Comparative Evaluation of Sagittal Alignment in Total Knee Arthroplasty: Robot Sensor Versus Surgeon’s Eye and Influencing Factors
Abstract
1. Introduction
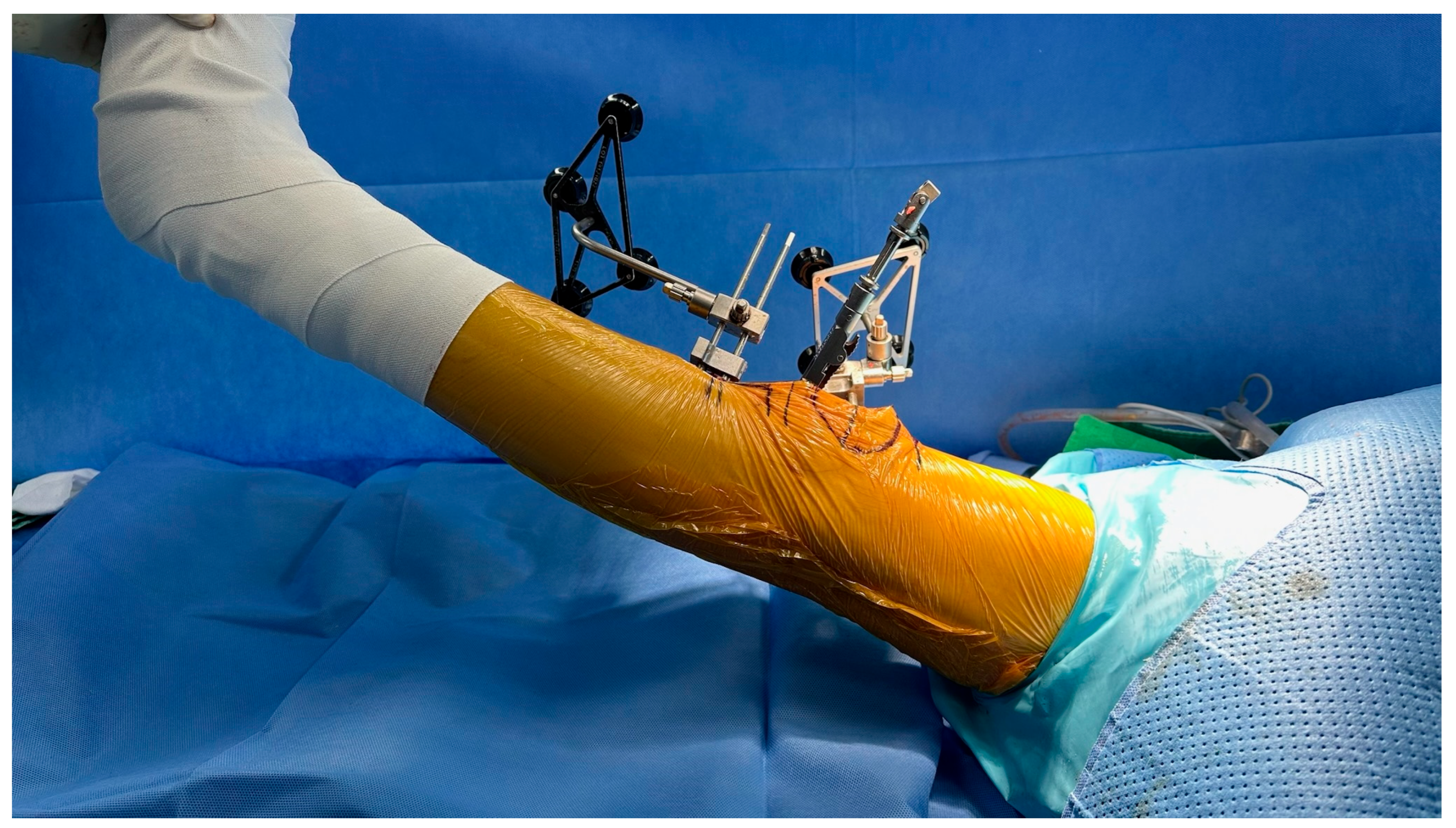
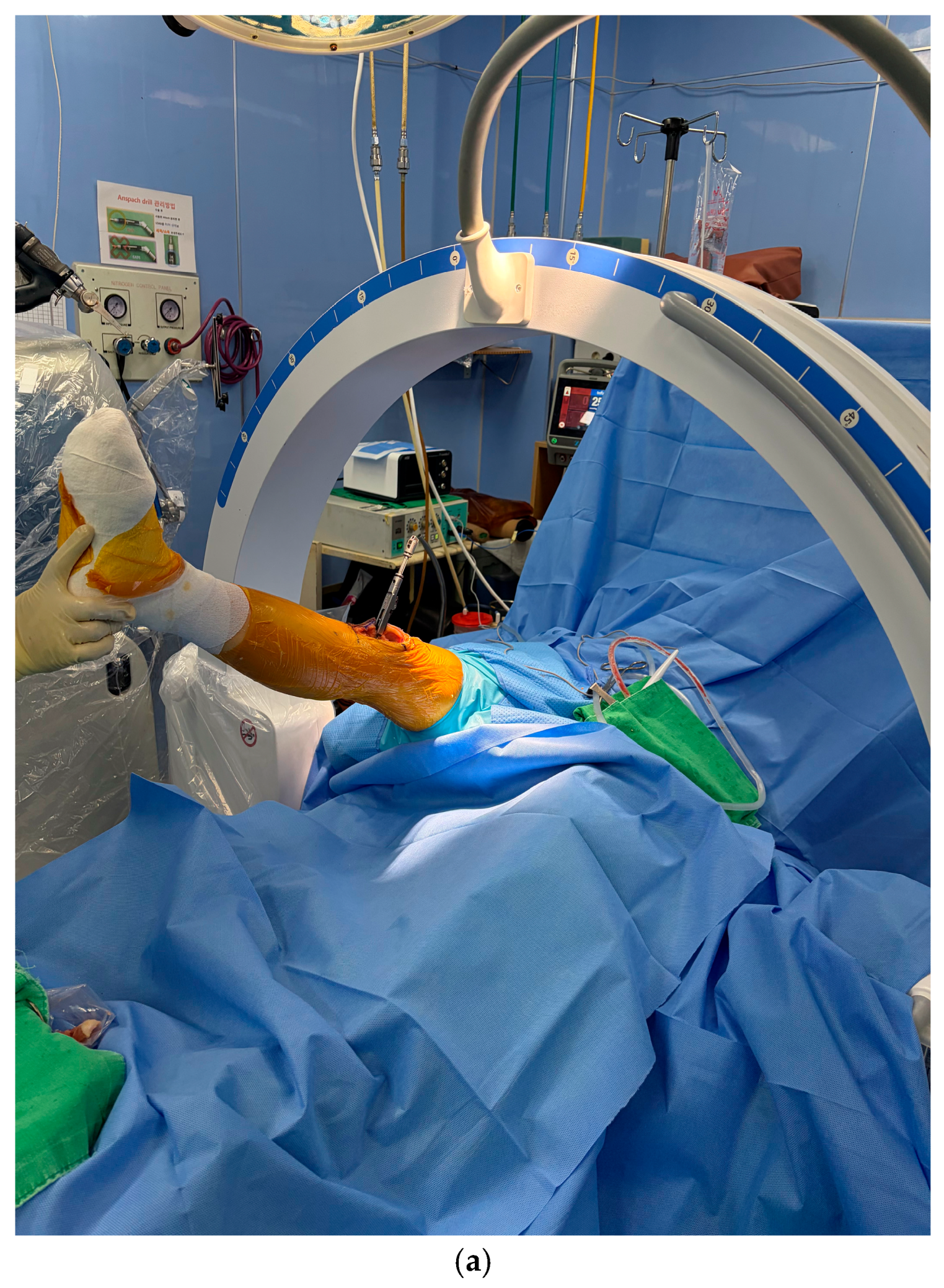
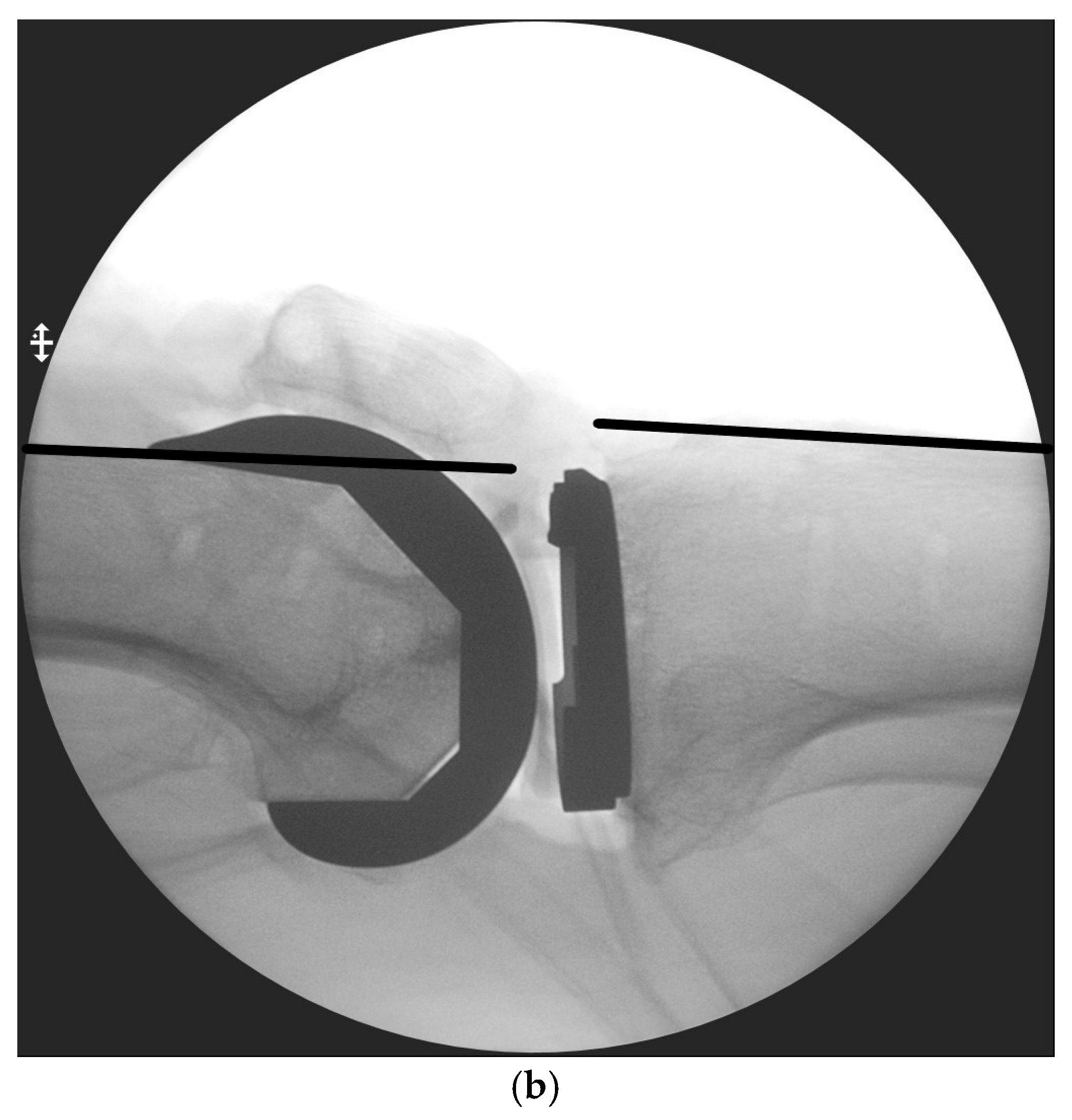
2. Materials and Methods
2.1. Ethics Statement
2.2. Statistical Analysis
3. Results
Inter-Observer Reliability (Secondary Analysis)
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TKA | Total Knee Arthroplasty |
| BMI | Body Mass Index |
| ICC | Intra-class Correlation Coefficient |
| SD | Standard Deviation |
| HKA | Hip–Knee–Ankle |
References
- Park, J.; Kim, T.W.; Kim, M.K.; Sun, J.; Bae, K.J.; Chang, M.J.; Chang, C.B.; Kang, S.-B. Analysis of Incidence and Risk Factors for Periprosthetic Fracture after Total Knee Arthroplasty in South Korea from 2010 to 2020 Based on National Registry Data. Clin. Orthop. Surg. 2025, 17, 408–416. [Google Scholar] [CrossRef]
- Carr, A.J.; Robertsson, O.; Graves, S.; Price, A.J.; Arden, N.K.; Judge, A.; Beard, D.J. Knee replacement. Lancet 2012, 379, 1331–1340. [Google Scholar] [CrossRef]
- Call, C.M.; McGrory, B.J.; Thompson, E.A.; Sommer, L.G.; Savadove, T.S. Treatment of Postoperative Instability Following Total Knee Arthroplasty in Patients With Parkinson’s Disease. Arthroplast. Today 2024, 25, 101273. [Google Scholar] [CrossRef]
- Mortazavi, S.M.J.; Razzaghof, M.; Noori, A.; Okati, A. Late-Onset De Novo Genu Recurvatum after Primary Total Knee Arthroplasty: A Potential Indication for Isolated Polyethylene Exchange. Arthroplast. Today 2020, 6, 492–495. [Google Scholar] [CrossRef]
- Sappey-Marinier, E.; Fernandez, A.; Shatrov, J.; Batailler, C.; Servien, E.; Huten, D.; Lustig, S. Management of fixed flexion contracture in primary total knee arthroplasty: Recent systematic review. SICOT-J. 2024, 10, 11. [Google Scholar] [CrossRef] [PubMed]
- Kazarian, G.S.; Lawrie, C.M.; Barrack, T.N.; Donaldson, M.J.; Miller, G.M.; Haddad, F.S.; Barrack, R.L. The Impact of Surgeon Volume and Training Status on Implant Alignment in Total Knee Arthroplasty. J. Bone Jt. Surg. Am. 2019, 101, 1713–1723. [Google Scholar] [CrossRef] [PubMed]
- Zaidi, F.; Goplen, C.M.; Bolam, S.M.; Monk, A.P. Accuracy and Outcomes of a Novel Cut-Block Positioning Robotic-Arm Assisted System for Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. Arthroplast. Today 2024, 29, 101451. [Google Scholar] [CrossRef]
- Sun, C.; Ma, Q.; Zhang, X.; Li, H.; Yang, X.; Cai, X. Improved alignment accuracy but similar early clinical outcomes with NAVIO imageless robotic-assisted vs. conventional total knee arthroplasty: A meta-analysis. J. Orthop. Surg. Res. 2025, 20, 619. [Google Scholar] [CrossRef]
- Sodhi, K.; Eaton-Brown, J.; Kumar, P.R.; Adebayo, O.; Searle, H.K.; Metcalfe, A.J.; Davis, E.T.; Khatri, C. Robotic-assisted total knee arthroplasty with MAKO is associated with improved functional outcomes: A systematic review and meta-analysis. Bone Jt. Open 2025, 6, 1382–1393. [Google Scholar] [CrossRef] [PubMed]
- Jeong, C.; Noh, J.H. Clinical and Radiological Analysis of Angular Deformity of Lower Extremities. J. Korean Fract. Soc. 2017, 30, 156–166. [Google Scholar] [CrossRef]
- van de Graaf, V.A.; Shen, T.S.; Wood, J.A.; Chen, D.B.; MacDessi, S.J. Addressing sagittal plane imbalance in primary total knee arthroplasty. Bone Jt. Open 2024, 5, 681–687. [Google Scholar] [CrossRef]
- Ritter, M.A.; Lutgring, J.D.; Davis, K.E.; Berend, M.E.; Pierson, J.L.; Meneghini, R.M. The role of flexion contracture on outcomes in primary total knee arthroplasty. J. Arthroplast. 2007, 22, 1092–1096. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Park, Y.B.; Lee, D.H.; Kim, K.H.; Ham, D.W.; Kim, S.H. Risk factors of hyperextension and its relationship with the clinical outcomes following mobile-bearing total knee arthroplasty. Arch. Orthop. Trauma Surg. 2019, 139, 1293–1305. [Google Scholar] [CrossRef]
- Laoruengthana, A.; Rattanaprichavej, P.; Suangyanon, P.; Galassi, M.; Teekaweerakit, P.; Pongpirul, K. Hyperextension following two different designs of fixed-bearing posterior-stabilized total knee arthroplasty. Eur. J. Orthop. Surg. Traumatol. 2022, 32, 1641–1650. [Google Scholar] [CrossRef]
- Zondervan, R.L.; Riggle, P.K.; Cien, A.J.; Penny, P.C.; Cochran, J.M. Postoperative Supine Sleeping Position Following Total Knee Arthroplasty Decreases Knee Flexion Contractures. Spartan Med. Res. J. 2024, 9, 35–42. [Google Scholar] [CrossRef]
- Koh, I.J.; Chang, C.B.; Kang, Y.G.; Seong, S.C.; Kim, T.K. Incidence, predictors, and effects of residual flexion contracture on clinical outcomes of total knee arthroplasty. J. Arthroplast. 2013, 28, 585–590. [Google Scholar] [CrossRef]
- Seo, J.-G.; Kim, B.-K.; Moon, Y.-W.; Kim, J.-H.; Yoon, B.-H.; Ahn, T.-K.; Lee, D.-H. Bony landmarks for determining the mechanical axis of the femur in the sagittal plane during total knee arthroplasty. Clin. Orthop. Surg. 2009, 1, 128–131. [Google Scholar] [CrossRef]
- Jacobs, C.A.; Christensen, C.P.; Hester, P.W.; Burandt, D.M.; Sciascia, A.D. Errors in visual estimation of flexion contractures during total knee arthroplasty. World J. Orthop. 2013, 4, 120–123. [Google Scholar] [CrossRef]
- Mako Total Knee 2.0 SmartRobotics Functional Knee Positioning; Stryker: Kalamazoo, MI, USA, 2023.
- MAKO TKA Application User Guide; Stryker: Kalamazoo, MI, USA, 2025.
- Richardson, M.K.; DiGiovanni, R.M.; McCrae, B.K., Jr.; Cooperman, W.S.; Ludington, J.; Heckmann, N.D.; Oakes, D.A. Robotic-Assisted Total Knee Arthroplasty in Obese Patients. Arthroplast. Today 2024, 26, 101320. [Google Scholar] [CrossRef] [PubMed]
- Kanna, R.; Brasanna, A.; Shetty, G.M.; Ravichandran, C. No influence of obesity on mid-term clinical, functional, and radiological results after computer-navigated total knee arthroplasty using a gap balancing technique. J. Clin. Orthop. Trauma 2021, 16, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Sekeitto, A.R.; McGale, J.G.; Montgomery, L.A.; Vasarhelyi, E.M.; Willing, R.; Lanting, B.A. Posterior-stabilized total knee arthroplasty kinematics and joint laxity: A hybrid biomechanical study. Arthroplasty 2022, 4, 53. [Google Scholar] [CrossRef] [PubMed]


| Normal-Weight Group (BMI < 25 kg/m2) | Overweight/Obesity Group (BMI ≥ 25 kg/m2) | p-Value | |
|---|---|---|---|
| Number of cases | 28 | 32 | |
| Age (years) | 73.1 (±5.8) | 72.4 (±8.0) | 0.676 |
| BMI (kg/m2) | 22.9 (±1.3) | 28.8 (±1.6) | <0.0001 |
| Preoperative HKA (°) | 8.1 (±3.3) | 8.5 (±3.4) | 0.668 |
| Preoperative tibia/femur length ratio | 0.4 (±0.2) | 0.4 (±0.2) | 0.186 |
| Preoperative height/lower extremity length ratio | 0.2 (±0.0) | 0.2 (±0.0) | 0.182 |
| Thigh circumference (cm) | 45.4 (±3.3) | 48.5 (±4.2) | 0.002 |
| Normal-Weight Group | p-Value | Overweight/Obesity Group | p-Value | |
|---|---|---|---|---|
| C-arm (°) | 3.4 (±3.4) | 0.095 | 2.6 (±2.7) | <0.0001 |
| Surgeon’s eyes (°) | 2.0 (±2.7) | 0.1 (±2.7) | ||
| C-arm (°) | 3.4 (±3.4) | 0.437 | 2.6 (±2.7) | 0.607 |
| MAKO (°) | 2.7 (±3.8) | 3.0 (±3.0) |
| Insert Thickness | Alignment (°) | Surgeon’s Eyes, n (%) | MAKO, n (%) | Match:Mismatch (%, n) | p-Value |
|---|---|---|---|---|---|
| 9 mm | 0° | 34 (56.7) | 7 (11.7) | 27:33 (45.0:55.0) | <0.0001 |
| >0° (FC) | 7 (11.7) | 35 (58.3) | |||
| <0° (HE) | 19 (31.7) | 18 (30.0) | |||
| 10 mm | 0° | 12 (20.0) | 10 (16.7) | 38:22 (63.3:36.7) | 0.05 |
| >0° (FC) | 34 (56.7) | 45 (75.0) | |||
| <0° (HE) | 14 (23.3) | 5 (8.3) | |||
| 11 mm | 0° | 12 (20.0) | 0 (0.0) | 45:15 (75.0:25.0) | <0.0001 |
| >0° (FC) | 42 (70.0) | 55 (91.7) | |||
| <0° (HE) | 6 (10.0) | 5 (8.3) |
| Insert (Stratum) | Category | Surgeon’s Eyes, n (%) | MAKO, n (%) | Match:Mismatch (n, %) | p-Value |
|---|---|---|---|---|---|
| 9 mm | <5° flexion | 41 (68.3) | 37 (61.7) | 44:16 (73.3:26.7) | 0.098 |
| ≥5° flexion | 0 (0.0) | 5 (8.3) | |||
| <0° hyperextension | 19 (31.7) | 18 (30.0) | |||
| 10 mm | <5° flexion | 45 (75.0) | 37 (61.7) | 34:26 (56.7:43.3) | <0.0001 |
| ≥5° flexion | 1 (1.1) | 18 (30.0) | |||
| <0° hyperextension | 14 (23.3) | 5 (8.3) | |||
| 11 mm | <5° flexion | 37 (61.7) | 18 (30.0) | 32:28 (53.3:46.7) | 0.001 |
| ≥5° flexion | 17 (28.3) | 37 (61.7) | |||
| <0° hyperextension | 6 (10.0) | 5 (8.3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, D.N.; Nam, C.H.; Baek, J.-H.; Ryu, S.; Heo, J.; Kim, J.H.; Lee, S.C.; Lee, S.W. Comparative Evaluation of Sagittal Alignment in Total Knee Arthroplasty: Robot Sensor Versus Surgeon’s Eye and Influencing Factors. J. Clin. Med. 2025, 14, 8242. https://doi.org/10.3390/jcm14228242
Lee DN, Nam CH, Baek J-H, Ryu S, Heo J, Kim JH, Lee SC, Lee SW. Comparative Evaluation of Sagittal Alignment in Total Knee Arthroplasty: Robot Sensor Versus Surgeon’s Eye and Influencing Factors. Journal of Clinical Medicine. 2025; 14(22):8242. https://doi.org/10.3390/jcm14228242
Chicago/Turabian StyleLee, Dong Nyoung, Chang Hyun Nam, Ji-Hoon Baek, Suengryol Ryu, Juneyoung Heo, Ji Hyun Kim, Su Chan Lee, and Sang Won Lee. 2025. "Comparative Evaluation of Sagittal Alignment in Total Knee Arthroplasty: Robot Sensor Versus Surgeon’s Eye and Influencing Factors" Journal of Clinical Medicine 14, no. 22: 8242. https://doi.org/10.3390/jcm14228242
APA StyleLee, D. N., Nam, C. H., Baek, J.-H., Ryu, S., Heo, J., Kim, J. H., Lee, S. C., & Lee, S. W. (2025). Comparative Evaluation of Sagittal Alignment in Total Knee Arthroplasty: Robot Sensor Versus Surgeon’s Eye and Influencing Factors. Journal of Clinical Medicine, 14(22), 8242. https://doi.org/10.3390/jcm14228242






