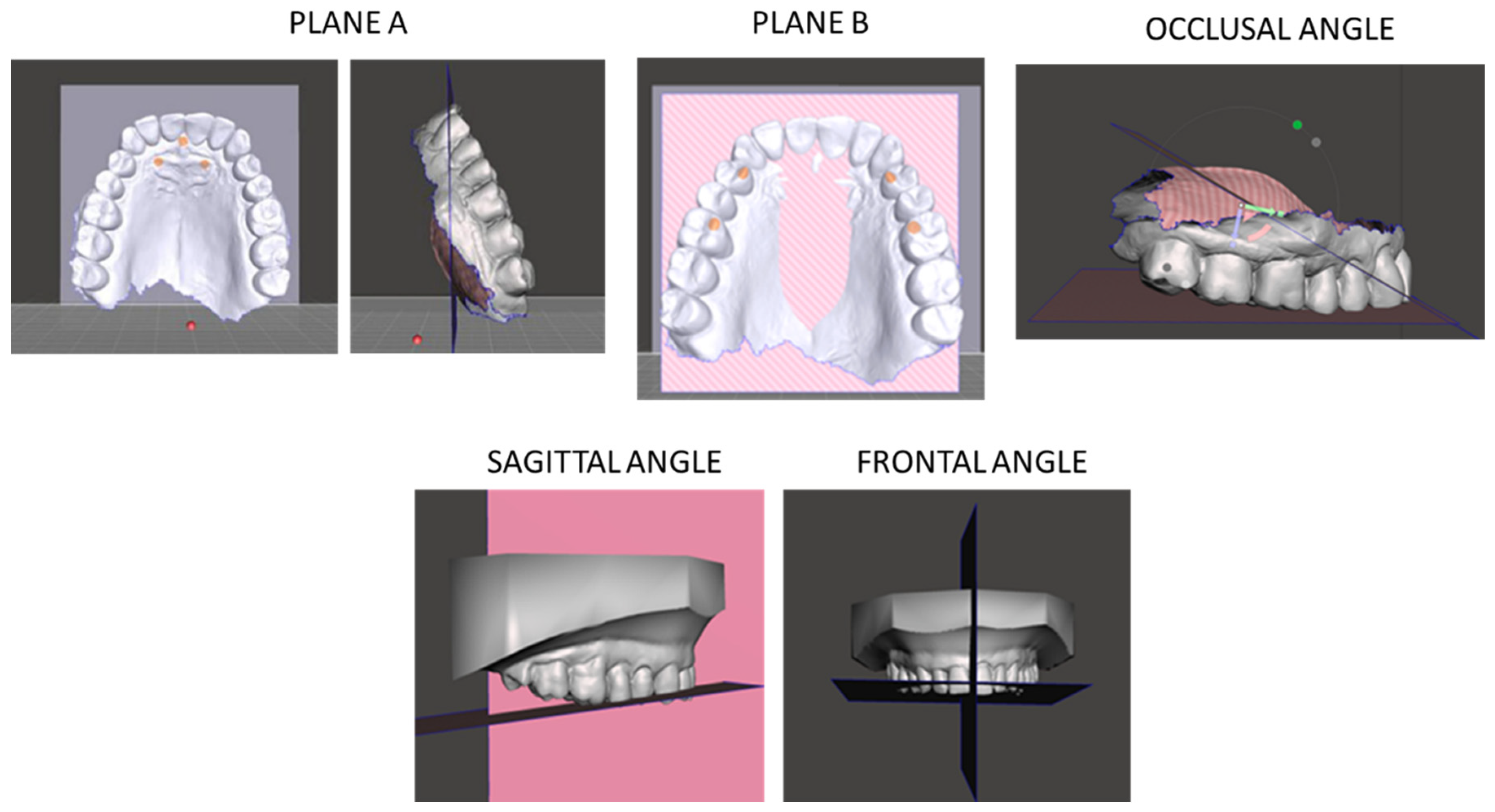
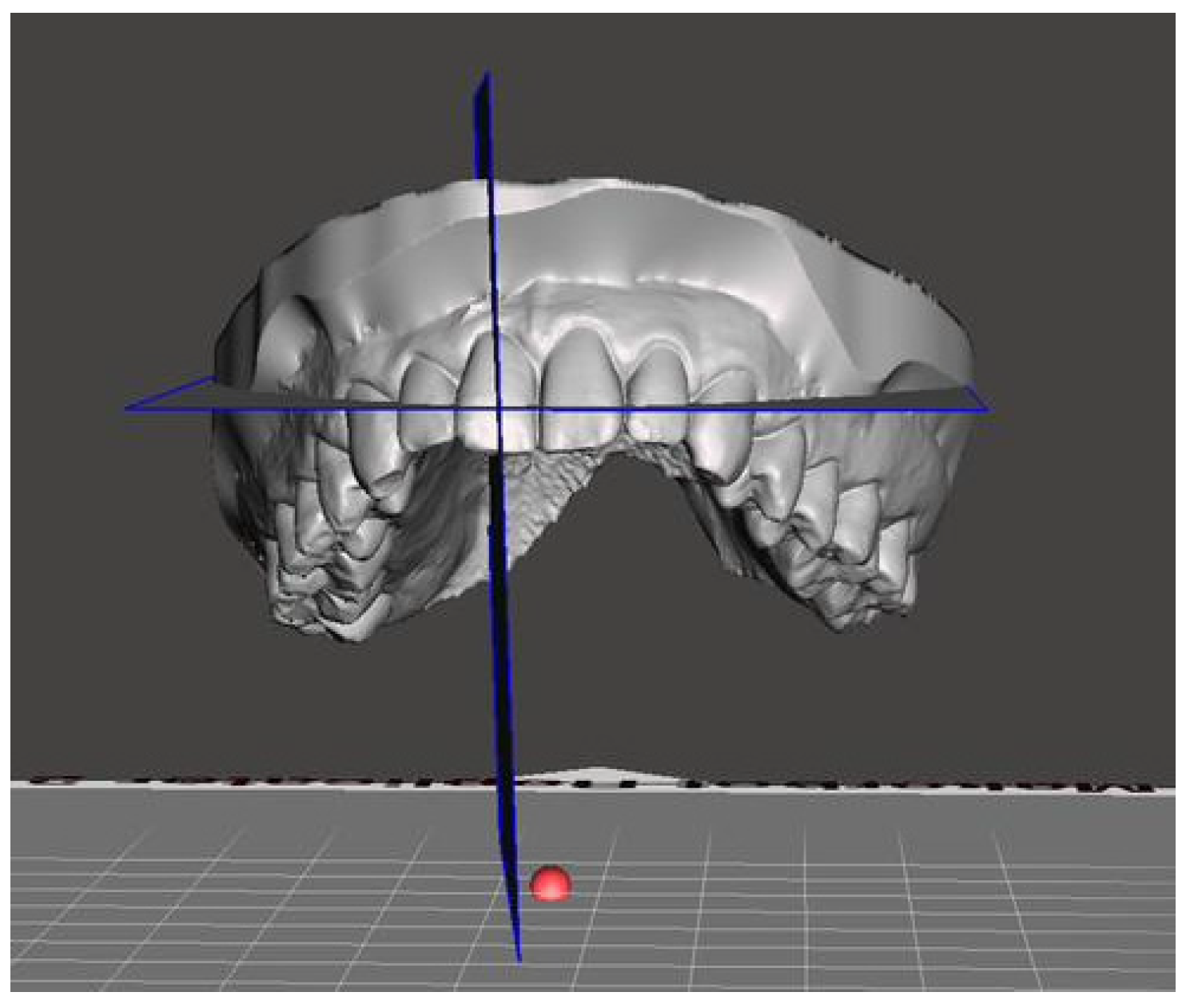

| Variable | Definition | Reference Planes |
|---|---|---|
| Occlusal angle | Angle formed by the intersection of two reference planes: a–b | Plane a: incisive papilla and palatal rugae; Plane b: palatal cusps of first maxillary premolars and mesio-palatal cusps of first maxillary molars |
| Sagittal angle | Angle formed by plane b and c | Plane b, Plane c: mid-palatal sagittal plane through incisive papilla |
| Frontal angle | Angle measured between by plane b and c on frontal plane | Plane b and c in frontal projection |
| Upper incisor inclination | Angle between long axis of upper central incisor and reference plane | Incisive papilla plane and long incisor axis |
| Variables | Time | Mean (°) | SD (°) | Median (°) | Min (°) | Max (°) | Passed Normality Test |
|---|---|---|---|---|---|---|---|
| Occlusal angle | T0 | 28.8 | 5.85 | 30.2 | 19.2 | 35.7 | No |
| Occlusal angle | T1 | 28.56 | 5.98 | 29.1 | 17.1 | 37.3 | No |
| Occlusal angle | Δ (T1 − T0) | −0.24 | 3.8 | −0.25 | −6.3 | −6.0 | Yes |
| Sagittal angle | T0 | 44.73 | 5.6 | 46.1 | 30.4 | 51.7 | No |
| Sagittal angle | T1 | 44.41 | 3.22 | 43.9 | 39.0 | 49.5 | No |
| Sagittal angle | Δ (T1 − T0) | −0.31 | 6.89 | −1.65 | −10.4 | 17.3 | No |
| Frontal angle | T0 | 90.11 | 1.61 | 89.8 | 87.2 | 92.5 | No |
| Frontal angle | T1 | 89.59 | 3.34 | 90.1 | 81.0 | 93.5 | No |
| Frontal angle | Δ (T1 − T0) | −0.52 | 3.82 | −0.1 | −8.0 | 4.8 | No |
| Upper incisors inclination | T0 | 33.4 | 2.93 | 33.3 | 28.6 | 39.6 | Yes |
| Upper incisors inclination | T1 | 34.95 | 3.86 | 34.75 | 29.2 | 44.5 | No |
| Upper incisors inclination | Δ (T1 − T0) | 1.55 | 5.89 | 2.1 | −10.4 | 12.9 | Yes |
| Variables | Mean | Standard Deviation | 95%CI | p | |
|---|---|---|---|---|---|
| AHI | T0 | 27.70 | 12.30 | 24.53–30.87 | 0.001 |
| T1 | 6.22 | 4.05 | 5.17–7.27 | ||
| ODI | T0 | 19.70 | 9.42 | 17.27–22.13 | 0.001 |
| T1 | 4.65 | 3.21 | 3.82–5.48 |
| Angle | Mean Pre-Treatment | Mean Post-Treatment | p | Statistic | df | 95% CI | Effect Size |
|---|---|---|---|---|---|---|---|
| Occlusal * | 28.80 ± 5.85° | 28.56 ± 5.98° | 0.694 | t = 0.328 | 59 | −1.2, 0.72 | −0.06 |
| Sagittal | 44.73 ± 5.6° | 44.41 ± 3.22° | 0.452 | Z = −0.53 | - | −2.05, 1.43 | −0.04 |
| Frontal | 90.11 ± 1.61° | 89.59 ± 3.34° | 0.820 | Z = −0.16 | - | −1.49, 0.45 | −0.14 |
| Upper * incisors inclination | 33.4 ± 2.93° | 34.95 ± 3.86° | 0.175 | t = −1.392 | 59 | 0.06, 3.04 | 0.26 |
| Study | Duration | Device Type/Description | Reported Changes |
|---|---|---|---|
| Ishida et al. [21] | 4 years | Custom titratable mandibular advancement device | Reduction in upper incisor inclination and overjet |
| Doff et al. [32] | 2 years | Adjustable two-piece MAD | Reduction in overjet and overbite; lower incisor proclination; upper incisor retroclination; no skeletal changes |
| Marklund et al. [33] | 2.5 ± 0.5 years | Protrusive oral appliance | Reduction in overjet and overbite; minor dentoalveolar effects |
| Chen et al. [34] | >3 years (meta-analysis) | Various long-term MADs | Reduction in overjet and overbite; upper incisor retroclination; lower incisor proclination; stable skeletal pattern; clockwise mandibular rotation |
| Linsen et al. [35] | T1: 11.9 ± 7.1 months T2: 31.9 ± 25.4 months | Wing-type vs. thrust-type MADs | 3D tooth movement; mesial occlusion; anterior open bite; decreased occlusal contacts |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lorusso, M.; Tepedino, M.; Papa, F.; Montaruli, G.; Esperouz, F.; Luciano, R.; Burlon, G.; Dioguardi, M.; Russo, L.L.; Ciavarella, D. Impact of Mandibular Advancement Therapy on Occlusal Plane Orientation and Incisor Inclination in Obstructive Sleep Apnea Patients: A Retrospcetive Observational Study. J. Clin. Med. 2025, 14, 8309. https://doi.org/10.3390/jcm14238309
Lorusso M, Tepedino M, Papa F, Montaruli G, Esperouz F, Luciano R, Burlon G, Dioguardi M, Russo LL, Ciavarella D. Impact of Mandibular Advancement Therapy on Occlusal Plane Orientation and Incisor Inclination in Obstructive Sleep Apnea Patients: A Retrospcetive Observational Study. Journal of Clinical Medicine. 2025; 14(23):8309. https://doi.org/10.3390/jcm14238309
Chicago/Turabian StyleLorusso, Mauro, Michele Tepedino, Francesca Papa, Graziano Montaruli, Fariba Esperouz, Rossella Luciano, Giuseppe Burlon, Mario Dioguardi, Lucio Lo Russo, and Domenico Ciavarella. 2025. "Impact of Mandibular Advancement Therapy on Occlusal Plane Orientation and Incisor Inclination in Obstructive Sleep Apnea Patients: A Retrospcetive Observational Study" Journal of Clinical Medicine 14, no. 23: 8309. https://doi.org/10.3390/jcm14238309
APA StyleLorusso, M., Tepedino, M., Papa, F., Montaruli, G., Esperouz, F., Luciano, R., Burlon, G., Dioguardi, M., Russo, L. L., & Ciavarella, D. (2025). Impact of Mandibular Advancement Therapy on Occlusal Plane Orientation and Incisor Inclination in Obstructive Sleep Apnea Patients: A Retrospcetive Observational Study. Journal of Clinical Medicine, 14(23), 8309. https://doi.org/10.3390/jcm14238309












