Delayed Occlusal Loading of a Definitive Cutback Zirconia Crown in Immediate Implant Placement for Single-Tooth Replacement: A Case Report
Abstract
1. Introduction
2. Materials and Methods
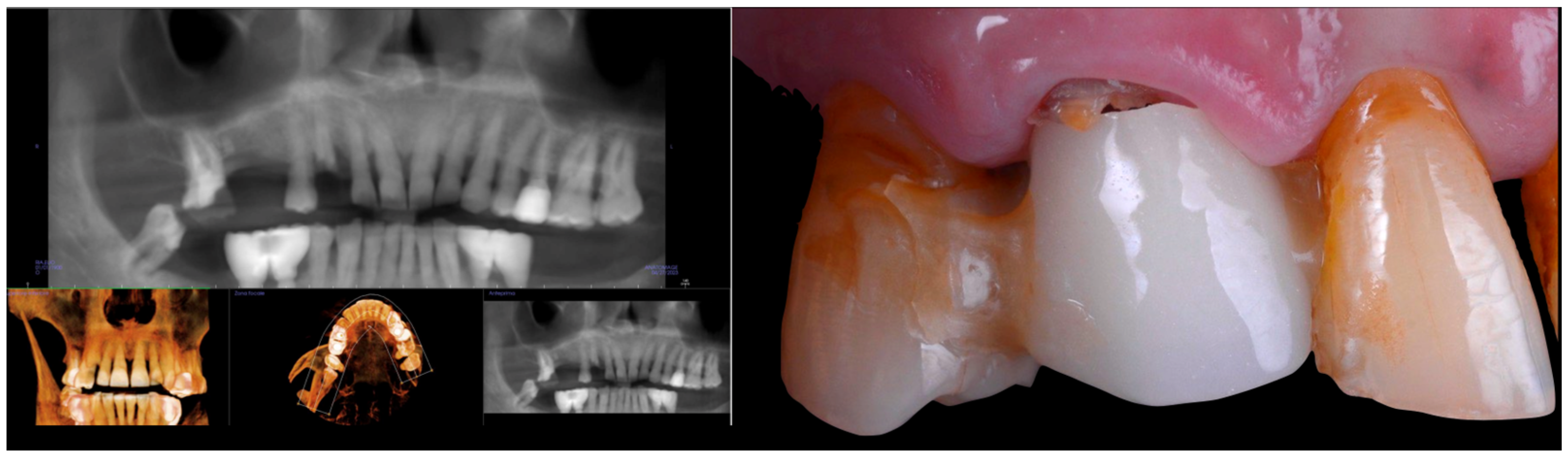
2.1. Case Presentation
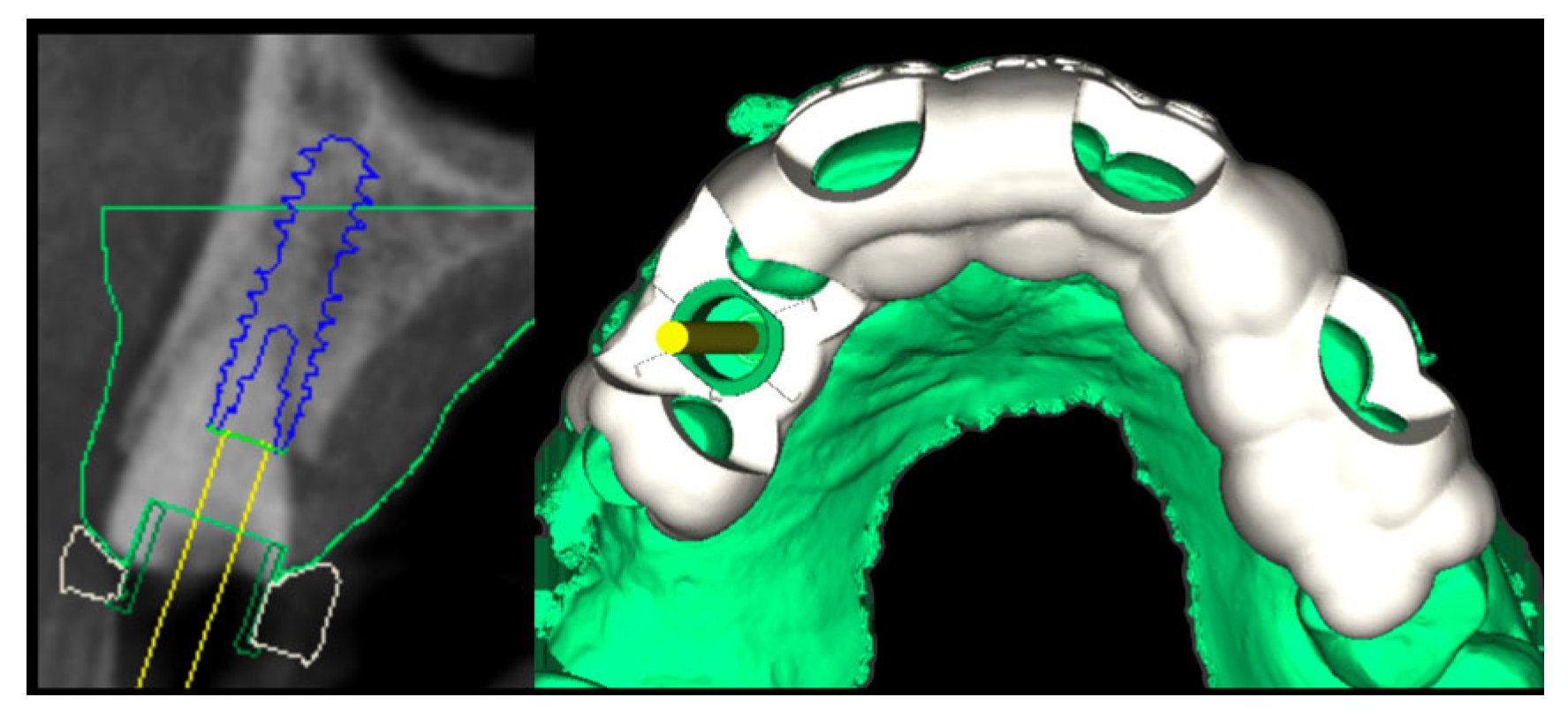
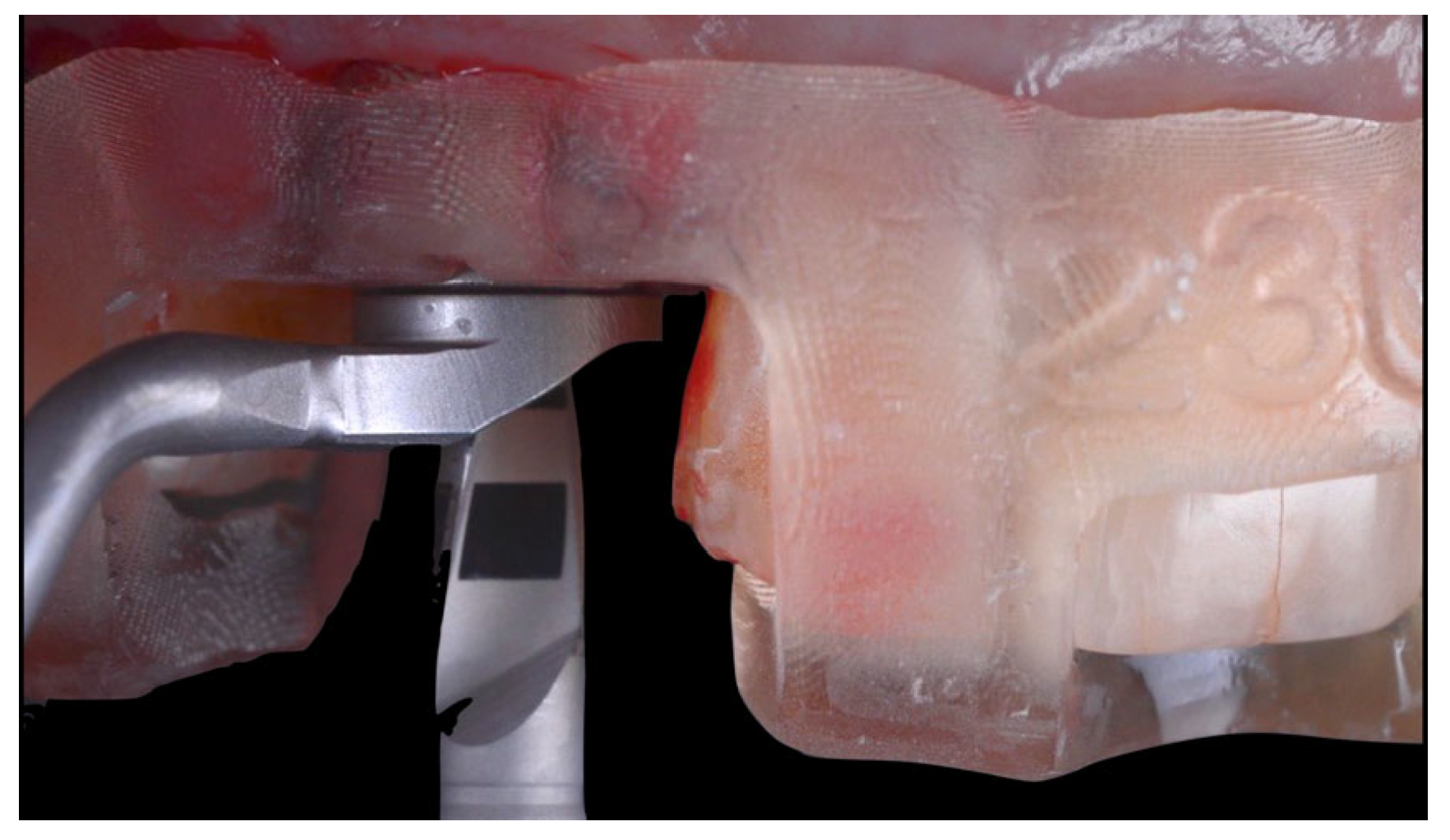
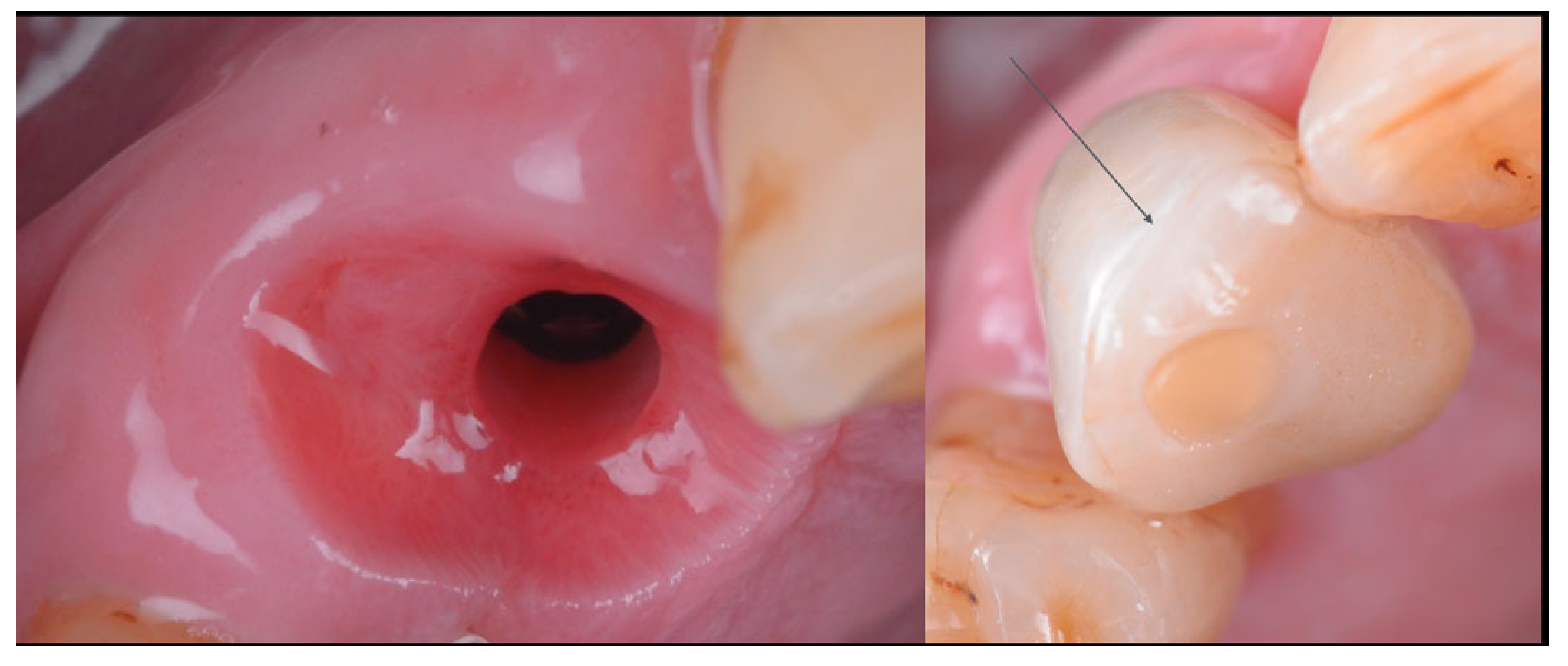
2.2. Surgery
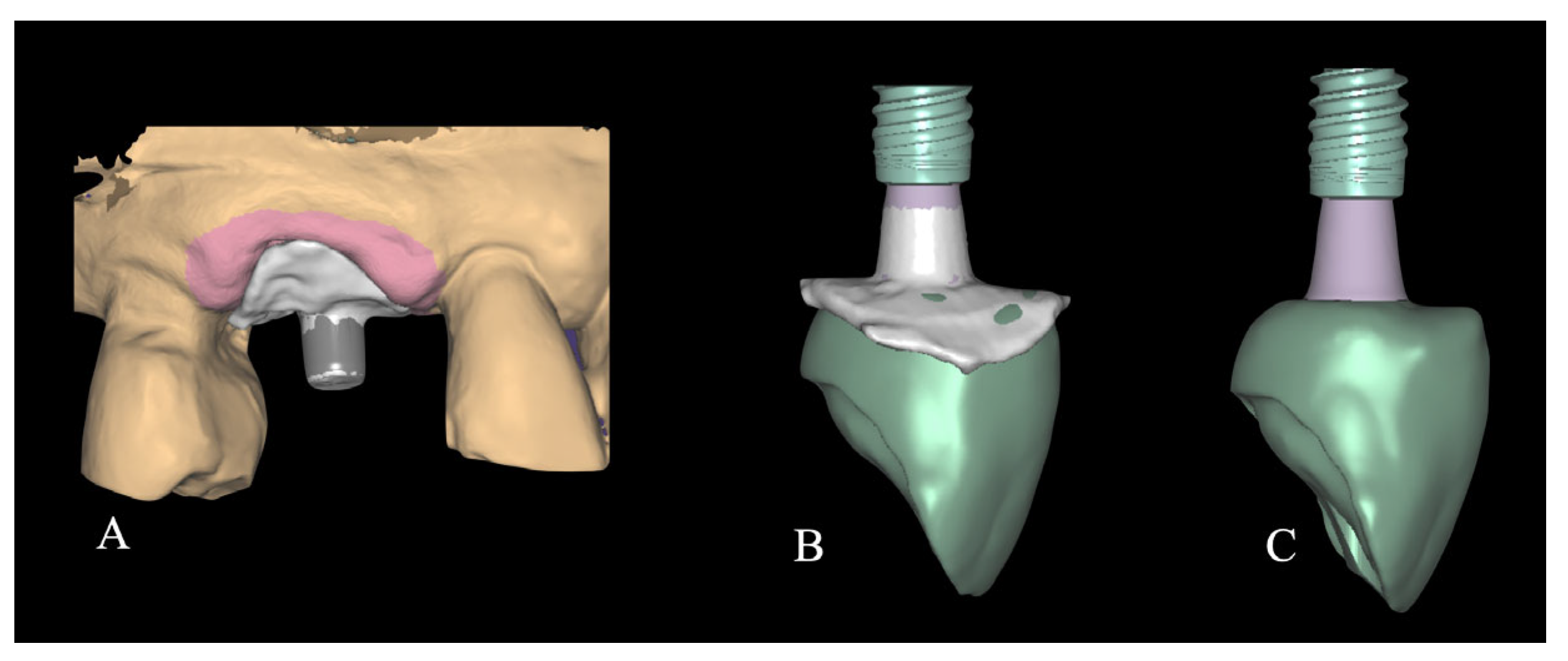
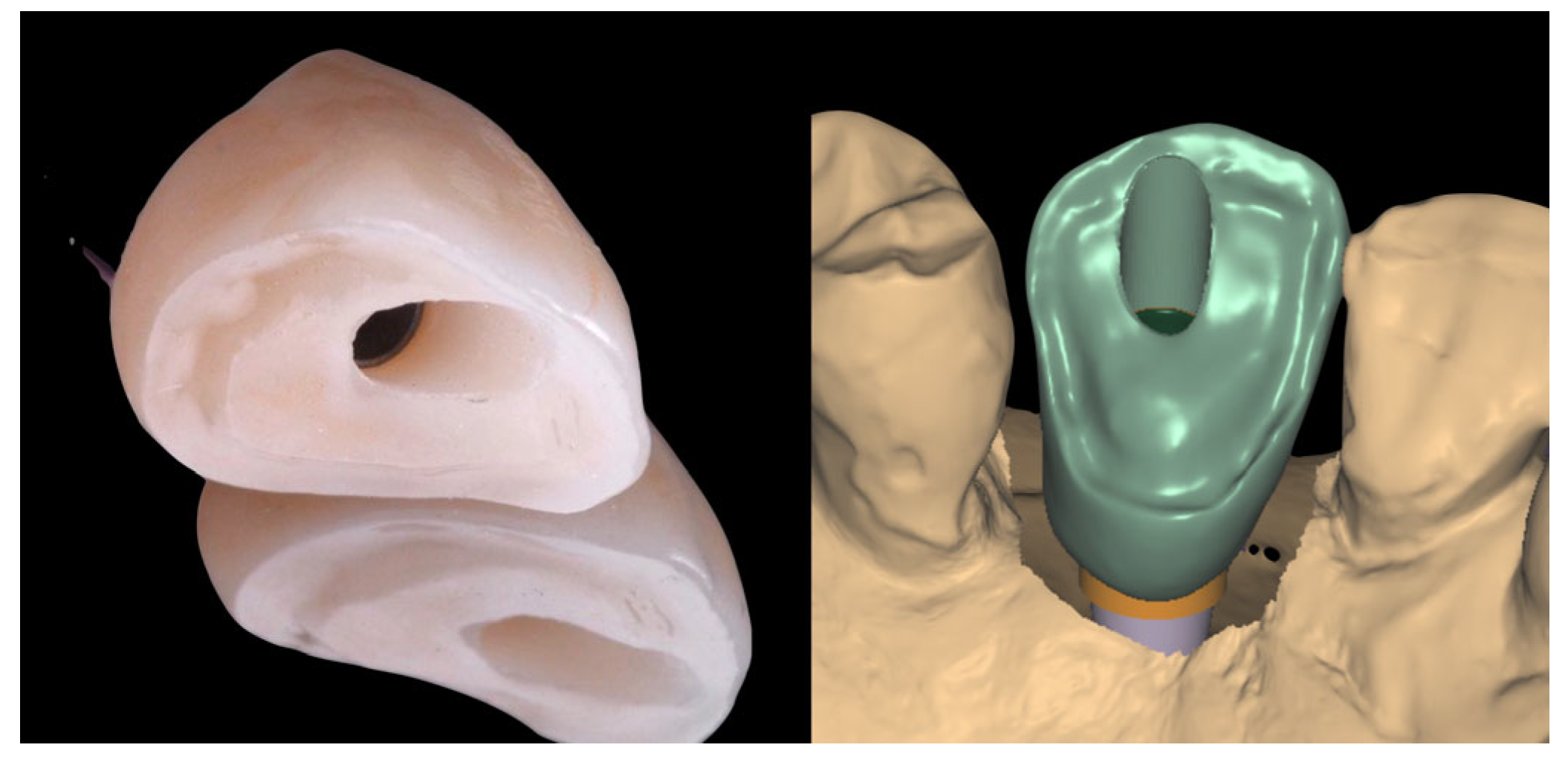
2.3. Laboratory Procedure
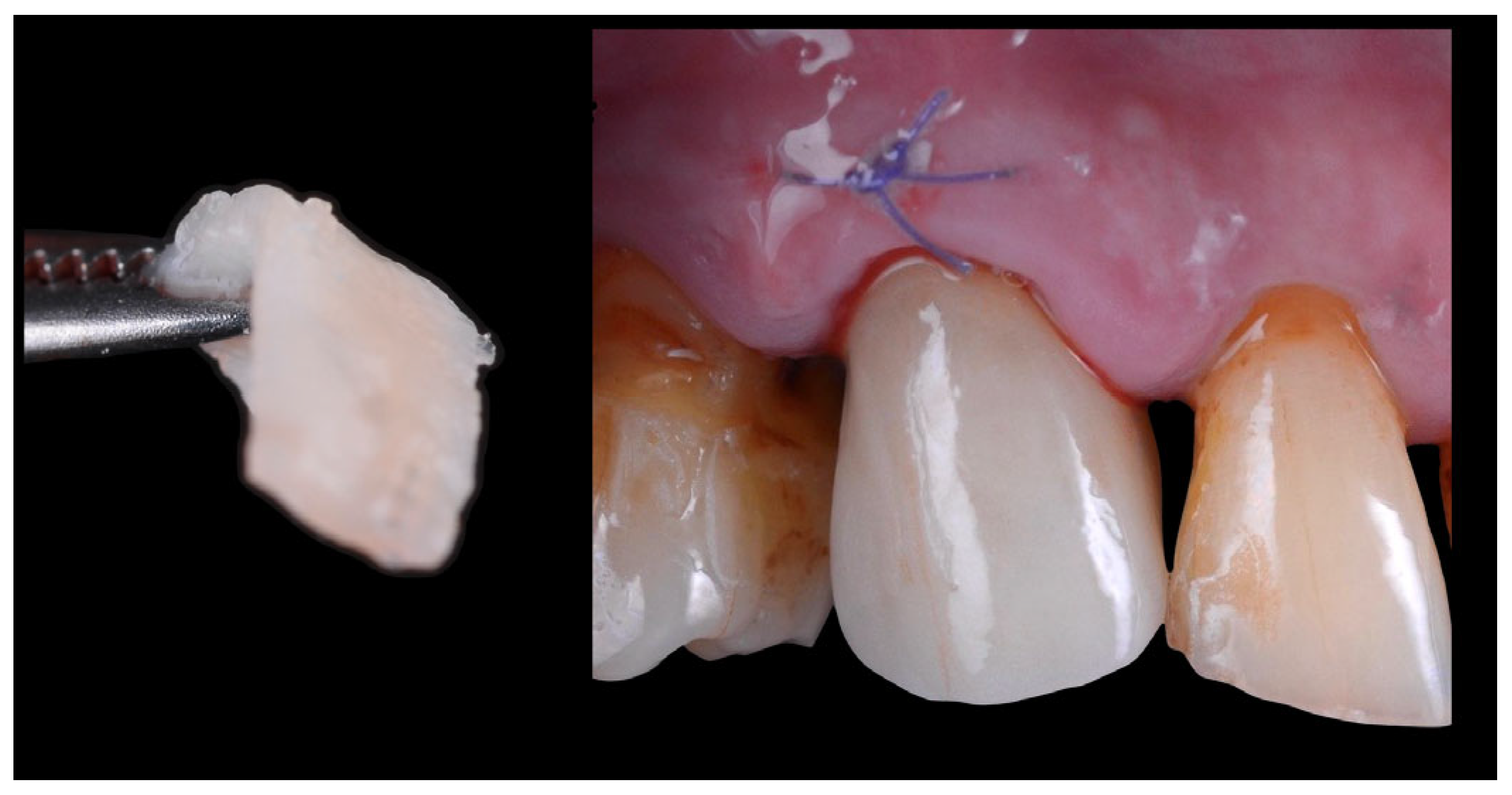
2.4. Crown Delivery
2.5. Definitive Overlay Adhesion
3. Discussion
4. Conclusions
- -
- Immediate implant placement with a one-time abutment and delayed occlusal veneering preserved peri-implant soft tissue architecture.
- -
- The protocol achieved excellent esthetic and functional outcomes at two-year follow-up.
- -
- The one-stage workflow reduced surgical and prosthetic interventions while maintaining tissue stability.
- -
- This approach may represent a predictable, tissue-preserving alternative to conventional multi-stage protocols.
- -
- Further controlled studies are required to confirm long-term clinical reliability and reproducibility.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ASA | American Society of Anesthesiologists |
References
- Chen, S.T.; Buser, D. Esthetic outcomes following immediate and early implant placement in the anterior maxilla—A systematic review. Int. J. Oral Maxillofac. Implant. 2014, 29, 186–215. [Google Scholar] [CrossRef]
- Canullo, L.; Bignozzi, I.; Cocchetto, R.; Cristalli, M.P.; Iannello, G. Immediate positioning of a definitive abutment versus repeated abutment replacements in post-extractive implants: 3-year follow-up of a randomised multicentre clinical trial. Eur. J. Oral Implantol. 2010, 3, 285–296. [Google Scholar] [PubMed]
- Toia, M.; Moreira, C.S.; Dias, D.R.; Corrà, E.; Ravidà, A.; Cecchinato, D. Fixed Full-Arch Maxillary Prostheses Supported by Four Versus Six Implants: 5-Year Results of a Multicenter Randomized Clinical Trial. Clin. Oral Implant. Res. 2025, 36, 298–313. [Google Scholar] [CrossRef] [PubMed]
- Tallarico, M.; Caneva, M.; Meloni, S.M.; Xhanari, E.; Covani, U.; Canullo, L. Definitive abutments placed at implant insertion and never removed: Is it an effective approach? A systematic review and meta-analysis of randomized controlled trials. J. Oral. Maxillofac. Surg. 2018, 76, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Mattheos, N.; Janda, M.; Acharya, A.; Pekarski, S.; Larsson, C. Impact of design elements of the implant supracrestal complex (ISC) on the risk of peri-implant mucositis and peri-implantitis: A critical review. Clin. Oral Implant. Res. 2021, 32, 181–202. [Google Scholar] [CrossRef]
- Parpaiola, A.; Norton, M.R.; Cecchinato, D.; Bressan, E.; Toia, M. Virtual Abutment Design: A Concept for Delivery of CAD/CAM Customized Abutments-Report of a Retrospective Cohort. Int. J. Periodontics Restor. Dent. 2013, 33, 51–58. [Google Scholar] [CrossRef]
- Sailer, I.; Zembic, A.; Jung, R.E.; Hämmerle, C.; Mattiola, A. Single-tooth implant reconstructions: Esthetic factors influencing the decision between titanium and zirconia abutments in anterior regions. Eur. J. Esthet. Dent. 2007, 2, 296. [Google Scholar]
- Wolters, U.; Wolf, T.; Stützer, H.; Schröder, T. ASA classification and perioperative variables as predictors of postoperative outcome. Br. J. Anaesth. 1996, 77, 217–222. [Google Scholar] [CrossRef]
- Thoma, D.S.; Gasser, T.J.; Hämmerle, C.H.; Strauss, F.J.; Jung, R.E. Soft tissue augmentation with a volume-stable collagen matrix or an autogenous connective tissue graft at implant sites: Five-year results of a randomized controlled trial post implant loading. J. Periodontol. 2023, 94, 230–243. [Google Scholar] [CrossRef]
- Naiem, S.N.; Al-Nawas, B.; Tawfik, O.K.; El-Nahass, H. Jumping gap in immediate implant placement in the esthetic zone: A virtual implant planning using cone-beam computed tomography. J. Prosthodont. Res. 2023, 68, 347–353. [Google Scholar] [CrossRef]
- Levine, R.A.; Ganeles, J.; Gonzaga, L.; Kan, J.K.; Randel, H.; Evans, C.D.; Chen, S.T. 10 keys for successful esthetic-zone single immediate implants. Compend. Contin. Educ. Dent. 2017, 38, 248–260. [Google Scholar]
- Morton, D.; Jaffin, R.; Weber, H.-P. Immediate restoration and loading of dental implants: Clinical considerations and protocols. Int. J. Oral Maxillofac. Implant. 2004, 19, 103–108. [Google Scholar]
- Blatz, M.B.; Sadan, A.; Kern, M. Resin-ceramic bonding: A review of the literature. J. Prosthet. Dent. 2003, 89, 268–274. [Google Scholar] [CrossRef]
- Chandran, K.R.S.; Goyal, M.; Mittal, N.; George, J.S. Accuracy of freehand versus guided immediate implant placement: A randomized controlled trial. J. Dent. 2023, 136, 104620. [Google Scholar] [CrossRef]
- Buser, D.; Chappuis, V.; Belser, U.C.; Chen, S. Implant placement post extraction in esthetic single tooth sites: When immediate, when early, when late? Periodontology 2000 2017, 73, 84–102. [Google Scholar] [CrossRef] [PubMed]
- Tatakis, D.N.; Chien, H.H.; Parashis, A.O. Guided implant surgery risks and their prevention. Periodontology 2000 2019, 81, 194–208. [Google Scholar] [CrossRef]
- Marchack, C.B. CAD/CAM-guided implant surgery and fabrication of an immediately loaded prosthesis for a partially edentulous patient. J. Prosthet. Dent. 2007, 97, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Abrahamsson, I.; Berglundh, T.; Lindhe, J. The mucosal barrier following abutment dis/reconnection: An experimental study in dogs. J. Clin. Periodontol. 1997, 24, 568–572. [Google Scholar] [CrossRef] [PubMed]
- Lazzara, R.J.; Porter, S.S. Platform switching: A new concept in implant dentistry for controlling postrestorative crestal bone levels. Int. J. Periodontics Restor. Dent. 2006, 26, 9–17. [Google Scholar]
- Berglundh, T.; Abrahamsson, I.; Welander, M.; Lang, N.P.; Lindhe, J. Morphogenesis of the peri-implant mucosa: An experimental study in dogs. Clin. Oral Implant. Res. 2007, 18, 1–8. [Google Scholar]
- Tomasi, C.; Tessarolo, F.; Caola, I.; Wennström, J.; Nollo, G.; Berglundh, T. Morphogenesis of peri-implant mucosa revisited: An experimental study in humans. Clin. Oral Implant. Res. 2014, 25, 997–1003. [Google Scholar] [CrossRef] [PubMed]
- Toia, M.; Stocchero, M.; Galli, S.; Papia, E.; Wennerberg, A.; Becktor, J.P. The use of implant-level connection in screw-retained fixed partial dentures: A 3-year randomised clinical trial. Clin. Oral Implant. Res. 2022, 33, 78–93. [Google Scholar] [CrossRef] [PubMed]
- Atieh, M.A.; Ibrahim, H.M.; Atieh, A.H. Platform switching for marginal bone preservation around dental implants: A systematic review and meta-analysis. J. Periodontol. 2010, 81, 1350–1366. [Google Scholar] [CrossRef] [PubMed]
- Bressan, E.; Grusovin, M.G.; Visconti, R.F.; Luongo, G.; Piombino, P.; Greco, K.; Buti, J.; Sbricoli, L.; Esposito, M. The Influence of Repeated Abutment Changes on Peri-Implant Tissue Stability and Keratinised Tissue on Peri-Implant Health: 12-Year Post-Loading Results From a Multicentre Randomised Controlled Trial. J. Periodontal Res. 2025. [Google Scholar] [CrossRef]
- Chokaree, P.; Poovarodom, P.; Chaijareenont, P.; Rungsiyakull, P. Effect of customized and prefabricated healing abutments on peri-implant soft tissue and bone in immediate implant sites: A randomized controlled trial. J. Clin. Med. 2024, 13, 886. [Google Scholar] [CrossRef]
- Ruhstorfer, M.; Güth, J.-F.; Stimmelmayr, M.; Waltenberger, L.; Schubert, O.; Graf, T. Systematic review of peri-implant conditions and aesthetic outcomes of customized versus conventional healing abutments. Int. J. Implant Dent. 2024, 10, 61. [Google Scholar] [CrossRef]
- Krautwald, L.; Smeets, R.; Stolzer, C.; Rutkowski, R.; Guo, L.; Reitmeier, A.; Gosau, M.; Henningsen, A. Osseointegration of zirconia implants after UV-light or cold atmospheric plasma surface treatment in vivo. Materials 2022, 15, 496. [Google Scholar] [CrossRef]
- Gomez-Meda, R.; Esquivel, J.; Blatz, M.B. The esthetic biological contour concept for implant restoration emergence profile design. J. Esthet. Restor. Dent. 2021, 33, 173–184. [Google Scholar] [CrossRef]
- González-Martín, O.; Lee, E.; Weisgold, A.; Veltri, M.; Su, H. Contour management of implant restorations for optimal emergence profiles: Guidelines for immediate and delayed provisional restorations. Int. J. Periodontics Restor. Dent. 2020, 40, 61–70. [Google Scholar] [CrossRef]
- Lyann, S.K.; Takagaki, T.; Nikaido, T.; Uo, M.; Ikeda, M.; Tagami, J. Effect of Different Surface Treatments on the Tensile Bond Strength to Lithium Disilicate Glass Ceramics. J. Adhes. Dent. 2018, 20, 261–268. [Google Scholar]
- Abu Haimed, T.S.; Alzahrani, S.J.; Attar, E.A.; Al-Turki, L.E. Effect of repressing lithium disilicate glass ceramics on the shear bond strength of resin cements. Materials 2023, 16, 6148. [Google Scholar] [CrossRef]
- de Araújo-Neto, V.G.; de Almeida Nobre, C.F.; Freitas, M.I.M.; Lima, R.B.W.; Sinhoreti, M.A.C.; Cury, A.A.D.B.; Giannini, M. Effect of hydrofluoric acid concentration on bond strength to glass-ceramics: A systematic review and meta-analysis of in-vitro studies. J. Adhes. Dent. 2023, 25, b4646943. [Google Scholar]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cosello, V.; Parpaiola, A.; Toia, M. Delayed Occlusal Loading of a Definitive Cutback Zirconia Crown in Immediate Implant Placement for Single-Tooth Replacement: A Case Report. J. Clin. Med. 2025, 14, 8053. https://doi.org/10.3390/jcm14228053
Cosello V, Parpaiola A, Toia M. Delayed Occlusal Loading of a Definitive Cutback Zirconia Crown in Immediate Implant Placement for Single-Tooth Replacement: A Case Report. Journal of Clinical Medicine. 2025; 14(22):8053. https://doi.org/10.3390/jcm14228053
Chicago/Turabian StyleCosello, Vincenzo, Andrea Parpaiola, and Marco Toia. 2025. "Delayed Occlusal Loading of a Definitive Cutback Zirconia Crown in Immediate Implant Placement for Single-Tooth Replacement: A Case Report" Journal of Clinical Medicine 14, no. 22: 8053. https://doi.org/10.3390/jcm14228053
APA StyleCosello, V., Parpaiola, A., & Toia, M. (2025). Delayed Occlusal Loading of a Definitive Cutback Zirconia Crown in Immediate Implant Placement for Single-Tooth Replacement: A Case Report. Journal of Clinical Medicine, 14(22), 8053. https://doi.org/10.3390/jcm14228053





