Preoperative Radiographic Thoracic Kyphosis Relates to Scapular Internal Rotation but Not Anterior Tilt in Candidates for Reverse Shoulder Arthroplasty: A Retrospective Radiographic Analysis from the FP-UCBM Shoulder Study Group
Abstract
1. Introduction
2. Materials and Methods
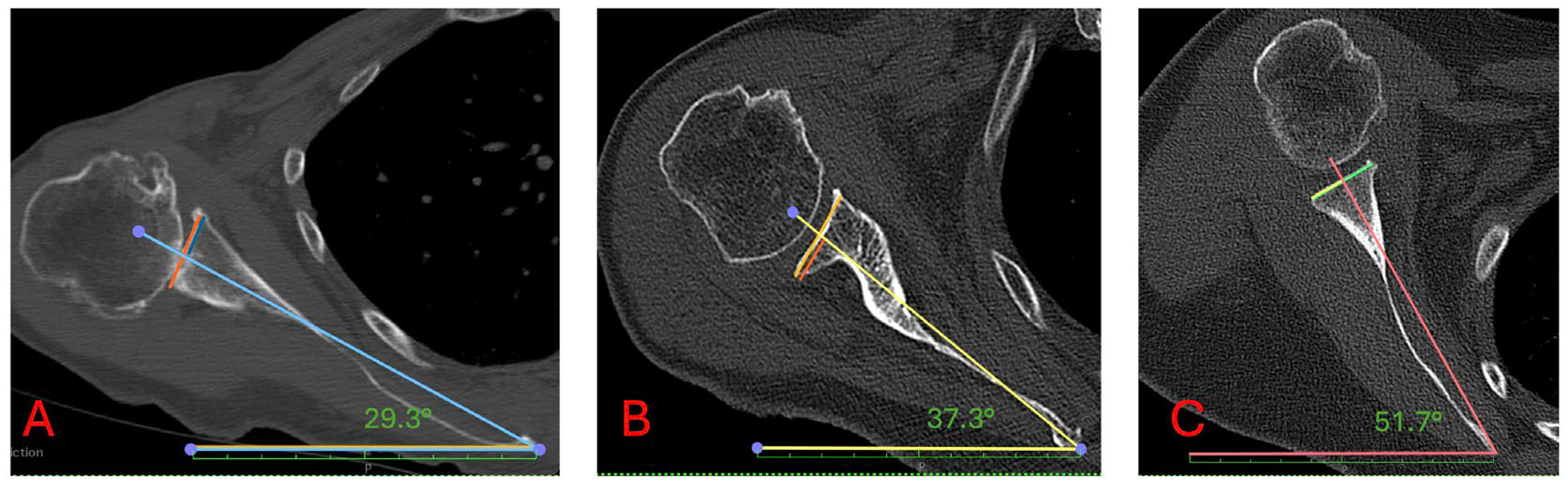
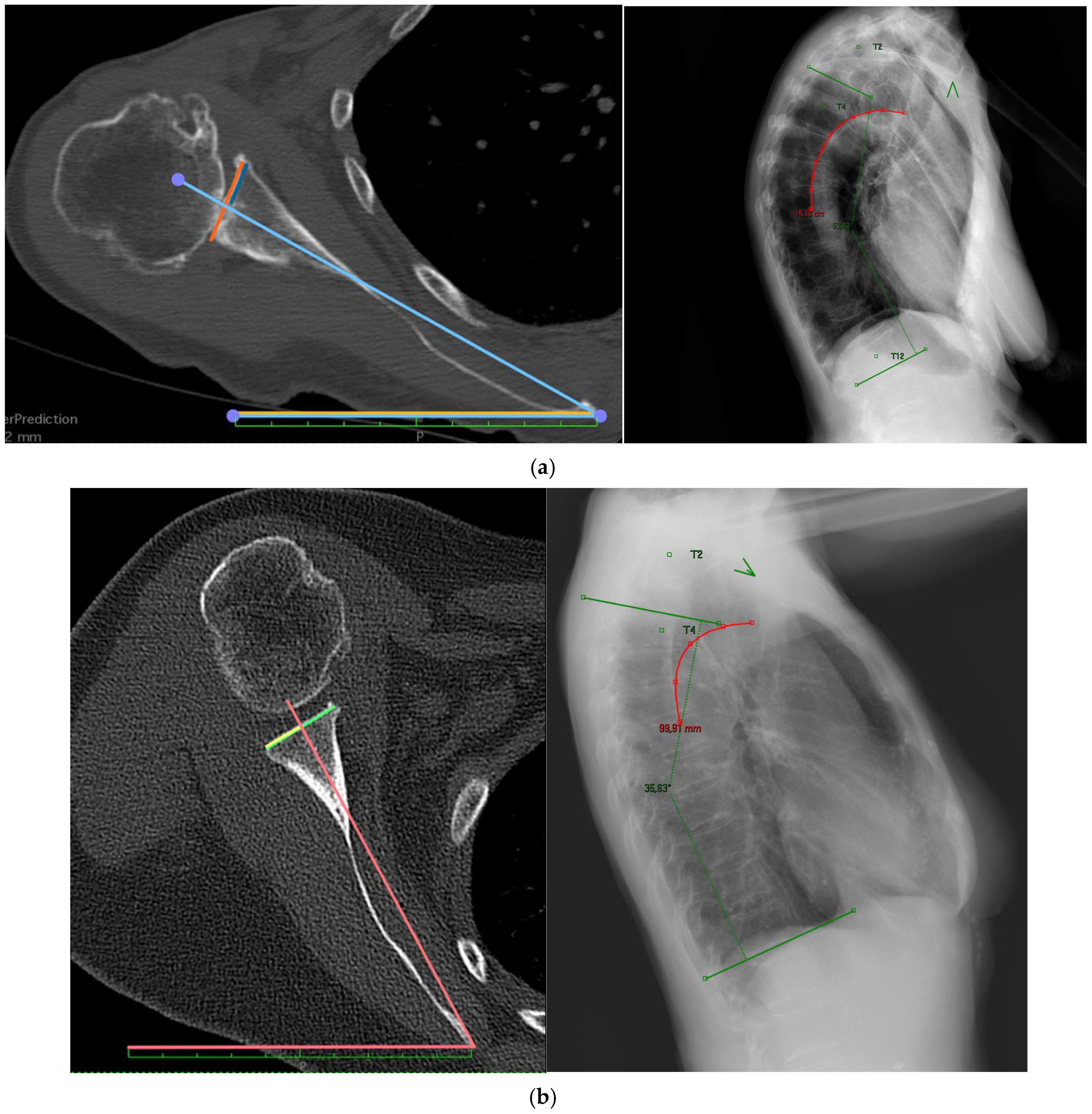
2.1. Radiological Analysis
2.2. Data Analysis
3. Results
3.1. Radiographic Measurements
3.2. Group Comparisons
3.3. Correlation Analyses
- In Group A, the correlation coefficient was R = 0.235 (p = 0.094),
- In Group B, R = 0.046 (p = 0.718),
- In Group C, R = 0.158 (p = 0.278).
3.4. Demographic Influences
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| RSA | Reverse shoulder arthroplasty |
| SIR | Scapular internal rotation |
| SD | Standard deviation |
| BMI | Body mass index |
References
- Pollock, R.G.; Deliz, E.D.; McIlveen, S.J.; Flatow, E.L.; Bigliani, L.U. Prosthetic replacement in rotator cuff—Deficient shoulders. J. Shoulder Elb. Surg. 1992, 1, 173–186. [Google Scholar] [CrossRef] [PubMed]
- Flatow, E.L.; Harrison, A.K. A History of Reverse Total Shoulder Arthroplasty. Clin. Orthop. 2011, 469, 2432–2439. [Google Scholar] [CrossRef] [PubMed]
- Khan, W.S.; Longo, U.G.; Ahrens, P.M.; Denaro, V.; Maffulli, N. A systematic review of the reverse shoulder replacement in rotator cuff arthropathy, rotator cuff tears, and rheumatoid arthritis. Sports Med. Arthrosc. Rev. 2011, 19, 366–379. [Google Scholar] [CrossRef]
- Franceschetti, E.; Giovannetti De Sanctis, E.; Gregori, P.; Paciotti, M.; Palumbo, A.; Franceschi, F. Angled BIO-RSA leads to better inclination and clinical outcomes compared to Standard BIO-RSA and eccentric reaming: A comparative study. Shoulder Elb. 2023, 15, 35–42. [Google Scholar] [CrossRef]
- Sulkar, H.J.; Aliaj, K.; Tashjian, R.Z.; Chalmers, P.N.; Foreman, K.B.; Henninger, H.B. High and low performers in internal rotation after reverse total shoulder arthroplasty: A biplane fluoroscopic study. J. Shoulder Elb. Surg. 2023, 32, e133–e144. [Google Scholar] [CrossRef]
- Hochreiter, B.; Hasler, A.; Hasler, J.; Kriechling, P.; Borbas, P.; Gerber, C. Factors influencing functional internal rotation after reverse total shoulder arthroplasty. JSES Int. 2021, 5, 679–687. [Google Scholar] [CrossRef]
- Kim, H.M.; Nguyen, M.; Groneck, A. Internal rotation limitation is prevalent following modern reverse shoulder arthroplasty and negatively affects patients’ subjective rating of the procedure. J. Shoulder Elb. Surg. 2024, 33, 2646–2654. [Google Scholar] [CrossRef]
- Franceschetti, E.; Gregori, P.; De Giorgi, S.; Martire, T.; Za, P.; Papalia, G.F.; Giurazza, G.; Longo, U.G.; Papalia, R. Machine learning can predict anterior elevation after reverse total shoulder arthroplasty: A new tool for daily outpatient clinic? Musculoskelet. Surg. 2024, 108, 163–171. [Google Scholar] [CrossRef]
- Bauer, S.; Blakeney, W.G.; Wang, A.W.; Ernstbrunner, L.; Corbaz, J.; Werthel, J.-D. Challenges for Optimization of Reverse Shoulder Arthroplasty Part II: Subacromial Space, Scapular Posture, Moment Arms and Muscle Tensioning. J. Clin. Med. 2023, 12, 1616. [Google Scholar] [CrossRef]
- Roche, C.P. Reverse Shoulder Arthroplasty Biomechanics. J. Funct. Morphol. Kinesiol. 2022, 7, 13. [Google Scholar] [CrossRef]
- Franceschetti, E.; Perricone, G.; De Rosa, A.; Tanzilli, A.; Gregori, P.; Giurazza, G.; Zampogna, B.; Shanmugasundaram, S.; Papalia, R. Eccentricity and greater size of the glenosphere increase impingement-free range of motion in glenoid lateralized reverse shoulder arthroplasty: A computational study. J. Clin. Orthop. Trauma. 2024, 56, 102527. [Google Scholar] [CrossRef] [PubMed]
- Sheth, M.; Kitziger, R.; Shah, A.A. Understanding loss of internal rotation after reverse shoulder arthroplasty: A narrative review of current literature. JSES Rev. Rep. Tech. 2024, 4, 647–653. [Google Scholar] [CrossRef] [PubMed]
- Polisetty, T.; Lohre, R.; Glass, E.A.; Swanson, D.P.; Bowler, A.R.; Vancleef, S.; Bartels, W.; Elmallah, R.; Elhassan, B.; Kirsch, J.M.; et al. Three-dimensional scapular orientation: A comparison of glenohumeral osteoarthritis and cuff tear arthropathy to the unaffected shoulder. Semin. Arthroplast. JSES 2024, 34, 639–647. [Google Scholar] [CrossRef]
- Sun, B.; Grad, J.; Liu, W.; Nam, D.; Sheth, U. The impact of scapular posture and sagittal spine alignment on motion and functional outcomes following reverse total shoulder arthroplasty: A scoping review. JSES Int. 2024, 8, 859–865. [Google Scholar] [CrossRef]
- Moroder, P.; Akgün, D.; Plachel, F.; Baur, A.D.J.; Siegert, P. The influence of posture and scapulothoracic orientation on the choice of humeral component retrotorsion in reverse total shoulder arthroplasty. J. Shoulder Elb. Surg. 2020, 29, 1992–2001. [Google Scholar] [CrossRef]
- Moroder, P.; Poltaretskyi, S.; Raiss, P.; Denard, P.J.; Werner, B.C.; Erickson, B.J.; Griffin, J.W.; Metcalfe, N.; Siegert, P. SECEC Grammont Award 2024: The critical role of posture adjustment for range of motion simulation in reverse total shoulder arthroplasty preoperative planning. Bone Jt. J. 2024, 106-B, 1284–1292. [Google Scholar] [CrossRef]
- Franceschetti, E.; Gregori, P.; de Sanctis, E.G.; Palumbo, A.; Paciotti, M.; Maffulli, N.M.; Franceschi, F. Return to Sport After Total Shoulder Arthroplasty and Hemiarthroplasty: A Systematic Review. Sports Med. Arthrosc. Rev. 2023, 31, 27–32. [Google Scholar] [CrossRef]
- Moroder, P.; Siegert, P.; Coifman, I.; Rüttershoff, K.; Spagna, G.; Scaini, A.; Weber, B.; Schneller, T.; Scheibel, M.; Audigé, L. Scapulothoracic orientation has a significant influence on the clinical outcome after reverse total shoulder arthroplasty. J. Shoulder Elb. Surg. 2024, 33, 2159–2170. [Google Scholar] [CrossRef]
- Constant, C.R.; Murley, A.H. A clinical method of functional assessment of the shoulder. Clin. Orthop. 1987, 214, 160–164. [Google Scholar] [CrossRef]
- Siegert, P.; Meraner, D.; Pokorny-Olsen, A.; Akgün, D.; Korn, G.; Albrecht, C.; Hofstaetter, J.G.; Moroder, P. Practical considerations for determination of scapular internal rotation and its relevance in reverse total shoulder arthroplasty planning. J. Orthop. Surg. 2023, 18, 279. [Google Scholar] [CrossRef]
- Moroder, P.; Urvoy, M.M.; Raiss, P.; Werthel, J.-D.; Akgün, D.; Chaoui, J.; Siegert, P. Patient Posture Affects Simulated ROM in Reverse Total Shoulder Arthroplasty: A Modeling Study Using Preoperative Planning Software. Clin. Orthop. 2022, 480, 619–631. [Google Scholar] [CrossRef]
- Jassim, S.S.; Ernstbrunner, L.; Ek, E.T. Does Humeral Component Version Affect Range of Motion and Clinical Outcomes in Reverse Total Shoulder Arthroplasty? A Systematic Review. J. Clin. Med. 2021, 10, 5745. [Google Scholar] [CrossRef]
- Moroder, P.; Danzinger, V.; Maziak, N.; Plachel, F.; Pauly, S.; Scheibel, M.; Minkus, M. Characteristics of functional shoulder instability. J. Shoulder Elb. Surg. 2020, 29, 68–78. [Google Scholar] [CrossRef]
- Reintgen, C.; Armington, S.; Vigan, M.; Werthel, J.-D.; Patrick, M.; King, J.; Wright, T.; Schoch, B. Influence of Thoracic Kyphosis on Reverse Total Shoulder Arthroplasty Outcomes. J. Am. Acad. Orthop. Surg. 2021, 29, 840–847. [Google Scholar] [CrossRef]
- Quek, J.; Pua, Y.-H.; Clark, R.A.; Bryant, A.L. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Man. Ther. 2013, 18, 65–71. [Google Scholar] [CrossRef]
- Lädermann, A.; Gueorguiev, B.; Charbonnier, C.; Stimec, B.V.; Fasel, J.H.; Zderic, I.; Hagen, J.; Walch, G. Scapular Notching on Kinematic Simulated Range of Motion After Reverse Shoulder Arthroplasty Is Not the Result of Impingement in Adduction. Medicine 2015, 94, e1615. [Google Scholar] [CrossRef]
- Gauci, M.-O.; Chaoui, J.; Berhouet, J.; Jacquot, A.; Walch, G.; Boileau, P. Can surgeons optimize range of motion and reduce scapulohumeral impingements in reverse shoulder arthroplasty? A computational study. Shoulder Elb. 2022, 14, 385–394. [Google Scholar] [CrossRef] [PubMed]
| Female | 113 (68.9%) |
|---|---|
| Age | 70.4 (9.5) |
| BMI | 28.0 (6.3) |
| Right shoulder | 115 (70.1%) |
| BMI: Body Mass Index; mean (SD) | 28.0 kg/m2 (SD 6.3) |
| Cobb Angle | Scapular Internal Rotation | Anterior Scapular Tilt |
|---|---|---|
| 40.7 (12.4) | 41.9 (8.4) | 24.1 (13.3) |
| Cobb Angle | Scapular Internal Rotation (Mean (SD)) | p-Value | Anterior Scapular Tilt (Mean (SD)) | p-Value |
|---|---|---|---|---|
| ≤36 | 40.3 (9.3) | 0.047 | 25.8 (13.0) | 0.570 |
| >36–46 | 41.8 (7.8) | 23.3 (12.5) | ||
| ≥47 | 43.7 (8.0) | 23.5 (14.8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Franceschetti, E.; Gregori, P.; Capperucci, C.; La Bruna, M.; Giurazza, G.; Tanzilli, A.; Paciotti, M.; Amato, C.; Longo, U.G.; Papalia, R. Preoperative Radiographic Thoracic Kyphosis Relates to Scapular Internal Rotation but Not Anterior Tilt in Candidates for Reverse Shoulder Arthroplasty: A Retrospective Radiographic Analysis from the FP-UCBM Shoulder Study Group. J. Clin. Med. 2025, 14, 8183. https://doi.org/10.3390/jcm14228183
Franceschetti E, Gregori P, Capperucci C, La Bruna M, Giurazza G, Tanzilli A, Paciotti M, Amato C, Longo UG, Papalia R. Preoperative Radiographic Thoracic Kyphosis Relates to Scapular Internal Rotation but Not Anterior Tilt in Candidates for Reverse Shoulder Arthroplasty: A Retrospective Radiographic Analysis from the FP-UCBM Shoulder Study Group. Journal of Clinical Medicine. 2025; 14(22):8183. https://doi.org/10.3390/jcm14228183
Chicago/Turabian StyleFranceschetti, Edoardo, Pietro Gregori, Chiara Capperucci, Mauro La Bruna, Giancarlo Giurazza, Andrea Tanzilli, Michele Paciotti, Cirino Amato, Umile Giuseppe Longo, and Rocco Papalia. 2025. "Preoperative Radiographic Thoracic Kyphosis Relates to Scapular Internal Rotation but Not Anterior Tilt in Candidates for Reverse Shoulder Arthroplasty: A Retrospective Radiographic Analysis from the FP-UCBM Shoulder Study Group" Journal of Clinical Medicine 14, no. 22: 8183. https://doi.org/10.3390/jcm14228183
APA StyleFranceschetti, E., Gregori, P., Capperucci, C., La Bruna, M., Giurazza, G., Tanzilli, A., Paciotti, M., Amato, C., Longo, U. G., & Papalia, R. (2025). Preoperative Radiographic Thoracic Kyphosis Relates to Scapular Internal Rotation but Not Anterior Tilt in Candidates for Reverse Shoulder Arthroplasty: A Retrospective Radiographic Analysis from the FP-UCBM Shoulder Study Group. Journal of Clinical Medicine, 14(22), 8183. https://doi.org/10.3390/jcm14228183









