Minimizing Permanent Pacemaker Implantation After TAVR: Current Strategies, Monitoring Pathways, and Future Directions
Abstract
1. Introduction
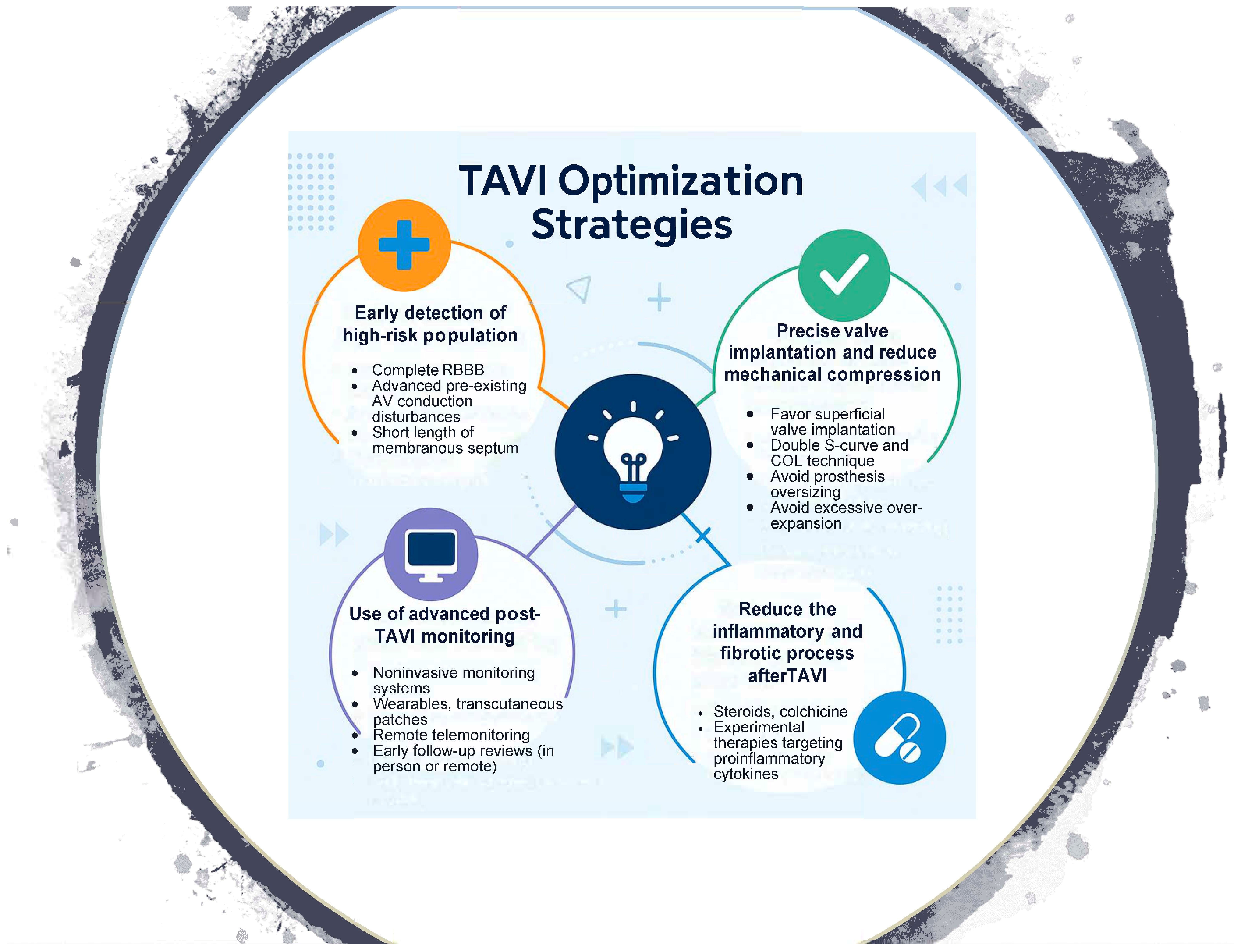
2. Procedural Techniques
- The double S-curve and the cusp-overlap technique: Recently introduced for self-expanding TAVR platforms, this method establishes the optimal fluoroscopic projection to guide valve implantation. Its objective is to achieve a shallower implantation at the aortic annulus, thereby reducing the risk of conduction disturbances by avoiding protrusion beyond the membranous septum, where the conduction system is more superficial. This strategy allows for more accurate control of implant depth and minimizes trauma to the conduction system, which may, in turn, decrease the incidence of permanent pacemaker implantation [5,6,7].
- The membranous septum: With current non-invasive imaging techniques, particularly computed tomography, the membranous septum can be accurately measured. Knowledge of its length provides valuable information for procedural planning, as it allows operators to perform higher valve implantations as a strategy to reduce the risk of high-grade atrioventricular block and, consequently, the need for permanent pacemaker implantation [8,9,10].
3. Patient and Valve Selection
- Baseline Conduction Disorders and Valve Type Selection: The presence of conduction abnormalities such as right bundle branch block (RBBB), left anterior fascicular block (LAFB), or bradyarrhythmias significantly increases the likelihood of permanent pacemaker implantation (PPI) after TAVR [11,12]. In the PARTNER trial, pre-existing conduction disturbances were independently associated with higher PPI rates, longer hospital stays, and a greater incidence of adverse clinical events [11]. In this context, balloon expandable valves are often preferred in patients with baseline conduction disease, as their greater implantation precision and reduced radial force on the conduction system are associated with lower PPI rates. Registry data suggest PPI rates as low as 4–8% with newer-generation balloon-expandable valves, compared with 10–20% for self-expanding valves [4], supporting their use as a strategy to mitigate conduction-related complications in higher-risk patients.
4. Pharmacologic Strategies
- Corticosteroids: Corticosteroids were initially investigated for their potential to attenuate the post-TAVR inflammatory response and limit conduction tissue edema. Early reports were encouraging; however, subsequent larger studies failed to demonstrate a consistent reduction in PPI incidence, and concerns persist regarding systemic side effects and the lack of clear patient selection criteria [13,14,15].
- Colchicine: Colchicine, a well-established anti-inflammatory agent, is currently being evaluated in the Co-STAR trial (NCT04870424), a randomized, double-blind, placebo-controlled study. The trial aims to determine colchicine’s efficacy in preventing fibrosis-related conduction disorders and atrial arrhythmias after TAVR by dampening the inflammatory process. This trial is ongoing, with primary results expected in mid-2025. If successful, it could establish the first pharmacologic approach specifically designed to reduce post-procedural conduction disturbances.
5. Post-Procedural Monitoring
- Electrocardiographic and Electrophysiological Surveillance: Continuous ECG monitoring for up to 7 days is recommended by the ESC/EHRA guidelines, supported by evidence showing that more than 50% of high-grade atrioventricular block events occur within the first 72 h after TAVR, although a relevant proportion may still develop later during hospitalization. For this reason, ambulatory monitoring with external systems or implantable loop recorders may be extended up to 30 days in selected cases [16]. In addition, invasive electrophysiological study (EPS) may be considered from the third day after TAVR, particularly in patients with new-onset left bundle branch block (LBBB), PR interval > 240 ms, QRS duration > 150 ms, or marked prolongation (>20 ms) in those with pre-existing conduction disease. An HV interval ≥ 70 ms is widely regarded as predictive of high-grade atrioventricular (AV) block, although some studies have proposed alternative thresholds, such as HV ≥ 65 ms or a delta HV ≥ 13 ms when comparing pre- and post-procedural measurements [16,17]. Together, these strategies highlight the importance of combining extended non-invasive monitoring with targeted invasive evaluation to refine risk stratification and guide timely pacemaker implantation.
6. Telemonitoring and Early Discharge Programs
- TeleTAVI Study: Demonstrated that early discharge supported by structured telemonitoring using artificial intelligence (AI) is both feasible and safe. The study included stratified discharge timing—very early (<24 h), early (24–48 h), and standard (>48 h)—coupled with daily follow-up through a virtual voice assistant using natural language processing. Patients in the early discharge arms had comparable 30-day event rates to those discharged later, while reporting high adherence and satisfaction with monitoring [18].
- Additionally, several studies are focused on pre-, intra-, and post-TAVR electrocardiographic monitoring to validate the performance of conduction disturbance risk scales (NCT05657912), estimate a reduction in disturbances through notifications during the procedure (NCT05465655), and monitor patients with pre-existing conduction disturbances or those that develop intra- or peri-procedurally after discharge [19,20].
7. Preventive Pacemaker Implantation
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TAVR | Transcatheter Aortic Valve Implantation |
| PPI | Permanent Pacemaker Implantation |
| RBBB | Right Bundle Branch Block |
| LAFB | Left Anterior Fascicular Block |
| LBBB | Left Bundle Branch Block |
| EPS | Electrophysiological Study |
Appendix A
References
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef] [PubMed]
- Yu, Q.; Fu, Q.; Xia, Y.; Wu, Y. Predictors, clinical impact, and management strategies for conduction abnormalities after transcatheter aortic valve replacement: An updated review. Front. Cardiovasc. Med. 2024, 11, 1370244. [Google Scholar] [CrossRef]
- Hamdan, A.; Guetta, V.; Klempfner, R.; Konen, E.; Raanani, E.; Glikson, M.; Goitein, O.; Segev, A.; Barbash, I.; Fefer, P.; et al. Inverse relationship between membranous septal length and the risk of atrioventricular block in patients undergoing transcatheter aortic valve implantation. JACC Cardiovasc. Interv. 2015, 8, 1218–1228. [Google Scholar] [CrossRef]
- Novelli, L.; Jamie, G.; Regazzoli, D.; Reimers, B.; Frontera, A.; Mangieri, A. How to predict conduction disturbances after transcatheter aortic valve replacement. Kardiol. Pol. 2023, 81, 330–337. [Google Scholar] [CrossRef]
- Tang, G.H.L.; Zaid, S.; Michev, I.; Ahmad, H.; Kaple, R.; Undemir, C.; Cohen, M.; Lansman, S.L. “cusp-overlap” view simplifies fluoroscopy-guided implantation of self-expanding valve in transcatheter aortic valve replacement. JACC Cardiovasc. Interv. 2018, 11, 1663–1665. [Google Scholar] [CrossRef]
- Ben-Shoshan, J.; Alosaimi, H.; Lauzier, P.T.; Pighi, M.; Talmor-Barkan, Y.; Overtchouk, P.; Martucci, G.; Spaziano, M.; Finkelstein, A.; Gada, H.; et al. Double S-curve versus cusp-overlap technique. JACC Cardiovasc. Interv. 2021, 14, 185–194. [Google Scholar] [CrossRef]
- Rawish, E.; Macherey, S.; Jurczyk, D.; Pätz, T.; Jose, J.; Stiermaier, T.; Eitel, I.; Frerker, C.; Schmidt, T. Reduction of permanent pacemaker implantation by using the cusp overlap technique in transcatheter aortic valve replacement: A meta-analysis. Clin. Res. Cardiol. 2023, 112, 633–644. [Google Scholar] [CrossRef] [PubMed]
- Bouzas-Mosquera, A.; Barbeito-Caamaño, C.; Martínez-Sapiña, M.J.; Otero-Muinelo, S.; Vázquez-Rodríguez, J.M. Noninvasive imaging techniques in transcatheter aortic valve implantation. Cir. Cardiovasc. 2024, 32, 58–64. [Google Scholar] [CrossRef]
- Jørgensen, T.J.; Hansson, N.; De Backer, O.; Bieliauskas, G.; Terkelsen, C.T.; Wang, X.; Jensen, J.J.; Christiansen, E.C.; Piazza, N.; Svendsen, J.S.; et al. Membranous septum morphology and risk of conduction abnormalities after transcatheter aortic valve implantation. EuroIntervention 2022, 17, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Baraka, M.; Kamal, D.; Mostafa, A.E. Depth of implantation in relation to membranous septum as a predictor of conduction disturbances after transcatheter aortic valve implantation. Indian Pacing Electrophysiol. J. 2024, 24, 133–139. [Google Scholar] [CrossRef]
- Gabbieri, D.; Ghidoni, I.; Mascheroni, G.; Chiarabelli, M.; D’aNniballe, G.; Pisi, P.; Meli, M.; Labia, C.; Barbieri, A.; Spina, F.; et al. Pacemaker implantation after surgical aortic valve replacement and balloon-expandable transcatheter aortic valve implantation: Incidence, predictors and prognosis. Heart Rhythm O2 2025, 6, 259–272. [Google Scholar] [CrossRef] [PubMed]
- Nazif, T.M.; Dizon, J.M.; Hahn, R.T.; Xu, K.; Babaliaros, V.; Douglas, P.S.; El-Chami, M.F.; Herrmann, H.C.; Mack, M.; Makkar, R.R.; et al. Predictors and clinical outcomes of permanent pacemaker implantation after transcatheter aortic valve replacement: The PARTNER (Placement of AoRtic TraNscathetER Valves) trial and registry. JACC Cardiovasc. Interv. 2015, 8 Pt A, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Oestreich, B.; Gurevich, S.; Adabag, S.; Kelly, R.; Helmer, G.; Raveendran, G.; Yannopoulos, D.; Biring, T.; Garcia, S. Exposure to glucocorticoids prior to transcatheter aortic valve replacement is associated with reduced incidence of high-degree AV block and pacemaker. Cardiovasc. Revasc. Med. 2019, 20, 328–331. [Google Scholar] [CrossRef]
- Barone, L.; Muscoli, S.; Belli, M.; Di Luozzo, M.; Sergi, D.; Marchei, M.; Prandi, F.R.; Uccello, G.; Romeo, F.; Barillà, F. Effect of acute CORticosteroids on conduction defects after Transcatheter Aortic Valve Implantation: The CORTAVI study. J. Cardiovasc. Med. 2023, 24, 676–679. [Google Scholar] [CrossRef]
- Tiago, C.; Dias Vaz, M.; Marques, A.; Barata, M.; Braga, J.P.; Boa, A.; Carvalho, A.F. Intraoperative corticosteroids and pacemaker implantation after transcatheter aortic valve replacement. Cureus. 2024, 16, e56824. [Google Scholar] [CrossRef] [PubMed]
- Glikson, M.; Nielsen, J.C.; Kronborg, M.B.; Michowitz, Y.; Auricchio, A.; Barbash, I.M.; Barrabés, J.A.; Boriani, G.; Braunschweig, F.; Brignole, M.; et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: Developed by the Task Force on cardiac pacing and cardiac resynchronization therapy of the European Society of Cardiology (ESC) with the special contribution of the European Heart Rhythm Association (EHRA). Eur. Heart J. 2021, 42, 3427–3520. [Google Scholar] [CrossRef] [PubMed]
- Rivard, L.; Schram, G.; Asgar, A.; Khairy, P.; Andrade, J.G.; Bonan, R.; Dubuc, M.; Guerra, P.G.; Ibrahim, R.; Macle, L.; et al. Electrocardiographic and electrophysiological predictors of atrioventricular block after transcatheter aortic valve replacement. Heart Rhythm 2015, 12, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Herrero, M.; Samper, R.; Riquelme, J.; Pineda, J.; Bordes, P.; Torres-Mezcua, F.; Valencia, J.; Torres-Saura, F.; Manso, M.G.; Ajo, R.; et al. Early discharge programme after transcatheter aortic valve implantation based on close follow-up supported by telemonitoring using artificial intelligence: The TeleTAVI study. Eur. Heart J.-Digit. Health 2024, 6, ztae089. [Google Scholar] [CrossRef]
- Muntané-Carol, G.; Okoh, A.K.; Chen, C.; Nault, I.; Kassotis, J.; Mohammadi, S.; Coromilas, J.; Lee, L.Y.; Alperi, A.; Philippon, F.; et al. Ambulatory electrocardiographic monitoring following minimalist transcatheter aortic valve replacement. JACC Cardiovasc. Interv. 2021, 14, 2711–2722. [Google Scholar] [CrossRef]
- Scotti, A.; Sturla, M.; Coisne, A.; Assafin, M.; Chau, M.; Ho, E.C.; Granada, J.F.; Ferrick, K.J.; Di Biase, L.; Latib, A. Monitoring conduction disturbances following TAVR: Feasibility study of early discharge using a novel telemetry patch. Int. J. Cardiol. 2022, 364, 35–37. [Google Scholar] [CrossRef]
- Zorman, M.; Bamford, P.; Coronelli, M.; Barnes, C.; Saunderson, C.; Gamble, J.; Dawkins, S.; Kharbanda, R.K.; Newton, J.; Banning, A.P.; et al. Prophylactic permanent pacemaker implantation for baseline right bundle branch block in patients undergoing transcatheter aortic valve replacement: Clinical efficacy, safety, and long-term pacing requirement. Struct. Heart 2024, 8, 100326. [Google Scholar] [CrossRef] [PubMed]
- Fukutomi, M.; Hokken, T.; Wong, I.; Bieliauskas, G.; Daemen, J.; de Jaegere, P.; Van Mieghem, N.; Søndergaard, L.; De Backer, O. Prophylactic permanent pacemaker strategy in patients with right bundle branch block undergoing transcatheter aortic valve replacement. Catheter. Cardiovasc. Interv. 2021, 98, E1017–E1025. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reyes Mitre, A.; de la Garza, H.L.; Guerreiro, C.E.; Medina, D.O.; Avila Gil, E.M.; Salvadores, P.J.; Baz Alonso, J.A.; Romo, A.I.; Jimenez Diaz, V.A. Minimizing Permanent Pacemaker Implantation After TAVR: Current Strategies, Monitoring Pathways, and Future Directions. J. Clin. Med. 2025, 14, 7700. https://doi.org/10.3390/jcm14217700
Reyes Mitre A, de la Garza HL, Guerreiro CE, Medina DO, Avila Gil EM, Salvadores PJ, Baz Alonso JA, Romo AI, Jimenez Diaz VA. Minimizing Permanent Pacemaker Implantation After TAVR: Current Strategies, Monitoring Pathways, and Future Directions. Journal of Clinical Medicine. 2025; 14(21):7700. https://doi.org/10.3390/jcm14217700
Chicago/Turabian StyleReyes Mitre, Alfonso, Hector Lopez de la Garza, Claudio Espada Guerreiro, Dahyr Olivas Medina, Erick Marlon Avila Gil, Pablo Juan Salvadores, José Antonio Baz Alonso, Andres Iñiguez Romo, and Victor Alfonso Jimenez Diaz. 2025. "Minimizing Permanent Pacemaker Implantation After TAVR: Current Strategies, Monitoring Pathways, and Future Directions" Journal of Clinical Medicine 14, no. 21: 7700. https://doi.org/10.3390/jcm14217700
APA StyleReyes Mitre, A., de la Garza, H. L., Guerreiro, C. E., Medina, D. O., Avila Gil, E. M., Salvadores, P. J., Baz Alonso, J. A., Romo, A. I., & Jimenez Diaz, V. A. (2025). Minimizing Permanent Pacemaker Implantation After TAVR: Current Strategies, Monitoring Pathways, and Future Directions. Journal of Clinical Medicine, 14(21), 7700. https://doi.org/10.3390/jcm14217700





