Early Advanced Airway Management and Clinical Outcomes in Out-of-Hospital Cardiac Arrest: A Nationwide Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Data Sources
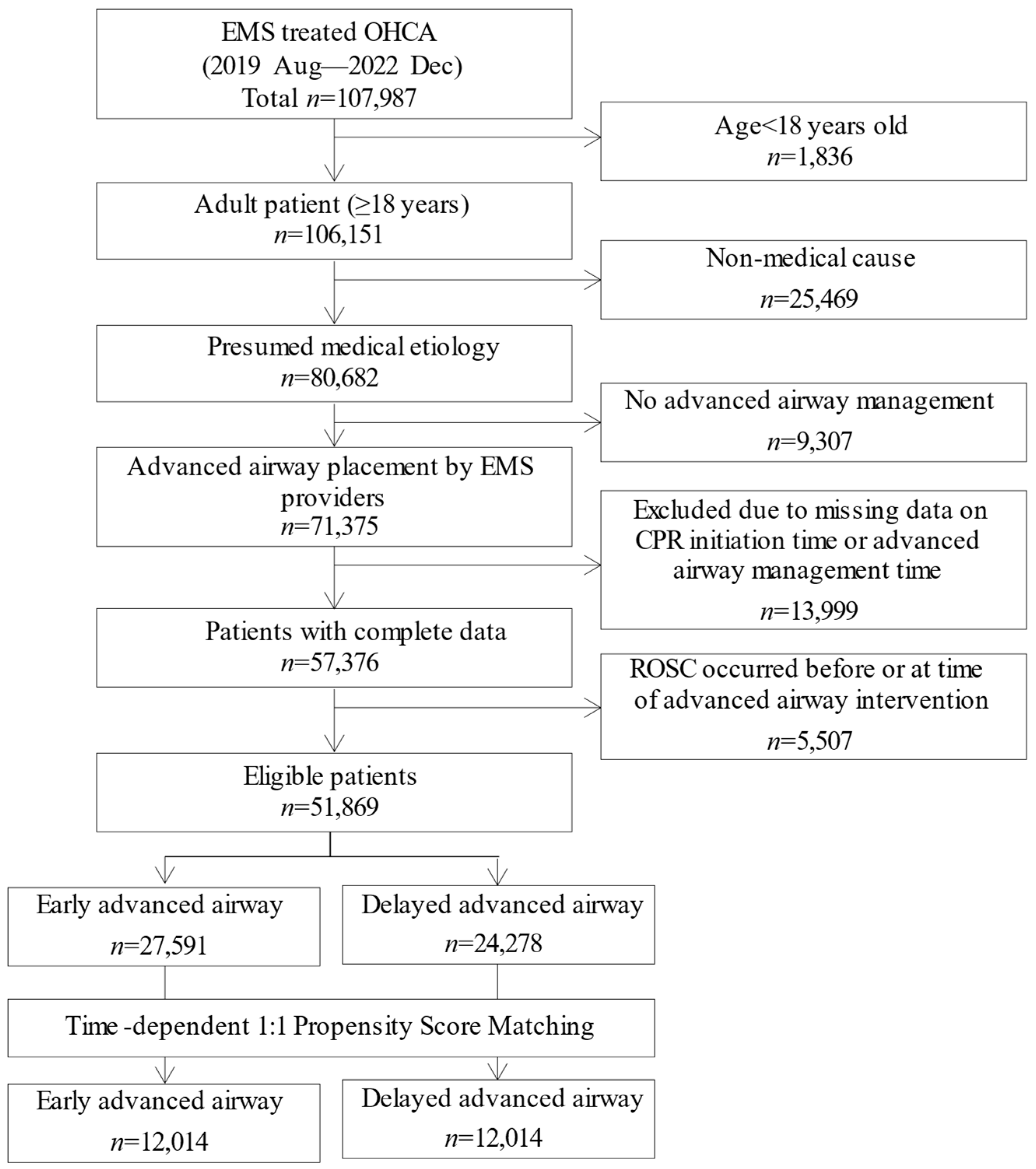
2.3. Study Population
2.4. Variables and Measurements
2.5. Outcomes
2.6. Statistical Analysis
3. Results
3.1. Patients
3.2. Baseline Characteristics in the Entire Cohort
3.3. Baseline Characteristics in the Matched Cohort
3.4. Clinical Outcomes
3.5. SEM Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| OHCA | Out-of-hospital cardiac arrest |
| EMS | Emergency medical services |
| AAM | Advanced airway management |
| CPR | Cardiopulmonary resuscitation |
| TTM | Targeted temperature management |
| PCI | Percutaneous coronary intervention |
| ECMO | Extracorporeal membrane oxygenation |
| ED | Emergency department |
| ROSC | Return of spontaneous circulation |
| CPC | Cerebral performance category |
| CI | Confidence interval |
| RR | Risk ratio |
| TDPSM | Time-dependent propensity score matching |
| SEM | Structural equation modeling |
| IV | Intravenous |
| IQR | Interquartile range |
| IRB | Institutional Review Board |
| SMD | Standardized mean difference |
| AHA | American Heart Association |
References
- Nishiyama, C.; Kiguchi, T.; Okubo, M.; Alihodžić, H.; Al-Araji, R.; Baldi, E.; Beganton, F.; Booth, S.; Bray, J.; Christensen, E.; et al. Three-year trends in out-of-hospital cardiac arrest across the world: Second report from the International Liaison Committee on Resuscitation (ILCOR). Resuscitation 2023, 186, 109757. [Google Scholar] [CrossRef] [PubMed]
- Perkins, G.D.; Graesner, J.T.; Semeraro, F.; Olasveengen, T.; Soar, J.; Lott, C.; Van de Voorde, P.; Madar, J.; Zideman, D.; Mentzelopoulos, S.; et al. European Resuscitation Council Guidelines 2021: Executive summary. Resuscitation 2021, 161, 1–60. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Lee, D.E.; Moon, S.; Ahn, J.Y.; Lee, W.K.; Kim, J.K.; Park, J.; Ryoo, H.W. Comparing the neurologic outcomes of patients with out-of-hospital cardiac arrest according to prehospital advanced airway management method and transport time interval. Clin. Exp. Emerg. Med. 2020, 7, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Newell, C.; Grier, S.; Soar, J. Airway and ventilation management during cardiopulmonary resuscitation and after successful resuscitation. Crit. Care 2018, 22, 190. [Google Scholar] [CrossRef]
- Merchant, R.M.; Topjian, A.A.; Panchal, A.R.; Cheng, A.; Aziz, K.; Berg, K.M.; Lavonas, E.J.; Magid, D.J. Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S337–S357. [Google Scholar] [CrossRef]
- Soar, J.; Böttiger, B.W.; Carli, P.; Couper, K.; Deakin, C.D.; Djärv, T.; Lott, C.; Olasveengen, T.; Paal, P.; Pellis, T.; et al. European Resuscitation Council Guidelines 2021: Adult advanced life support. Resuscitation 2021, 161, 115–151. [Google Scholar] [CrossRef]
- Kishihara, Y.; Amagasa, S.; Yasuda, H.; Kashiura, M.; Shinzato, Y.; Moriya, T. Evaluation of the optimal timing for advanced airway management for adult patients with out-of-hospital cardiac arrest: A retrospective observational study from a multicenter registry. Resusc. Plus 2025, 23, 100957. [Google Scholar] [CrossRef]
- Amagasa, S.; Iwamoto, S.; Kashiura, M.; Yasuda, H.; Kishihara, Y.; Uematsu, S. Early Versus Late Advanced Airway Management for Pediatric Patients with Out-of-Hospital Cardiac Arrest. Ann. Emerg. Med. 2024, 83, 185–195. [Google Scholar] [CrossRef]
- Benoit, J.L.; McMullan, J.T.; Wang, H.E.; Xie, C.; Xu, P.; Hart, K.W.; Stolz, U.; Lindsell, C.J. Timing of Advanced Airway Placement after Witnessed Out-of-Hospital Cardiac Arrest. Prehosp. Emerg. Care 2019, 23, 838–846. [Google Scholar] [CrossRef]
- Benoit, J.L.; Prince, D.K.; Wang, H.E. Mechanisms linking advanced airway management and cardiac arrest outcomes. Resuscitation 2015, 93, 124–127. [Google Scholar] [CrossRef]
- Jarman, A.F.; Hopkins, C.L.; Hansen, J.N.; Brown, J.R.; Burk, C.; Youngquist, S.T. Advanced Airway Type and Its Association with Chest Compression Interruptions During Out-of-Hospital Cardiac Arrest Resuscitation Attempts. Prehosp Emerg. Care 2017, 21, 628–635. [Google Scholar] [CrossRef]
- Park, J.H.; Song, K.J.; Shin, S.D. The prehospital emergency medical service system in Korea: Its current status and future direction. Clin. Exp. Emerg. Med. 2023, 10, 251–254. [Google Scholar] [CrossRef]
- Otto, Q.; Nolan, J.P.; Chamberlain, D.A.; Cummins, R.O.; Soar, J. Utstein Style for emergency care—The first 30 years. Resuscitation 2021, 163, 16–25. [Google Scholar] [CrossRef]
- Park, J.H.; Choi, Y.; Ro, Y.S.; Song, K.J.; Shin, S.D. Establishing the Korean Out-of-Hospital cardiac arrest registry (KOHCAR). Resusc. Plus 2024, 17, 100529. [Google Scholar] [CrossRef]
- Becker, L.B.; Aufderheide, T.P.; Geocadin, R.G.; Callaway, C.W.; Lazar, R.M.; Donnino, M.W.; Nadkarni, V.M.; Abella, B.S.; Adrie, C.; Berg, R.A.; et al. Primary outcomes for resuscitation science studies: A consensus statement from the American Heart Association. Circulation 2011, 124, 2158–2177. [Google Scholar] [CrossRef]
- Lu, B. Propensity score matching with time-dependent covariates. Biometrics 2005, 61, 721–728. [Google Scholar] [CrossRef]
- Zhang, Z.; Li, X.; Wu, X.; Qiu, H.; Shi, H. Propensity score analysis for time-dependent exposure. Ann. Transl. Med. 2020, 8, 246. [Google Scholar] [CrossRef] [PubMed]
- Stuart, E.A.; Lee, B.K.; Leacy, F.P. Prognostic score-based balance measures can be a useful diagnostic for propensity score methods in comparative effectiveness research. J. Clin. Epidemiol. 2013, 66, S84–S90.e81. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z. Structural equation modeling in the context of clinical research. Ann. Transl. Med. 2017, 5, 102. [Google Scholar] [CrossRef] [PubMed]
- Neth, M.R.; Idris, A.; McMullan, J.; Benoit, J.L.; Daya, M.R. A review of ventilation in adult out-of-hospital cardiac arrest. J. Am. Coll. Emerg. Physicians Open 2020, 1, 190–201. [Google Scholar] [CrossRef]
- Choi, Y.; Kim, T.H.; Hong, K.J.; Song, K.J.; Shin, S.D. Association between prehospital airway management methods and neurologic outcome in out-of-hospital cardiac arrest with respiratory cause: A nationwide retrospective observational study. Signa Vitae 2022, 18, 34–40. [Google Scholar] [CrossRef]
- Andersen, L.W.; Granfeldt, A.; Callaway, C.W.; Bradley, S.M.; Soar, J.; Nolan, J.P.; Kurth, T.; Donnino, M.W. Association Between Tracheal Intubation During Adult In-Hospital Cardiac Arrest and Survival. JAMA 2017, 317, 494–506. [Google Scholar] [CrossRef]
- Okubo, M.; Komukai, S.; Izawa, J.; Aufderheide, T.P.; Benoit, J.L.; Carlson, J.N.; Daya, M.R.; Hansen, M.; Idris, A.H.; Le, N.; et al. Association of Advanced Airway Insertion Timing and Outcomes After Out-of-Hospital Cardiac Arrest. Ann. Emerg. Med. 2022, 79, 118–131. [Google Scholar] [CrossRef]
- Lee, S.H.; Ryoo, H.W. Outcomes in patients with out-of-hospital cardiac arrest according to prehospital advanced airway management timing: A retrospective observational study. J. Yeungnam Med. Sci. 2024, 41, 288–295. [Google Scholar] [CrossRef]
- Onoe, A.; Kajino, K.; Daya, M.R.; Nakamura, F.; Nakajima, M.; Kishimoto, M.; Sakuramoto, K.; Muroya, T.; Ikegawa, H.; Hock Ong, M.E.; et al. Improved neurologically favorable survival after OHCA is associated with increased pre-hospital advanced airway management at the prefecture level in Japan. Sci. Rep. 2022, 12, 20498. [Google Scholar] [CrossRef] [PubMed]
- Kajino, K.; Iwami, T.; Kitamura, T.; Daya, M.; Ong, M.E.; Nishiuchi, T.; Hayashi, Y.; Sakai, T.; Shimazu, T.; Hiraide, A.; et al. Comparison of supraglottic airway versus endotracheal intubation for the pre-hospital treatment of out-of-hospital cardiac arrest. Crit. Care 2011, 15, R236. [Google Scholar] [CrossRef] [PubMed]
| Early Advanced Airway | Delayed Advanced Airway | SMD | |
|---|---|---|---|
| n = 27,591 | n = 24,278 | ||
| Demographic characteristics | |||
| Age, years | 72.6 | 72 | 0.042 |
| Female, n (%) | 10,122 (36.7) | 9146 (37.7) | 0.02 |
| Diabetes, n (%) | 7374 (26.7) | 6731 (27.7) | 0.022 |
| Hypertension, n (%) | 10,691 (38.7) | 9705 (40.0) | 0.025 |
| Stroke, n (%) | 2539 (9.2) | 2363 (9.7) | 0.018 |
| Heart disease, n (%) | 5432 (19.7) | 4831 (19.9) | 0.005 |
| Arrest characteristics | |||
| Year of arrest | 0.075 | ||
| 2019, n (%) | 970 (3.5) | 583 (2.4) | |
| 2020, n (%) | 8219 (29.8) | 7716 (31.8) | |
| 2021, n (%) | 9117 (33.0) | 7969 (32.8) | |
| 2022, n (%) | 9285 (33.7) | 8010 (33.0) | |
| Urbanization level of arrest location | 0.074 | ||
| Metropolitan, n (%) | 14,191 (51.4) | 13,276 (54.7) | |
| Urban, n (%) | 3694 (13.4) | 3280 (13.5) | |
| Rural, n (%) | 9706 (35.2) | 7722 (31.8) | |
| Public place, n (%) | 5010 (18.2) | 3356 (13.8) | 0.118 |
| Witnessed, n (%) | 11,342 (46.7) | 12,258 (44.4) | 0.046 |
| Bystander CPR, n (%) | 19,068 (69.1) | 13,614 (56.1) | 0.272 |
| EMS characteristics | |||
| Multi-tier response, n (%) | 23,945 (86.8) | 20,636 (85.0) | 0.051 |
| Response time, min [IQR] | 9.0 [7.0, 12.0] | 8.0 [6.0, 11.0] | 0.155 |
| Scene time, min [IQR] | 14.0 [11.0, 17.0] | 16.0 [13.0, 19.0] | 0.453 |
| Transport time, min [IQR] | 8.0 [6.0, 11.0] | 8.0 [6.0, 10.0] | 0.062 |
| Advanced airway management type | 0.166 | ||
| Supraglottic airway, n (%) | 26,577 (96.3) | 22,465 (92.5) | |
| Endotracheal intubation, n (%) | 1014 (3.7) | 1813 (7.5) | |
| IV line insertion, n (%) | 18,472 (66.9) | 16,403 (67.6) | 0.013 |
| Prehospital epinephrine, n (%) | 6167 (22.4) | 5998 (24.7) | 0.056 |
| Initial shockable rhythm, n (%) | 4246 (15.8) | 2837 (11.7) | 0.108 |
| Prehospital intervention characteristics (time to prehospital interventions from EMS-initiated CPR) [min] | |||
| Advanced airway, median [IQR] | 3.0 [2.0, 4.0] | 7.0 [5.0, 9.0] | 1.545 |
| Rhythm analysis, median [IQR] | 0.0 [0.0, 1.0] | 1.0 [0.0, 1.0] | 0.257 |
| First defibrillation, median [IQR] | 1.0 [1.0, 4.0] | 2.0 [1.0, 5.0] | 0.128 |
| IV line insertion, median [IQR] | 5.0 [3.0, 7.0] | 8.0 [6.0, 10.0] | 0.899 |
| Epinephrine administration, median [IQR] | 8.0 [6.0, 11.0] | 10.0 [8.0, 13.0] | 0.497 |
| ED level | |||
| Level 1, n (%) | 6507 (23.6) | 6270 (25.8) | 0.108 |
| Level 2, n (%) | 12,620 (45.7) | 11,727 (48.3) | |
| Level 3, n (%) | 8464 (30.7) | 6281 (25.9) | |
| Hospital management | |||
| Reperfusion, n (%) | 1930 (7.0) | 1148 (4.7) | 0.097 |
| Targeted temperature management, n (%) | 1026 (3.7) | 832 (3.4) | 0.016 |
| ECMO, n (%) | 344 (1.2) | 310 (1.3) | 0.003 |
| Early Advanced Airway | Delayed Advanced Airway | SMD | |
|---|---|---|---|
| n = 12,014 | n = 12,014 | ||
| Demographic characteristics | |||
| Age, years | 72.2 | 71.6 | 0.038 |
| Female, n (%) | 4414 (36.7) | 4414 (36.7) | 0.003 |
| Diabetes, n (%) | 3301 (27.5) | 3145 (26.2) | 0.029 |
| Hypertension, n (%) | 4627 (38.5) | 4627 (38.5) | 0.024 |
| Stroke, n (%) | 1124 (9.4) | 1102 (9.2) | 0.006 |
| Heart disease, n (%) | 2386 (19.9) | 2386 (19.9) | 0.012 |
| Arrest characteristics | |||
| Year of arrest | <0.001 | ||
| 2019, n (%) | 356 (3.0) | 356 (3.0) | |
| 2020, n (%) | 3998 (33.3) | 3998 (33.3) | |
| 2021, n (%) | 4248 (35.4) | 4248 (35.4) | |
| 2022, n (%) | 3412 (28.4) | 3412 (28.4) | |
| Arrest location urbanization level | 0.096 | ||
| Metropolitan, n (%) | 6015 (50.1) | 6592 (54.9) | |
| Urban, n (%) | 4352 (36.2) | 3940 (32.8) | |
| Rural, n (%) | 1647 (13.7) | 1482 (12.3) | |
| Public location, n (%) | 2461 (20.5) | 1931 (16.1) | 0.114 |
| Witnessed arrest, n (%) | 5451 (45.4) | 5675 (47.2) | 0.037 |
| Bystander CPR, n (%) | 8321 (69.3) | 8321 (69.3) | <0.001 |
| EMS characteristics | |||
| Multi-tier response, n (%) | 10166 (84.6) | 10499 (87.4) | 0.080 |
| Response time, min [IQR] | 8.0 [6.0, 11.0] | 8.0 [6.0, 11.0] | 0.015 |
| Scene time, min [IQR] | 14.0 [12.0, 17.0] | 15.0 [12.0, 18.0] | 0.184 |
| Transport time, min [IQR] | 7.0 [4.0, 11.0] | 7.0 [5.0, 11.0] | 0.006 |
| Advanced airway type, n (%) | 0.086 | ||
| Supraglottic airway, n (%) | 11,679 (96.9) | 11,361 (95.2) | |
| Endotracheal intubation, n (%) | 374 (3.1) | 576 (4.8) | |
| IV-line insertion, n (%) | 7637 (63.6) | 8119 (67.6) | 0.085 |
| Prehospital epinephrine, n (%) | 2236 (18.6) | 2580 (21.5) | 0.072 |
| Initial shockable rhythm, n (%) | 1968 (16.4) | 2837 (16.4) | <0.001 |
| Prehospital intervention characteristics (time from EMS-initiated CPR) [min] | |||
| Advanced airway, median [IQR] | 3.0 [2.0, 4.0] | 8.0 [6.0, 9.0] | 1.902 |
| Rhythm analysis, median [IQR] | 0.0 [0.0, 1.0] | 1.0 [0.0, 1.0] | 0.212 |
| First defibrillation, median [IQR] | 1.0 [1.0, 3.0] | 2.0 [1.0, 4.0] | 0.061 |
| IV-line insertion, median * [IQR] | 4.0 [3.0, 7.0] | 6.0 [4.0, 9.0] | 0.488 |
| Epinephrine administration, median * [IQR] | 8.0 [6.0, 11.0] | 10.0 [7.0, 12.0] | 0.280 |
| ED level | 0.113 | ||
| Level 1, n (%) | 2735 (22.8) | 3053 (25.4) | |
| Level 2, n (%) | 5443 (45.3) | 5732 (47.7) | |
| Level 3, n (%) | 3836 (31.9) | 3229 (26.9) | |
| Hospital management | |||
| Reperfusion, n (%) | 906 (7.5) | 906 (7.5) | <0.001 |
| Targeted temperature management, n (%) | 470 (3.9) | 470 (3.9) | <0.001 |
| ECMO, n (%) | 155 (1.3) | 194 (1.6) | 0.027 |
| n/N (%) | Risk Ratio (95% CI) | ||
|---|---|---|---|
| Unadjusted | Adjusted * | ||
| Prehospital ROSC | |||
| Delayed advanced airway | 1258/12,014 (10.5%) | Reference | Reference |
| Early advanced airway | 1414/12,014 (11.8%) | 1.13 (1.05–1.21) | 1.21 (1.12–1.29) |
| Survival to discharge | |||
| Delayed advanced airway | 929/12,014 (7.7%) | Reference | Reference |
| Early advanced airway | 1016/12,014 (8.5%) | 1.10 (1.01–1.20) | 1.08 (1.00–1.17) |
| Good neurological recovery | |||
| Delayed advanced airway | 614/12,014 (5.1%) | Reference | Reference |
| Early advanced airway | 699/12,014 (5.8%) | 1.14 (1.03–1.27) | 1.12 (1.01–1.23) |
| Variable | Advanced Airway Only (n = 16,239) | Advanced Airway + Epinephrine (n = 3859) | Advanced Airway + Defibrillation (n = 2979) | Advanced Airway + Epinephrine + Defibrillation (n = 957) |
|---|---|---|---|---|
| Initial rhythm analysis delay (min) | 0.611 (<0.05) | 0.515(<0.05) | 0.643 (<0.05) | 0.539 (<0.05) |
| Epinephrine administration delay (min) | - | 0.244 (<0.05) | - | 0.202 (<0.05) |
| Defibrillation delay (min) | - | - | 0.228 (<0.05) | −0.039 (0.33) |
| Endotracheal intubation | 0.865 (<0.05) | 2.254 (<0.05) | 1.427 (<0.05) | 1.442 (<0.05) |
| Metropolitan | 0.043 (0.33) | 0.326 (<0.05) | 0.045 (0.65) | 0.395 (<0.05) |
| Public place | −0.03 (0.64) | −0.216 (0.08) | −0.003 (0.97) | −0.114 (0.52) |
| Multi-tier EMS response | 0.259 (<0.05) | 0.107 (0.60) | 0.095 (0.49) | 0.043(0.92) |
| Witnessed arrest | −0.023 (0.59) | −0.202 (0.13) | −0.064 (0.55) | −0.079 (0.67) |
| Bystander CPR | 0.016 (0.73) | 0.008 (0.94) | −0.112 (0.36) | 0.156 (0.47) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.H.; Lee, D.; Jung, E.; Ryu, H.H.; Park, J.H.; Ro, Y.S.; Song, K.J. Early Advanced Airway Management and Clinical Outcomes in Out-of-Hospital Cardiac Arrest: A Nationwide Observational Study. J. Clin. Med. 2025, 14, 7652. https://doi.org/10.3390/jcm14217652
Lee JH, Lee D, Jung E, Ryu HH, Park JH, Ro YS, Song KJ. Early Advanced Airway Management and Clinical Outcomes in Out-of-Hospital Cardiac Arrest: A Nationwide Observational Study. Journal of Clinical Medicine. 2025; 14(21):7652. https://doi.org/10.3390/jcm14217652
Chicago/Turabian StyleLee, Jung Ho, Dahae Lee, Eujene Jung, Hyun Ho Ryu, Jeong Ho Park, Young Sun Ro, and Kyoung Jun Song. 2025. "Early Advanced Airway Management and Clinical Outcomes in Out-of-Hospital Cardiac Arrest: A Nationwide Observational Study" Journal of Clinical Medicine 14, no. 21: 7652. https://doi.org/10.3390/jcm14217652
APA StyleLee, J. H., Lee, D., Jung, E., Ryu, H. H., Park, J. H., Ro, Y. S., & Song, K. J. (2025). Early Advanced Airway Management and Clinical Outcomes in Out-of-Hospital Cardiac Arrest: A Nationwide Observational Study. Journal of Clinical Medicine, 14(21), 7652. https://doi.org/10.3390/jcm14217652







