Anatomical Reconstruction of Chronic Distal Biceps Tendon Ruptures Using a Tripled Semitendinosus Auto-Graft, Tension-Slide Technique and Interference Screw: Description of a New Surgical Technique and Preliminary Results
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
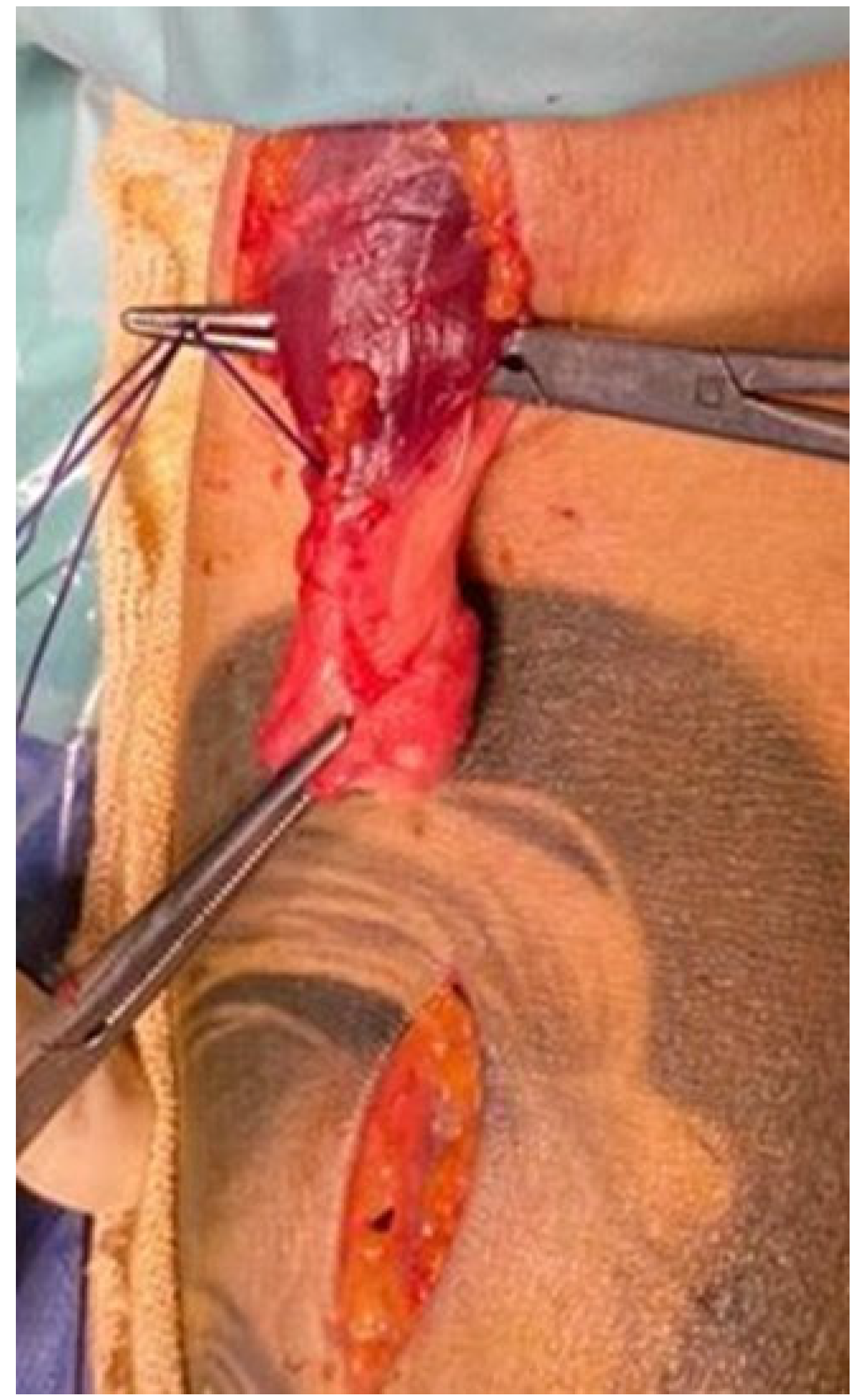
2.2. Surgical Technique
2.3. Post-Surgical Rehabilitation Phase
2.4. Outcome Assessment and Classification
2.5. Statistical Analysis
- Surgical timing (early ≤6 weeks vs. late ≥7 weeks);
- Age (≤46 years vs. >46 years);
- TMG asymmetry (absent <10% vs. present ≥10%).
3. Results
Statistical Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Beneš, M.; Kachlík, D.; Kunc, V. Surgical anatomy for reinsertion of the distal tendon of the biceps brachii muscle. Rozhl. Chir. 2025, 104, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Safran, M.R.; Graham, S.M. Distal biceps tendon ruptures: Incidence, demographics, and the effect of smoking. Clin. Orthop. Relat. Res. 2002, 404, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Kelly, M.P.; Perkinson, S.G.; Ablove, R.H.; Tueting, J.L. Distal biceps tendon ruptures: An epidemiological analysis using a large population database. Am. J. Sports Med. 2015, 43, 2012–2017. [Google Scholar] [CrossRef] [PubMed]
- O’Driscoll, S.W.; Goncalves, L.B.; Dietz, P. The hook test for distal biceps tendon avulsion. Am. J. Sport Med. 2007, 35, 1865–1869. [Google Scholar] [CrossRef]
- Kelly, E.W.; Morrey, B.F.; O’Driscoll, S.W. Complications of repair of the distal biceps tendon with the modified two-incision technique. J. Bone Jt. Surg. Am. 2000, 82, 1575–1581. [Google Scholar] [CrossRef]
- Tjoumakaris, F.P.; Bradley, J.P. Distal Biceps Injuries. Clin. Sports Med. 2020, 39, 661–672. [Google Scholar] [CrossRef] [PubMed]
- Bajwa, A.; Simon, M.J.K.; Leith, J.M.; Moola, F.O.; Goetz, T.J.; Lodhia, P. Surgical Results of Chronic Distal Biceps Ruptures: A Systematic Review. Orthop. J. Sports Med. 2022, 10, 23259671211065772. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hang, D.W.; Bach, B.R., Jr.; Bojchuk, J. Repair of chronic distal biceps brachii tendon rupture using free autogenous semitendinosus tendon. Clin. Orthop. Relat. Res. 1996, 323, 188–191. [Google Scholar] [CrossRef] [PubMed]
- Wiley, W.B.; Noble, J.S.; Dulaney, T.D.; Bell, R.H.; Noble, D.D. Late reconstruction of chronic distal biceps tendon ruptures with a semitendinosus autograft technique. J. Shoulder Elb. Surg. 2006, 15, 440–444. [Google Scholar] [CrossRef] [PubMed]
- Morrell, N.T.; Mercer, D.M.; Moneim, M.S. Late reconstruction of chronic distal biceps tendon ruptures using fascia lata autograft and suture anchor fixation. Tech. Hand Up. Extrem. Surg. 2012, 16, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Cross, M.B.; Egidy, C.C.; Wu, R.H.; Osbahr, D.C.; Nam, D.; Dines, J.S. Single-incision chronic distal biceps tendon repair with tibialis anterior allograft. Int. Orthop. 2014, 38, 791–795. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Phadnis, J.; Flannery, O.; Watts, A.C. Distal biceps reconstruction using an Achilles tendon allograft, transosseous EndoButton, and Pulvertaft weave with tendon wrap technique for retracted, irreparable distal biceps ruptures. J. Shoulder Elbow Surg. 2016, 25, 1013–1019. [Google Scholar] [CrossRef] [PubMed]
- Fontana, M.; Trimarchi, A.; Colozza, A. Lacertus fibrosus augmentation for distal biceps brachii rupture repair: Surgical technique. Musculoskelet Surg. 2016, 100 (Suppl. S1), 85–88. [Google Scholar] [CrossRef] [PubMed]
- Frank, T.; Seltser, A.; Grewal, R.; King, G.J.W.; Athwal, G.S. Management of chronic distal biceps tendon ruptures: Primary repair vs. semitendinosus autograft reconstruction. J. Shoulder Elb. Surg. 2019, 28, 1104–1110. [Google Scholar] [CrossRef] [PubMed]
- Goyal, N.; Wilson, D.J.; Salzano, M.B.; Fernandez, J.J.; Cohen, M.S.; Wysocki, R.W. Restoration of peak strength and endurance following distal biceps reconstruction with allograft for chronic ruptures. J. Shoulder Elb. Surg. 2020, 29, 853–858. [Google Scholar] [CrossRef] [PubMed]
- Bolia, I.K.; Shontz, E.C.; Dobitsch, A.; Mayfield, C.K.; Bashrum, B.S.; Weber, A.E. Female patient with bilateral distal biceps tendon reconstruction: A case report. Trauma Case Rep. 2023, 47, 100870. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Boonrod, A.; Harasymczuk, M.; Ramazanian, T.; Boonrod, A.; Smith, J.; O’Driscoll, S.W. The Turtle Neck Sign: Identification of Severe Retracted Distal Biceps Tendon Rupture. Orthop. J. Sports Med. 2022, 10, 23259671211065030. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hendy, B.A.; Padegimas, E.M.; Harper, T.; Lazarus, M.D.; Abboud, J.A.; Namdari, S.; Horneff, J.G. Outcomes of chronic distal biceps reconstruction with tendon grafting: A matched comparison with primary repair. JSES Int. 2020, 5, 302–306. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vishwanathan, K.; Soni, K. Distal biceps rupture: Evaluation and management. J. Clin. Orthop. Trauma 2021, 19, 132–138. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Beeler, S.; Hecker, A.; Bouaicha, S.; Meyer, D.C.; Wieser, K. Indirect markers for length adjustment in distal biceps tendon allograft reconstruction. PLoS ONE 2021, 16, e0257057. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alamir, M.A.; Alotaibi, K.M. Chronic Distal Biceps Tendon Rupture With Allograft Reconstruction. Cureus 2022, 14, e30805. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Metikala, S.; Portnoff, B.; Herickhoff, P. Staged Achilles Allograft Reconstruction of Chronic Bilateral Simultaneous Tears of the Retracted Distal Biceps Tendon Using a Novel Fixation Technique. Cureus 2022, 14, e25172. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Moriya, K.; Maki, Y.; Koda, H.; Tsubokawa, N. A Novel Reconstruction Technique for Chronic Distal Biceps Tendon Rupture: A Case Report. JBJS Case Connect. 2023, 13, e23. [Google Scholar] [CrossRef] [PubMed]
- Maeda, A.; Shino, K.; Horibe, S.; Nakata, K.; Buccafusca, G. Anterior cruciate ligament reconstruction with multistranded autogenous semitendinosus tendon. Am. J. Sports Med. 1996, 24, 504–509. [Google Scholar] [CrossRef] [PubMed]
- Hudak, P.L.; Amadio, P.C.; Bombardier, C. Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder and hand). Am. J. Ind. Med. 1996, 29, 602–608. [Google Scholar] [CrossRef]
- Cusick, M.C.; Bonnaig, N.S.; Azar, F.M.; Mauck, B.M.; Smith, R.A.; Throckmorton, T.W. Accuracy and reliability of the Mayo elbow performance score (MEPS). J. Hand Surg. Am. 2014, 39, 1146–1150. [Google Scholar] [CrossRef]
- MacGregor, L.J.; Hunter, A.M.; Orizio, C.; Fairweather, M.M.; Ditroilo, M. Assessment of skeletal muscle contractile properties by radial displacement: The case for tensiomyography. Sports Med. 2018, 48, 1607–1620. [Google Scholar] [CrossRef]
- Wilson, H.V.; Johnson, M.I.; Francis, P. Repeated stimulation, inter-stimulus interval and inter-electrode distance alters muscle contractile properties as measured by Tensiomyography. PLoS ONE 2018, 13, e0191965. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kojić, F.; Ranisavljev, I.; Ćosić, D.; Popović, D.; Stojiljković, S.; Ilić, V. Effects of resistance training on hypertrophy, strength and tensiomyography parameters of elbow flexors: Role of eccentric phase duration. Biol. Sport 2021, 38, 587–594. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Srinivasan, R.C.; Pederson, W.C.; Morrey, B.F. Distal Biceps Tendon Repair and Reconstruction. J. Hand Surg. Am. 2020, 45, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Synovec, J.D.; Traven, S.A.; Griffith, A.T.; Novikov, D.; Li, X.; Woolf, S.K.; Eichinger, J.K.; Slone, H.S. Outcomes and complications after different surgical techniques for the treatment of chronic distal biceps tendon ruptures: A systematic review and quantitative synthesis. JSES Rev. Rep. Tech. 2022, 2, 323–331. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]


| Case | Gender | Age | Side | Time from Injury to Surgery (Week) | Follow-Up (Months) | Elbow ROM Compared to Other Side | Forearm ROM Compared to Other Side | Tensiomyography Muscular Strength Asymmetries | DASH Score | MEPS | Results |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 39 | R | 5 | 40 | NO DIFF | NO DIFF | NO DIFF | 6 | 92 | EXCELL |
| 2 | M | 51 | R | 7 | 29 | −15 EXT | −20 SUP −10 PRON | −15% | 16 | 84 | GOOD |
| 3 | M | 43 | R | 5 | 32 | NO DIFF | NO DIFF | NO DIFF | 8 | 92 | EXCELL |
| 4 | M | 38 | L | 6 | 47 | NO DIFF | NO DIFF | NO DIFF | 7 | 90 | EXCELL |
| 5 | F | 41 | R | 4 | 28 | NO DIFF | NO DIFF | NO DIFF | 9 | 92 | EXCELL |
| 6 | M | 49 | R | 4 | 33 | −10 EXT | NO DIFF | NO DIFF | 12 | 86 | GOOD |
| 7 | M | 52 | R | 8 | 35 | −10 EXT | −15 SUP −10 PRON | −15% | 10 | 86 | GOOD |
| 8 | M | 59 | L | 9 | 41 | −10 FLEX | −20 SUP −15 PRON | −15% | 15 | 76 | GOOD |
| 9 | F | 43 | L | 5 | 37 | NO DIFF | NO DIFF | NO DIFF | 8 | 94 | EXCELL |
| 10 | M | 48 | R | 7 | 20 | −15 EXT | −15 SUP −15 PRON | −10.0% | 12 | 86 | GOOD |
| 11 | M | 54 | R | 10 | 30 | −10 FLEX | −20 SUP −15 PRON | NO DIFF | 15 | 78 | GOOD |
| 12 | M | 28 | R | 5 | 36 | NO DIFF | NO DIFF | NO DIFF | 5 | 94 | EXCELL |
| 13 | M | 50 | R | 7 | 46 | −10 EXT | −15 SUP −15 PRON | −10.0% | 16 | 86 | GOOD |
| Group Comparison | Subgroup | DASH (Mean ± SD) | MEPS (Mean ± SD) | t-Value | p-Value |
|---|---|---|---|---|---|
| Surgery timing | Early (≤6 weeks, n = 7) | 8.8 ± 2.5 | 91.7 ± 2.1 | t = −2.63/4.39 | p = 0.028/0.004 |
| Surgery timing | Late (≥7 weeks, n = 6) | 12.8 ± 3.7 | 82.5 ± 5.2 | ||
| Age group | ≤46 years (n = 7) | 7.9 ± 2.3 | 92.3 ± 2.1 | t = −5.37/6.36 | p < 0.001/<0.001 |
| Age group | >46 years (n = 6) | 13.7 ± 1.8 | 81.7 ± 4.0 | ||
| TMG asymmetry | Absent (<10%, n = 8) | 8.3 ± 2.7 | 91.8 ± 2.5 | t = −4.18/5.26 | p = 0.002/0.002 |
| TMG asymmetry | Present (≥10%, n = 5) | 14.8 ± 2.6 | 80.4 ± 4.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pulcinelli, F.M.; Caterini, A.; Rovere, G.; D’Ambrosio, M.; Minnetti, G.M.; Farsetti, P.; De Maio, F. Anatomical Reconstruction of Chronic Distal Biceps Tendon Ruptures Using a Tripled Semitendinosus Auto-Graft, Tension-Slide Technique and Interference Screw: Description of a New Surgical Technique and Preliminary Results. J. Clin. Med. 2025, 14, 7948. https://doi.org/10.3390/jcm14227948
Pulcinelli FM, Caterini A, Rovere G, D’Ambrosio M, Minnetti GM, Farsetti P, De Maio F. Anatomical Reconstruction of Chronic Distal Biceps Tendon Ruptures Using a Tripled Semitendinosus Auto-Graft, Tension-Slide Technique and Interference Screw: Description of a New Surgical Technique and Preliminary Results. Journal of Clinical Medicine. 2025; 14(22):7948. https://doi.org/10.3390/jcm14227948
Chicago/Turabian StylePulcinelli, Ferdinando Maria, Alessandro Caterini, Giuseppe Rovere, Matteo D’Ambrosio, Giacomo Maria Minnetti, Pasquale Farsetti, and Fernando De Maio. 2025. "Anatomical Reconstruction of Chronic Distal Biceps Tendon Ruptures Using a Tripled Semitendinosus Auto-Graft, Tension-Slide Technique and Interference Screw: Description of a New Surgical Technique and Preliminary Results" Journal of Clinical Medicine 14, no. 22: 7948. https://doi.org/10.3390/jcm14227948
APA StylePulcinelli, F. M., Caterini, A., Rovere, G., D’Ambrosio, M., Minnetti, G. M., Farsetti, P., & De Maio, F. (2025). Anatomical Reconstruction of Chronic Distal Biceps Tendon Ruptures Using a Tripled Semitendinosus Auto-Graft, Tension-Slide Technique and Interference Screw: Description of a New Surgical Technique and Preliminary Results. Journal of Clinical Medicine, 14(22), 7948. https://doi.org/10.3390/jcm14227948






