Cement Leakage in Cement-Augmented Fenestrated Pedicle Screws for Osteoporotic Spine: Risk Stratification with Quantitative Computed Tomography Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Approval
2.2. Patient Selection and Inclusion Criteria
2.3. Surgical Procedure and Cement Injection Protocol
2.4. CT Evaluation and Definition of Cement Leakage
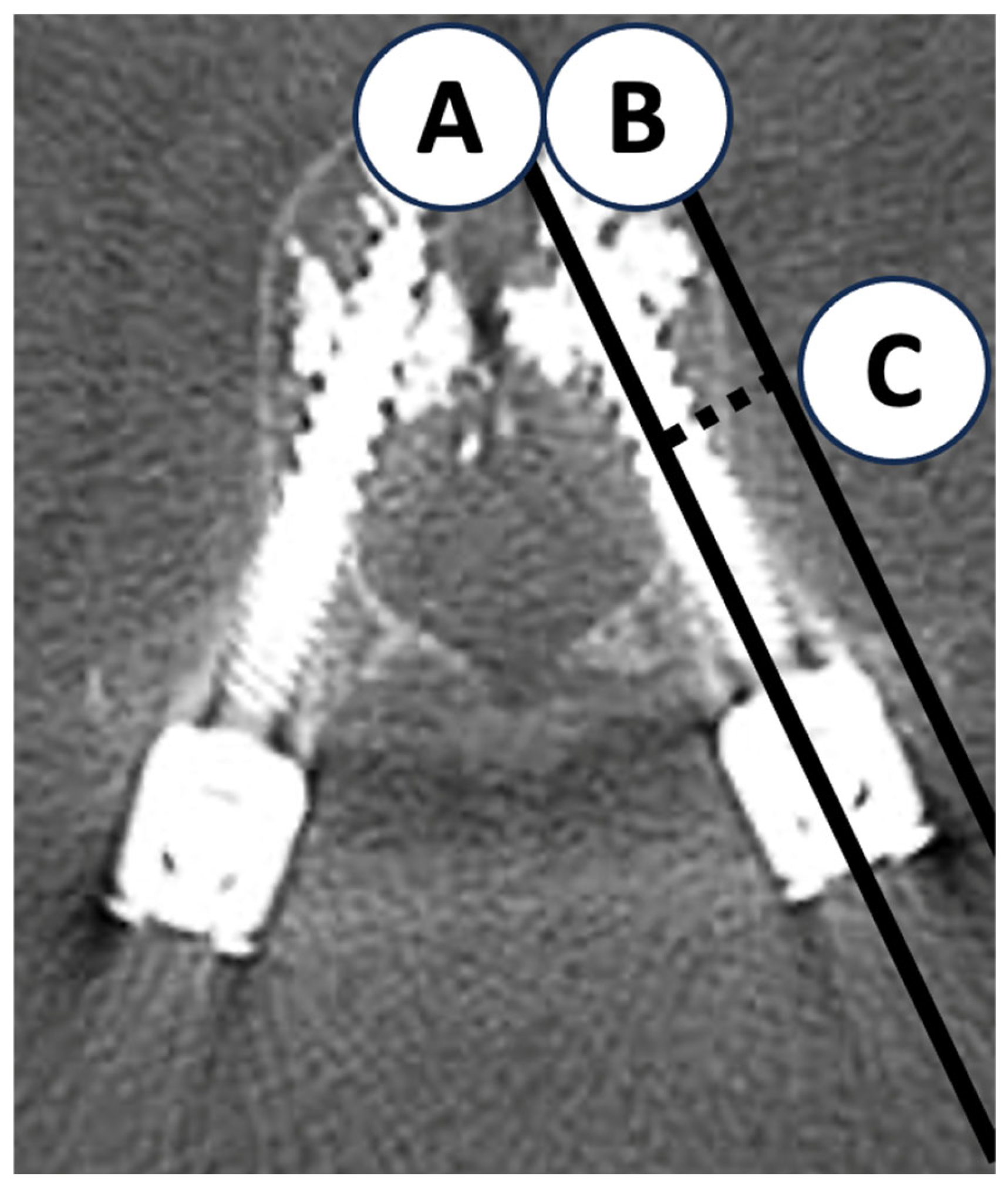
2.5. Quantitative Measurements
2.6. Statistical Analysis and Sample Size Estimation
3. Results
3.1. Patient and Screw Characteristics
3.2. Frequency and Distribution of Cement Leakage
3.3. Univariate and Multivariate Logistic Regression Analyses
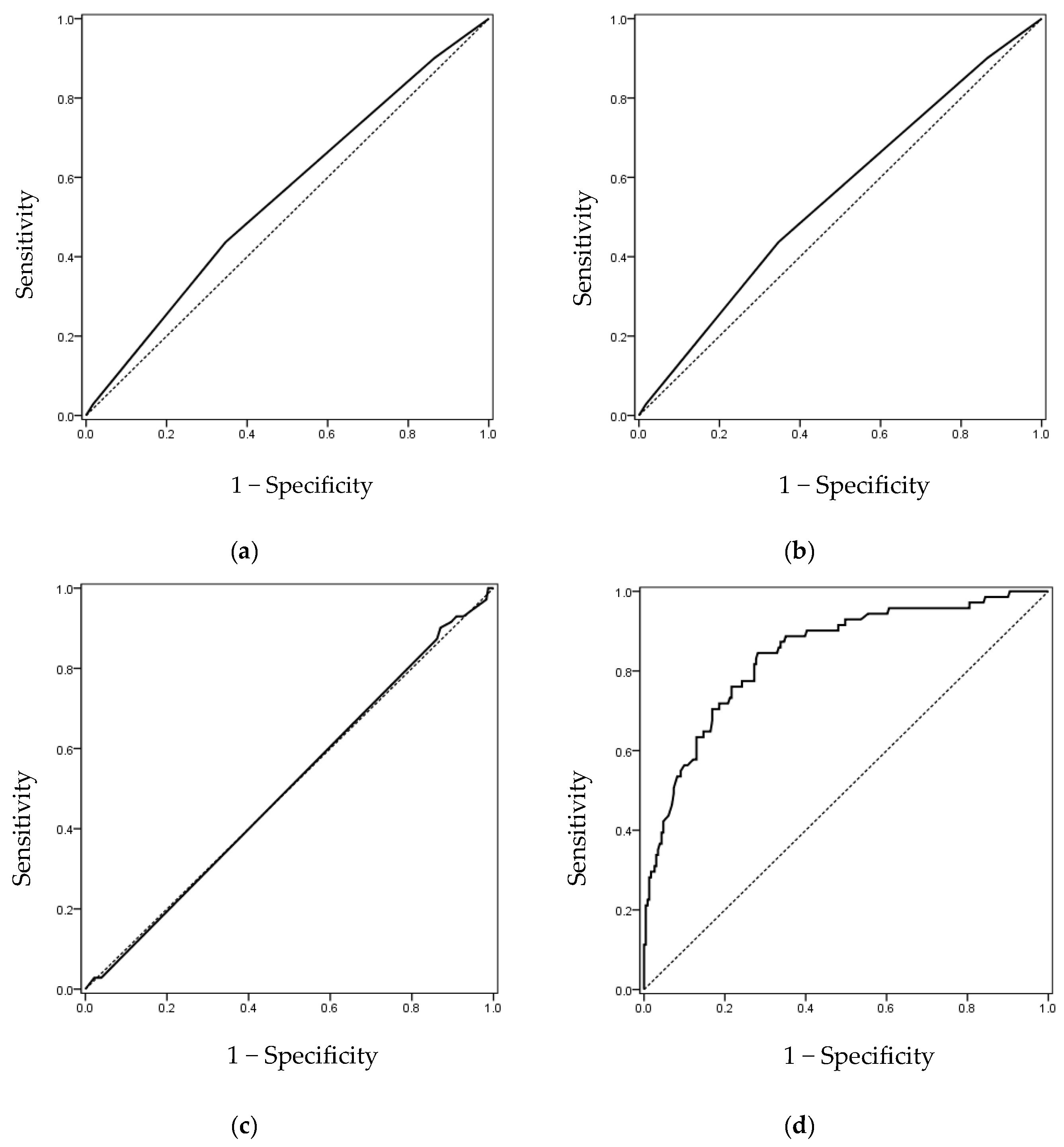
3.4. Receiver Operating Characteristic Curve Analysis at the Screw Level
3.5. Analysis at the Vertebral Level (HU Values)
3.6. Analysis at the Patient Level (Age and Sex)
3.7. Interaction and Collinearity Analysis
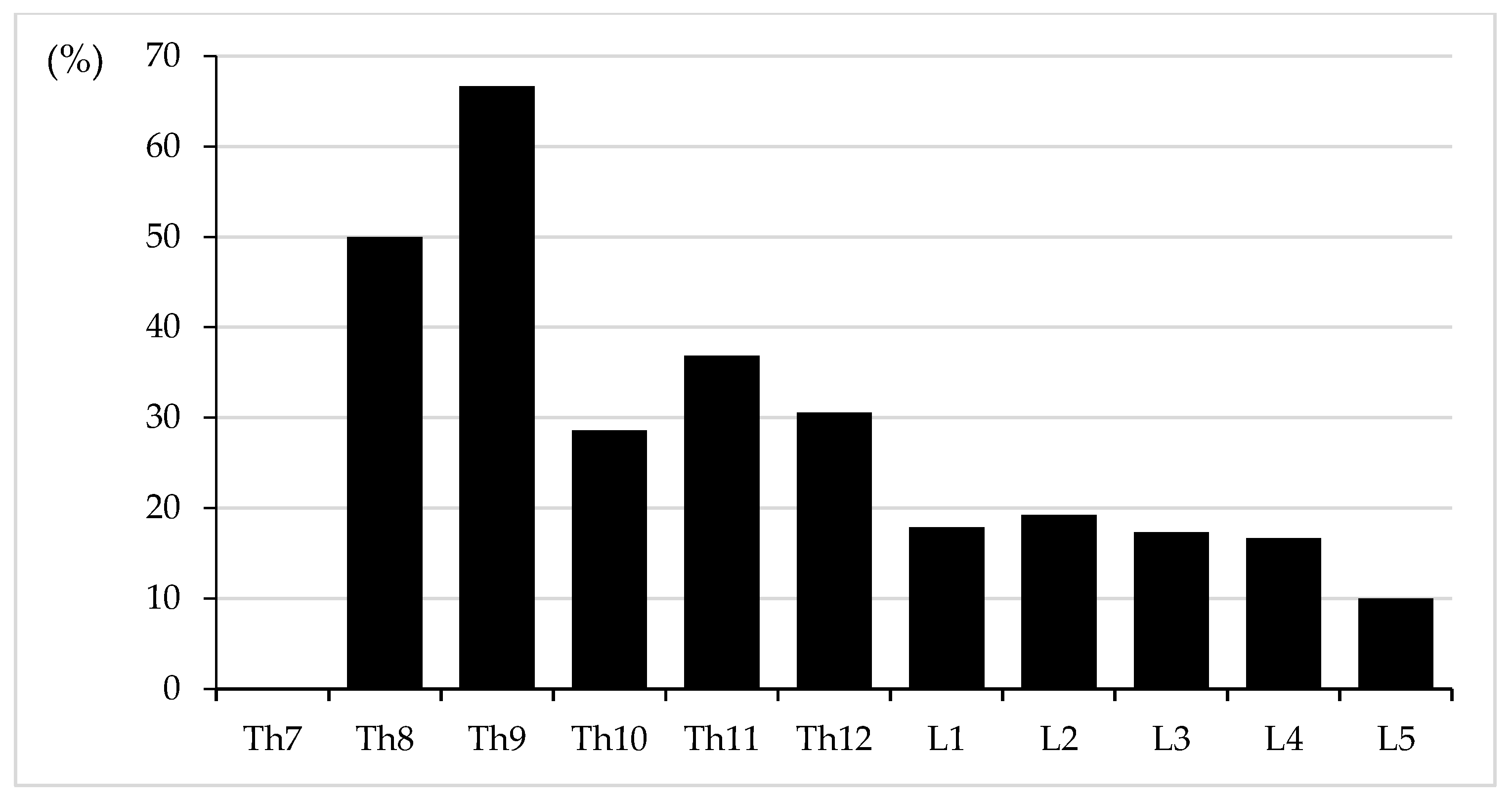
3.8. Analysis by Vertebral Level
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cummings, S.R.; Melton, L.J. Epidemiology and outcomes of osteoporotic fractures. Lancet 2002, 359, 1761–1767. [Google Scholar] [CrossRef] [PubMed]
- Galbusera, F.; Volkheimer, D.; Reitmaier, S.; Berger-Roscher, N.; Kienle, A.; Wilke, H.J. Pedicle screw loosening: A clinically relevant complication? Eur. Spine J. 2015, 24, 1005–1016. [Google Scholar] [CrossRef] [PubMed]
- Groen, R.J.M.; Groenewegen, H.J.; van Alphen, H.A.M.; Hoogland, P.V.J.M. Morphology of the human internal vertebral venous plexus: A cadaver study after intravenous araldite CY 221 injection. Anat. Rec. 1997, 249, 285–294. [Google Scholar] [CrossRef]
- Marie-Hardy, L.; Pascal-Moussellard, H.; Barnaba, A.; Bonaccorsi, R.; Scemama, C. Screw loosening in posterior spine fusion: Prevalence and risk factors. Glob. Spine J. 2020, 10, 598–602. [Google Scholar] [CrossRef]
- Weiser, L.; Huber, G.; Sellenschloh, K.; Viezens, L.; Puschel, K.; Morlock, M.M.; Lehmann, W. Insufficient stability of pedicle screws in osteoporotic vertebrae: Biomechanical correlation of bone mineral density and pedicle screw fixation strength. Eur. Spine J. 2017, 26, 2891–2897. [Google Scholar] [CrossRef]
- Iwanaga, J.; Rustagi, T.; Ishak, B.; Johal, J.; David, G.; Reina, M.A.; Dumont, A.S.; Tubbs, R.S. Venous drainage of lumbar vertebral bodies: Anatomic study with application to kyphoplasty, vertebroplasty, and pedicle screw complications. World Neurosurg. 2020, 137, e286–e290. [Google Scholar] [CrossRef]
- Guo, H.Z.; Tang, Y.C.; Guo, D.Q.; Zhang, S.C.; Li, Y.X.; Mo, G.Y.; Luo, P.J.; Zhou, T.P.; Ma, Y.H.; Liang, D.; et al. The cement leakage in cement-augmented pedicle screw instrumentation in degenerative lumbosacral diseases: A retrospective analysis of 202 cases and 950 augmented pedicle screws. Eur. Spine J. 2019, 28, 1661–1669. [Google Scholar] [CrossRef]
- Hoppe, S.; Keel, M.J. Pedicle screw augmentation in osteoporotic spine: Indications, limitations and technical aspects. Eur. J. Trauma. Emerg. Surg. 2017, 43, 3–8. [Google Scholar] [CrossRef]
- Liu, Y.; Xiao, J.; He, L.; Yin, X.; Song, L.; Zhou, R.; Zeng, J.; Liu, P.; Dai, F. Risk factor analysis of bone cement leakage for polymethylmethacrylate-augmented cannulated pedicle screw fixation in spinal degenerative diseases. Heliyon 2023, 9, e15167. [Google Scholar] [CrossRef]
- Yu, W.; Liang, D.; Yao, Z.; Zhang, H.; Zhong, Y.; Tang, Y.; Jiang, X.; Cai, D. The potential impact of basivertebral foramen morphology and pedicle screw placement on epidural cement leakage with cement-augmented fenestrated pedicle screw fixation: A multicenter retrospective study of 282 patients and 1404 augmented screws. Neurosurgery 2023, 93, 66–74. [Google Scholar] [CrossRef]
- Yeom, J.S.; Kim, W.J.; Choy, W.S.; Lee, C.K.; Chang, B.S.; Kang, J.W. Leakage of cement in percutaneous transpedicular vertebroplasty for painful osteoporotic compression fractures. J. Bone Jt. Surg. Br. 2003, 85, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, J.J.; Anderson, P.A.; Rosas, H.G.; Buchholz, A.L.; Au, A.G. Hounsfield units for assessing bone mineral density and strength: A tool for osteoporosis management. J. Bone Jt. Surg. Am. 2011, 93, 1057–1063. [Google Scholar] [CrossRef] [PubMed]
- Mueller, J.U.; Baldauf, J.; Marx, S.; Kirsch, M.; Schroeder, H.W.; Pillich, D.T. Cement leakage in pedicle screw augmentation: A prospective analysis of 98 patients and 474 augmented pedicle screws. J. Neurosurg. Spine 2016, 25, 103–109. [Google Scholar] [CrossRef]
- Shin, H.K.; Koo, H.W.; Kim, K.H.; Yoon, S.W.; Sohn, M.J.; Lee, B.J. The usefulness of trabecular CT attenuation measurement at L4 level to predict screw loosening after degenerative lumbar fusion surgery: Consider number of fused levels and postoperative sagittal balance. Spine 2022, 47, 745–753. [Google Scholar] [CrossRef]
- Sun, H.B.; Jing, X.S.; Shan, J.L.; Bao, L.; Wang, D.C.; Tang, H. Risk factors for pulmonary cement embolism associated with percutaneous vertebral augmentation: A systematic review and meta-analysis. Int. J. Surg. 2022, 101, 106632. [Google Scholar] [CrossRef]
- Potet, J.; Weber-Donat, G.; Curis, E.; Arnaud, F.X.; Thome, A.; Valbousquet, L.; Peroux, E.; Geffroy, Y.; Bouzad, C.; Kervella, Y.; et al. Incidence of pulmonary cement embolism after real-time CT fluoroscopy-guided vertebroplasty. J. Vasc. Interv. Radiol. 2013, 24, 1853–1860. [Google Scholar] [CrossRef]
- Trumm, C.G.; Jakobs, T.F.; Zech, C.J.; Helmberger, T.K.; Reiser, M.F.; Hoffmann, R.T. CT fluoroscopy-guided percutaneous vertebroplasty for the treatment of osteolytic breast cancer metastases: Results in 62 sessions with 86 vertebrae treated. J. Vasc. Interv. Radiol. 2008, 19, 1596–1606. [Google Scholar] [CrossRef]
- Choe, D.H.; Marom, E.M.; Ahrar, K.; Truong, M.T.; Madewell, J.E. Pulmonary embolism of polymethyl methacrylate during percutaneous vertebroplasty and kyphoplasty. AJR Am. J. Roentgenol. 2004, 183, 1097–1102. [Google Scholar] [CrossRef]
- Kim, H.J.; Park, E.S.; Lee, S.H.; Oh, T.H.; Park, C.H.; Shin, Y.H. Cardiac perforation caused by cement embolus after cement-augmented pedicle screw instrumentation: A case of report. J. Minim. Invasive Spine Surg. Technol. 2020, 5, 31–35. [Google Scholar] [CrossRef]
- Takahashi, S.; Sohgawa, E.; Suzuki, A.; Yamamoto, A.; Sasaki, R.; Tanaka, K.; Terai, H.; Hoshino, M.; Toyoda, H.; Tamai, K.; et al. Percutaneous endovascular retrieval of large cement leakage into the right atrium following cement-augmented pedicle screw instrumentation. Spine Surg. Relat. Res. 2021, 5, 446–449. [Google Scholar] [CrossRef]
- Lenga, P.; Bajwa, A.A.; Schneider, T.; Iwanaga, J.; Tubbs, R.S.; Kiening, K.L.; Unterberg, A.W.; Ishak, B. High rate of pulmonary cement embolism after cement-augmented pedicle screw fixation: A 12-year single-center study. J. Neurol. Surg. A Cent. Eur. Neurosurg. 2024, 85, 117–125. [Google Scholar] [CrossRef]
- Takahashi, S.; Sakai, D.; Ogasawara, S.; Sasaki, R.; Uematsu, M.; Hyakumachi, T.; Hiyama, A.; Katoh, H.; Terai, H.; Suzuki, A.; et al. The risk of intravenous cement leakage and short-term outcomes of selective cement-augmented pedicle screws: A multicenter retrospective study. Clin. Spine Surg. 2024, 38, E419–E424. [Google Scholar] [CrossRef]
- Janssen, I.; Ryang, Y.M.; Gempt, J.; Bette, S.; Gerhardt, J.; Kirschke, J.S.; Meyer, B. Risk of cement leakage and pulmonary embolism by bone cement-augmented pedicle screw fixation of the thoracolumbar spine. Spine J. 2017, 17, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Tucker, W.D.; Shrestha, R.; Burns, B. Anatomy, Abdomen and Pelvis: Inferior Vena Cava. In StatPearls; StatPearls Publishing 2025; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2023. [Google Scholar]
- Borg, N.; Cutsforth-Gregory, J.; Oushy, S.; Huynh, T.; Savastano, L.E.; Cloft, H.J.; Lanzino, G.; Brinjikji, W. Anatomy of spinal venous drainage for the neurointerventionalist: From puncture site to intervertebral foramen. AJNR. Am. J. Neuroradiol. 2022, 43, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Berman, D.J.; Schiavi, A.; Frank, S.M.; Duarte, S.; Schwengel, D.A.; Miller, C.R. Factors that influence flow through intravascular catheters: The clinical relevance of Poiseuille’s law. Transfusion. 2020, 60, 1410–1417. [Google Scholar] [CrossRef] [PubMed]
- Kutoglu, T.; Turut, M.; Kocabiyik, N.; Ozan, H.; Yildirim, M. Anatomical analysis of azygos vein system in human cadavers. Rom. J. Morphol. Embryol. 2012, 53, 1051–1056. [Google Scholar]
- Tamagawa, S.; Nojiri, H.; Takano, H.; Itoi, A.; Yokota, R.; Shiobara, T.; Ishii, K.; Takeuchi, T.; Kojo, T.; Ishii, Y.; et al. Risk Factors for cement leakage in cement-augmented pedicle screw fixation: A multicenter study of 140 patients and 650 screws. Glob. Spine. J. 2025, 1–9. [Google Scholar] [CrossRef]
- Weiser, L.; Sellenschloh, K.; Puschel, K.; Morlock, M.M.; Viezens, L.; Lehmann, W.; Huber, G. Reduced cement volume does not affect screw stability in augmented pedicle screws. Eur. Spine J. 2020, 29, 1297–1303. [Google Scholar] [CrossRef]
- Frankel, B.M.; D’Agostino, S.; Wang, C. A biomechanical cadaveric analysis of polymethylmethacrylate-augmented pedicle screw fixation. J. Neurosurg. Spine 2007, 7, 47–53. [Google Scholar] [CrossRef]

| Variable | Overall (n = 79 Patients) |
|---|---|
| Age, y, mean ± SD | 76.8 ± 8.38 |
| Sex, male/female, n (%) | 14 (17.7)/65 (82.3) |
| Mean HU value of instrumented vertebrae | 84.86 ± 43.59 |
| Instrumented vertebral level, n (%) | Thoracic 114 (37.8) Lumbar 188 (62.3) |
| Number of inserted CAFPSs, n | 302 |
| Screw diameter, mm, mean ± SD | 6.45 ± 0.71 |
| Screw length, mm, mean ± SD | 43.69 ± 3.49 |
| Screw laterality, n (%) | Right 151 (50.0) Left 151 (50.0) |
| Cement volume per screw, mL | 0.96 ± 0.17 |
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| Variable | OR | 95% CI | p-Value | OR | 95% CI | p-Value |
| Right side (vs. left) | 1.503 | 0.879–2.572 | 0.137 | 2.498 | 1.270–4.913 | 0.008 |
| Screw diameter (per 1 mm) | 0.775 | 0.532–1.127 | 0.182 | 0.856 | 0.533–1.374 | 0.519 |
| Screw length (per 5 mm) | 0.752 | 0.511–1.108 | 0.149 | 1.511 | 0.918–2.489 | 0.105 |
| Cement volume (per 0.1 mL) | 1.021 | 0.881–1.183 | 0.782 | n.e. | ||
| Lateral cortical wall distance (per 1 mm) | 0.582 | 0.506–0.669 | <0.001 | 0.547 | 0.469–0.638 | <0.001 |
| Variable | AUC | 95% CI | p-Value | Cut-Off Value | Sensitivity | Specificity |
|---|---|---|---|---|---|---|
| Screw diameter | 0.555 | 0.480–0.630 | 0.158 | ≤6.5 | 0.592 | 0.532 |
| Screw length | 0.552 | 0.475–0.629 | 0.187 | ≤42.5 | 0.437 | 0.654 |
| Cement volume | 0.502 | 0.426–0.578 | 0.967 | ≤0.85 | 0.901 | 0.130 |
| Lateral cortical wall distance | 0.842 | 0.789–0.896 | <0.001 | ≤9.21 | 0.845 | 0.719 |
| Inserting Screws | Cement Leakage Screws | |
|---|---|---|
| Th7 | 2 | 0 * (0.0) |
| Th8 | 4 | 2 * (50.0) |
| Th9 | 6 | 4 * (66.7) |
| Th10 | 28 | 8 * (28.6) |
| Th11 | 38 | 14 * (36.8) |
| Th12 | 36 | 11 * (30.6) |
| Thoracic (Th1–12) | 114 | 39 * (34.2) |
| L1 | 28 | 5 * (17.9) |
| L2 | 52 | 10 * (19.2) |
| L3 | 52 | 9 * (17.3) |
| L4 | 36 | 6 * (16.7) |
| L5 | 20 | 2 * (10.0) |
| Lumbar (L1–5) | 188 | 32 * (17.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shinohara, A.; Kanai, T.; Katsumi, S.; Obata, S.; Wakiya, H.; Tsuzuki, T.; Saito, M. Cement Leakage in Cement-Augmented Fenestrated Pedicle Screws for Osteoporotic Spine: Risk Stratification with Quantitative Computed Tomography Analysis. J. Clin. Med. 2025, 14, 8178. https://doi.org/10.3390/jcm14228178
Shinohara A, Kanai T, Katsumi S, Obata S, Wakiya H, Tsuzuki T, Saito M. Cement Leakage in Cement-Augmented Fenestrated Pedicle Screws for Osteoporotic Spine: Risk Stratification with Quantitative Computed Tomography Analysis. Journal of Clinical Medicine. 2025; 14(22):8178. https://doi.org/10.3390/jcm14228178
Chicago/Turabian StyleShinohara, Akira, Tomoaki Kanai, Shunsuke Katsumi, Shintaro Obata, Hiroki Wakiya, Takero Tsuzuki, and Mitsuru Saito. 2025. "Cement Leakage in Cement-Augmented Fenestrated Pedicle Screws for Osteoporotic Spine: Risk Stratification with Quantitative Computed Tomography Analysis" Journal of Clinical Medicine 14, no. 22: 8178. https://doi.org/10.3390/jcm14228178
APA StyleShinohara, A., Kanai, T., Katsumi, S., Obata, S., Wakiya, H., Tsuzuki, T., & Saito, M. (2025). Cement Leakage in Cement-Augmented Fenestrated Pedicle Screws for Osteoporotic Spine: Risk Stratification with Quantitative Computed Tomography Analysis. Journal of Clinical Medicine, 14(22), 8178. https://doi.org/10.3390/jcm14228178





