Resilience and Intrinsic Capacity in Older Adults: A Review of Recent Literature
Abstract
1. Introduction
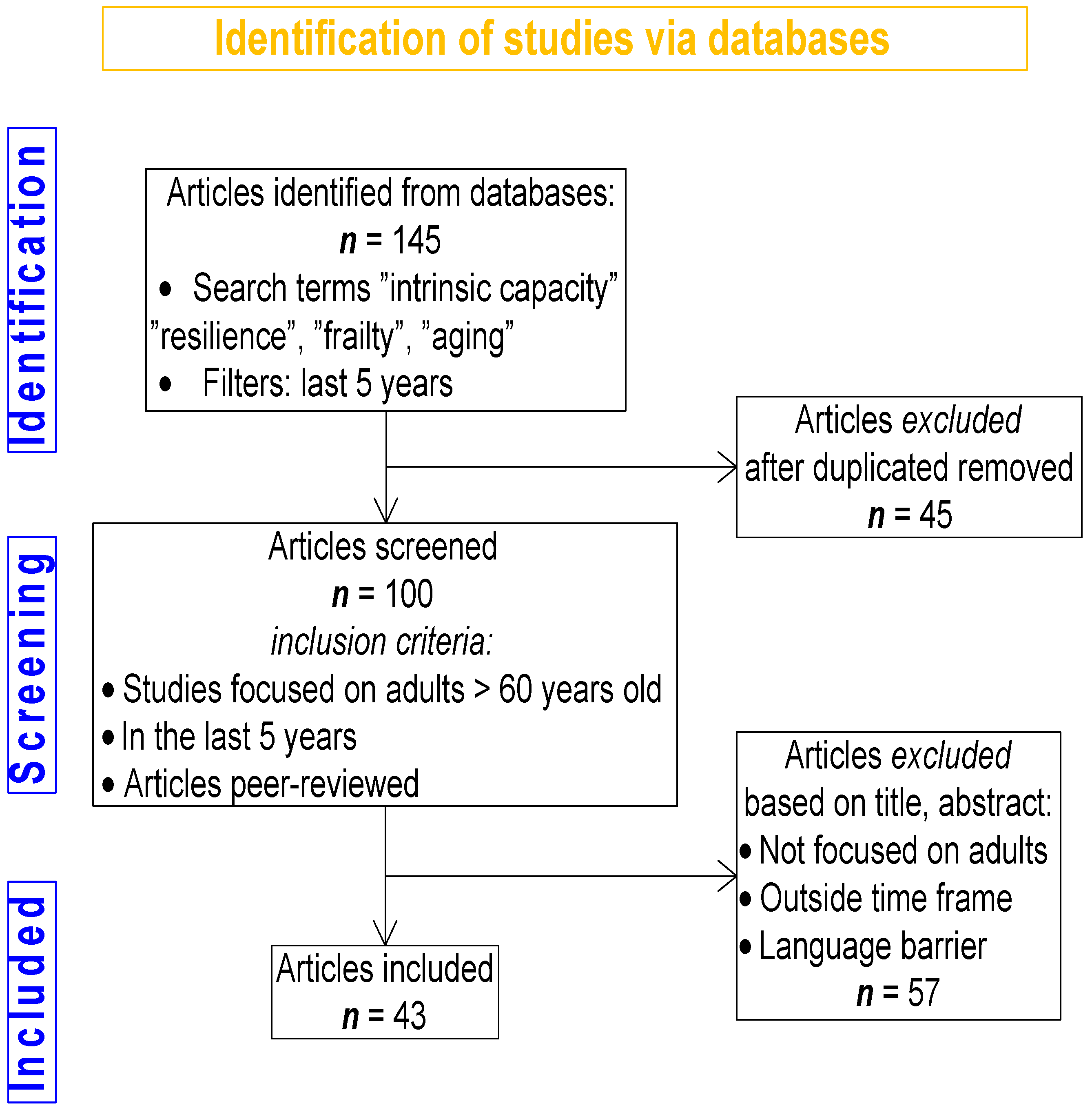
2. Methods
3. Results
3.1. Resilience
3.1.1. Definition
3.1.2. Understanding Resilience—Theoretical Frameworks
3.1.3. Types of Resilience
3.1.4. Factors Influencing Resilience
3.1.5. Multisystem Interactions in Resilience
3.1.6. Immunomodulation: Balanced Neuro-Immune Interplay
3.1.7. Physical Resilience (PR) and Frailty
3.1.8. Measurement of Resilience
3.2. Intrinsic Capacity—Conceptual Framework
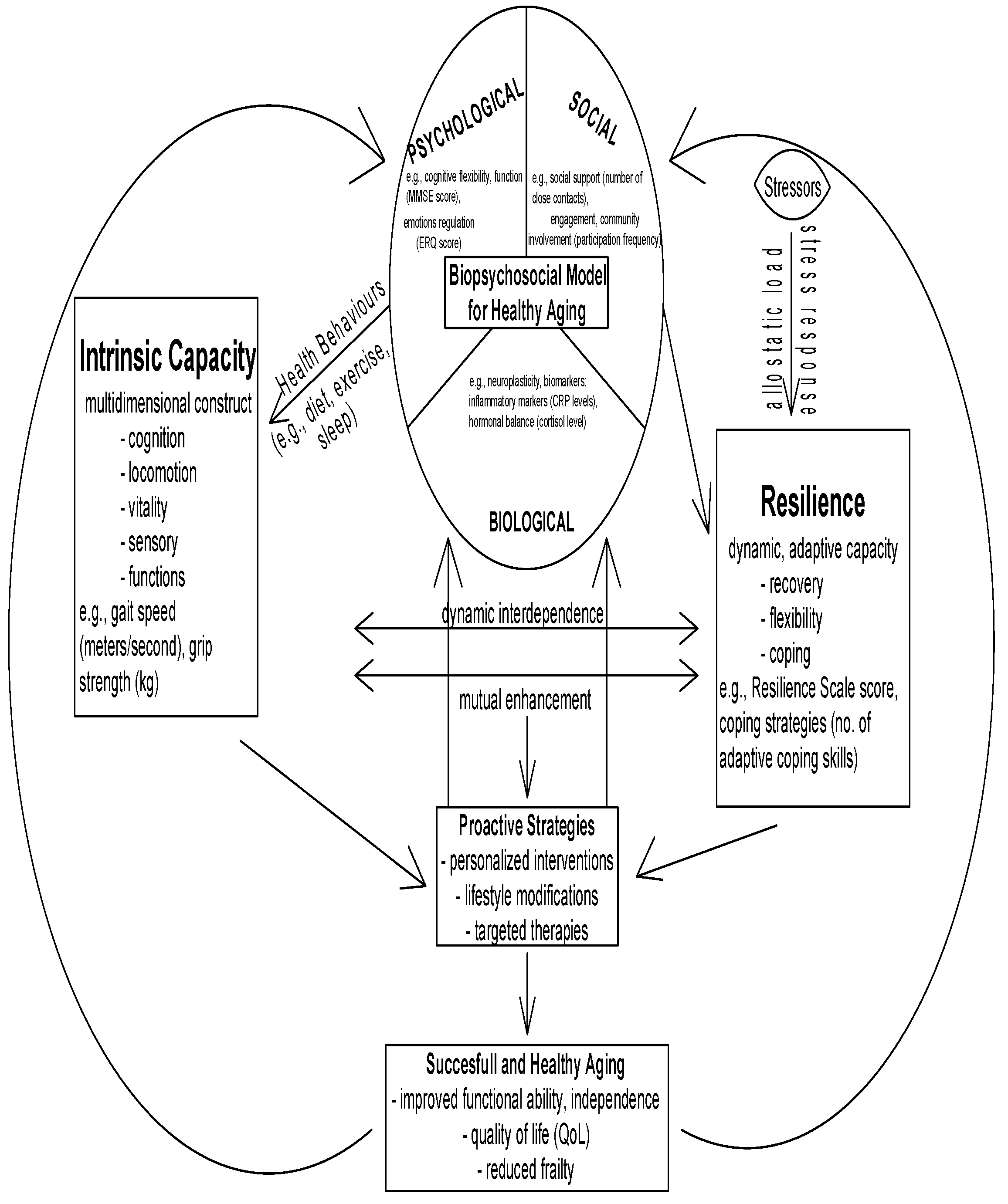
3.2.1. Factors Influencing IC—Biopsychosocial Mechanisms of IC
3.2.2. Measurement of Intrinsic Capacity
- Cognitive: Cognitive evaluation consists of a test battery that includes four components: (a) temporal orientation; (b) delayed recall of 10 common words (episodic memory); (c) a semantic memory questionnaire (based on four questions about general knowledge); and (d) a semantic verbal fluency task (executive functioning, vocabulary size, and lexical access speed). There are authors that use the MMSE test as a quantification of cognitive status [82].
- Psychological: The GDS stands as the most frequent tool used for evaluating depressive symptoms in patients. There are also scales to evaluate sleep quality, a key contributor to mental health outcomes [83].
- Sensory: To evaluate hearing/visual acuity, individuals are asked basic questions to rate their self-assessment of hearing and vision abilities, e.g., “How do you rate your hearing capacity (even when using a hearing device)?” and “How good is your eyesight?”. Participants responded to these questions by selecting from five options: “excellent”, “good”,” fair”, “poor”, or “very poor” [84].
- Locomotor: Balance and gait speed are usually used to estimate lower limb physical functionality. Balance evaluation uses the SPPB (Short Physical Performance Battery), while gait speed is calculated by measuring the time to walk three meters at the usual pace either with or without assistance devices.
- Vitality: The vitality domain combines various underlying factors including nutrition, alongside strength and energy levels. The nutritional status is determined with the help of an MNA test, the handgrip strength of the dominant hand is measured using a dynamometer, and the level of energy is evaluated by asking the subjects to rate their ability to advance tasks during the previous week and how they felt the degree of exhaustion, e.g., “How often did the routine activities require a major effort to be completed?”, and “How often did you feel you could not carry things forward?” [85]. These tools will help healthcare providers monitor changes in intrinsic capacity over time and allow for timely interventions [86].
3.2.3. Interrelation of Resilience and Intrinsic Capacity
How Resilience Influences Intrinsic Capacity
How Intrinsic Capacity Supports Resilience
Illustrative Examples
3.2.4. Intervention to Improve IC and Resilience and Future Directions
3.2.5. The Importance of Assessing Resilience and IC
3.2.6. Impact of CGA, Resilience, and Intrinsic Capacity on Mortality, Disability, Institutionalization, Morbidity, Quality of Life, and Polypharmacy in Older Patients
4. Discussion
4.1. Summary of Main Findings
4.1.1. Overview of Included Studies
4.1.2. Thematic Categorization of Findings
- Assessment Methods of Resilience and Intrinsic Capacity
- b.
- Interventions to Enhance Resilience and Intrinsic Capacity
- -
- Multi-domain exercise programs: Several systematic reviews and meta-analyses demonstrated that structured multicomponent exercise (aerobic, resistance, balance training) significantly improves intrinsic capacity, reducing frailty, and enhancing physical and cognitive performance [14,120,121]. For example, one study reported a 1126% increase in gait speed and a decline in frailty prevalence after >12 weeks of supervised exercise.
- -
- -
- -
- c.
- Effectiveness of Interventions Based on Study Outcomes
- -
- -
- -
4.2. Clinical Implications
4.3. Research Implications
5. Conclusions
6. Limitations
7. Future Directions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 5 May 2025).
- Rudnicka, E.; Napierała, P.; Podfigurna, A.; Męczekalski, B.; Smolarczyk, R.; Grymowicz, M. The World Health Organization (WHO) approach to healthy aging. Maturitas 2020, 139, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Beard, J.R.; Officer, A.; de Carvalho, I.A.; Sadana, R.; Pot, A.M.; Michel, J.P.; Lloyd-Sherlock, P.; Epping-Jordan, J.E.; Peeters, G.M.E.; Mahanani, W.R.; et al. The World report on ageing and health: A policy framework for healthy ageing. Lancet 2016, 387, 2145–2154. [Google Scholar] [CrossRef] [PubMed]
- López-Otín, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. The hallmarks of aging. Cell 2013, 153, 1194–1217. [Google Scholar] [CrossRef]
- López-Otín, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. Hallmarks of aging: An expanding universe. Cell 2023, 186, 243–278. [Google Scholar] [CrossRef] [PubMed]
- Kaeberlein, M.; Rabinovitch, P.S.; Martin, G.M. Healthy aging: The ultimate preventative medicine. Science 2015, 350, 1191–1193. [Google Scholar] [CrossRef]
- Katz, S.; Calasanti, T. Critical perspectives on successful aging: Does it “appeal more than it illuminates”? Gerontologist 2015, 55, 26–33. [Google Scholar] [CrossRef]
- Chhetri, J.K.; Ma, L.; Chan, P. Physical resilience: A novel approach for healthy aging. J. Frailty Sarcopenia Falls 2022, 7, 29–31. [Google Scholar] [CrossRef]
- Windle, G. What is resilience? A review and concept analysis. Clin. Gerontol. 2011, 21, 152–169. [Google Scholar] [CrossRef]
- Tredgold, T. On the transverse strength and resilience of timber. Philos. Mag. 1818, 51, 214–216. [Google Scholar] [CrossRef]
- Cosco, T.D.; Howse, K.; Brayne, C. Healthy ageing, resilience and wellbeing. Epidemiol. Psychiatr. Sci. 2017, 26, 579–583. [Google Scholar] [CrossRef]
- Hadley, E.C.; Kuchel, G.A.; Newman, A.B. Report: NIA workshop on measures of physiologic resiliencies in human aging. J. Gerontol. Ser. A 2017, 72, 980–990. [Google Scholar] [CrossRef]
- Whitson, H.E.; Duan-Porter, W.; Schmader, K.E.; Morey, M.C.; Cohen, H.J.; Colón-Emeric, C.S. Physical resilience in older adults: Systematic review and development of an emerging construct. J. Gerontol. Ser. A 2016, 71, 489–495. [Google Scholar] [CrossRef]
- George, T.; Shah, F.; Tiwari, A.; Gutierrez, E.; Ji, J.; Kuchel, G.A.; Cohen, H.J.; Sedrak, M.S. Resilience in older adults with cancer: A scoping literature review. J. Geriatr. Oncol. 2023, 14, 101349. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Custodero, C.; Demurtas, J.; Smith, L.; Barbagallo, M.; Maggi, S.; Cella, A.; Vanacore, N.; Aprile, P.L.; Ferrucci, L.; et al. Systematic review and umbrella review on comprehensive geriatric assessment in older adults. Age Ageing 2022, 51, afac104. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Shang, S.; Gao, Y.; Zhai, J.; Cheng, X.; Yang, C.; Zhang, R. Measurements of intrinsic capacity in older adults: A scoping review and quality assessment. J. Am. Med. Dir. Assoc. 2023, 24, 267–276.e2. [Google Scholar] [CrossRef] [PubMed]
- Hamaker, M.; Gijzel, S.; Rostoft, S.; van den Bos, F. Intrinsic capacity and resilience: Taking frailty to the next level. J. Geriatr. Oncol. 2023, 14, 101421. [Google Scholar] [CrossRef]
- López-Ortiz, S.; Lista, S.; Peñín-Grandes, S.; Pinto-Fraga, J.; Valenzuela, P.L.; Nisticò, R.; Emanuele, E.; Lucia, A.; Santos-Lozano, A. Defining and assessing intrinsic capacity in older people: A systematic review and a proposed scoring system. Ageing Res. Rev. 2022, 79, 101640. [Google Scholar] [CrossRef]
- Luo, H.; Zheng, Z.; Yuan, Z.; Hu, H.; Sun, C. The effectiveness of multicomponent exercise in older adults with cognitive frailty: A systematic review and meta-analysis. Arch. Public Health 2024, 82, 229. [Google Scholar] [CrossRef]
- Travers, J.; Romero-Ortuno, R.; Langan, F.; MacNamara, F.; McCormack, D.; McDermott, C.; McEntire, J.; McKiernan, J.; Lacey, S.; Doran, P.; et al. Building resilience and reversing frailty: A randomized controlled trial of a primary care intervention for older adults. Age Ageing 2023, 52, afad012. [Google Scholar] [CrossRef]
- Wu, Y.C.; Shen, S.F.; Lee, S.Y.; Chen, L.K.; Tung, H.H. The effectiveness of mind-body approaches for enhancing resilience in older adults: A systematic review and network meta-analysis. Arch. Gerontol. Geriatr. 2023, 109, 104949. [Google Scholar] [CrossRef]
- Górska, S.; Singh Roy, A.; Whitehall, L.; Irvine Fitzpatrick, L.; Duffy, N.; Forsyth, K. A systematic review and correlational meta-analysis of factors associated with resilience of normally aging, community-living older adults. Gerontologist 2022, 62, e520–e533. [Google Scholar] [CrossRef]
- Gijzel, S.M.W.; Rector, J.; van Meulen, F.B.; van der Loeff, R.S.; van de Leemput, I.A.; Scheffer, M.; Olde Rikkert, M.G.M.; Melis, R.J.F. Measurement of dynamical resilience indicators improves the prediction of recovery following hospitalization in older adults. J. Am. Med. Dir. Assoc. 2020, 21, 525–530.e4. [Google Scholar] [CrossRef]
- Lei, H.; Huffman, D.M.; Salmon, A.B.; LeBrasseur, N.K.; Carter, C.; Richardson, A.; Austad, S.; Ladiges, W. Resilience to aging is a heterogeneous characteristic defined by physical stressors. Aging Pathobiol. Ther. 2022, 4, 19–22. [Google Scholar] [CrossRef]
- Whitson, H.E.; Cohen, H.J.; Schmader, K.E.; Morey, M.C.; Kuchel, G.; Colón-Emeric, C.S. Physical resilience: Not simply the opposite of frailty. J. Gerontol. Ser. A 2018, 66, 1459–1461. [Google Scholar] [CrossRef] [PubMed]
- Angevaare, M.J.; Monnier, A.A.; Joling, K.J.; Smalbrugge, M.; Schellevis, F.G.; Hertogh, C.M.P.M.; Huisman, M. The application of the concept of resilience in aging research and older adult care: A focus group study. Front. Med. 2020, 7, 365. [Google Scholar] [CrossRef]
- Rowe, J.W.; Kahn, R.L. Successful aging. Gerontologist 1997, 37, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Parker, C.B.; Colón-Emeric, C.; Huebner, J.L.; Chou, C.-H.; Kraus, V.B.; Pieper, C.F.; Sloane, R.; Whitson, H.E.; Orwig, D.; Crabtree, D.M.; et al. Biomarkers associated with physical resilience after hip fracture. J. Gerontol. Ser. A 2020, 75, e166–e172. [Google Scholar] [CrossRef] [PubMed]
- Southwick, S.M.; Bonanno, G.A.; Masten, A.S.; Panter-Brick, C.; Yehuda, R. Resilience definitions, theory, and challenges: Interdisciplinary perspectives. Eur. J. Psychotraumatol. 2014, 5, 25338. [Google Scholar] [CrossRef]
- Ungar, M. The social ecology of resilience: Addressing contextual and cultural ambiguity of a nascent construct. Am. J. Orthopsychiatry 2011, 81, 1–17. [Google Scholar] [CrossRef]
- Colon-Emeric, C.; Schmader, K.; Cohen, H.J.; Morey, M.; Whitson, H. Ageing and physical resilience after health stressors. Stress Health 2023, 39, 48–54. [Google Scholar] [CrossRef]
- Karatsoreos, I.N.; McEwen, B.S. The neurobiology and physiology of resilience and adaptation across the life course: An annual review. J. Child Psychol. Psychiatry 2013, 54, 337–347. [Google Scholar] [CrossRef] [PubMed]
- Karatsoreos, I.N.; McEwen, B.S. Psychobiological allostasis: Resistance, resilience, and vulnerability. Trends Cogn. Sci. 2011, 15, 576–584. [Google Scholar] [CrossRef] [PubMed]
- Witham, M.D.; Sayer, A.A. Biological resilience in older people—A step beyond frailty? Eur. Geriatr. Med. 2015, 6, 101–102. [Google Scholar] [CrossRef]
- Smith, S.M.; Vale, W.W. The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. Dialogues Clin. Neurosci. 2006, 8, 383–395. [Google Scholar] [CrossRef]
- Jin, Y.; Bhattarai, M.; Kuo, W.C.; Bratzke, L.C. Relationship between resilience and self-care in people with chronic conditions: A systematic review and meta-analysis. J. Clin. Nurs. 2023, 32, 2041–2055. [Google Scholar] [CrossRef]
- Bonanno, G.A.; Mancini, A.D. Beyond resilience and PTSD: Mapping the heterogeneity of responses to potential trauma. Psychol. Trauma Theory Res. Pract. Policy 2012, 4, 74–83. [Google Scholar] [CrossRef]
- Tugade, M.M.; Fredrickson, B.L.; Barrett, L.F. Psychological resilience and positive emotional granularity: Examining the benefits of positive emotions on coping and health. J. Personal. 2004, 72, 1161–1190. [Google Scholar] [CrossRef]
- Gross, J.J. Emotion regulation: Current status and future prospects. Psychol. Inq. 2015, 26, 1–26. [Google Scholar] [CrossRef]
- Waugh, C.E.; Koster, E.H. A resilience framework for promoting stable remission from depression. Clin. Psychol. Rev. 2015, 41, 49–60. [Google Scholar] [CrossRef]
- Luthar, S.S.; Sawyer, J.A.; Brown, P.J. Conceptual issues in studies of resilience: Past, present, and future. Ann. N. Y. Acad. Sci. 2006, 1094, 105–115. [Google Scholar] [CrossRef]
- Montine, T.J.; Cholerton, B.A.; Corrada, M.M.; Edland, S.D.; Flanagan, M.E.; Hemmy, L.S.; Kawas, C.H.; White, L.R. Concepts for brain aging: Resistance, resilience, reserve, and compensation. Alzheimer’s Res. Ther. 2019, 11, 22. [Google Scholar] [CrossRef]
- Walston, J.; Varadhan, R.; Xue, Q.L.; Buta, B.; Sieber, F.; Oni, J.; Imus, P.; Crews, D.C.; Artz, A.; Schrack, J.; et al. A study of physical resilience and aging (SPRING): Conceptual framework, rationale, and study design. J. Am. Geriatr. Soc. 2023, 71, 2393–2405. [Google Scholar] [CrossRef]
- Horgan, S.; Prorok, J.; Ellis, K.; Mullaly, L.; Cassidy, K.L.; Seitz, D.; Checkland, C. Optimizing older adult mental health in support of healthy aging: A pluralistic framework to inform transformative change across community and healthcare domains. Int. J. Environ. Res. Public Health 2024, 21, 664. [Google Scholar] [CrossRef]
- Zhang, Q. An interpretable biological age. Lancet Healthy Longev. 2023, 4, e662–e663. [Google Scholar] [CrossRef]
- Gabrawy, M.M.; Campbell, S.; Carbone, M.A.; Morozova, T.V.; Arya, G.H.; Turlapati, L.B.; Walston, J.D.; Starz-Gaiano, M.; Everett, L.; Mackay, T.F.C.; et al. Lisinopril preserves physical resilience and extends lifespan in a genotype-specific manner in Drosophila melanogaster. J. Gerontol. Ser. A 2019, 74, 1844–1852. [Google Scholar] [CrossRef]
- Deslandes, A.; Moraes, H.; Ferreira, C.; Veiga, H.; Silveira, H.; Mouta, R.; Pompeu, F.A.; Coutinho, E.S.; Laks, J. Exercise and mental health: Many reasons to move. Neuropsychobiology 2009, 59, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Feder, A.; Nestler, E.J.; Charney, D.S. Psychobiology and molecular genetics of resilience. Nat. Rev. Neurosci. 2009, 10, 446–457. [Google Scholar] [CrossRef] [PubMed]
- Aliaz, D.; Loya, A.; Gersner, R.; Haramati, S.; Chen, A.; Zangen, A. Resilience to chronic stress is mediated by hippocampal brain-derived neurotrophic factor. J. Neurosci. 2011, 31, 4475–4483. [Google Scholar] [CrossRef] [PubMed]
- Marcolongo-Pereira, C.; Castro, F.C.A.Q.; Barcelos, R.M.; Chiepe, K.C.M.; Rossoni Junior, J.V.; Ambrosio, R.P.; Chiarelli-Neto, O.; Pesarico, A.P. Neurobiological mechanisms of mood disorders: Stress vulnerability and resilience. Front. Behav. Neurosci. 2022, 16, 1006836. [Google Scholar] [CrossRef]
- Parker, C.B.; Forbes, M.P.; Vahia, I.V.; Forester, B.P.; Jeste, D.V.; Reynolds, C.F. Facing the change together: Reflections of coping and resilience from American geriatric psychiatrists during COVID-19. Int. Psychogeriatr. 2020, 32, 1107–1111. [Google Scholar] [CrossRef]
- Ménard, C.; Pfau, M.L.; Hodes, G.E.; Russo, S.J. Immune and neuroendocrine mechanisms of stress vulnerability and resilience. Neuropsychopharmacology 2017, 42, 62–80. [Google Scholar] [CrossRef]
- Ketcham, A.; Matus, A.; Riegel, B. Resilience and depressive symptoms in adults with cardiac disease: A systematic review. J. Cardiovasc. Nurs. 2022, 37, 312–323. [Google Scholar] [CrossRef] [PubMed]
- Shields, G.S.; Spahr, C.M.; Slavich, G.M. Psychosocial interventions and immune system function: A systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry 2020, 77, 1031–1043. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S. Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiol. Rev. 2007, 87, 873–904. [Google Scholar] [CrossRef] [PubMed]
- Joëls, M.; Baram, T.Z. The neuro-symphony of stress. Nat. Rev. Neurosci. 2009, 10, 459–466. [Google Scholar] [CrossRef]
- Belloni, G.; Cesari, M. Frailty and intrinsic capacity: Two distinct but related constructs. Front. Med. 2019, 6, 133. [Google Scholar] [CrossRef]
- Ng, T.P.; Feng, L.; Nyunt, M.S.Z.; Niti, M.; Tan, B.Y.; Chan, G.; Khoo, S.A.; Chan, S.M.; Yap, P.; Yap, K.B. Nutritional, physical, cognitive, and combined interventions and frailty reversal among older adults: A randomized controlled trial. Am. J. Med. 2015, 128, 1225–1236.e1. [Google Scholar] [CrossRef]
- Kolk, D.; Melis, R.J.F.; MacNeil-Vroomen, J.L.; Buurman, B.M. Physical resilience in daily functioning among acutely ill hospitalized older adults: The Hospital-ADL study. J. Am. Med. Dir. Assoc. 2022, 23, 903.e1–903.e12. [Google Scholar] [CrossRef]
- Varadhan, R.; Walston, J.D.; Bandeen-Roche, K. Can a link be found between physical resilience and frailty in older adults by studying dynamical systems? J. Am. Geriatr. Soc. 2018, 66, 1455–1458. [Google Scholar] [CrossRef]
- Li, J.; Liu, P.; Zhang, Y.; Wang, G.; Zhou, Y.; Xing, Y.; Zhang, L.; Li, Y.; Ma, L. Development of the clinical physical resilience assessment scale (CHEES) in Chinese older adults. J. Frailty Aging 2024, 13, 125–130. [Google Scholar] [CrossRef]
- Chhetri, J.K.; Xue, Q.L.; Ma, L.; Chan, P.; Varadhan, R. Intrinsic capacity as a determinant of physical resilience in older adults. J. Nutr. Health Aging 2021, 25, 1006–1011. [Google Scholar] [CrossRef]
- Pedone, C.; Costanzo, L.; Finamore, P.; Bandinelli, S.; Ferrucci, L.; Incalzi, R.A.A. Defining resilience in older people: Does a subjective definition of stressor work? J. Gerontol. Ser. A 2021, 76, 1480–1485. [Google Scholar] [CrossRef]
- Laskow, T.; Zhu, J.; Buta, B.; Oni, J.; Sieber, F.; Bandeen-Roche, K.; Walston, J.; Franklin, P.D.; Varadhan, R. Risk factors for nonresilient outcomes in older adults after total knee replacement. J. Gerontol. Ser. A 2022, 77, 1915–1922. [Google Scholar] [CrossRef]
- Wister, A.; Li, L.; Ferris, J.; Kim, B.; Klasa, K.; Linkov, I. Resilience among older adults with multimorbidity using the Connor-Davidson scale in the Canadian Longitudinal Study on Aging: Health behaviour, socio-economic, and social support predictors. BMC Public Health 2024, 24, 2567. [Google Scholar] [CrossRef] [PubMed]
- Aizpurua-Perez, I.; Arregi, A.; Labaka, A.; Martinez-Villar, A.; Perez-Tejada, J. Psychological resilience and cortisol levels in adults: A systematic review. Am. J. Hum. Biol. 2023, 35, e23954. [Google Scholar] [CrossRef] [PubMed]
- Ferrucci, L.; Gonzalez-Freire, M.; Fabbri, E.; Simonsick, E.; Tanaka, T.; Moore, Z.; Salimi, S.; Sierra, F.; de Cabo, R. Measuring biological aging in humans: A quest. Aging Cell 2020, 19, e13080. [Google Scholar] [CrossRef] [PubMed]
- Tai, A.P.L.; Leung, M.K.; Geng, X.; Lau, W.K.W. Conceptualizing psychological resilience through resting-state functional MRI in a mentally healthy population: A systematic review. Front. Behav. Neurosci. 2023, 17, 1175064. [Google Scholar] [CrossRef]
- Colón-Emeric, C.; Pieper, C.F.; Schmader, K.E.; Sloane, R.; Bloom, A.; McClain, M.; Magaziner, J.; Huffman, K.M.; Orwig, D.; Crabtree, D.M.; et al. Two approaches to classifying and quantifying physical resilience in longitudinal data. J. Gerontol. Ser. A 2020, 75, 731–738. [Google Scholar] [CrossRef]
- Resnick, B.; Galik, E.; Dorsey, S.; Scheve, A.; Gutkin, S. Reliability and validity testing of the physical resilience measure. Gerontologist 2011, 51, 643–652. [Google Scholar] [CrossRef]
- Wu, L.; Tan, Y.; Liu, Y. Factor structure and psychometric evaluation of the Connor-Davidson resilience scale in a new employee population of China. BMC Psychiatry 2017, 17, 49. [Google Scholar] [CrossRef]
- de Oliveira, V.P.; Ferriolli, E.; Lourenço, R.A.; González-Bautista, E.; Barreto, P.d.S.; de Mello, R.G.B. The sensitivity and specificity of the WHO’s ICOPE screening tool, and the prevalence of loss of intrinsic capacity in older adults: A scoping review. Maturitas 2023, 177, 107818. [Google Scholar] [CrossRef]
- Beard, J.R.; Si, Y.; Liu, Z.; Chenoweth, L.; Hanewald, K. Intrinsic capacity: Validation of a new WHO concept for healthy aging in a longitudinal Chinese study. J. Gerontol. Ser. A 2022, 77, 94–100. [Google Scholar] [CrossRef]
- Zhou, J.; Chang, H.; Leng, M.; Wang, Z. Intrinsic capacity to predict future adverse health outcomes in older adults: A scoping review. Healthcare 2023, 11, 450. [Google Scholar] [CrossRef] [PubMed]
- Meng, L.C.; Huang, S.T.; Peng, L.N.; Chen, L.K.; Hsiao, F.Y. Biological features of the outcome-based intrinsic capacity composite scores from a population-based cohort study: Pas de deux of biological and functional aging. Front. Med. 2022, 9, 851882. [Google Scholar] [CrossRef] [PubMed]
- Beyene, M.B.; Visvanathan, R.; Amare, A.T. Intrinsic capacity and its biological basis: A scoping review. J. Frailty Aging 2024, 13, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Lu, F.; Liu, S.; Liu, X.; Li, J.; Jiang, S.; Sun, X.; Huang, X.; Wang, X. Comparison of the predictive value of intrinsic capacity and comorbidity on adverse health outcomes in community-dwelling older adults. Geriatr. Nurs. 2023, 50, 222–226. [Google Scholar] [CrossRef]
- Tay, L.; Tay, E.L.; Mah, S.M.; Latib, A.; Koh, C.; Ng, Y.S. Association of intrinsic capacity with frailty, physical fitness, and adverse health outcomes in community-dwelling older adults. J. Frailty Aging 2023, 12, 7–15. [Google Scholar] [CrossRef]
- Koivunen, K.; Schaap, L.A.; Hoogendijk, E.O.; Schoonmade, L.J.; Huisman, M.; van Soolingen, N. Exploring the conceptual framework and measurement model of intrinsic capacity defined by the World Health Organization: A scoping review. Ageing Res. Rev. 2022, 80, 101685. [Google Scholar] [CrossRef]
- Leung, A.Y.M.; Su, J.J.; Lee, E.S.H.; Fung, J.T.S.; Molassiotis, A. Intrinsic capacity of older people in the community using WHO integrated care for older people (ICOPE) framework: A cross-sectional study. BMC Geriatr. 2022, 22, 304. [Google Scholar] [CrossRef]
- World Health Organization. Integrated Care for Older People, 2nd ed.; WHO: Geneva, Switzerland, 2025; Available online: https://www.who.int/publications/i/item/9789240103726 (accessed on 25 May 2025).
- Pappalettera, C.; Carrarini, C.; Miraglia, F.; Vecchio, F.; Rossini, P.M. Cognitive resilience/reserve: Myth or reality? A review of definitions and measurement methods. Alzheimer’s Dement. 2024, 20, 3567–3586. [Google Scholar] [CrossRef]
- Lim, M.L.; Lim, D.; Gwee, X.; Nyunt, M.S.; Kumar, R.; Ng, T.P. Resilience, stressful life events, and depressive symptomatology among older Chinese adults. Aging Ment. Health 2015, 19, 1005–1014. [Google Scholar] [CrossRef]
- Nascimento, L.M.; Cruz, T.G.; Silva, J.F.; Silva, L.P.; Inácio, B.B. Use of intrinsic capacity domains as a screening tool in public health. Int. J. Environ. Res. Public Health 2023, 20, 4227. [Google Scholar] [CrossRef] [PubMed]
- Aliberti, M.J.R.; Bertola, L.; Szlejf, C.; Oliveira, D.; Piovezan, R.D.; Cesari, M.; de Andrade, F.B.; Lima-Costa, M.F.; Perracini, R.L.; Ferri, C.P.; et al. Validating intrinsic capacity to measure healthy aging in an upper middle-income country: Findings from the ELSI-Brazil. Lancet Reg. Health—Am. 2022, 12, 100284. [Google Scholar] [CrossRef] [PubMed]
- Rojano, I.; Luque, X.; Blancafort-Alias, S.; Prat Casanovas, S.; Forné, S.; Vergara, N.M.; Povill, P.F.; Royo, M.V.; Serrano, R.; Sanchez-Rodriguez, D.; et al. Identification of decreased intrinsic capacity: Performance of diagnostic measures of the ICOPE screening tool in community-dwelling older people in the VIMCI study. BMC Geriatr. 2023, 23, 106. [Google Scholar] [CrossRef] [PubMed]
- Frolova, E.; Arosio, B.; Lim, W.S. Editorial: Intrinsic capacity and resilience vs. frailty: On the way to healthy aging. Front. Med. 2023, 10, 1155648. [Google Scholar] [CrossRef]
- Yu, R.; Leung, J.; Leung, G.; Woo, J. Towards healthy ageing: Using the concept of intrinsic capacity in frailty prevention. J. Nutr. Health Aging 2022, 26, 30–36. [Google Scholar] [CrossRef]
- Maheshwari, S.; Dai, C.; Giri, S.; Harmon, C.; Tucker, A.; Fowler, M.E.; Outlaw, D.; Williams, G.R. Intrinsic capacity and survival among older adults with gastrointestinal malignancies: The Cancer and Aging Resilience Evaluation registry. Cancer 2024, 130, 3530–3539. [Google Scholar] [CrossRef]
- Rippl, M.; Huemer, M.T.; Schwettmann, L.; Grill, E.; Peters, A.; Drey, M.; Thorand, B. Comparison of robustness, resilience, and intrinsic capacity including prediction of long-term adverse health outcomes: The KORA-Age study. J. Nutr. Health Aging 2025, 29, 100433. [Google Scholar] [CrossRef]
- Turusheva, A.V.; Kotovskaya, Y.V.; Frolova, E.V. The impact of psychological resilience, as a component of intrinsic capacity, on the risk of developing atrial fibrillation. Adv. Gerontol. 2023, 36, 239–246. (In Russian) [Google Scholar] [PubMed]
- Guaraldi, G.; Milic, J.; Barbieri, S.; Marchiò, T.; Caselgrandi, A.; Motta, F.; Beghè, B.; Verduri, A.; Belli, M.; Gozzi, L.; et al. Quality of life and intrinsic capacity in patients with post-acute COVID-19 syndrome is in relation to frailty and resilience phenotypes. Sci. Rep. 2023, 13, 8956. [Google Scholar] [CrossRef]
- Hu, F.W.; Yueh, F.R.; Fang, T.J.; Chang, C.M.; Lin, C.Y. Testing a conceptual model of physiologic reserve, intrinsic capacity, and physical resilience in hospitalized older patients: A structural equation modeling. Geriatrics 2024, 70, 165–172. [Google Scholar] [CrossRef]
- de Souto Barreto, P.; Rolland, Y.; Ferrucci, L.; Arai, H.; Bischoff-Ferrari, H.; Duque, G.; Fielding, R.A.; Beard, J.R.; Muscedere, J.; Sierra, F.; et al. Looking at frailty and intrinsic capacity through a geroscience lens: The ICFSR & Geroscience Task Force. Nat. Aging 2023, 3, 1474–1479. [Google Scholar] [CrossRef]
- Huang, C.H.; Okada, K.; Matsushita, E.; Uno, C.; Satake, S.; Martins, B.A.; Kuzuya, M. The association of social frailty with intrinsic capacity in community-dwelling older adults: A prospective cohort study. BMC Geriatr. 2021, 21, 515. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Bautista, E.; Andrieu, S.; Gutiérrez-Robledo, L.M.; García-Chanes, R.E.; de Souto Barreto, P. In the quest of a standard index of intrinsic capacity: A critical literature review. J. Nutr. Health Aging 2020, 24, 959–965. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Yang, T.; Wang, X.; He, X.; Dong, J.; Qian, Q.; Zhang, X.; Zheng, J.; Ma, Y. The ability of decline in intrinsic capacity to indicate the risk of mortality in older adults: A meta-analysis. Maturitas 2024, 189, 108109. [Google Scholar] [CrossRef] [PubMed]
- Sirikul, W.; Buawangpong, N.; Pinyopornpanish, K.; Siviroj, P. Impact of multicomponent exercise and nutritional supplement interventions for improving physical frailty in community-dwelling older adults: A systematic review and meta-analysis. BMC Geriatr. 2024, 24, 958. [Google Scholar] [CrossRef]
- Tay, L.; Tay, E.L.; Mah, S.M.; Latib, A.; Ng, Y.S. Intrinsic capacity rather than intervention exposure influences reversal to robustness among prefrail community-dwelling older adults: A non-randomized controlled study of a multidomain exercise and nutrition intervention. Front. Med. 2022, 9, 971497. [Google Scholar] [CrossRef]
- Lim, K.Y.; Lo, H.C.; Cheong, I.F.; Wang, Y.Y.; Jian, Z.R.; Chen, I.C.; Chan, Y.C.; Lee, S.D.; Chou, C.C.; Yang, F.L. Healthy eating enhances intrinsic capacity, thus promoting functional ability of retirement home residents in Northern Taiwan. Nutrients 2022, 14, 2225. [Google Scholar] [CrossRef]
- Merchant, R.A.; Chan, Y.H.; Anbarasan, D.; Woo, J. The impact of exercise and cognitive stimulation therapy on intrinsic capacity composite score in pre-frail older adults: A pre-post intervention study. J. Frailty Aging 2024, 13, 131–138. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Aging and Health; WHO: Geneva, Switzerland, 2015; Available online: https://www.who.int/publications/i/item/9789241565042 (accessed on 25 May 2025).
- Yoshimura, Y.; Matsumoto, A.; Inoue, T.; Okamura, M.; Kuzuya, M. Protein supplementation alone or combined with exercise for sarcopenia and physical frailty: A systematic review and meta-analysis of randomized controlled trials. Arch. Gerontol. Geriatr. 2025, 131, 105783. [Google Scholar] [CrossRef]
- Oktaviana, J.; Zanker, J.; Vogrin, S.; Duque, G. The effect of protein supplements on functional frailty in older persons: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2020, 86, 103938. [Google Scholar] [CrossRef] [PubMed]
- Liao, X.; Shen, J.; Li, M. Effects of multi-domain intervention on intrinsic capacity in older adults: A systematic review of randomized controlled trials. Exp. Gerontol. 2023, 174, 112112. [Google Scholar] [CrossRef]
- Sánchez-Sánchez, J.L.; Lu, W.H.; Gallardo-Gómez, D.; Del Pozo Cruz, B.; de Souto Barreto, P.; Lucia, A.; Valenzuela, P.L. Association of intrinsic capacity with functional decline and mortality in older adults: A systematic review and meta-analysis of longitudinal studies. Lancet Healthy Longev. 2024, 5, e480–e492. [Google Scholar] [CrossRef] [PubMed]
- Toth, E.E.; Ihász, F.; Ruíz-Barquín, R.; Szabo, A. Physical activity and psychological resilience in older adults: A systematic review of the literature. J. Aging Phys. Act. 2023, 32, 276–286. [Google Scholar] [CrossRef] [PubMed]
- George, P.P.; Lun, P.; Ong, S.P.; Lim, W.S. A rapid review of the measurement of intrinsic capacity in older adults. J. Nutr. Health Aging 2021, 25, 774–782. [Google Scholar] [CrossRef]
- Ji, L.; Jazwinski, S.M.; Kim, S. Frailty and biological age. Ann. Geriatr. Med. Res. 2021, 25, 141–149. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Sayer, A.A. Sarcopenia. Lancet 2019, 393, 2636–2646. [Google Scholar] [CrossRef]
- Charles, A.; Buckinx, F.; Locquet, M.; Reginster, J.Y.; Petermans, J.; Gruslin, B.; Bruyère, O. Prediction of adverse outcomes in nursing home residents according to intrinsic capacity proposed by the World Health Organization. J. Gerontol. Ser. A 2020, 75, 1594–1599. [Google Scholar] [CrossRef]
- Ahmadi, S.; Afshar, P.F.; Malakouti, K.; Azadbakht, M. The relationship between intrinsic capacity and functional ability in older adults. BMC Geriatr. 2025, 25, 57. [Google Scholar] [CrossRef]
- Zhou, Y.; Ma, L. Intrinsic capacity in older adults: Recent advances. Aging Dis. 2022, 13, 353–359. [Google Scholar] [CrossRef]
- Liu, A.; You, Y.; Wang, Y.; Li, L.; Yuan, J. Research on intrinsic capacity as a predictor of falls and disability in community-dwelling elderly. Front. Aging 2025, 6, 1589369. [Google Scholar] [CrossRef]
- Romaa, M.F.B.; Garçãob, N.I.B.; Covinskyc, K.E.; Alibertab, M.J.R. Delivering patient-centered care: Outcomes of comprehensive geriatric assessment across healthcare settings. Geriatr. Gerontol. Int. 2023, 16, 1–12. [Google Scholar] [CrossRef]
- Ellis, G.; Gardner, M.; Tsiachristas, A.; Langhorne, P.; Burke, O.; Harwood, R.H.; Conroy, S.P.; Kircher, T.; Somme, D.; Saltvedt, I.; et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst. Rev. 2017, 2017, CD006211. [Google Scholar] [CrossRef] [PubMed]
- Bao, D.Y.; Wu, L.Y.; Cheng, Q.Y. Effect of a comprehensive geriatric assessment nursing intervention model on older patients with diabetes and hypertension. World J. Clin. Cases 2024, 12, 4065–4073. [Google Scholar] [CrossRef] [PubMed]
- Yen, P.C.; Lo, Y.T.; Lai, C.C.; Lee, C.C.; Fang, C.J.; Chang, C.M.; Yang, Y.C. Effectiveness of outpatient geriatric evaluation and management intervention on survival and nursing home admission: A systematic review and meta-analysis of randomized controlled trials. BMC Geriatr. 2023, 23, 414. [Google Scholar] [CrossRef]
- Pereza, M.; Goulart, B.; Zuchen, F.; Fonseca, F.L.; Lourenço, R.A. The impact of intrinsic capacity and physical resilience on health outcomes: A case report. Geriatr. Gerontol. Int. 2023, 17, 1–4. [Google Scholar] [CrossRef]
- Xu, Y.; Ji, T.; Li, X.; Yang, Y.; Zheng, L.; Qiu, Y.; Chen, L.; Li, G. The effectiveness of the comprehensive geriatric assessment for older adults with frailty in hospital settings: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2024, 159, 104849. [Google Scholar] [CrossRef]
- Sum, G.; Nicholas, S.O.; Nai, Z.L.; Ding, Y.Y.; Tan, W.S. Health outcomes and implementation barriers and facilitators of comprehensive geriatric assessment in community settings: A systematic integrative review [PROSPERO registration no.: CRD42021229953]. BMC Geriatr. 2022, 22, 379. [Google Scholar] [CrossRef]
- Safitri, E.D.; Ranakusuma, R.W.; Siagian, N.K.P.; Marsigit, J.; Saldi, S.R.F.; Widyaningsih, W.; Istanti, R.; Azwar, M.K.; Siregar, R.A.; Harimurti, K.; et al. The effectiveness of comprehensive geriatric assessment intervention for older people in outpatient setting: A systematic review/meta-analysis. BMC Geriatr. 2025, 25, 418. [Google Scholar] [CrossRef]
- Vidinha Pereira, A.L.; Vaz, A.; Paúl, C.; Santiago, L.; Rosendo, I. Comprehensive geriatric assessment in primary healthcare: A scoping review protocol. BMJ Open 2025, 15, e091095. [Google Scholar] [CrossRef]
- Yang, X.; Li, S.; Xu, L.; Liu, H.; Li, Y.; Song, X.; Bao, J.; Liao, S.; Xi, Y.; Guo, G. Effects of multicomponent exercise on frailty status and physical function in frail older adults: A meta-analysis and systematic review. Exp. Gerontol. 2024, 197, 112604. [Google Scholar] [CrossRef]
- Sihvola, S.; Kuosmanen, L.; Kvist, T. Resilience and related factors in colorectal cancer patients: A systematic review. Eur. J. Oncol. Nurs. 2022, 56, 102079. [Google Scholar] [CrossRef] [PubMed]
- Andaloro, S.; Cacciatore, S.; Risoli, A.; Comodo, R.M.; Brancaccio, V.; Calvani, R.; Giusti, S.; Schlögl, M.; D’Angelo, E.; Tosato, M.; et al. Hip fracture as a systemic disease in older adults: A narrative review on multisystem implications and management. Med. Sci. 2025, 13, 89. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Vélez, R.; Iriarte-Fernández, M.; Santafé, G.; Malanda, A.; Beard, J.R.; Garcia-Hermoso, A.; Izquierdo, M. Association of intrinsic capacity with incidence and mortality of cardiovascular disease: Prospective study in UK Biobank. J. Cachexia Sarcopenia Muscle 2023, 14, 2054–2063. [Google Scholar] [CrossRef] [PubMed]
- Zarate Rodriguez, J.G.; Cos, H.; Koenen, M.; Cook, J.; Kasting, C.; Raper, L.; Guthrie, T.; Strasberg, S.M.; Hawkins, W.G.; Hammill, C.W.; et al. Impact of prehabilitation on postoperative mortality and the need for non-home discharge in high-risk surgical patients. J. Am. Coll. Surg. 2023, 237, 558–567. [Google Scholar] [CrossRef]
- Lee, W.J.; Peng, L.N.; Lin, M.H.; Kim, S.; Hsiao, F.Y.; Chen, L.K. Enhancing intrinsic capacity and related biomarkers in community-dwelling multimorbid older adults through integrated multidomain interventions: Ancillary findings from the Taiwan integrated geriatric (TIGER) trial. J. Am. Med. Dir. Assoc. 2024, 25, 757–763.e4. [Google Scholar] [CrossRef]
- Ding, X.; Zhao, F.; Wang, Q.; Zhu, M.; Kan, H.; Fu, E.; Wei, S.; Li, Z. Effects of interventions for enhancing resilience in cancer patients: A systematic review and network meta-analysis. Clin. Psychol. Rev. 2024, 108, 102381. [Google Scholar] [CrossRef]
- Koivunen, K.; Lindeman, K.; Välimaa, M.; Rantanen, T. Investigating resilience through intrinsic capacity networks in older adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2024, 79, glae048. [Google Scholar] [CrossRef]
- Cesari, M.; Landi, F.; Vellas, B.; Bernabei, R.; Marzetti, E. Sarcopenia and physical frailty: Two sides of the same coin. Front. Aging Neurosci. 2014, 6, 192. [Google Scholar] [CrossRef]
- Sánchez-Sánchez, J.L.; de Souto Barreto, P.; Antón-Rodrigo, I.; Ramón-Espinoza, F.; Marín-Epelde, I.; Sánchez-Latorre, M.; Moral-Cuesta, D.; Casas-Herrero, Á. Effects of a 12-week Vivifrail exercise program on intrinsic capacity among frail cognitively impaired community-dwelling older adults: Secondary analysis of a multicentre randomised clinical trial. Age Ageing 2022, 51, afac303. [Google Scholar] [CrossRef]
- Trică, A.; Golu, F.; Sava, N.I.; Licu, M.; Zanfirescu, Ș.A.; Adam, R.; David, I. Resilience and successful aging: A systematic review and meta-analysis. Acta Psychol. 2024, 248, 104357. [Google Scholar] [CrossRef]
- Li, J.; Chhetri, J.K.; Ma, L. Physical resilience in older adults: Potential use in promoting healthy aging. Ageing Res. Rev. 2022, 81, 101701. [Google Scholar] [CrossRef]
| Term | Definition | Characteristics | Interrelationship |
|---|---|---|---|
| Resilience | The dynamic ability to adapt to stressors, bounce back from adversity, and maintain or regain stability across mental, emotional, and physical domains. | Adapts to both acute and chronic stressors, influenced by intrinsic and extrinsic factors, including social support and coping mechanisms. | Relies on intrinsic capacity, supports recovery and adaptation, enhances functional ability. |
| Intrinsic Capacity | A holistic measure of an individual’s physical and mental capacities, comprising domains like cognition, locomotion, vitality, and psychological well-being. | Multidimensional, focuses on baseline reserves, influenced by biological, psychological, and social factors. | Supports resilience, indicative of functional reserve and overall health. |
| Functional Ability | The capacity to meet daily needs, make decisions, and maintain independence, reflecting the practical application of intrinsic capacities and resilience. | Practical, day-to-day application, dependent on both intrinsic capacity and resilience, sensitive to environmental support. | Enhanced by strong intrinsic capacity and resilience, reflective of successful aging. |
| Successful Aging | A process of maintaining physical health, mental well-being, active engagement in life, and independence through aging. | Encompasses both intrinsic capacity and resilience, characterized by reduced chronic disease burden, high function, and quality of life. | Achieved through optimized intrinsic capacity, resilience, and supportive environments, indicating healthy aging. |
| Type of Resilience | Definition | Typical Examples | Determined by | Diagnostic Scales/Tools | Purpose of the Scales |
|---|---|---|---|---|---|
| Acute Resilience | The ability to respond quickly and effectively to a sudden, singular, or intense stressor | Recovery after surgery, a fall, or a stroke | Speed of recovery, baseline functional status, nervous and hormonal system reactivity |
|
|
| Chronic Resilience | The ability to maintain functionality and cope with a persistent or recurring stressor over time | Living with a chronic illness, long-term disability, ongoing psychosocial stress | Long-term coping mechanisms, social support, psychological factors, and lifestyle |
|
|
| Type of Resilience | Definition | Typical Examples | Determined by | Diagnostic Scales/Tools | Purpose of Scales |
|---|---|---|---|---|---|
| Psychological Resilience | The capacity to maintain or regain stable mental health and adapt well in the face of adversity, sustaining functioning without long-term psychological disruption | Coping with trauma, major life changes, interpersonal crises | Cognitive appraisal, self-efficacy, optimism, social support, coping skills | CD-RISC, RS-14/RS-25, Brief Resilience Scale | Assess resilience as maintenance/adaptation; evaluate interventions; predict long-term mental health outcomes |
| Emotional Resilience | The ability to recognize, manage, and recover from emotional stressors and regulate emotional responses effectively | Managing sadness, anger, fear, grief; sustaining equilibrium in emotional upheaval | Emotional awareness, regulation, optimism, internal/external resource use | ERQ, emotional intelligence inventories | Evaluate emotional coping, regulation capacity, and recovery from emotional disruption |
| General Health Resilience | A broad construct referring to the ability to maintain or return to overall good health status across domains (mental, physical, functional) in response to health challenges | Sustaining quality of life during chronic illness, multimorbidity, or after hospitalization | Multi-domain functioning: self-rated health, behavior, social support, lifestyle factors | WHOQOL-BREF, health-related quality-of-life scales, multi-domain resilience questionnaires | Assess long-term well-being, guide care planning, and evaluate adaptation across health domains |
| Physical Resilience | The ability to resist functional decline or recover functional abilities following physical stressors; rooted in physiological reserve and recovery trajectory | Recovering mobility after surgery or fall, restoring strength after illness | Physiological reserve, baseline function, neuromuscular and hormonal reactivity | Short Physical Performance Battery (SPPB), Clinical Frailty Scale (CFS), grip strength test, gait speed, Physical Resilience Scale | Evaluate functional capacity, Predict recovery trajectory, Guide rehabilitation planning and care decisions. |
| Domain/Method | Assessment Tool | Advantages | Limitations | Scope/Applicable Population |
|---|---|---|---|---|
| Composite Intrinsic Capacity (IC) | Summed/averaged standardized domain scores | Captures multidimensional reserve; flexible across studies | Heterogeneous scoring; poor cross-study comparability; no standard reference | Research in health in older adults |
| Locomotion | Short Physical Performance Battery (SPPB; chair stand, gait speed, balance | Strong predictor of disability and mortality, widely validated; objective and reliable | Requires space, in-person testing, trained staff; time-consuming in high-throughput settings | Community-dwelling and clinical geriatric populations |
| Gait speed test (4–6 m walk) | Validated predictor of adverse outcomes; simple, quick, robust across settings | May not fully capture mobility nuances (e.g., dynamic stability) | Used in both outpatient and inpatient older adults | |
| Vitality | Handgrip strength (dynamometer) | Correlates with muscle mass and mortality, easy to administer | Single measure of vitality only; affected by participant effort | Broader adult and older adult cohorts |
| Mini-Nutritional Assessment—Short Form (MNA—SF) | Multidimensional; validated nutritional risk screening | Less objective; may miss early declines, relies on self-report | Community-living and clinical older adults | |
| Appendicular skeletal muscle mass (Bioelectrical impedance Analysis) | Linked to frailty; objective quantitative measure | Affected by hydration status; equipment dependent | Research and clinical settings with equipment | |
| Cognition | Mini-Mental State Examination (MMSE) | Widely used and normed | Ceiling/floor effects; educational/cultural bias | Primary care and specialist geriatric assessments |
| Psychological | Geriatric Depression Scale (GDS 10/15) | Short and feasible; validated for elderly depressive symptoms | Not resilience-specific; self-report subject to bias; mood-sensitive | Depressive screening in older adults |
| Sensory | Self-reported vision and hearing questionnaires | Suitable for large samples; easy, low-cost | Poor sensitivity to subclinical losses; subjective; recall bias | Population surveys and primary care |
| Snellen/Tumbling E chart, audiometry | Flexible across studies; captures multidimensional reserve | No standard reference; poor cross-study comparability; heterogeneous scoring | Ophthalmology/audiology clinics | |
| Physical Resilience (PR) | Physical Resilience Scale (PRS): 15-item self-report scale developed to assess older adults’ physical resilience in response to health stressors | Correlates significantly with general resilience measures and physical activity; demonstrated good internal consistency and moderate test–retest reliability; I Self-report | Includes few highly challenging items, making it less sensitive in individuals with high baseline resilience | Community-dwelling older adults in US housing sites (age ~76), with single-group repeated measures |
| Physical resilience instrument for older adults (PRIFOR-16): 16-item multidimensional scale assessing positive thinking, ADL coping, and hope. Validated in post-acute hospital populations in Taiwan | Reflects a multidimensional conceptualization of resilience; suitable for older adults recovering from acute illness; excellent internal consistency; strong criterion validity with frailty, cognition, depression | Certain items show ceiling effects in high-functioning individuals; mostly validated in hospital-based samples in Asia; no published data on test–retest reliability or responsiveness | Vulnerable and frail ≥65-year-olds in Taiwanese hospital wards; verified for predictive validity over 1 month | |
| PRIFOR-4 (Short Form) | Brief; maintains conceptual focus of long-form; easy to administer in busy clinical environments | Psychometric data on test–retest reliability still limited; convergent validity modest; shortened length may reduce sensitivity to nuanced coping strategies | Designed for quick clinical screening; same hospitalized older adult group as PRIFOR-16 | |
| Connor–Davidson Resilience Scale (CD-RISC) | Detects adaptive coping; psychometrically robust | Structure inconsistencies; self-report; cultural biases; may not reflect actual physiological resilience | General population, military, clinical groups (e.g., PTSD, surgery) | |
| CHEES Scale (Comprehensive High-functioning Engagement and Evaluation Scale) | Assesses engagement and resilience behaviors | Still under validation; multidimensional | Suitable for community-dwelling and clinical populations | |
| Residual Methods (e.g., residual distance to predicted decline) | Detects subtle changes over time | Complex modeling; requires longitudinal data | Research settings, longitudinal studies | |
| Dynamic Balance Recovery Measures: Limits of Stability Tests, Postural Sway Analysis | Measures balance recovery, dynamic stability | Requires specialized equipment; in-lab only | Clinical and research settings; fall-risk assessment |
| Intervention Type | IC Domains Targeted | Components | Key Findings | Author (Year) |
|---|---|---|---|---|
| Multicomponent Exercise Program | Locomotion, strength, balance, cognition | ≥12 wk. supervised/group exercise combining aerobic, resistance, balance training | Significant frailty reduction; improvements in muscle strength, gait speed, balance; improved SPPB (Short Physical Performance Battery), and TUG (Timed Up and Go) score | Yang (2024) [124] |
| Multicomponent Exercise in Cognitive Frailty | Cognitive, locomotion, strength | Group-based aerobic + resistance >120 min/week | Improved cognition, grip strength, lower limb strength, and frailty | Luo (2024) [19] |
| Home-Based Strength Training + Protein (1.2 g/kg/day) | Vitality, locomotion | Resistance exercises + dietary protein guidance for 3 mo. | Frailty decreased from 17.7% to 6.3% vs. control (OR 0.23); improved grip strength and bone mass | Travers (2023) [20] |
| Protein Supplementation + Exercise (Meta-analysis) | Muscle mass, strength, performance | Whey/EAAs + resistance training ≥24 wk. | Improved skeletal muscle index, and improved handgrip vs. exercise only | Yoshimura (2025) [103] |
| Protein Alone (Meta-analysis) | Muscle mass, strength, function | Oral protein Supplementation (≥15 g/d) | No significant benefit on LBM, strength, SPPB, or gait | Oktaviana (2020) [104] |
| Study/Source | Study Design | Population | Interventions | Targeted IC Domains | Main Outcomes | Reported Effectiveness | Duration | Frequency and Intensity | Adherence Rate |
|---|---|---|---|---|---|---|---|---|---|
| Yang et al. (2024) [124] | Systematic review and meta-analysis | Frail older adults | ≥12-week multicomponent exercise | Locomotion, strength, balance, cognition | Frailty reduction, gait speed increase, muscle strength improvement | >20% reduction in frailty; significant performance gains | ≥12 weeks | 3 sessions/week, 60 min/session | 85% |
| Yoshimura et al. (2025) [103] | Systematic review and meta-analysis | Older adults with sarcopenia | Protein supplementation ± exercise | Vitality, locomotion | Muscle mass and strength ↑, fall risk ↓ | Notable improvements in physical function | Variable | 3–4 sessions/week, moderate intensity | 80% |
| Wu et al. (2023) [21] | Systematic review and meta-analysis | Community-dwelling older adults | Mind-body interventions (mindfulness, yoga) | Psychological, resilience | Resilience and mental health ↑ | Significant psychological resilience enhancements | Variable | 1–2 sessions/week, 30–60 min/session | Varies |
| Li et al. (2024) [97] | Meta-analysis | Community-dwelling older adults | Multi-domain interventions (exercise, nutrition, cognitive) | Multiple IC domains | Frailty, functional decline, mortality ↓ | Significant improvements; lower adverse events | Variable | Varies, multi-domain interventions | 75% |
| Luo et al. (2024) [19] | Systematic review and meta-analysis | Older adults with cognitive frailty | ≥12-week multicomponent exercise | Locomotion, cognition | Gait, strength, frailty ↓ | Improved physical and cognitive functions | ≥12 weeks | 3 sessions/week, 60 min/session | 75–80% |
| Travers et al. (2023) [20] | RCT | Older adults | 6-month multicomponent program | Physical, cognitive, nutritional | Frailty and disability ↓ | 77% reduction in frailty; improved quality of life | 6 months | 4 sessions/week, 45 min/session | 80% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grigoraș, G.; Ilie, A.C.; Turcu, A.-M.; Albișteanu, S.-M.; Lungu, I.-D.; Ștefăniu, R.; Pîslaru, A.I.; Gavrilovici, O.; Alexa, I.D. Resilience and Intrinsic Capacity in Older Adults: A Review of Recent Literature. J. Clin. Med. 2025, 14, 7729. https://doi.org/10.3390/jcm14217729
Grigoraș G, Ilie AC, Turcu A-M, Albișteanu S-M, Lungu I-D, Ștefăniu R, Pîslaru AI, Gavrilovici O, Alexa ID. Resilience and Intrinsic Capacity in Older Adults: A Review of Recent Literature. Journal of Clinical Medicine. 2025; 14(21):7729. https://doi.org/10.3390/jcm14217729
Chicago/Turabian StyleGrigoraș, Gabriela, Adina Carmen Ilie, Ana-Maria Turcu, Sabinne-Marie Albișteanu, Iulia-Daniela Lungu, Ramona Ștefăniu, Anca Iuliana Pîslaru, Ovidiu Gavrilovici, and Ioana Dana Alexa. 2025. "Resilience and Intrinsic Capacity in Older Adults: A Review of Recent Literature" Journal of Clinical Medicine 14, no. 21: 7729. https://doi.org/10.3390/jcm14217729
APA StyleGrigoraș, G., Ilie, A. C., Turcu, A.-M., Albișteanu, S.-M., Lungu, I.-D., Ștefăniu, R., Pîslaru, A. I., Gavrilovici, O., & Alexa, I. D. (2025). Resilience and Intrinsic Capacity in Older Adults: A Review of Recent Literature. Journal of Clinical Medicine, 14(21), 7729. https://doi.org/10.3390/jcm14217729





