Echocardiographic Hemodynamics After Aortic Valve Replacement, Wheat, and Bentall Procedure
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Statement
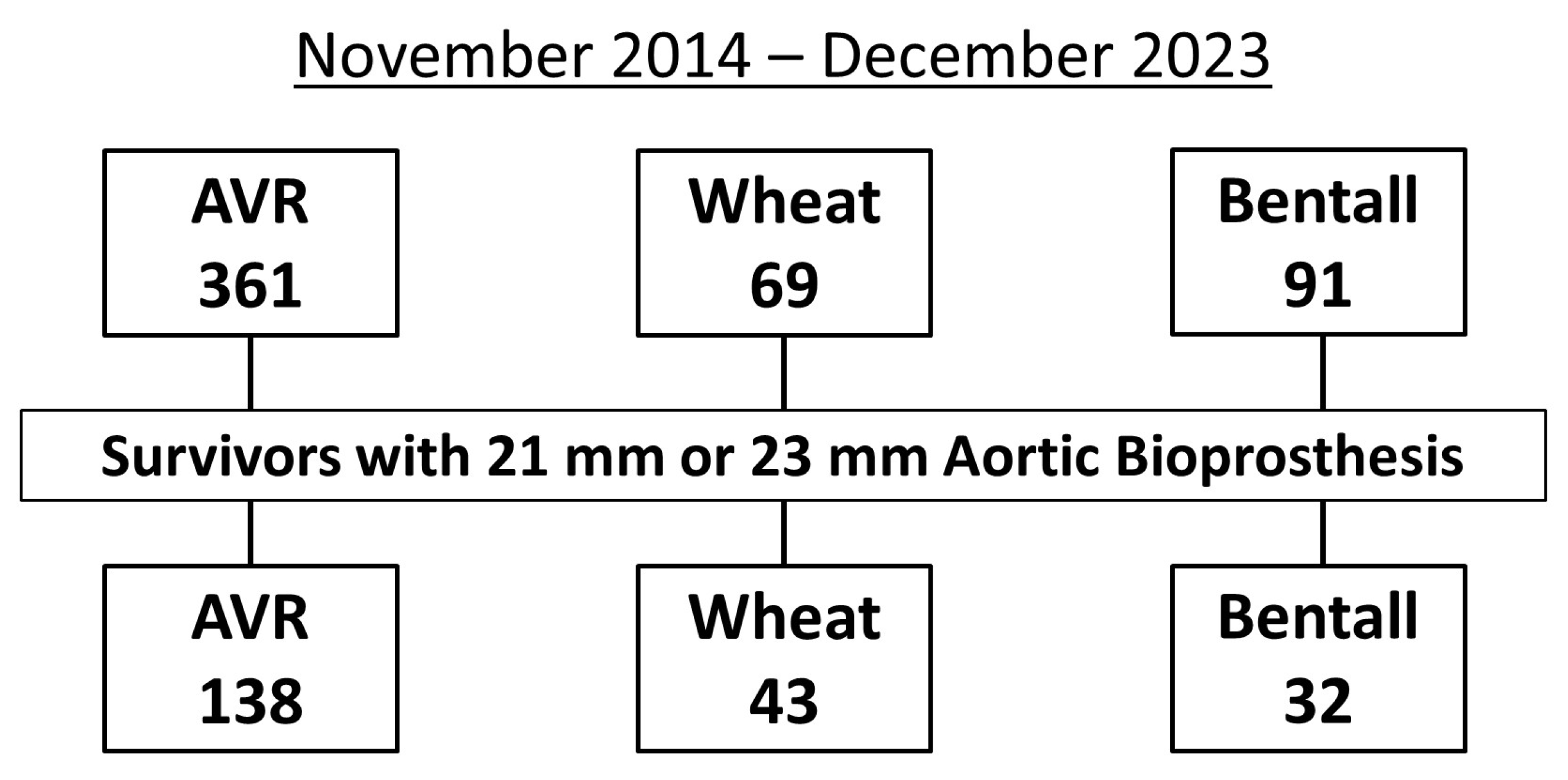
2.2. Study Patients
2.3. Echocardiography
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Operative Data
3.3. Echocardiographic Data
3.4. Propensity Score-Matched Comparisons
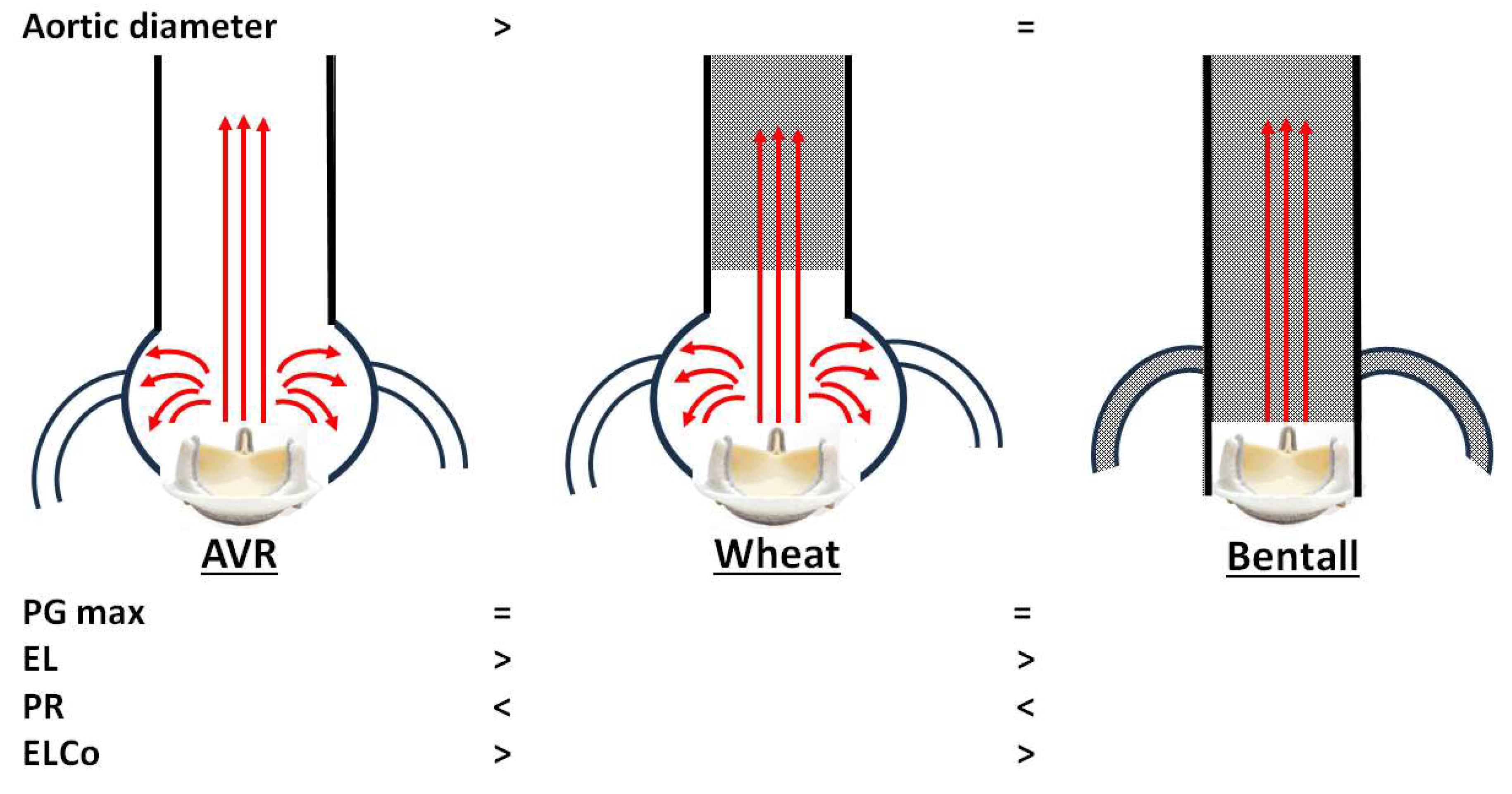
4. Discussion
- 1.
- Unexpectedly, overestimation of PG max was not observed in either the Wheat or Bentall groups, despite replacement of the ascending aorta with a smaller vascular graft.
- 2.
- In the AVR group, a smaller Ad was associated with a higher PG max after AVR. Patients with PG max > 30 mmHg had a significantly smaller Ad than those with PG max ≤ 30 mmHg.
- 3.
- Both the Wheat and Bentall groups demonstrated higher PR and lower EL values compared with the AVR group.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abbas, A.E.; Mando, R.; Hanzel, G.; Goldstein, J.; Shannon, F.; Pibarot, P. Hemodynamic principles of prosthetic aortic valve evaluation in the transcatheter aortic valve replacement era. Echocardiography 2020, 37, 738–757. [Google Scholar] [CrossRef]
- Bach, D.S.; Schmitz, C.; Dohmen, G.; Aaronson, K.D.; Steinseifer, U.; Kleine, P. In vitro assessment of prosthesis type and pressure recovery characteristics: Doppler echocardiography overestimation of bileaflet mechanical and bioprosthetic aortic valve gradients. J. Thorac. Cardiovasc. Surg. 2012, 144, 453–458. [Google Scholar] [CrossRef]
- Baumgartner, H.; Schima, H.; Kühn, P. Discrepancies between Doppler and catheter gradients across bileaflet aortic valve prostheses. Am. J. Cardiol. 1993, 71, 1241–1243. [Google Scholar] [CrossRef]
- Garcia, D.; Dumesnil, J.G.; Durand, L.G.; Kadem, L.; Pibarot, P. Discrepancies between catheter and Doppler estimates of valve effective orifice area can be predicted from the pressure recovery phenomenon: Practical implications with regard to quantification of aortic stenosis severity. J. Am. Coll. Cardiol. 2003, 41, 435–442. [Google Scholar] [CrossRef]
- Midha, P.A.; Raghav, V.; Sharma, R.; Condado, J.F.; Okafor, I.U.; Rami, T.; Kumar, G.; Thourani, V.H.; Jilaihawi, H.; Babaliaros, V.; et al. The Fluid Mechanics of Transcatheter Heart Valve Leaflet Thrombosis in the Neosinus. Circulation 2017, 136, 1598–1609. [Google Scholar] [CrossRef]
- Reddy, Y.N.V.; Miranda, W.R.; Nishimura, R.A. Measuring pressure gradients after transcatheter aortic valve implantation: Rethinking the Bernoulli principle. J. Am. Heart Assoc. 2021, 10, e022515. [Google Scholar] [CrossRef]
- Svensson, L.G. Approach for insertion of aortic composite valve grafts. Ann. Thorac. Surg. 1992, 54, 376–378. [Google Scholar] [CrossRef]
- Pibarot, P.; Salaun, E.; Dahou, A.; Avenatti, E.; Guzzetti, E.; Annabi, M.S.; Toubal, O.; Bernier, M.; Beaudoin, J.; Ong, G.; et al. PARTNER 3 Investigators. PARTNER 3 investigators. echocardiographic results of transcatheter versus surgical aortic valve replacement in low-risk patients: The PARTNER 3 Trial. Circulation 2020, 141, 1527–1537. [Google Scholar] [CrossRef] [PubMed]
- Voelker, W.; Reul, H.; Stelzer, T.; Schmidt, A.; Karsch, K.R. Pressure recovery in aortic stenosis: An in vitro study in a pulsatile flow model. J. Am. Coll. Cardiol. 1992, 20, 1585–1593. [Google Scholar] [CrossRef] [PubMed]
- Garcia, D.; Pibarot, P.; Dumesnil, J.G.; Sakr, F.; Durand, L.G. Assessment of aortic valve stenosis severity: A new index based on the energy loss concept. Circulation 2000, 101, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Reil, J.C.; Marquetand, C.; Busch-Tilge, C.; Ivannikova, M.; Rudolph, V.; Aboud, A.; Ensminger, S.; Schäfers, H.J.; Stierle, U.; Reil, G.H. Functional interaction of aortic valve and ascending aorta in patients after valve-sparing procedures. Sci. Rep. 2023, 13, 15340. [Google Scholar] [CrossRef]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013, 48, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Bahlmann, E.; Cramariuc, D.; Gerdts, E.; Gohlke-Baerwolf, C.; Nienaber, C.A.; Eriksen, E.; Wachtell, K.; Chambers, J.; Kuck, K.H.; Ray, S. Impact of pressure recovery on echocardiographic assessment of asymptomatic aortic stenosis: A SEAS substudy. JACC Cardiovasc. Imaging 2010, 3, 555–562. [Google Scholar] [CrossRef]
- Heinrich, R.S.; Fontaine, A.A.; Grimes, R.Y.; Sidhaye, A.; Yang, S.; Moore, K.E.; Levine, R.A.; Yoganathan, A.P. Experimental analysis of fluid mechanical energy losses in aortic valve stenosis: Importance of pressure recovery. Ann. Biomed. Eng. 1996, 24, 685–694. [Google Scholar] [CrossRef]
- Singh, G.K.; Mowers, K.L.; Marino, C.; Balzer, D.; Rao, P.S. Effect of pressure recovery on pressure gradients in congenital stenotic outflow lesions in pediatric patients-clinical implications of lesion severity and geometry: A Simultaneous Doppler Echocardiography and Cardiac Catheter Correlative Study. J. Am. Soc. Echocardiogr. 2020, 33, 207–217. [Google Scholar] [CrossRef]
- Hatoum, H.; Hahn, R.T.; Lilly, S.; Dasi, L.P. Differences in pressure recovery between balloon expandable and self-expandable transcatheter aortic valves. Ann. Biomed. Eng. 2020, 48, 860–867. [Google Scholar] [CrossRef]
- Abbas, A.E.; Mando, R.; Kadri, A.; Khalili, H.; Hanzel, G.; Shannon, F.; Al-Azizi, K.; Waggoner, T.; Kassas, S.; Pilgrim, T.; et al. Comparison of transvalvular aortic mean gradients obtained by intraprocedural echocardiography and invasive measurement in balloon and self-expanding transcatheter valves. J. Am. Heart Assoc. 2021, 10, e021014. [Google Scholar] [CrossRef] [PubMed]
- Samaee, M.; Hatoum, H.; Biersmith, M.; Yeats, B.; Gooden, S.C.; Thourani, V.H.; Hahn, R.T.; Lilly, S.; Yoganathan, A.; Dasi, L.P. Gradient and pressure recovery of a self-expandable transcatheter aortic valve depends on ascending aorta size: In vitro study. JTCVS Open 2022, 9, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Morota, T.; Takamoto, S. Development and physical characteristics of novel zero-porosity vascular graft “triplex(®)”. Ann. Vasc. Dis. 2013, 6, 67–73. [Google Scholar] [CrossRef]
- Narita, M.; Shirasaka, T.; Ushioda, R.; Kamiya, H. Triplex vascular prostheses elongation in post-operative course. J. Surg. Case Rep. 2022, 6, rjac255. [Google Scholar] [CrossRef]
- Etz, C.D.; Homann, T.; Silovitz, D.; Bodian, C.A.; Luehr, M.; Di Luozzo, G.; Plestis, K.A.; Griepp, R.B. Vascular graft replacement of the ascending and descending aorta: Do Dacron grafts grow? Ann. Thorac. Surg. 2007, 84, 1206–1212. [Google Scholar] [CrossRef] [PubMed]
- Nazer, R.I.; Alhothali, A.; Albarrati, A. In vitro modeling of crimped Dacron vascular grafts for aortic root replacement. Am. J. Cardiovasc. Dis. 2023, 13, 59–67. [Google Scholar] [PubMed]
- Johal, G.; Jonnala, V.; Pourafkari, L.; Sedghi, S.; Jafarsis, S.; Fernandez, S.; Iyer, V.; Nader, N.D. Energy loss index as a predictor of all-cause mortality after transcatheter aortic valve replacement: A long-term follow-up. Echocardiography 2023, 40, 327–334. [Google Scholar] [CrossRef] [PubMed]

| Variables | AVR (n = 138) | Wheat (n = 43) | Bentall (n = 32) | p Value |
|---|---|---|---|---|
| Age, years | 74 ± 6 | 74 ± 8 | 71 ± 7 | <0.001 |
| Male gender, n (%) | 101 (73) | 31 (72) | 24 (75) | 0.87 |
| Height, cm | 161 ± 8 | 163 ± 9 | 163 ±8 | 0.89 |
| Weight, kg | 60 ± 11 | 60 ± 11 | 61 ± 12 | 0.84 |
| Hypertension, n (%) | 109 (78) | 32 (74) | 25 (78) | 0.65 |
| Hyperlipidemia, n (%) | 75 (54) | 21 (49) | 15 (47) | 0.23 |
| Diabetes mellitus, n (%) | 32 (23) | 7 (16) | 6 (19) | 0.02 |
| Previous stroke, n (%) | 14 (10) | 2 (5) | 3 (9) | 0.68 |
| Lung disease, n (%) | 32 (23) | 8 (19) | 6 (19) | 0.67 |
| Smoking habit, n (%) | 68 (49) | 20 (47) | 15 (47) | 0.79 |
| Liver disease, n (%) | 5 (4) | 1 (2) | 0 | 0.15 |
| Chronic kidney disease, n (%) | 62 (45) | 16 (37) | 13 (41) | 0.32 |
| Peripheral artery disease, n (%) | 10 (7) | 1 (2) | 0 | 0.25 |
| Atrial fibrillation, n (%) | 28 (20) | 4 (9) | 1 (3) | <0.001 |
| CTR on X-ray, % | 54 ± 7 | 53 ± 8 | 55 ± 7 | 0.71 |
| Variables | AVR (n = 138) | Wheat (n = 43) | Bentall (n = 32) | p Value |
|---|---|---|---|---|
| Urgency or emergency | 4 (3) | 1 (2) | 2 (6) | 0.82 |
| Redo surgery | 2 (1) | 2 (5) | 2 (6) | 0.66 |
| Primary disease of aortic valve | ||||
| Aortic valve stenosis | 81 (57) | 27 (62) | 4 (13) | <0.001 |
| Aortic valve regurgitation | 57 (43) | 16 (38) | 28 (87) | |
| Bicuspid aortic valve | 36 (26) | 14 (33) | 9 (28) | 0.71 |
| Isolated AVR | 50 (36) | 0 | 0 | - |
| Concomitant procedures | 88 (64) | |||
| MVR | 12 (9) | 1 (2) | 2 (6) | 0.24 |
| MVP | 17 (12) | 1 (2) | 3 (9) | 0.18 |
| CABG | 41 (28) | 10 (23) | 11 (34) | 0.29 |
| Operation, min | 363 ± 85 | 438 ± 131 | 528 ± 104 | <0.001 |
| Cardiopulmonary bypass, min | 185 ± 50 | 222 ± 55 | 297 ± 66 | <0.001 |
| Cardiac ischemia, min | 127 ± 36 | 160 ± 35 | 222 ± 46 | <0.001 |
| Lowest body temperature, °C | 31 ±2 | 25±3 | 25±4 | <0.001 |
| Circulatory arrest, n (%) | 4 (3) | 34 (79) | 16 (50) | <0.001 |
| AVR bioprosthesis | 0.37 | |||
| Avalus | 27 (63) | 22 (69) | ||
| Magna ease | 36 (26) | 5 (12) | 5 (16) | |
| Inspiris | 26 (19) | 6 (14) | 2 (6) | |
| Mosaic | 2 (1.5) | 3 (7) | 3 (9) | |
| Epic | 2 (1.5) | 2 (5) | ||
| AVR size | 0.54 | |||
| 21 mm | 79 (57) | 23 (53) | 12 (38) | |
| 23 mm | 59 (43) | 20 (47) | 20 (62) | |
| Vascular prosthesis | 0.94 | |||
| Triplex | 42 (98) | 32 (100) | ||
| J Graft | 1 (2) | |||
| Vascular prosthesis size | 0.24 | |||
| 22 mm | 1 (2) | |||
| 24 mm | 8 (19) | 7 (22) | ||
| 26 mm | 12 (28) | 18 (56) | ||
| 28 mm | 17 (40) | 7 (22) | ||
| 30 mm | 4 (9) | |||
| 32 mm | 1 (2) | |||
| Variables | AVR (n = 138) | Wheat (n = 43) | Bentall (n = 32) | p Value |
|---|---|---|---|---|
| Preoperative | ||||
| LVDd, mm | 45 ± 7 | 47 ± 7 | 48 ±10 | 0.32 |
| LVDs, mm | 32 ± 9 | 31 ± 8 | 36 ± 12 | 0.12 |
| LVEF, % | 55 ± 10 | 56 ± 9 | 50 ± 11 | 0.02 |
| LVMI, g/m2 | 109 ± 33 | 102 ± 27 | 121 ± 56 | 0.42 |
| RWT | 0.49 ± 0.10 | 0.50 ± 0.07 | 0.50 ± 0.08 | 0.72 |
| Postoperative | ||||
| Aorta area, mm2 | 1074 ± 236 | 746 ± 184 | 696 ± 106 | <0.01 |
| Aorta diameter, mm | 36.7 ± 4.4 | 30.6 ± 3.4 | 29.7 ± 2.3 | <0.01 |
| PG max, mmHg | 23.3 ± 7.1 | 21.6 ± 7.7 | 17.8 ± 83 | <0.01 |
| EOA, cm2 | 1.38 ± 0.25 | 1.38 ± 0.26 | 1.46 ± 0.30 | 0.643 |
| PR, mmHg | 5.20 ± 1.75 | 5.75 ± 2.96 | 6.47 ± 2.19 | 0.034 |
| PRI | 0.23 ± 0.06 | 0.31 ± 0.06 | 0.34 ± 0.06 | 0.034 |
| EL, mmHg | 17.5 ± 5.9 | 14.5 ± 6.4 | 10.7 ± 5.1 | 0.026 |
| ELCo, cm2/m2 | 1.00 ± 0.22 | 1.06 ± 0.25 | 1.20 ± 0.33 | 0.029 |
| Variables | AVR (n = 38) | Wheat (n = 38) | p Value |
|---|---|---|---|
| Patient characteristics | |||
| Age, years | 72 ± 8 | 74 ± 8 | 0.273 |
| Gender, male, n (%) | 25 (66) | 25 (66) | 1.000 |
| CTR on X-ray, % | 53 ± 6 | 54 ± 8 | 0.301 |
| Atrial fibrillation, n (%) | 3 (8) | 3 (8) | 1.000 |
| AS/AR, n (%) | 20 (53)/18 (47) | 22 (58)/16 (42) | 0.823 |
| Chronic kidney disease, n (%) | 16 (42) | 14 (37) | 0.815 |
| Diabetes mellitus, n (%) | 5 (13) | 6 (16) | 1.000 |
| Preoperative echocardiographic data | |||
| LVDd, mm | 44 ± 6 | 44 ± 7 | 0.776 |
| LVDs, mm | 31 ± 8 | 30 ± 8 | 0.827 |
| LVEF, % | 55 ± 9 | 56 ± 8 | 0.593 |
| Postoperative echocardiographic data | |||
| Aorta area, mm2 | 1085 ± 224 | 745 ± 189 | <0.001 |
| Aorta diameter, mm | 37.0 ± 3.9 | 30.6 ± 3.5 | <0.001 |
| PG max, mmHg | 23.6 ± 6.5 | 21.7 ± 7.8 | 0.257 |
| EOA, cm2 | 1.41 ± 0.26 | 1.37 ± 0.25 | 0.511 |
| PR, mmHg | 5.36 ± 1.77 | 6.47 ± 2.16 | 0.019 |
| PRI | 0.23 ± 0.06 | 0.30 ± 0.06 | 0.034 |
| EL, mmHg | 17.9 ± 5.4 | 14.6 ± 6.3 | 0.020 |
| ELCo, cm2/m2 | 1.01 ± 0.27 | 1.06 ± 0.25 | 0.402 |
| Variables | AVR (n = 24) | Bentall (n = 24) | p Value |
|---|---|---|---|
| Patient characteristics | |||
| Age, years | 72 ± 6 | 71 ± 6 | 0.925 |
| Gender, male, n (%) | 16 (67) | 19 (79) | 0.517 |
| CTR on X-ray, % | 54 ± 7 | 56 ± 8 | 0.236 |
| Atrial fibrillation, n (%) | 2 (8) | 2 (8) | 1.000 |
| AS/AR, n (%) | 3 (13)/21 (87) | 4 (17)/20 (83) | 0.923 |
| Chronic kidney disease, n (%) | 8 (33) | 11 (46) | 0.471 |
| Diabetes mellitus, n (%) | 6 (25) | 4 (17) | 0.724 |
| Preoperative echocardiographic data | |||
| LVDd, mm | 48 ± 9 | 48 ± 11 | 0.813 |
| LVDs, mm | 35 ± 12 | 36±12 | 0.748 |
| LVEF, % | 52 ± 10 | 51 ± 11 | 0.571 |
| Postoperative echocardiographic data | |||
| Aorta area, mm2 | 1088 ± 205 | 699 ± 115 | <0.001 |
| Aorta diameter, mm | 37.1 ± 3.6 | 29.7 ± 2.5 | <0.001 |
| PG max, mmHg | 24.5 ± 8.9 | 18.9 ± 7.9 | 0.028 |
| EOA, cm2 | 1.40 ± 0.30 | 1.46 ± 0.27 | 0.550 |
| PR, mmHg | 5.33 ± 1.64 | 6.23 ± 2.95 | 0.022 |
| PRI | 0.23 ± 0.06 | 0.33 ± 0.06 | < 0.001 |
| EL, mmHg | 18.7 ± 8.1 | 11.3 ± 4.8 | 0.001 |
| ELCo, cm2/m2 | 1.03 ± 0.32 | 1.17 ± 0.32 | 0.168 |
| Variables | Wheat (n = 21) | Bentall (n = 21) | p Value |
|---|---|---|---|
| Patient characteristics | |||
| Age, years | 74 ± 8 | 71 ± 6 | 0.180 |
| Gender, male, n (%) | 17 (81) | 17 (81) | 1.000 |
| CTR on X-ray, % | 53 ± 6 | 54 ± 8 | 0.661 |
| Atrial fibrillation, n (%) | 1 (5) | 1 (5) | 1.000 |
| AS/AR, n (%) | 10 (48)/11 (52) | 4 (19)/17 (81) | 0.100 |
| Chronic kidney disease, n (%) | 12 (57) | 9 (43) | 0.538 |
| Diabetes mellitus, n (%) | 3 (14) | 3 (14) | 1.000 |
| Preoperative echocardiographic data | |||
| LVDd, mm | 46 ± 7 | 46 ± 8 | 1.000 |
| LVDs, mm | 33 ± 8 | 34 ± 8 | 0.884 |
| LVEF, % | 54 ± 10 | 53 ± 8 | 0.958 |
| Postoperative echocardiographic data | |||
| Aorta area, mm2 | 773 ± 241 | 700 ± 127 | 0.247 |
| Aorta diameter, mm | 31.1 ± 4.3 | 29.7 ± 2.8 | 0.250 |
| PG max, mmHg | 21.8 ± 7.5 | 18.4 ± 7.9 | 0.166 |
| EOA, cm2 | 1.43 ± 0.24 | 1.49 ± 0.28 | 0.494 |
| PR, mmHg | 6.00 ± 3.04 | 6.48 ± 2.24 | 0.572 |
| PRI | 0.30 ± 0.06 | 0.34 ± 0.06 | 0.053 |
| EL, mmHg | 15.0 ± 5.9 | 10.8 ± 4.6 | 0.019 |
| ELCo, cm2/m2 | 1.01 ± 0.21 | 1.19 ± 0.33 | 0.049 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niwa, W.; Takami, Y.; Maekawa, A.; Yamana, K.; Akita, K.; Amano, K.; Matsuhashi, K.; Takagi, Y.; Abe, T. Echocardiographic Hemodynamics After Aortic Valve Replacement, Wheat, and Bentall Procedure. J. Clin. Med. 2025, 14, 7627. https://doi.org/10.3390/jcm14217627
Niwa W, Takami Y, Maekawa A, Yamana K, Akita K, Amano K, Matsuhashi K, Takagi Y, Abe T. Echocardiographic Hemodynamics After Aortic Valve Replacement, Wheat, and Bentall Procedure. Journal of Clinical Medicine. 2025; 14(21):7627. https://doi.org/10.3390/jcm14217627
Chicago/Turabian StyleNiwa, Wakana, Yoshiyuki Takami, Atsuo Maekawa, Koji Yamana, Kiyotoshi Akita, Kentaro Amano, Kazuki Matsuhashi, Yasushi Takagi, and Tomonobu Abe. 2025. "Echocardiographic Hemodynamics After Aortic Valve Replacement, Wheat, and Bentall Procedure" Journal of Clinical Medicine 14, no. 21: 7627. https://doi.org/10.3390/jcm14217627
APA StyleNiwa, W., Takami, Y., Maekawa, A., Yamana, K., Akita, K., Amano, K., Matsuhashi, K., Takagi, Y., & Abe, T. (2025). Echocardiographic Hemodynamics After Aortic Valve Replacement, Wheat, and Bentall Procedure. Journal of Clinical Medicine, 14(21), 7627. https://doi.org/10.3390/jcm14217627







