Periapical Lesion Healing After Retreatment and Root Canal Filling with a Bioceramic-Based Sealer: A Randomized Clinical Study with 1-Year Follow-Up
Abstract
1. Introduction
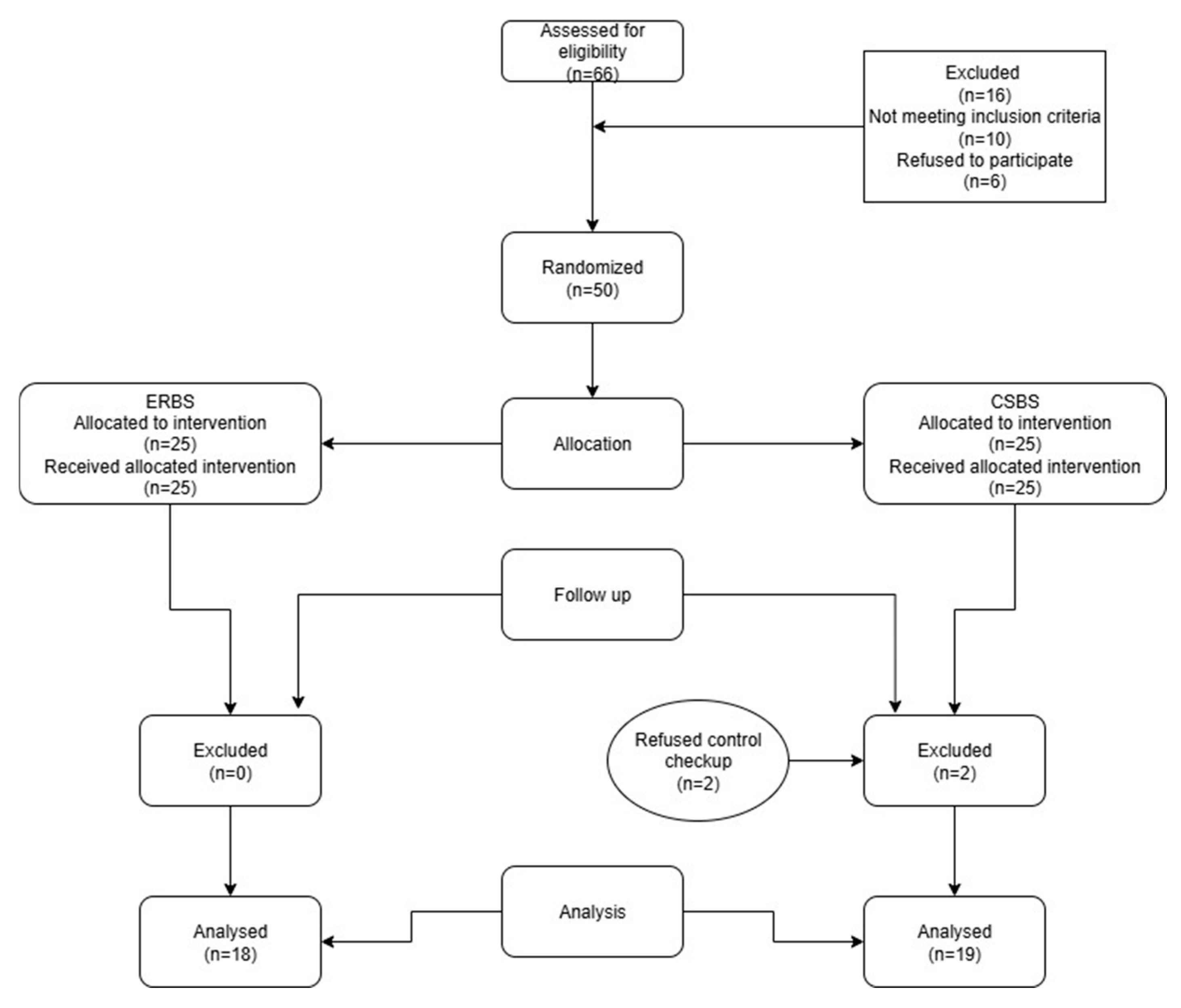
2. Materials and Methods
2.1. Study Design and Ethics
2.2. Patients
2.3. Root Canal Chemomechanical Treatment
2.4. Root Canal Obturation Protocol
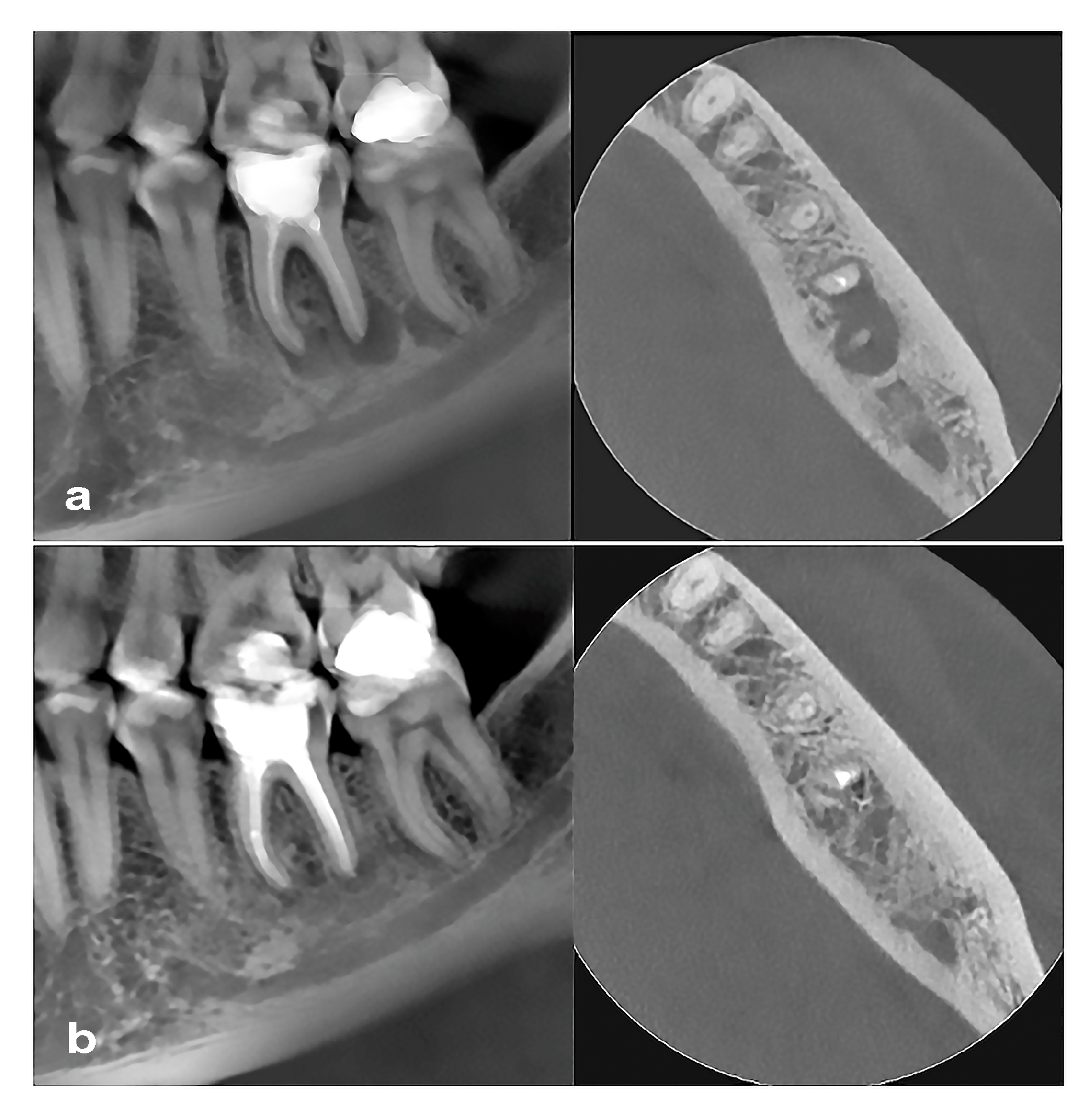
2.5. Cone Beam Computed Tomography Evaluation
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AP | Apical periodontitis |
| CBCT | Cone beam computed tomography |
| CLC | Cold lateral condensation |
| CSBSs | Calcium silicate-based sealers |
| EDTA | Ethylenediaminetetraacetic acid |
| ERBS | Epoxy resin-based sealer |
| PL | Periapical lesion |
| SC | Single cone |
| UAI | Ultrasonically activated irrigation |
| WL | Working length |
| WVC | Warm vertical compaction |
References
- Al-Haddad, A.; Che Ab Aziz, Z.A. Bioceramic-based root canal sealers: A review. Int. J. Biomater. 2016, 2016, 9753210. [Google Scholar] [CrossRef] [PubMed]
- Camilleri, J.; Atmeh, A.; Li, X.; Meschi, N. Present status and future directions: Hydraulic materials for endodontic use. Int. Endod. J. 2022, 55 (Suppl. 3), 710–777. [Google Scholar] [CrossRef]
- Cardinali, F.; Camilleri, J. A critical review of the material properties guiding the clinician’s choice of root canal sealers. Clin. Oral Investig. 2023, 27, 4147–4155. [Google Scholar] [CrossRef]
- Kwak, S.W.; Koo, J.; Song, M.; Jang, I.H.; Gambarini, G.; Kim, H.C. Physicochemical properties and biocompatibility of various bioceramic root canal sealers: In vitro study. J. Endod. 2023, 49, 871–879. [Google Scholar] [CrossRef]
- Dimitrova-Nakov, S.; Uzunoglu, E.; Ardila-Osorio, H.; Baudry, A.; Richard, G.; Kellermann, O.; Goldberg, M. In vitro bioactivity of Bioroot™ RCS, via A4 mouse pulpal stem cells. Dent. Mater. 2015, 31, 1290–1297. [Google Scholar] [CrossRef]
- Wang, Z.; Shen, Y.; Haapasalo, M. Antimicrobial and antibiofilm properties of bioceramic materials in endodontics. Materials 2021, 14, 7594. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cimpean, S.I.; Burtea, A.L.C.; Chiorean, R.S.; Dudescu, M.C.; Antoniac, A.; Robu, A.; Campian, R.S.; Timis, L.I. Evaluation of bond strength of four different root canal sealers. Materials 2022, 15, 4966. [Google Scholar] [CrossRef]
- Sfeir, G.; Zogheib, C.; Patel, S.; Giraud, T.; Nagendrababu, V.; Bukiet, F. Calcium silicate-based root canal sealers: A narrative review and clinical perspectives. Materials 2021, 14, 3965. [Google Scholar] [CrossRef] [PubMed]
- Álvarez-Vásquez, J.L.; Erazo-Guijarro, M.J.; Domínguez-Ordoñez, G.S.; Ortiz-Garay, É.M. Epoxy resin-based root canal sealers: An integrative literature review. Dent. Med. Probl. 2024, 61, 279–291. [Google Scholar] [CrossRef] [PubMed]
- Guivarc’h, M.; Jeanneau, C.; Giraud, T.; Pommel, L.; About, I.; Azim, A.A.; Bukiet, F. An international survey on the use of calcium silicate-based sealers in non-surgical endodontic treatment. Clin. Oral Investig. 2020, 24, 417–424. [Google Scholar] [CrossRef]
- Trope, M.; Bunes, A.; Debelian, G. Root filling materials and techniques: Bioceramics a new hope? Endod. Topics 2015, 32, 86–96. [Google Scholar] [CrossRef]
- Alves Silva, E.C.; Tanomaru-Filho, M.; da Silva, G.F.; Delfino, M.M.; Cerri, P.S.; Guerreiro-Tanomaru, J.M. Biocompatibility and bioactive potential of new calcium silicate–based endodontic sealers: Bio-C sealer and sealer plus BC. J. Endod. 2020, 46, 1470–1477. [Google Scholar] [CrossRef]
- da Costa Ribeiro, C.E.V.; Lena, I.M.; Santi, S.S.; Malta, C.P.; Zanatta, F.B.; Morgental, R.D. Effects of laser treatment on bond strength of epoxy resin and calcium silicate-based sealers: A systematic review and meta-analysis of in vitro studies. Clin. Oral Investig. 2024, 28, 644. [Google Scholar] [CrossRef] [PubMed]
- Ye, Y.; Hosseinpour, S.; Wen, J.; Peters, O.A. In Vitro Bioactivity and Cytotoxicity Assessment of Two Root Canal Sealers. Materials 2025, 18, 3717. [Google Scholar] [CrossRef] [PubMed]
- Ramos, R.F.; da Silva, J.C.; de Melo, M.E.F.; de Sousa, L.B.; de Oliveira, M.A.; Bispo, E.C.I.; Costa, R.A.; Martins, D.C.M.; Silva-Carvalho, A.É.; Guerra, E.N.S.; et al. Antimicrobial, toxicity, and cellular interactions of bioceramic sealers in periodontal ligament: In vitro insights. Clin. Oral Investig. 2025, 29, 505. [Google Scholar] [CrossRef] [PubMed]
- Khandelwal, A.; Janani, K.; Teja, K.; Jose, J.; Battineni, G.; Riccitiello, F.; Valletta, A.; Palanivelu, A.; Spagnuolo, G. Periapical Healing following Root Canal Treatment Using Different Endodontic Sealers: A Systematic Review. BioMed Res. Int. 2022, 2022, 3569281. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sabeti, M.A.; Karimpourtalebi, N.; Shahravan, A.; Dianat, O. Clinical and radiographic failure of nonsurgical endodontic treatment and retreatment using single-cone technique with calcium silicate-based sealers: A systematic review and meta-analysis. J. Endod. 2024, 50, 735–746.e1. [Google Scholar] [CrossRef]
- Zamparini, F.; Lenzi, J.; Duncan, H.F.; Spinelli, A.; Gandolfi, M.G.; Prati, C. The efficacy of premixed bioceramic sealers versus standard sealers on root canal treatment outcome, extrusion rate and post-obturation pain: A systematic review and meta-analysis. Int. Endod. J. 2024, 57, 1021–1042. [Google Scholar] [CrossRef] [PubMed]
- Seron, M.A.; Nunes, G.P.; Ferrisse, T.M.; Strazzi-Sahyon, H.B.; Victorino, F.R.; Dos Santos, P.H.; Gomes-Filho, J.E.; Cintra, L.T.A.; Sivieri-Araujo, G. Postoperative pain after root canal filling with bioceramic sealers: A systematic review and meta-analysis of randomized clinical trials. Odontology 2023, 111, 793–812. [Google Scholar] [CrossRef] [PubMed]
- Hopewell, S.; Chan, A.W.; Collins, G.S.; Hróbjartsson, A.; Moher, D.; Schulz, K.F.; Tunn, K.; Aggarwal, R.; Berkwits, M.; Berlin, J.A.; et al. CONSORT 2025 Statement: Updated guideline for reporting randomised trials. Lancet 2025, 405, 1633–1640. [Google Scholar] [CrossRef]
- Davies, A.; Mannocci, F.; Mitchell, P.; Andiappan, M.; Patel, S. The detection of periapical pathoses in root filled teeth using single and parallax periapical radiographs versus cone beam computed tomography—A clinical study. Int. Endod. J. 2015, 48, 582–592. [Google Scholar] [CrossRef]
- Boutsioukis, C.; Arias-Moliz, M.T. Present status and future directions—Irrigants and irrigation methods. Int. Endod. J. 2022, 55 (Suppl. 3), 588–612. [Google Scholar] [CrossRef]
- Schloss, T.; Sonntag, D.; Kohli, M.R.; Setzer, F.C. A Comparison of 2- and 3-dimensional healing assessment after endodontic surgery using cone-beam computed tomographic volumes or periapical radiographs. J. Endod. 2017, 43, 1072–1079. [Google Scholar] [CrossRef]
- Pažin, B.; Lauc, T.; Bago, I. Effect of photodynamic therapy on the healing of periapical lesions after root canal retreatment: 1-year follow up randomized clinical trial. Photodiagn. Photodyn. Ther. 2024, 45, 103907. [Google Scholar] [CrossRef]
- Šimundić Munitić, M.; Poklepović Peričić, T.; Utrobičić, A.; Bago, I.; Puljak, L. Antimicrobial efficacy of commercially available endodontic bioceramic root canal sealers: A systematic review. PLoS ONE 2019, 14, e0223575. [Google Scholar] [CrossRef]
- Bardini, G.; Casula, L.; Ambu, E.; Musu, D.; Mercadè, M.; Cotti, E. A 12-month follow-up of primary and secondary root canal treatment in teeth obturated with a hydraulic sealer. Clin. Oral Investig. 2021, 25, 2757–2764. [Google Scholar] [CrossRef]
- Li, J.; Chen, L.; Zeng, C.; Liu, Y.; Gong, Q.; Jiang, H. Clinical outcome of bioceramic sealer iRoot SP extrusion in root canal treatment: A retrospective analysis. Head Face Med. 2022, 18, 28. [Google Scholar] [CrossRef] [PubMed]
- Bardini, G.; Bellido, M.M.; Rossi-Fedele, G.; Casula, L.; Dettori, C.; Ideo, F.; Cotti, E. A 4-year follow-up of root canal obturation using a calcium silicate-based sealer and a zinc oxide-eugenol sealer: A randomized clinical trial. Int. Endod. J. 2025, 58, 193–208. [Google Scholar] [CrossRef] [PubMed]
- Simon, S.; Beauquis, J.; Colombel, H.; Dorn, A.; Marchi, V.; Robert, S.; Souleau, G.; Ravalec, N.; Huguet-Jaime, F.; Chazaud, K.; et al. Clinical efficacy of root canal treatment at 2 years using a new ready-to-use injectable calcium silicate-based sealer: A multicentric randomised controlled trial. Int. Endod. J. 2025, 58, 1420–1432. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Cho, S.Y.; Choi, Y.; Kim, D.H.; Shin, S.J.; Jung, I.Y. Clinical efficacy of sealer-based obturation using calcium silicate sealers: A randomized clinical trial. J. Endod. 2022, 48, 144–151. [Google Scholar] [CrossRef]
- Ballal, N.V.; Gandhi, P.; Shenoy, P.A.; Dummer, P.M.H. Evaluation of various irrigation activation systems to eliminate bacteria from the root canal system: A randomized controlled single blinded trial. J. Dent. 2020, 99, 103412. [Google Scholar] [CrossRef] [PubMed]
- Doğan, M.U.; Arıcıoğlu, B.; Köse, T.E.; Çıkman, A.Ş.; Öksüzer, M.Ç. Association between the irrigation-agitation techniques and Periapical Healing of large periapical lesions: A randomized controlled trial. Clin. Oral Investig. 2024, 28, 376. [Google Scholar] [CrossRef] [PubMed]
- Bidra, A.S. Evidence-based prosthodontics: Fundamental considerations, limitations, and guidelines. Dent. Clin. N. Am. 2014, 58, 1–17. [Google Scholar] [CrossRef]
- Spinelli, A.; Zamparini, F.; Lenzi, J.; Gandolfi, M.G.; Prati, C. Three-year Clinical Outcome of Root Canal Treatment Using a Single-cone Technique and Ceraseal Premixed Bioceramic Sealer: A Prospective Cohort Study. Eur. Endod. J. 2024, 9, 383–393. [Google Scholar] [CrossRef]
- Patel, S.; Mannocci, F.; Shemesh, H.; Wu, M.-K.; Wesselink, P.; Lambrechts, P. Radiographs and CBCT—time for a reassessment? Int. Endod. J. 2011, 44, 887–888. [Google Scholar] [CrossRef]
- Patel, S.; Brown, J.; Pimentel, T.; Kelly, R.D.; Abella, F.; Durack, C. Cone beam computed tomography in Endodontics—A review of the literature. Int. Endod. J. 2019, 52, 1138–1152. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Wilson, R.; Dawood, A.; Foschi, F.; Mannocci, F. The detection of periapical pathosis using digital periapical radiography and cone beam computed tomography—Part 2: A 1-year post-treatment follow-up. Int. Endod. J. 2012, 45, 711–723. [Google Scholar] [CrossRef]
| Volume of Periapical Lesion | Experimental Groups | Minimal | Maximal | Percentiles | ||
|---|---|---|---|---|---|---|
| 25th | Median | 75th | ||||
| Baseline | AH Plus | 117.71 | 15,549.9 | 188.92 | 330.16 | 975.73 |
| BioRoot RCS | 95.44 | 12,663.9 | 173.73 | 533.77 | 1284.84 | |
| At 1 year | AH Plus | 0 | 8575.65 | 0 | 30.57 | 355.34 |
| BioRoot RCS | 0 | 1068.61 | 49.52 | 110.78 | 437.44 | |
| Reduction in periapical lesion volume after 1 year (%) | AH Plus | 11.13 | 100.00 | 37.23 | 86.98 | 100.00 |
| BioRoot RCS | 6.64 | 100.00 | 34.77 | 86.95 | 91.76 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pažin, B.; Lauc, T.; Petričević, G.K.; Gabrić, D.; Bago, I. Periapical Lesion Healing After Retreatment and Root Canal Filling with a Bioceramic-Based Sealer: A Randomized Clinical Study with 1-Year Follow-Up. J. Clin. Med. 2025, 14, 8267. https://doi.org/10.3390/jcm14238267
Pažin B, Lauc T, Petričević GK, Gabrić D, Bago I. Periapical Lesion Healing After Retreatment and Root Canal Filling with a Bioceramic-Based Sealer: A Randomized Clinical Study with 1-Year Follow-Up. Journal of Clinical Medicine. 2025; 14(23):8267. https://doi.org/10.3390/jcm14238267
Chicago/Turabian StylePažin, Boris, Tomislav Lauc, Gabrijela Kapetanović Petričević, Dragana Gabrić, and Ivona Bago. 2025. "Periapical Lesion Healing After Retreatment and Root Canal Filling with a Bioceramic-Based Sealer: A Randomized Clinical Study with 1-Year Follow-Up" Journal of Clinical Medicine 14, no. 23: 8267. https://doi.org/10.3390/jcm14238267
APA StylePažin, B., Lauc, T., Petričević, G. K., Gabrić, D., & Bago, I. (2025). Periapical Lesion Healing After Retreatment and Root Canal Filling with a Bioceramic-Based Sealer: A Randomized Clinical Study with 1-Year Follow-Up. Journal of Clinical Medicine, 14(23), 8267. https://doi.org/10.3390/jcm14238267






