Novel Application of the Lagis LapBase Cap in Transvaginal NOTES Hysterectomy: Surgical Outcomes and Cost-Effectiveness in 107 Cases
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
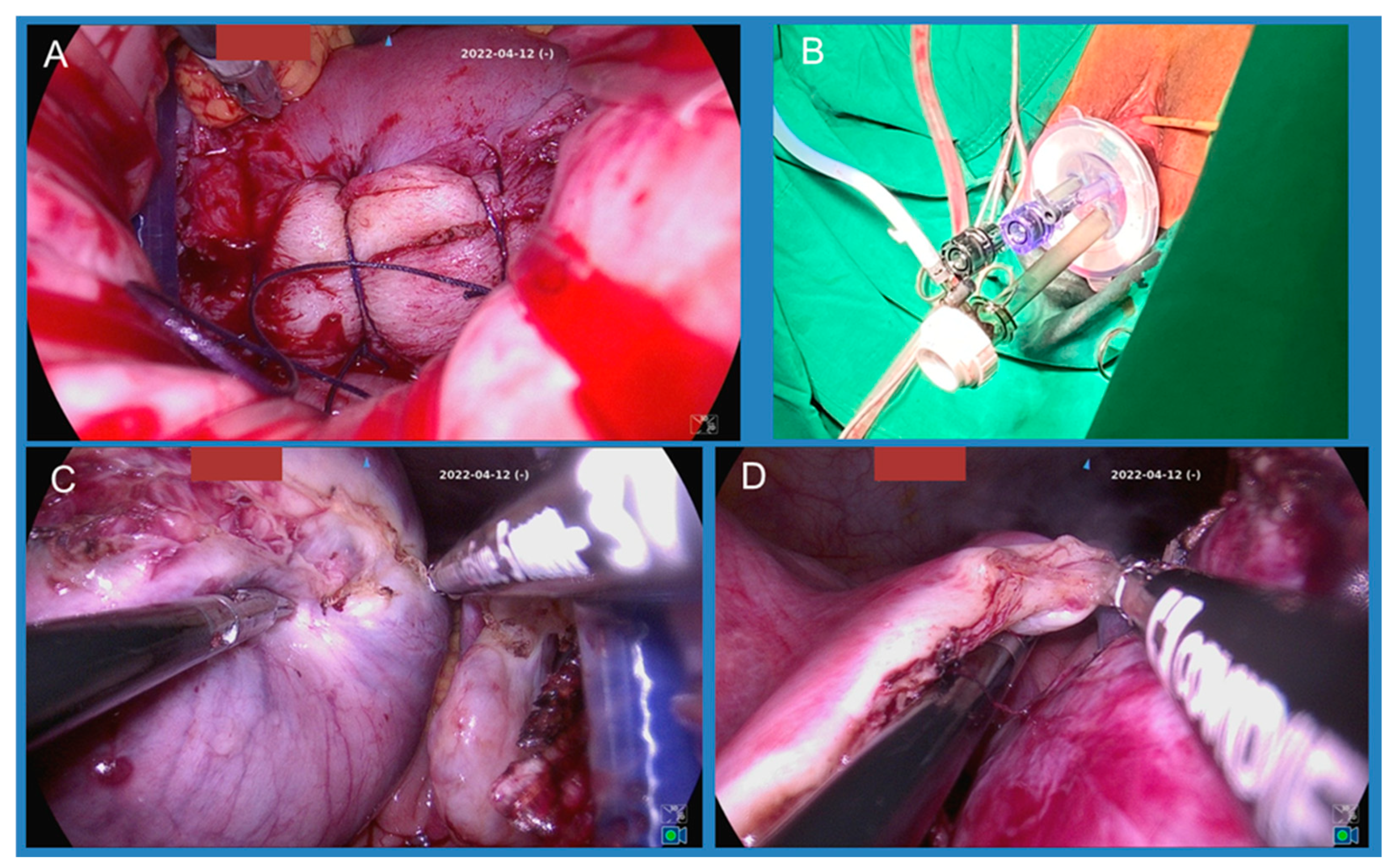
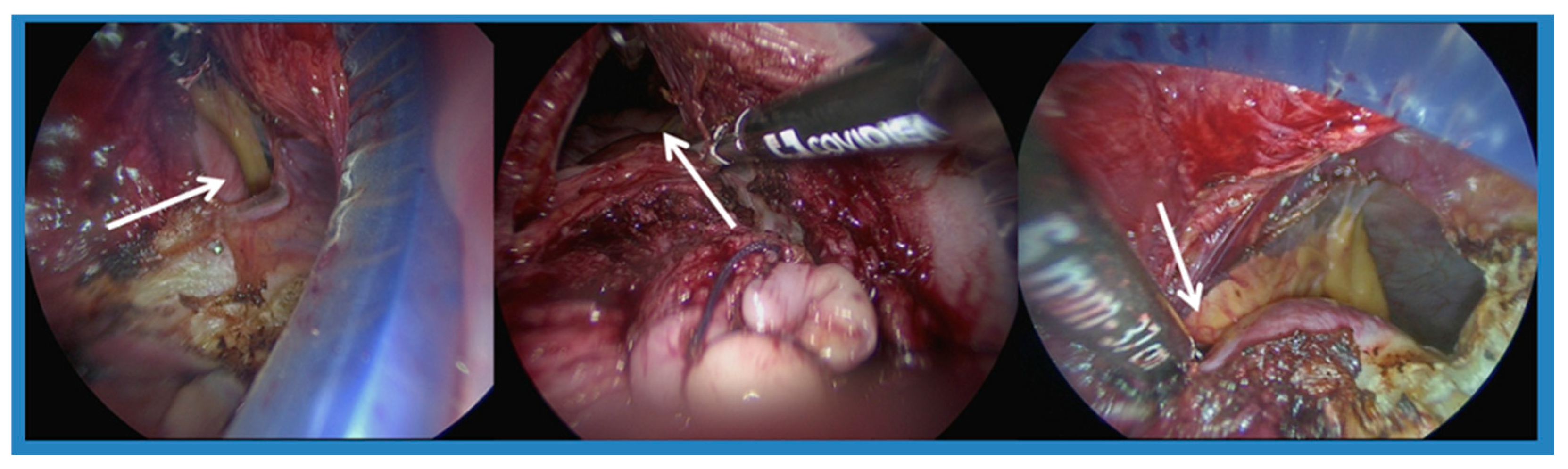
2.2. Surgical Technique
2.3. Outcome Measures
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| vNOTES | vaginal Natural Orifice Transluminal Endoscopic Surgery |
| LAVH | laparoscopic-assistance vaginal hysterectomy |
| BMI | Body mass index |
References
- Kalloo, A.N.; Singh, V.K.; Jagannath, S.B.; Niiyama, H.; Hill, S.L.; Vaughn, C.A.; Magee, C.A.; Kantsevoy, S.V. Flexible transgastric peritoneoscopy: A novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest. Endosc. 2004, 60, 114–117. [Google Scholar] [CrossRef] [PubMed]
- Temtanakitpaisan, T.; Wu, K.-Y.; Huang, C.-Y.; Jaiswal, A.; Yen, C.-F.; Lee, C.-L. The outcomes of transvaginal NOTES hysterectomy in various uterine sizes. Taiwan. J. Obstet. Gynecol. 2018, 57, 842–845. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-L.; Wu, K.-Y.; Su, H.; Wu, P.-J.; Han, C.-M.; Yen, C.-F. Hysterectomy by transvaginal natural orifice transluminal endoscopic surgery (NOTES): A series of 137 patients. J. Minim. Invasive Gynecol. 2014, 21, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-J.; Huang, H.-Y.; Huang, C.-Y.; Su, H. Hysterectomy via transvaginal natural orifice transluminal endoscopic surgery for nonprolapsed uteri. Surg. Endosc. 2014, 29, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Baekelandt, J.F.; De Mulder, P.; Le Roy, I.; Mathieu, C.; Laenen, A.; Enzlin, P.; Weyers, S.; Mol, B.W.J.; Bosteels, J. Hysterectomy by transvaginal natural orifice transluminal endoscopic surgery versus laparoscopy as a day-care procedure: A randomised controlled trial. BJOG Int. J. Obstet. Gynaecol. 2018, 126, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Chaccour, C.; Giannini, A.; D’AUgè, T.G.; Ayed, A.; Allahqoli, L.; Alkatout, I.; Laganà, A.S.; Chiantera, V.; D’ORia, O.; Sleiman, Z. Hysterectomy Using Vaginal Natural Orifice Transluminal Endoscopic Surgery Compared with Classic Laparoscopic Hysterectomy: A New Advantageous Approach? A Systematic Review on Surgical Outcomes. Gynecol. Obstet. Investig. 2023, 88, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Li, J.; Hua, K.; Chen, Y. Transvaginal natural orifice transluminal endoscopic surgery (vNOTES) hysterectomy for uterus weighing ≥1 kg. BMC Surg. 2020, 20, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Baron, C.; Netter, A.; Tourette, C.; Pivano, A.; Agostini, A.; Crochet, P. Initial experience with vNOTES hysterectomy for benign conditions in a French university hospital. Hum. Reprod. Open 2022, 14, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Nulens, K.; Bosteels, J.; De Rop, C.; Baekelandt, J. vNOTES Hysterectomy for Large Uteri: A Retrospective Cohort Study of 114 Patients. J. Minim. Invasive Gynecol. 2021, 28, 1351–1356. [Google Scholar] [CrossRef] [PubMed]
- Tan, R.C.A.; Ying, K.O.J.; Ng, Q.J.; Qi, M.; Lee, J.M.; Bhutia, K. vNOTES hysterectomy for patients with large uteri: Initial experience in the largest Tertiary Centre in Singapore. Eur. J. Obstet. Gynecol. Reprod. Biol. 2025, 310, 113952. [Google Scholar] [CrossRef] [PubMed]
- Reid, S.; Lu, C.; Casikar, I.; Reid, G.; Abbott, J.; Cario, G.; Chou, D.; Kowalski, D.; Cooper, M.; Condous, G. Prediction of pouch of Douglas obliteration in women with suspected endometriosis using a new real-time dynamic transvaginal ultrasound technique: The sliding sign. Ultrasound Obstet. Gynecol. 2012, 41, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Alcázar, J.L.; Eguez, P.M.; Forcada, P.; Ternero, E.; Martínez, C.; Pascual, M.Á.; Guerriero, S. Diagnostic accuracy of sliding sign for detecting pouch of Douglas obliteration and bowel involvement in women with suspected endometriosis: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2022, 60, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Kaya, C.; Alay, I.; Cengiz, H.; Yıldız, G.O.; Baghaki, H.S.; Yasar, L. Comparison of hysterectomy cases performed via conventional laparoscopy or vaginally assisted natural orifice transluminal endoscopic surgery: A paired sample cross-sectional study. J. Obstet. Gynaecol. 2020, 41, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Hurni, Y.; Simonson, C.; Di Serio, M.; Lachat, R.; Bodenmann, P.; Seidler, S.; Huber, D. Feasibility and safety of vNOTES for gynecological procedures in obese patients. J. Gynecol. Obstet. Hum. Reprod. 2023, 52, 102687. [Google Scholar] [CrossRef] [PubMed]
- Bratzler, D.W.; Dellinger, E.P.; Olsen, K.M.; Perl, T.M.; Auwaerter, P.G.; Bolon, M.K.; Fish, D.N.; Napolitano, L.M.; Sawyer, R.G.; Slain, D.; et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am. J. Health Pharm. 2013, 70, 195–283. [Google Scholar] [CrossRef] [PubMed]
- Park, H.S.; Kim, T.-J.; Song, T.; Kim, M.K.; Lee, Y.-Y.; Choi, C.H.; Lee, J.-W.; Kim, B.-G.; Bae, D.-S. Single-port access (SPA) laparoscopic surgery in gynecology: A surgeon’s experience with an initial 200 cases. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011, 154, 81–84. [Google Scholar] [CrossRef] [PubMed]
| Uterine Weight < 300 gm (n = 66) | Uterine Weight ≥300 gm (n = 38) | |
|---|---|---|
| Age (years) | 44.1 (32–55) | 44.8 (28–52) |
| Parity | 2 (2.1) | 2 (2.0) |
| nulliparous (n) | 2 | 3 |
| Delivery type | ||
| vaginal delivery (n) | 50 (75.8%) | 28 (73.7%) |
| cesarean section (n) | 20 (30.3%) | 9 (23.7%) |
| no history of vaginal delivery (n) | 16 (24.2%) | 10 (26.3%) |
| Body mass index (BMI) (mean) | 23.8 (17.3–37.8) | 24.8 (18.3–32.1) |
| BMI < 24 (n) | 39 (59.1%) | 17 (44.7%) |
| BMI ≥ 24 (n) | 27 (40.9%) | 21 (55.3%) |
| History of abdominal and pelvic surgery, excluding C/S (n) | 8 | 6 |
| Preoperative anemia (Hb < 11) (n) | 19 (28.8%) | 22 (57.9%) |
| Uterine Weight < 300 gm (n = 66) | Uterine Weight ≥ 300 gm (n = 38) | |
|---|---|---|
| Operation time (minutes) | 81 | 98 |
| Estimated blood loss (mL) | 71 (minimal–300) | 143 (50–400) |
| Blood transfusion (n) | 7 (2U) | 10 (2–8U) |
| Hb change (excluding patients needing blood transfusion) | −1.1 (0.3 to −4.6) | −0.9 (−0.1 to −2.4) |
| Length of stay (days) | 2.92 | 3.23 |
| Uterine Weight < 300 gm | Uterine Weight ≥ 300 gm | |||
|---|---|---|---|---|
| BMI < 24 (n = 39) | BMI ≥ 24 (n = 27) | BMI < 24 (n = 17) | BMI ≥ 24 (n = 21) | |
| Operation time (minutes) | 82 | 80 | 89 | 106 |
| Estimated blood loss (mL) | 79 | 59 | 118 | 164 |
| Blood transfusion (n) | 3 | 4 | 3 | 7 |
| Hb change (excluding patients needing blood transfusion) | −1.3 (0.1 to −4.6) | −0.8 (0.3 to −2.5) | −0.8 (−0.1 to −2) | −1.0 (−0.1 to −2.4) |
| Length of stay (days) | 3.07 | 2.70 | 3 | 3.42 |
| CS > 2 times (14) | CS 1 Time (15) | Only VD (70) | Nullipara (5) | |
|---|---|---|---|---|
| Uterine size | 336.6 | 284.0 | 300.4 | 287.3 |
| BMI | 23.81 | 24.38 | 24.04 | 26.65 |
| Operation times | 100 | 90 | 83 | 110 |
| Estimated blood loss (mL) | 89.2 | 92 | 98 | 130 |
| Blood transfusion (n) | 3 | 1 | 11 | 2 |
| Admission days | 3 | 2.86 | 3.07 | 3.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsieh, Y.-T.; Liang, S.-B.; Hsu, Y.-F.; Hsu, C.-S. Novel Application of the Lagis LapBase Cap in Transvaginal NOTES Hysterectomy: Surgical Outcomes and Cost-Effectiveness in 107 Cases. J. Clin. Med. 2025, 14, 7796. https://doi.org/10.3390/jcm14217796
Hsieh Y-T, Liang S-B, Hsu Y-F, Hsu C-S. Novel Application of the Lagis LapBase Cap in Transvaginal NOTES Hysterectomy: Surgical Outcomes and Cost-Effectiveness in 107 Cases. Journal of Clinical Medicine. 2025; 14(21):7796. https://doi.org/10.3390/jcm14217796
Chicago/Turabian StyleHsieh, Yu-Tung, Shi-Bei Liang, Yu-Fang Hsu, and Chun-Shuo Hsu. 2025. "Novel Application of the Lagis LapBase Cap in Transvaginal NOTES Hysterectomy: Surgical Outcomes and Cost-Effectiveness in 107 Cases" Journal of Clinical Medicine 14, no. 21: 7796. https://doi.org/10.3390/jcm14217796
APA StyleHsieh, Y.-T., Liang, S.-B., Hsu, Y.-F., & Hsu, C.-S. (2025). Novel Application of the Lagis LapBase Cap in Transvaginal NOTES Hysterectomy: Surgical Outcomes and Cost-Effectiveness in 107 Cases. Journal of Clinical Medicine, 14(21), 7796. https://doi.org/10.3390/jcm14217796







